Back to Journals » Clinical Ophthalmology » Volume 17
Public and Physicians Perception of Oculoplastic Surgery Subspecialty in Saudi Arabia
Authors Baghazal A , Hanafi S, Bogari A
Received 13 June 2023
Accepted for publication 14 August 2023
Published 22 August 2023 Volume 2023:17 Pages 2493—2504
DOI https://doi.org/10.2147/OPTH.S425712
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Alaa Baghazal,1 Somaya Hanafi,1 Ahmad Bogari2
1Department of Ophthalmology, King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia; 2Department of Otorhinolaryngology, Head and Neck Surgery, Ministry of Health, Riyadh, Saudi Arabia
Correspondence: Alaa Baghazal, Email [email protected]
Objective: Oculoplastic surgery is a highly specialized subspecialty that studies pathologies of the orbit, lacrimal system, and eyelids. Although it is an independent ophthalmological subspecialty, many procedures fall within the shared scope and anatomical area of oculoplastic surgery, otorhinolaryngology, and plastic and reconstructive surgery, which tend to confuse physicians and patients seeking medical advice. In this study, our goal is to evaluate the perception of oculoplastic surgery among the public and physicians.
Methodology: A cross-sectional study in which data were collected from an online questionnaire formulated by the authors. The questionnaire included 18 questions divided into two categories: demographics and targeted questions that serve the objective of the study. Each answer option to targeted questions was encoded with either one or zero points, and each participant’s response was scored accordingly, with the maximum score being 22 points, reflecting the highest perception rate according to the questionnaire.
Results: Data were collected from 1029 questionnaire responses, with 202 of the respondents belonging to physicians. The highest number of responses was from females which consisted 82% of our sample. Perception scores were higher among physicians with a mean of 12.3 ± 2.9 points compared to a mean score of 11.2 ± 2.9 among the public. Age played a statistically significant factor in both physicians and the public as younger participants’ scores were higher.
Conclusion: Insufficient knowledge of oculoplastic surgery subspecialty was observed among the public and physicians. Moreover, core aspects of oculoplastic field such as lacrimal system pathology and orbit pathology were less recognized by participants of our study, which highlights the importance of raising awareness of oculoplastic surgery and the diversity of the field, to enhance referral patterns among physicians and improve medical advice seeking among the public resulting in better health care.
Keywords: oculoplastic surgery, public perception, physicians’ perception, Saudi Arabia
Introduction
Oculoplastic surgery is a highly specific subspecialty that studies pathologies of the orbit, lacrimal system, and eyelids. It has rapidly evolved since the Second World War, when victims suffered facial injuries that necessitated highly specialized reconstructive surgeries. Although it is an independent ophthalmological subspecialty, many procedures fall within the shared scope of oculoplastic surgery, otorhinolaryngology and plastic and reconstructive surgery, considering the same anatomical area.1 Oculoplastic procedures can be purely aesthetic, reconstructive, therapeutic, diagnostic, or functional. Due to the high demand of aesthetic procedures worldwide and the expanding influence of social media advertising for cosmetic procedures, oculoplastic surgery has been gaining more interest among ophthalmologists and the public.1,2 However, misperceptions can occur due to the surgical overlap between oculoplastic surgery and other surgical specialties.3 Literature has documented a lack of awareness of ophthalmological conditions among the public. Moreover, physicians have been deficient in knowledge regarding common emergent ophthalmological conditions, which could reflect the lack of exposure to ophthalmology during medical training and subsequently less convenience when encountering ophthalmic complaints.4–7 In this study, we aim to evaluate the perception of oculoplastic subspecialty among the public and physicians.
Materials and Methods
Study Design, Study Subjects and Study Tool
A cross-sectional study in which data were collected from an online questionnaire formulated by the authors and randomly distributed by non-medical data collectors. Distribution of questionnaire was free of selection control and responses were collected anonymously. The study population consisted of participants aged from 20 to 70 years who live in Saudi Arabia; however, ophthalmologists were excluded from the study. The online questionnaire included 18 questions divided into two main categories: demographics and targeted scored questions that serve the objective of the study. Questions were either of multiple choice or checkbox type. Each answer option to scored questions was encoded with either one or zero points, and each participant’s response was scored accordingly, with the maximum score being 22 points, reflecting the highest perception rate according to the questionnaire. The questionnaire was originally written in English then translated to Arabic by a bilingual familiar with medical terms, followed by back translation into English by a bilingual familiar with medical term and blind to the original form. A pilot study was conducted on 25 participants to ensure the questionnaire efficiency and accurate interpretation of the questionnaire content by the participants.
