Back to Journals » Psychology Research and Behavior Management » Volume 16
Psychotic-Like Experiences and Suicidal Ideation Among Adolescents: The Chain Mediating Role of Insomnia Symptoms and Resilience
Authors Luo X, Yu T, Yang Z, Wang D
Received 7 July 2023
Accepted for publication 25 August 2023
Published 1 September 2023 Volume 2023:16 Pages 3519—3530
DOI https://doi.org/10.2147/PRBM.S426363
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Xi Luo,1– 3 Taowen Yu,4 Zilu Yang,5 Dongfang Wang6
1School of Educational Science, Hunan Normal University, Changsha, Hunan Province, People’s Republic of China; 2Cognition and Human Behavior Key Laboratory of Hunan Province, Changsha, Hunan Province, People’s Republic of China; 3Hunan First Normal University, Changsha, Hunan Province, People’s Republic of China; 4Department of Applied Psychology, Changsha Normal University, Changsha, Hunan Province, People’s Republic of China; 5College of Education, Hunan Agricultural University, Changsha, Hunan Province, People’s Republic of China; 6Guangdong Key Laboratory of Mental Health and Cognitive Science, Ministry of Education Key Laboratory of Brain Cognition and Educational Science, Centre for Studies of Psychological Applications, School of Psychology, South China Normal University, Guangzhou, Guangdong Province, People’s Republic of China
Correspondence: Taowen Yu, Department of Applied Psychology, Changsha Normal University, Xingsha Road, Changsha, People’s Republic of China, Email [email protected] Dongfang Wang, School of Psychology, South China Normal University, Shipai Road, Guangzhou, People’s Republic of China, Email [email protected]
Background: Individuals who experience psychotic-like experiences (PLEs) are at significant risk of suicide-related behaviors. This two-wave longitudinal study aimed to investigate the relationships among PLEs, insomnia symptoms, resilience, and suicidal ideation (SI) among adolescents.
Methods: A total of 2231 college students [mean age (standard deviation) = 20.02 (1.39) years] completed two web-based surveys. Participants completed self-report measures of sample characteristics, PLEs, insomnia symptoms, resilience, and SI.
Results: The findings indicated a significantly positive correlation between PLEs and SI that was sequentially mediated by insomnia symptoms and resilience. Furthermore, insomnia symptoms and resilience played a chain-mediating role between PLEs and adolescent SI.
Conclusion: These findings suggest potential mechanism for the PLEs-SI link, which helps us better understand how PLEs can influence individual SI and provides important information for early prevention.
Keywords: psychotic-like experiences, insomnia symptoms, resilience, suicidal ideation, adolescents
Introduction
The suicide rates among adolescents world-wide has increased significantly in recent decades.1 Suicide is the second main cause of death among adolescents aged 10–24 years.2 Suicidal ideation (SI), or suicidal thoughts,3 is one of the strongest predictors of eventual suicidal behavior.4 According to previous studies, the pooled prevalence of adolescent SI within the last year in low- and middle-income countries is 16.2%.5 A large number of scholars have conducted in-depth research on adolescent SI and for this reason many of the risk factors have been well explored.
Psychotic-like experiences (PLEs) are defined as the resemblance of positive symptoms of psychosis in the absence of a full-blown psychotic disorder and as subthreshold psychotic symptomatology in the general population.6,7 PLEs are prevalent in the adolescent population, with 17% of children aged 9–12 years and 7.5% of adolescents aged 13–18 years experiencing PLEs.8 One study of UK adolescents aged 12–24 years showed that 8.1% of participants had PLEs.9 Recent evidence suggests that 15.4% of Chinese adolescents aged 10–20 years have current frequent PLEs.10 According to the psychosis proneness-persistence-impairment model,11 genetic predisposition influences widely distributed and transitory population expression of psychosis during development. In other words, these genetic factors may interact with environmental factors during childhood, which may lead to biological and psychological sensitization. These traits have the potential to contribute to the persistence of common, transitory developmental PLEs with adverse outcomes. Sufficient evidence suggested that PLEs in adolescence can predict the development of subsequent psychotic disorders (eg, schizophrenia)12,13 and non-psychotic disorders (eg, depression).14,15 Moreover, the existing research suggests that having PLEs is associated with an elevated risk of occurrence of suicidality.16,17 One meta-analysis revealed that people with PLEs might be twice as likely to report SI.18 The link between PLEs and SI still exists after adjusting for previous mental disorders.19 Among these studies, PLEs were estimated as a whole rather than as distinct subtypes, such as delusional and hallucinatory experiences. Given the occurrence of PLEs and SI during adolescence and their association, screening of PLEs and its different components may be particularly important for suicide prevention efforts in the adolescent age group and college settings. Moreover, the PLEs-SI link can be explained by psychosocial factors and common causes that contribute to cumulative stress.16,20 The specific mechanisms between PLEs and SI, however, remain unknown.
