Back to Journals » Local and Regional Anesthesia » Volume 16
Quadratus Lumborum Block as a Cornerstone for Neonatal Intestinal Surgery Enhanced Recovery (ERAS): A Case Series
Authors Hoffmann C, Snow A, Chedid C, Abi Shadid C, Miyasaka EA
Received 16 July 2023
Accepted for publication 12 September 2023
Published 10 October 2023 Volume 2023:16 Pages 165—171
DOI https://doi.org/10.2147/LRA.S403567
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Cassandra Hoffmann,1 Angela Snow,2 Celine Chedid,3 Carol Abi Shadid,3 Eiichi A Miyasaka4
1Pediatric Anesthesiology, Akron Children’s Hospital, Akron, OH, USA; 2Pediatric Anesthesiology, Nemours Children’s Hospital, Wilmington, DE, USA; 3Pediatric Anesthesiology, University Hospitals Rainbow Babies and Children’s Hospital, Cleveland, OH, USA; 4Pediatric Surgery, University Hospitals Rainbow Babies and Children’s Hospital, Cleveland, OH, USA
Correspondence: Eiichi A Miyasaka, Pediatric Surgery, University Hospitals Rainbow Babies and Children’s Hospital, 11100 Euclid Ave, MAC 1000, Cleveland, OH, 44106, USA, Tel +1 216-844-3015, Fax +1 216-844-8647, Email [email protected]
Purpose: Neonates present unique challenges for pediatric surgical teams. To optimize outcomes, it is imperative to standardize perioperative care by using early extubation and multimodal analgesic techniques. The quadratus lumborum (QL) block provides longer duration and superior pain relief than other single-injection abdominal fascial plane techniques. The purpose of this case series was to report our initial experience with QL blocks in neonatal patients treated with intestinal ERAS.
Patients and Methods: Ten neonates requiring intestinal surgery at a single tertiary care center who received QL blocks between December 2019 and April 2022 for enhanced recovery were studied. Bilateral QL blocks were performed with 0.5 mL/kg of 0.25% ropivacaine per side with an adjuvant of 1 mcg/kg of dexmedetomidine.
Results: Gestational age at birth ranged from 32.2 to 41 weeks. The median age, weight, and American Society of Anesthesiologists (ASA) score at the time of surgery was 5 days [range 7.5 hours, 60 days], 2.84 kg [range 1.5, 4.5], and 3, respectively. Bilateral QL blocks were performed without complications in all patients. Two patients were outside the neonatal range from birth to surgery, but were under 42 weeks gestational age when corrected for prematurity. All patients were extubated with well-controlled pain, and no patient required reintubation within the first 24 hours. Postoperatively, median cumulative morphine equivalents were 0.16 mg/kg [range 0, 0.79] and six patients received scheduled acetaminophen. Morphine (0.1 mg/kg) was administered to patients with a modified neonatal infant pain scale (NIPS) score greater than or equal to 4, and pain was reassessed 1 hour after administration (Appendix).
Conclusion: When developing intestinal ERAS protocols, Bilateral QL blocks may be considered for postoperative analgesia in the neonatal population. Further prospective studies are required to validate this approach in neonates.
Keywords: neonatal pain, neonatal regional anesthesia, early neonatal extubation, neonatal intestinal surgery, neonatal enhanced recovery
Introduction
Neonates present unique perioperative challenges for the care teams. Several patients require complex surgical interventions and have increased perioperative morbidity and mortality rates. Prolonged intubation is associated with increased adverse respiratory events, and the pharmacodynamics of opioids in neonates varies within a narrow therapeutic window.1–4 To optimize neonatal patient outcomes, it is imperative to standardize perioperative care by using early extubation and multimodal analgesic techniques. Enhanced recovery after surgery (ERAS) protocols encourage perioperative standardization to improve the outcomes in several patient populations.
The implementation of regional techniques is often the cornerstone of enhanced recovery pathways. The addition of fascial plane blocks to postoperative pain regimens often results in decreased postoperative pain and opioid use. The quadratus lumborum (QL) block provides a longer duration of pain control than single-injection neuraxial techniques and superior pain relief compared to other fascial plane techniques for pediatric abdominal surgery.5,6 The purpose of this case series is to report our initial experience with QL blocks for neonatal intestinal ERAS.
Materials and Methods
Study Design and Population
After University Hospitals IRB approval (STUDY20221455), electronic medical records were queried retrospectively at a single tertiary care center to identify neonates requiring intestinal surgery who received QL blocks between December 2019 and April 2022 for enhanced recovery. Data pertaining to patient demographics, surgical procedures, block techniques, analgesics, and pain scores were also collected. Exclusion criteria included ASA physical status IV, local anesthetic allergy, surgical time greater than 6 hours, and significant comorbidities requiring post-operative intubation.