Statistical Analysis
A Pearson’s Chi-squared test was used to assess the differences in demographic characteristics in terms of different factors that might have influenced the choice of a surgeon for cosmetic purposes. The difference in knowledge score between physicians and non-physicians was assessed using a Wilcoxon rank sum test. For the factors associated with knowledge scores among subgroups of physicians and non-physicians, we used a Wilcoxon rank sum test for variables with two categories and a Kruskal–Wallis rank sum test for variables with three or more categories. The significantly associated variables from the inferential analysis were further used as independent variables in two multivariable general linear models (using the knowledge scores of physicians and non-physicians in each model as dependent variables). The outcomes of the regression analysis were expressed as beta coefficients and 95% confidence intervals (95% CIs). A p value of <0.05 indicated statistical significance.
Ethical Considerations
Privacy and confidentiality of participants were maintained throughout the study. All participants provided informed consent, in accordance with the Declaration of Helsinki. Ethical approval was obtained from King Fahad Armed Forces Hospital Research and Ethics Committee (reference number: REC497).
Results
Demographic
A total of 1029 records were analyzed with physicians constituting 19.6% of the sample (202 respondents). A female predominance was noted as they represented 82% of total responses, 75.2% of physicians and 83.7% of the public respondents. Demographic characteristics are illustrated in Table 1. Suboptimal perception scores were observed in all questionnaire respondents, however, lower scores belonged to the public. The median knowledge score for the public was 11.0 (9.0 to 13.0), the minimum was 3.0 and the maximum was 22.0. Physicians had a higher knowledge score with a median of 12 (10.0 to 14.0), the minimum was 3.0 and the maximum was 21.0. Further descriptive analysis of knowledge scores is shown in Table 2 and Figure 1. Focusing on physicians, the highest number of responses belonged to obstetrics and gynecology followed by dentistry and internal medicine Figure 2. Knowledge score did not differ significantly based on the occupational degree (p = 0.543), history of visiting an oculoplastic surgeon (p = 0.754) or undergoing facial cosmetic procedures (p = 0.775). Knowledge scores differed significantly based on age (p = 0.035) and being specialized in emergency medicine (p = 0.029), pathology (p = 0.047) and radiology (p = 0.034) Table 3. On the adjusted analysis, higher knowledge scores were independently associated with being specialized in emergency medicine (OR = 4.0, 95% CI, 1.5 to 6.5, p = 0.002) and radiology (OR = 1.8, 95% CI, 0.1 to 3.5, p = 0.035). Conversely, physicians aged 40 to 49 years had significantly lower knowledge scores (OR = −1.8, 95% CI, −3.1 to −0.6, p = 0.004) Table 4. Among the public, there were significant differences in knowledge scores based on participants’ ages (p = 0.001) and occupation (p = 0.015). Knowledge score did not differ significantly based on the history of visiting an oculoplastic surgeon (p = 0.708), or history of undergoing facial cosmetic procedures (p = 0.286). Table 5. Multivariable regression analysis revealed that participants aged 50 to 59 years were independently associated with having low knowledge scores (OR = −0.7, 95% CI, −1.4 to −0.04, p = 0.038) Table 6.
 |
Table 1 Demographic and Occupational Characteristics (n = 1029) |
 |
Table 2 Descriptive Analysis of Knowledge Score Among the Overall Sample, Physicians, and Non-Physicians |
 |
Table 3 Factors Associated with Knowledge Scores Among Physicians (n = 202) |
 |
Table 4 Predictors of High Knowledge Scores Among Physicians (n = 202) |
 |
Table 5 Factors Associated with Knowledge Scores Among Non-Physicians (n = 827) |
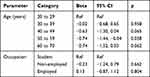 |
Table 6 Predictors of High Knowledge Scores Among Non-Physicians (n = 827) |
 |
Figure 1 Boxplots depicting the difference in knowledge scores between physicians and non-physicians (n = 1029). |
 |
Figure 2 The percentages of physicians’ specialties (n=202). |
Understanding the Role of an Oculoplastic Surgeon