Insomnia symptoms are also not uncommon among adolescents,21 serving as a robust risk factor for adolescent suicidality.22,23 Wang et al found that insomnia symptoms might affect the development and persistence of SI during COVID-19 lockdown.24 Meanwhile, insomnia commonly co-occurs with PLEs. Insomnia symptoms appear to increase risk of PLEs, which in turn will increase sleep disturbance, leading to a potential cycle of experiential reinforcement.25 Cross-sectional evidence showed that higher PLEs are associated with poorer sleep quality in college students.26 A recent survey of 938 adolescents aged 14–25 years revealed that baseline PLEs not only associated the subsequent presentation of insomnia but also correlated with its severity.27 This finding suggests that increased PLEs are associated with greater insomnia symptoms, and in turn, an elevated risk of insomnia symptoms can predict SI. Thus, insomnia symptoms may be an underlying mediating mechanism between PLEs and SI.
Resilience refers to the capacity of adapting well over time in the face of adverse conditions or recover from negative life events.28 Theoretically, resilience is a dynamic process in which individuals show positive adaptations to stress, crises, and adversity.29 Based on the Resilience Framework theory, resilience may be a modifiable factor,30 negative life events possibly lead to adverse mental outcomes, including impairment of resilience.31,32 Thus, we hypothesize that PLEs may be a stressor for adolescents that reduces their level of resilience. Indeed, clinical observational research has shown that individuals who suffering from PLEs have a lower level of resilience than those without PLEs.33 One survey of 432 college students also found that higher PLEs are associated with lower resilience.34 What’s more, much literature supports the protective effect of resilience on SI.35 There is a negative association between resilience and SI among adolescents.36 Collectively, resilience may act as a mediator in an individual’s psychological processes. Barahmand and Heydari (2016) also found that resilience partially mediates the relationship between PLEs and psychological distress.34
Furthermore, previous studies have demonstrated that insomnia symptoms may influence resilience. For example, one study of school-age children indicated that irregular bedtimes, shorter sleep durations, and greater sleep disturbances reduced their level of resilience.37 Another prospective study showed that higher sleep rhythmicity, lower fatigue levels and infrequent sleep difficulties predicted higher behavioral control in adolescence, which in turn predicted resilience in young adulthood.38 Although existing evidence draws a clear association between insomnia symptoms and resilience,39 the associations among PLEs, insomnia symptoms, resilience, and SI in adolescents remain unexplored.
Although, a great number of studies have revealed a cross-sectional association between PLEs and SI in adolescents,40 prospective studies are limited. Within such few studies, little is known about the interactive effect of PLEs on SI among adolescents in college campus settings. College students are at the peak age and primary setting for developing PLEs and SI.41 Importantly, much research about the PLEs-SI link did not control for individual’s psychotic diagnoses,42 which inflate the association between PLEs and SI. Accordingly, we conduct a two-wave longitudinal survey to explore the effect of PLEs on SI among college students without psychiatric conditions. Meanwhile, whether the relationship between PLEs and SI can be explained by other symptoms and psychological factors are unclear; therefore, this study attempts to investigate the mediating role of insomnia symptoms and resilience on the PLEs-SI relationship. Finally, In order to fully understand the PLEs-SI association, this study further investigated the role of different types of PLEs (delusional and hallucinatory experiences) with SI. The current study aims to test the following hypotheses:
Hypothesis 1 (H1): PLEs have a positive effect on adolescents SI. Hypothesis 2 (H2): Insomnia symptoms mediate the positive association between PLEs and adolescents’ SI. Hypothesis 3 (H3): Resilience mediates the positive association between PLEs and adolescents’ SI. Hypothesis 4 (H4): Insomnia symptoms and resilience have a chain mediating effect on the effect of PLEs on adolescents’ SI.