The study protocol was approved by the ethics committee of University Hospitals. All data were collected confidential by the authors. Written informed consent was obtained from the parents or guardians for publication of medical data and imaging materials. All procedures in the study were in accordance with the ethical standards of the Declaration of Helsinki 1964 and its later amendments or comparable ethical standards.
Anesthetic Technique
All neonates greater than 32 weeks gestational age, ASA physical status I–III, on room air or minimal oxygen requirements, with absence of apnea spells, and requiring abdominal surgery were considered candidates for early extubation and enhanced recovery with QL block. Informed consent for the regional technique was obtained from parents or guardians.
Preoperatively, null per os (NPO) status was confirmed and the patients were maintained on intravenous (IV) dextrose fluid. The perioperative care team handoff was completed and the pre-transport temperature was recorded. Patients were transported to the operating room via NICU (neonatal intensive care unit) isolette to maintain euthermic conditions. Normothermia was maintained intraoperatively using an overhead radiant warmer, underbody air warmer, and lined hat placement. The room temperature was maintained above 26 degrees Celsius at all times. General anesthesia was induced with fentanyl–1–3 ug/kg, rocuronium and maintained with sevoflurane. After the airway was secured with an endotracheal tube and a timeout was performed, the patients were turned in the lateral decubitus position and ultrasound-guided QL blocks were performed (Figure 1). A high-frequency linear ultrasound probe was placed on the iliac crest and in the transverse position to the posterior axillary line. The fourth lumbar vertebral body and its transverse process, the QL, erector spinae, and psoas muscles were also identified. A (40 mm) peripheral nerve block needle (SonoPlex) was directed towards the thoracolumbar fascia from the posterior aspect of the transducer to the posteromedial anterolateral direction between the psoas and QL muscles, anterior to the QL muscle. After needle tip confirmation with hydrodissection of normal saline, 0.5 mL/kg of 0.2% or 0.25% ropivacaine and adjuvant (0.5 mcg/kg of dexmedetomidine were injected per side), for a total of 1mL/kg of 0.2% or 0.25% ropivacaine and 1 mcg/kg of dexmedetomidine. All patients received acetaminophen 15 mg/kg intra-operatively unless contraindicated, with additional fentanyl as required to treat increases in heart rate or blood pressure greater than 20% of the baseline values. Goal-directed fluid therapy was utilized. All the patients received antibiotics according to the perioperative surgical guidelines of the hospital.
At the conclusion of the surgical procedure, patients were assessed for extubation. Patients previously receiving IV caffeine for apnea of prematurity in the NICU received one dose of caffeine citrate prior to extubation. The neuromuscular blockade was reversed using sugammadex 4 mg/kg prior to extubation. All the patients were successfully extubated in the operating room after the procedure.
Postoperatively, patients received scheduled acetaminophen and breakthrough morphine per the NICU team assessment and protocol. The exclusion criteria for scheduled IV acetaminophen included elevated bilirubin levels. Pain was assessed every 4 hours using a modified NIPS score. This pain score includes all parameters found in the NIPS score and accounts for variations in the vital signs. For patients with NIPS score greater than or equal to 4, rescue analgesia of morphine (0.1 mg/kg) was administered and pain was reassessed 1 hour after administration (Figure 2).
Data Collection and Analysis
Patient demographics, diagnoses, operative details, and anesthetic records were collected. Frequency distributions and means were determined for the baseline categorical variables.
Results
Ten neonates were identified and Table 1 presents demographic data regarding patient age, weight, and procedure. The median age and weight at the time of surgery was 5 days [range 7.5 hours, 60 days] and 2.84 kg [range 1.5, 4.5]. One patient had complex congenital heart disease and two patients had complicated comorbidities, including short bowel syndrome and adrenal insufficiency. Two patients were outside the neonatal range from birth to surgery, but were under 42 weeks gestational age when corrected for prematurity.
 |
Table 1 Demographic Data of Case Series |
No major complications occurred during any of the anesthetic or surgical procedures. Ultrasound-guided QL blocks were administered pre-operatively in 5 patients and post-operatively in 5 patients. The timing of block administration was left to the discretion of the anesthetic provider. Most post-operative blocks are performed in cases with increased surgical time, as a postoperative block provides full benefit and duration of the regional technique for postoperative analgesia. Patients received standard 0.5mL/kg volume dosing of local anesthetic for the quadratus lumborum block with either 0.2% or 0.25% ropivacaine. Dexmedetomidine (1 mcg/kg) was added as a block adjunct to prolong block duration. All patients were extubated at the end of the procedure, and none required reintubation within the first 24 hours after surgery. Three patients with a history of apnea of prematurity received IV caffeine prior to extubation, but did not receive any additional caffeine after their arrival back to the NICU. The median post-operative morphine equivalents were 0.16 mg/kg [range 0, 0.79]. Six patients received scheduled IV acetaminophen 48 hours after surgery (Table 2).