When asked who an oculoplastic surgeon is through a multiple-choice question, 66.5% of the public chose an ophthalmologist subspecialized in oculoplasty in contrast to 81.2% of the physicians. Moreover, participants were given a list of surgeries including eyelid, orbit, lacrimal, cataract, retina, glaucoma, refractive, and strabismus surgery, and were asked to choose what oculoplastic surgery concerned, 93.1% of physicians chose eyelid surgery; however, only 54.5% and 37.1% thought an oculoplastic surgeon would perform orbit and lacrimal surgery, respectively. Non-physicians answered similarly with a percentage of 89.2%, 47.6%, and 30.6% for eyelid surgery, orbit surgery, and lacrimal surgery, respectively. Also, participants were given a list of conditions including eyelid tumors, eyelid reconstruction, orbital wall fractures, orbital lesions, lacrimal pathology, uveitis, optic nerve pathology, glaucoma, and strabismus, then were asked to choose what can be managed by an oculoplastic surgeon. Most physicians thought that eyelid tumors (77.2%), eyelid reconstruction (92.1%), and orbital wall fractures (50.5%) are managed by an oculoplastic surgeon. However, only 34.7% and 41.6% chose orbital lesions and lacrimal pathology, respectively. In contrast, of the public 60.3%, 83.1%, 45.5%, 27.7% and 26.2% chose eyelid tumors, eyelid reconstruction, orbital wall fractures, orbital lesions, and lacrimal pathology, respectively. On a further note, more than 40% of all participants thought that an oculoplastic surgeon deals with strabismus and performs strabismus surgery, similarly, almost 40% of all participants thought that refractive surgery falls within oculoplastic surgery scope. Additionally, participants were asked about their choice of a surgeon for ptosis management through a checkbox question, 82.7% of physicians and 75.8% of the public chose an oculoplastic surgeon, 32.2% of physicians and 44.4% of the public chose a plastic and reconstructive surgeon, and 5.4% of physicians and 4.6% of the public chose an otorhinolaryngologist surgeon subspecialized in facial plastic surgery (FPS). Likewise, when asked about participants’ choice of a surgeon for proptosis management through a check-box question, 90.6% of physicians and 86% of the public chose an oculoplastic surgeon, and 18.8% of physicians and 30.6% of the public chose a plastic and reconstructive surgeon, and 5% of physicians and 6.2% of the public chose an otorhinolaryngologist surgeon subspecialized in FPS, respectively.
Understanding the Surgical Overlap Between Oculoplastic Surgeon, Plastic and Reconstructive Surgeon, and Otorhinolaryngologist Surgeon Subspecialized in Facial Plastic Surgery
Some conditions like dermatochalasis, eyelid tumors, and nasolacrimal duct obstruction are not limited to oculoplastic surgery, considering the shared anatomical area between oculoplastic surgery and other surgical specialties. Participants were asked who were qualified to do eyelid cosmetic procedures, 54% of physicians and the public chose a plastic and reconstructive surgeon, 81.7% of physicians and 66.9% of the public chose an oculoplastic surgeon, and 11.4% of physicians and 7.6% of the public chose an otorhinolaryngologist surgeon subspecialized in FPS. Moreover, participants were asked to select one or more surgeons whom they are likely to visit for blepharoplasty, eyelid tumors, and nasolacrimal duct obstruction. Most physicians were more likely to visit an oculoplastic surgeon for blepharoplasty (83.2%), eyelid tumors (92.6%), and nasolacrimal duct obstruction (91.1%). The public responded similarly with a percentage of 78.5%, 86.6%, and 83.2% for each blepharoplasty, eyelid tumor, and nasolacrimal duct obstruction, respectively. A less percentage of physicians were likely to visit a plastic and reconstructive surgeon for blepharoplasty 37.1% and eyelid tumors 17.8%; however, a few chose an otorhinolaryngologist surgeon subspecialized in FPS for blepharoplasty 5% and eyelid tumors 5.4%. Similarly, the public were less likely to visit a plastic and reconstructive surgeon for each blepharoplasty 45% and eyelid tumor 23%. Furthermore, physicians and the public were more likely to choose an otorhinolaryngologist surgeon subspecialized in FPS over a plastic and reconstructive surgeon for the treatment of nasolacrimal duct obstruction with a percentage of 19.2% compared to 12.2%. To conclude, the selection pattern of answers was similar among physicians and the public for all three given conditions. An otorhinolaryngologist surgeon subspecialized in FPS was unlikely to be chosen for blepharoplasty and eyelid tumors, however, participants thought that an otorhinolaryngologist surgeon subspecialized in FPS is more likely to treat nasolacrimal duct obstruction than a plastic and reconstructive surgeon. In contrast, most participants were likely to visit an oculoplastic surgeon for all three given conditions. Table 7 demonstrates a detailed description of participants’ responses to knowledge items.