Materials and Methods
Participants and Procedure
A convenience sample of college students were recruited from two colleges in Changsha City, Hunan Province, China. The data in the current study were collected and managed using the “Survey Star” system. Prior to the study, the researchers sent a survey invitation letter to the participants via e-mail. Students were asked to register with their contact information and upload an electronic version of the informed consent form if they were willing to participate in the study. They accessed the online survey by scanning the quick response code of the questionnaire with their mobile phone. We keep participants’ personal information and survey results confidential, and the participants were made aware of their right to withdraw freely at any time. The investigation was carried out in accordance with the Helsinki Declaration as revised 1989 and approved by the Ethics Committees of Hunan Normal University.
Data was collected online from the College Mental Health Survey in Hunan Province, China. The Survey is a routine survey conducted each academic year. From April 7 to May 16, 2022, we conducted the baseline survey (Time 1, T1), and 3259 responses to the survey. From November 19 to December 22, 2022 (Time 2, T2), the second wave of the survey was conducted in the same population. 2448 college students participated and 2276 of them were retained from T1. The chi-square test and t-test were used to compare the participants who participated at T2 with those who did not in sample characteristics variables at T1. There was no significant difference in sex (t = 1.79, p = 0.395) and age (t = 1.22, p = 0.201) between these two groups. To control the quality of the survey responses, the inclusion criteria for participation included: (a) age < 24 years [A definition of 10~24 years corresponds more closely to adolescent growth and popular understandings of this life phase (Sawyer et al, 2018)]; (b) time to complete the survey >5 minutes; and (c) have no mental disorders diagnoses that were identified by self-report. We removed 45 responses since they did not meet the inclusion criteria (28 students reported have prior psychotic disorders diagnoses). A total of 2231 college students provided complete data on all measures in two web-based surveys and were included in the final analysis.
Measures
PLEs
PLEs at T1 were measured using the Chinese simplified version of the positive subscale of the Community Assessment of Psychological Experiences (CAPE-P8).43,44 The CAPE-P8 is a self-reported scale based on the CAPE45 that assesses the frequency of PLEs experienced by the participant in the past month. It consists of 8 items, clustering into two dimensions: delusional experiences (DEs: eg, “Do you ever feel as if people seem to drop hints about you or say things with a double meaning?”) and hallucinatory experiences (HEs: eg, “Do you ever hear voices when you are alone?”). Each item is rated on a 4-point Likert scale ranging from 1 (“never”) to 4 (“nearly always”). Higher scores suggest an increased frequency of PLEs. Participants were categorized as having frequent PLEs if they selected “often” or “nearly always” on one or more items.46,47 The internal consistency of the scale was satisfactory in the present study, with a Cronbach’s alpha value of 0.83.
Insomnia Symptoms
Insomnia symptoms at T1 were assessed with the Chinese version of the Youth Self Rating Insomnia Scale (YSIS).48 It consists of eight items that assess the severity of insomnia over the past month. Each item is rated on a 5-point Likert scale ranging from 1 (“Never”) to 5 (“5–7 times /week”), with higher scores showing more severe insomnia symptoms. This scale has been used in previous studies to measure insomnia symptoms in college students.49 In this study, Cronbach’s α was 0.89.
Resilience
The Chinese version of the 10-item Connor-Davidson Resilience Scale (CD-RISC-10) was used to examine adolescents’ resilience status at T1.50 This is a one-dimensional scale (eg, “I am able to adapt to change”, “I can deal with whatever comes”), and each item is rated on a five-point Likert scale ranging from 0 (“not true at all”) to 4 (“true nearly all the time”). Higher scores indicate better resilience. In this study, Cronbach’s α was 0.97.