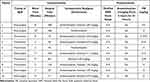 |
Table 2 Block Data, Intraoperative and Post-Operative Pain Requirements |
Discussion
Standardization of perioperative care is essential to optimize patient outcomes. Implementation of ERAS protocols has been shown to reduce post-surgical complications, hospital length of stay, hospital costs, and improve patient satisfaction. The addition of multimodal analgesia and regional anesthesia techniques is vital for its success.
Neonates have significant pain management limitations with variable opioid pharmacodynamic profiles and a narrow therapeutic window. These limitations often contribute to the occurrence of apnea and development of tolerance, which can require postoperative intubation. Prolonged intubation has been associated with an increased incidence of adverse respiratory events.
In addition, neuraxial techniques present technical challenges with potentially significant neurological complications1–4 and often require a catheter for a prolonged duration of blockade and adequate postoperative pain control. Fascial plane blocks have the benefit of increased block duration and allow the provider to forgo the catheter placement. The QL block has been proven superior to other abdominal fascial plane techniques and caudal for postoperative pain control.5,6 The inclusion of multimodal and regional anesthesia techniques provides a solution for the development and adaptation of ERAS protocols for neonatal patients. Recent ERAS Society initiatives have led to consensus guidelines for neonatal intestinal surgery.7,8
In 2020, the ERAS Society developed consensus guidelines for perioperative care in neonatal intestinal surgery encompassing preoperative, intraoperative, and postoperative elements to enhance the quality of care in neonatal abdominal surgery.9 The guidelines were limited to neonates > 37 weeks of gestation without major comorbidities, who underwent intestinal resection surgery within the first 4 weeks of life. Patients with complex surgical conditions, such as necrotizing enterocolitis, abdominal wall defects, and short bowel syndrome, were excluded. Consensus evidence on perioperative analgesia supports the use of multimodal analgesia in the postoperative period, with high-quality and strong evidence to support scheduled postoperative acetaminophen and the use of regional techniques. Additional recommendations of moderate quality and strong evidence were identified for using an opioid-limiting strategy and managing breakthrough pain with the lowest effective dose of opioids.
The quadratus lumborum block was first described by Blanco et al in 2007, with the local anesthetic deposited anterolaterally to the QL muscle. Since then, modifications have been made to the location of local anesthetic deposition. Several studies have compared the safety and efficacy of different injection techniques.10,11
Multiple case reports have described the success of the transversus abdominal plane block in neonatal abdominal surgery.12–14 One study evaluated blood bupivacaine concentrations after a transversus abdominis plane (TAP) block to identify the safe plasma levels of local anesthetics after fascial plane blocks in neonates. The highest upper prediction limit for blood concentration was significantly lower than potentially toxic plasma levels, suggesting a low risk of local anesthetic toxicity in neonates after abdominal fascial plane blocks.15
Zhao et al conducted a meta-analysis of seven randomized controlled trials, including a total of 346 pediatric patients undergoing lower abdominal surgery, in which the quadratus lumborum block was compared to other analgesic techniques. Lower abdominal surgeries included inguinal hernia repair, orchiopexy, and hydrocelectomy. The primary outcome measured was the rate and time to postoperative rescue analgesia, and the secondary outcomes included postoperative pain scores, patient satisfaction, and block-related complications. The QL block resulted in a significant reduction in the rate of rescue analgesia in the first 24 hours and reduced pain scores at 2, 4, and 12 hours postoperatively.16
The role of QL block in the neonatal population is yet to be well described. Recently, a case report described the use of bilateral QL blocks in a term neonate undergoing laparoscopic ovarian cyst removal. Their use of bilateral QL blocks with intraoperative and postoperative acetaminophen allowed for an opioid-free anesthetic.17 This case series focuses on the introduction of QL block for neonatal intestinal ERAS. Building on the current ERAS society guidelines, we developed and implemented a protocol for neonatal patients utilizing the QL block as the regional technique of choice in conjunction with scheduled IV acetaminophen for postoperative pain control. In contrast to the ERAS society guidelines, three patients were less than 37 weeks post-conceptual age (PCA) at the time of surgery, one patient had complex congenital heart disease, and two patients had complicated comorbidities including short bowel syndrome and adrenal insufficiency. Despite the current guidelines, these techniques may benefit patients with more complex physiology. The implementation of neonatal intestinal ERAS resulted in successful extubation in the immediate post-operative period and allowed for adequate postoperative pain control. If patients required rescue analgesia, successful pain treatment was achieved with an opioid-limiting strategy utilizing a reduced dose.