 |
Table 7 Participants’ Responses to Knowledge Items (n = 1029) |
Factors That Influenced the Choice of a Surgeon for Cosmetic Purpose
Among physicians, the most common factors that influenced their perception were the advice from other physicians 81.7% and the experience of relatives and friends 68.3% Figure 3A. The influence of relatives and friends’ experience was significantly higher among participants aged 20–29 years 84.5% compared to other age categories, including 30–39 years 67.2%, 40–49 years 63%, 50–59 years 40%, and 60–70 years 44.4%. Conversely, the influence of advice from another doctor was significantly lower among physicians aged 20–29 years 69% than those aged 30–39 years 85.1%, 40–49 years 85.2%, 50–59 years 100% and 60–70 years 96.3%. In contrast, the most reported influencing factors by the public were Google search 81.5% and social media 70.7% Figure 3B. The impact of relatives’ and friends’ experience decreased significantly with advanced age from 76.4% to 74.2%, 63.8%, 65.3%, and 58.7%, and the impact of social media decreased also from 37.9% to 31.3%, 27.5%, 29.5% and 17.4% among those aged 20–29 years, 30–39 years, 40–49 years, 50–59 years, and 60–70 years, respectively. Non-employed respondents were significantly less influenced by the experience of relatives and friends 63.5% than students 76.7% and employed participants 71.8%.
 |
Figure 3 The percentages of participants’ responses regarding the factors that influenced the choice of a surgeon for cosmetic purposes among physicians (A) and non-physicians (B). |
Discussion
Although oculoplastic surgery subspeciality is gaining more interest in recent years, there seems to be a misconception of its scope among physicians and the public. This misconception can be attributed to multiple factors including and not limited to surgical overlap between oculoplastic surgery and other surgical specialties and the growing effect of social media on aesthetic surgeries.1,8,9 The significance of a true consistent image of oculoplastic surgery can be reflected greatly in health care, especially in referral patterns between physicians which require knowledge of vital aspects in the field. Furthermore, awareness of the role of an oculoplastic surgeon among the public has a major influence on seeking medical advice. Misconceptions of plastic surgery and facial plastic surgery were documented by multiple studies in the literature,3,8,10–13 and this could be reflected in oculoplastic surgery as they share a common scope which is aesthetic surgeries. Low levels of knowledge in oculoplastic surgery have been reported among medical students in Saudi Arabia.11 In fact, knowledge about ophthalmological conditions in general was non-sufficient among physicians and the public in several studies,4–7 however, no studies evaluated knowledge and perception of oculoplastic surgery among physicians and the public. Our study showed that knowledge about the diversity of oculoplastic field was the most deficient in our sample, as participants were more likely to be informed about aesthetic aspects of the field but lack information about core aspects of the field such as lacrimal system and orbit conditions. Similar findings were reported in a study that evaluated the perception of plastic and reconstructive surgery among the public and physicians, where patients lacked knowledge about core non-aesthetic aspects of the field such as hand surgery and burns.14 Nowadays, social media has a significant influence on our society, and many seek medical information through social media,15–17 a study by Montemurro et al showed that 95% of patients use the internet before visiting a plastic surgeon for an aesthetic procedure and 46% used social media,18 this increases the demand on physicians to share their knowledge on social media platforms to educate the public. Dorfman et al reported that most plastic surgery-related content on Instagram was posted by non-board-certified surgeons, and a minority of posts were for educational purposes, reflecting the likelihood of spreading inaccurate information, and the potential risk to patients’ health.16 Moreover, a study by Park et al showed that well-established Instagram accounts by certified oculoplastic surgeons are still few in the United States, and mostly belonged to physicians who work in private sections, reflecting the pressure on them to expand their reach and the paucity of educational driven accounts.17 Similarly, in our study, the most reported influencing factors while choosing a surgeon for an aesthetic purpose by the public were Google search 81.5% and social media 70.7%. Therefore, we encourage oculoplastic surgeons to raise awareness about the diversity of oculoplastic surgery field through social media platforms, campaigns, and brochures. Moreover, we encourage raising awareness among physicians about the role of an oculoplastic surgeon to improve health care and promote optimal referral patterns. Limitations of our study include an insufficient number of physicians, as our physicians’ sample may be not representative; moreover, more studies are needed to consolidate the findings of our study as no similar studies evaluating oculoplastic surgery perception among physicians or the public were found in the literature.
Conclusion
Insufficient knowledge of oculoplastic surgery subspecialty was observed among the public and physicians, and core aspects of the field such as lacrimal system pathology and orbit pathology were less recognized by participants of our study. This could lead to difficulties reaching an oculoplastic surgeon when required and errors during physicians’ referrals. Moreover, we would like to highlight the expanding demand for evidence-based medicine by qualified physicians on social media platforms; therefore, it is our recommendation to increase awareness of oculoplastic surgery and encourage oculoplastic surgeons to be active on social media platforms through educational accounts to spread awareness, share knowledge and expand their reach.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Disclosure
Authors declare no conflict of interest in this research.