SI
The Chinese version of the Self-rating Idea of Suicide Scale (SIOSS) was used to assess SI at T1 and T2.51 It consists of 26 items that are divided into four dimensions: helplessness (12 items, eg, “I want to end my life”), pessimism (5 items, eg, “I feel that life is worthwhile”, reverse scoring), sleeping (4 items, eg, “I wake up too early”), and masking (5 items, eg, “Sometimes I also tell lies”). Each item is answered as “Yes” (1 point) or “No” (0 points). The first three subscales (helplessness, pessimism, and sleeping) are summed to obtain a total SI score, with higher scores suggesting a stronger SI. Meanwhile, participants were excluded if they had scores above 4 on the masking subscale. The SIOSS is widely used in the measurement of SI among Chinese adolescents.52 To eliminate tautological overlap with insomnia, we excluded the 4 sleep-related items from SIOSS, and only the hopelessness and pessimism scores were used to indicate the level of SI (17 items). In this study, Cronbach’s α of the 17-item SIOSS was 0.78 and 0.75 at T1 and T2, respectively.
Sample Characteristics
Data on the characteristics of the sample were collected with a questionnaire developed for the study at T1, including sex (female/male), grade (freshman/sophomore/junior/senior), age, ethnicity (Han/others), single-child status (yes/no), parental marital status (good/poor), boarding status (yes/no), parents’ education (primary school or less/junior high school/senior high school), and family income status (<3000 RMB/3000-5000 RMB/>5000 RMB).53
Statistical Analyses
All analyses were conducted using SPSS 23.0. The Harman’s one-factor test through exploratory factor analysis was performed to examine common method variance before regression analysis.54 Pearson’s correlations were conducted to assess the associations between the scores of PLEs, insomnia symptoms, resilience, and SI. The mediation hypotheses were tested using PROCESS models.55 Following Hayes’ suggestions, Model 6 was employed to obtain quantitative evidence of the chain mediation effects: T1 PLEs were entered as the predictor, T1 insomnia symptoms and T1 resilience as the mediators, and T2 SI as the outcome. Given the potential impact of socio-demographics, such as sex,10 age,10 boarding school experience,56 parental education,57 on individual mental health (eg, PLEs and SI), all sample characteristic variables and T1 SI were included as covariates in the analysis.
Results
Common Method Bias Test
Factor analysis of all the measurement indexes (PLEs, insomnia symptoms, resilience, and SI) and the findings of the unrotated factor analysis showed that there were nine factors with eigenvalues greater than 1. The initial eigenvalue of the first factor was 20.739, which did not exceed 40%, indicating that there was no serious common method bias.
Sample Characteristics
The mean age for the 2231 adolescents was 20.02 years (SD = 1.39). Of all the participants, 30.6% (n=682) were male and 69.4% (n = 1549) were female. Other characteristics of the sample are presented in Table 1.
 |
Table 1 Sample Characteristicsa |
Prevalence of PLEs in This Sample
As shown in Table 2, more than one-third (36.3%, N = 809) of participants were reported to have at least one PLE over the past month. Only 3.3% (N = 73) adolescents experienced frequent PLEs in the past month.
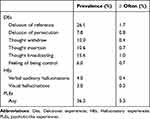 |
Table 2 The Prevalence of Current PLEs Among the Current Sample |
Correlation Analysis
The descriptive statistics and correlation coefficients for the research variables are shown in Table 3. The findings indicated that T2 SI was positively correlated with T1 PLEs (r = 0.332, p < 0.001) and T1 insomnia symptoms (r = 0.309, p < 0.001) and negatively correlated with T1 resilience (r = −0.257, p < 0.001). T1 PLEs tended to be positively associated with T1 insomnia symptoms (r = 0.417, p < 0.001) and negatively correlated with T1 resilience (r = −0.239, p < 0.001).
 |
Table 3 Descriptive Statistics and Correlation Analysis |
Testing Insomnia Symptoms and Resilience as a Chain Mediator
Mediated models of T1 insomnia symptoms and T1 resilience were evaluated after controlling for all sample characteristics (Table 4: Model 1). T1 PLEs had a significant positive effect on T1 insomnia symptoms (β = 0.458, t = 21.312, p < 0.001). T1 PLEs (β = −0.155, t = −6.320, p < 0.001) and T1 insomnia symptoms (β = −0.241, t = −10.934, p < 0.001) significantly negatively predicted T1 resilience. In addition, T1 PLEs (β = 0.236, t = 9.938, p < 0.001) and T1 insomnia symptoms (β = 0.171, t = 7.855 p < 0.001) significantly positively predicted T2 SI, and T1 resilience played a significant negative role in T2 SI (β = −0.151, t = −7.396, p < 0.001).