The limitations of this case series include the small sample size and lack of a control group, which can result in bias. Additional prospective studies are needed to further evaluate the use of QL blocks for neonatal enhanced recovery.
Conclusion
The addition of QL blocks and scheduled acetaminophen administration for neonatal intestinal ERAS may provide effective postoperative analgesia and minimize postoperative opioid requirements. Additional research is required to evaluate the potential role of QL blocks as a regional technique for neonatal intestinal ERAS.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
1. Disma N, Veyckemans F, Virag K, et al. Morbidity and mortality after anesthesia in early life: results of the European prospective multicenter observational study, neonate and children audit of anesthesia practice in Europe (NECTARINE). BJA. 2021;126(6):1157–1172. doi:10.1016/j.bja.2021.02.016
2. Wakimoto Y, Burjonrappa S. Enhanced recovery after surgery (ERAS) protocols in neonates should focus on the respiratory tract. Pediatr Surg Int. 2019;35(6):635–642. PMID: 30712081. doi:10.1007/s00383-019-04437-w
3. Pacifici GM. Clinical pharmacology of fentanyl in preterm infants. A review. Ped Neonatol. 2015;56(3):143–148. doi:10.1016/j.pedneo.2014.06.002
4. Harris KC, Holowachuk S, Pitfield S, et al. Should early extubation be the goal for children after congenital cardiac surgery? J Thorac Cardiovasc Surg. 2014;148(6):2642–2648. doi:10.1016/j.jtcvs.2014.06.093
5. Dontukurthy S, Mofidi R. The role of interfascial plane blocks in pediatric regional anesthesia: a narrative review of current perspectives and updates. Anesthesiol Res Pract. 2020;2020:8892537. doi:10.1155/2020/8892537
6. Öksüz G, Bilal B, Gürkan Y, et al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med. 2017;42(5):674–679. doi:10.1097/AAP.0000000000000645
7. Altman AD, Helpman L, McGee J, et al. Enhanced recovery after surgery: implementing a new standard of surgical care. CMAJ. 2019;191(17):E469–E475. doi:10.1503/cmaj.180635
8. Brindle ME, Heiss K, Scott MJ, et al. Embracing change: the era for pediatric ERAS is here. Pediatr Surg Int. 2019;35(6):631–634. doi:10.1007/s00383-019-04476-3
9. Brindle ME, McDiarmid C, Short K, et al. Consensus guidelines for perioperative care in neonatal intestinal surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2020;44(8):2482–2492. doi:10.1007/s00268-020-05530-1
10. Hussein M. Ultrasound-guided quadratus lumborum block in pediatrics: transmuscular versus intra-muscular approach. J Anesth. 2018;32(6):850–855. doi:10.1007/s00540-018-2563-z
11. Akerman M, Pejčić N, Veličković I. A Review of the Quadratus Lumborum Block and ERAS. Front Med. 2018;5:44. doi:10.3389/fmed.2018.00044
12. Jacobs A, Bergmans E, Arul GS, Thies K-C. The transversus abdominis plane (TAP) block in neonates and infants – results of an audit. Pediatr Anesth. 2011;21(10):1078–1080. doi:10.1111/j.1460-9592.2011.03628.x
13. Hardy CA. Transverse abdominis plane block in neonates: is it a good alternative to caudal anesthesia for postoperative analgesia following abdominal surgery? Pediatr Anesth. 2009;19(1):56. doi:10.1111/j.1460-9592.2008.02742.x
14. Bielsky A, Efrat R, Suresh S. Postoperative analgesia in neonates after major abdominal surgery: “TAP” our way to success! Pediatr Anesth. 2009;19(5):541–542. doi:10.1111/j.1460-9592.2009.02988.x
15. Suresh S, De Oliveira GS. Blood bupivacaine concentrations after transversus abdominis plane block in neonates: a prospective observational study. Anesth Analg. 2016;122(3):814–817. doi:10.1213/ANE.0000000000001088
16. Zhao W, Li S, Wu B, et al. “Quadratus lumborum block is an effective postoperative analgesic technique in pediatric patients undergoing lower abdominal surgery: a meta-analysis. Pain Physician. 2021;24(5):E555–E563.
17. Smedile F, Giordano G, Padua M, Pariante R. Bilateral Quadratus Lumborum block in a neonate having undergone laparoscopic ovarian cyst removal. Indian J Anaesth. 2020;64(11):995–997. doi:10.4103/ija.IJA_382_20
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