References
1. Saleh GM, Athanasiadis I, Collin JRO. Training and oculoplastics: past, present and future. Orbit. 2013;32(2):111–116. doi:10.3109/01676830.2013.764448
2. Heidekrueger PI, Juran S, Ehrl D, Aung T, Tanna N, Broer PN. Global aesthetic surgery statistics: a closer look. J Plast Surg Hand Surg. 2017;51:270–274. doi:10.1080/2000656X.2016.1248842
3. Gill P, Bruscino-Raiola F, Leung M. Public perception of the field of plastic surgery. ANZ J Surg. 2011;81:669–72. 10.1111/J.1445–2197.2011.05753.x. doi:10.1111/j.1445-2197.2011.05753.x
4. Attebo K, Mitchell P, Cumming R, Smith W. Knowledge and beliefs about common eye diseases. Aust N Z J Ophthalmol. 1997;25:283–287. doi:10.1111/j.1442-9071.1997.tb01516.x
5. Uhr JH, Mishra K, Wei C, Wu AY. Awareness and knowledge of emergent ophthalmic disease among patients in an internal medicine clinic. JAMA Ophthalmol. 2016;134:424–431. doi:10.1001/JAMAOPHTHALMOL.2015.6212
6. Uhr JH, Governatori NJ, Zhang QE, et al. Training in and comfort with diagnosis and management of ophthalmic emergencies among emergency medicine physicians in the United States. Eye. 2020;34:1504–1511. doi:10.1038/s41433-020-0889-x
7. Li B, Michaelov E, Waterman R, Sharan S. Ophthalmology as a career choice among medical students: a survey of students at a Canadian medical school. BMC Med Educ. 2022;22(1):225. doi:10.1186/s12909-022-03295-w
8. Schmuter G, North VS, Kazim M, Tran AQ. Medical accuracy of patient discussions in oculoplastic surgery on social media. Ophthalmic Plast Reconstr Surg. 2023;39(2):132–135. doi:10.1097/IOP.0000000000002257
9. Tingley J, Allen RC, Barmettler A. Oculoplasticsandsocialmedia: a review of social media in oculoplastics and relevant subspecialties. Orbit. 2022;41:141–149. doi:10.1080/01676830.2021.1930064
10. Mortada HH, Alqahtani YA, Seraj HZ, Albishi WK, Aljaaly HA. Perception of plastic surgery and the role of media among medical students: cross-sectional study. Interact J Med Res. 2019;8:e12999. doi:10.2196/12999
11. Seraj H, Mortada H. Knowledge and awareness of oculoplastic surgery among medical students. Int J Med Res Health Sci. 2019;8:86–92.
12. Almarghoub MA, Almarzouq SF, Alissa SI. Public perception of plastic surgery in Saudi Arabia. Plast Reconstr Surg Glob Open. 2019;7(3):e2143. doi:10.1097/GOX.0000000000002143
13. Rosenthal E, Clark JM, Wax MK, Cook TA. Emerging perceptions of facial plastic surgery among medical students. Otolaryngol Head Neck Surg. 2001;125(5):478–482. doi:10.1067/mhn.2001.119676
14. Dunkin CSJ, Pleat JM, Jones SAM, Goodacre TEE. Perception and reality - a study of public and professional perception of plastic surgery. Br J Plast Surg. 2003;56:437–443. doi:10.1016/s0007-1226(03)00188-7
15. ALBalawi HB, Alraddadi O. Ophthalmology practice and social media influences: a patients based cross-sectional study among social media users. Int J Environ Res Public Health. 2022;19(21):13911. doi:10.3390/ijerph192113911
16. Dorfman RG, Vaca EE, Mahmood E, Fine NA, Schierle CF. Plastic surgery-related hashtag utilization on Instagram: implications for education and marketing. Aesthet Surg J. 2018;38:332–338. doi:10.1093/asj/sjx120
17. Park SSE, Akella SS, Moon JY, et al. Building your brand: analysis of successful oculoplastic surgeons on social media. Ophthalmic Plast Reconstr Surg. 2020;36:582–589. doi:10.1097/IOP.0000000000001654
18. Montemurro P, Porcnik A, Heden P, Otte M. The influence of social media and easily accessible online information on the aesthetic plastic surgery practice: literature review and our own experience. Aesthetic Plast Surg. 2015;39:270–277. doi:10.1007/s00266-015-0454-3
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