 |
Table 4 Mediation Model of is Between PLEs and SI |
As shown in Table 5 (Model 1), T1 PLEs was positively correlated with T2 SI (β = 0.354, 95% confidence interval [CI]: 0.311–0.398), supporting H1. In addition, after including T1 insomnia symptoms and T1 resilience, the direct relationship between T1 PLEs and T2 SI remained significant (β = 0.236, 95% CI: 0.190–0.283), which indicated that T1 insomnia symptoms partially mediated the relationship between T1 PLEs and T2 SI (β = 0.078, 95% CI: 0.053–0.108), supporting H2. The results also revealed that T1 resilience partially mediated the positive relationship between T1 PLEs and T2 SI (β = 0.023, 95% CI: 0.012–0.038). This finding supported H3. Meanwhile, insomnia symptoms appeared to play a stronger mediating role in PLEs and SI than resilience. Moreover, when T1 insomnia symptoms and T1 resilience were entered into the model, the bootstrapping analysis found that T1 PLEs had a negative impact on T2 SI through T1 insomnia symptoms and T1 resilience sequentially, and its chain mediating effect was 0.017, with a 95% CI not containing zero [0.010, 0.025]. Therefore, H4 was fully supported (Figure 1).
 |
Table 5 Mediating Effect Analysis of the Chain Mediating Model |
Consistent mediating effects of insomnia symptoms and resilience were also found in the relationship between DEs (Model 2)/ HEs (Model 3) and SI (see Table 4 and Table 5). Our finding indicated that DEs seem to have a stronger effect on SI than HEs (β: 0.203 vs 0.085).
Discussion
This study sought to provide new evidence on the underlying processes and mechanisms of the positive link between PLEs and adolescents’ SI, with a longitudinal study design. We conceptualized and operationalized a chain mediating model that presents the connections among PLEs, SI, insomnia symptoms, and resilience, with the latter two variables as sequential mediators. Empirical evidence supports our hypothesized model, suggesting that PLEs may affect adolescents’ SI by worsening insomnia symptoms and subsequently impairing their resilience. This research adds significantly to the field’s body of knowledge and has valuable implications for educational and clinical practice.
In the current sample, we found that 36.3% college students had at least one PLE, and 3.3% students reported frequent PLEs in the past month. The prevalence rates are much lower than Chinese high school students (49.3% and 15.4%) using consistent criteria.10 Although PLEs are prevalent in childhood and adolescence, they are mostly transient in nature and often disappear with age.11 Our findings confirmed H1, which was that PLEs are positively associated with SI among adolescents, and are in line with the results reported in previous literature of adolescents and young adults documenting that higher PLEs increase the risk of SI.40,58 This relationship may be better explained by other psychopathology symptoms (ie, depressive symptoms) that are commonly comorbid with SI.40 Studies have also reported increased affective reactivity and poorer coping abilities to negative life events in individuals with PLEs as risk factors for SI.59,60
Our observations confirmed H2, which was that the direct link between PLEs and SI is mediated by insomnia symptoms. Previous work has suggested that adolescents with PLEs may have more impairment in quality and duration of sleep, developing more frequent and severe insomnia symptoms.26,61 We also observed an association between insomnia symptoms and SI, which consistent with previous studies. A study by Wu et al with 2379 undergraduate students, indicated that insomnia symptoms were positively associated with SI.62 McCall et al also concluded that improving insomnia symptoms in clinical patients may effectively reduce SI.63 The relationship between insomnia symptoms and SI may be supported by neurobiological evidence. Sleep insufficiency and circadian anomalies affect frontal/executive functions during the daytime and nighttime. Low activation of the frontal lobe may, in turn, reduce problem-solving abilities and increase impulsive behavior, both of which can increase the likelihood of suicidal behaviors.64 Our results also indicated that resilience has a specific mediating effect on the link between PLEs and SI (H3). This observation is in line with the results reported in previous studies documenting that higher resilience reduces the risk of SI.35,36 According to early theories, resilience as a resource can reduce the number of stressors65 and buffer the effects of stressors on psychological outcomes.66 Our finding is also consistent with previous work on young adults documenting that resilience is a mediator in the association between PLEs and psychological distress.34
Our results suggest that insomnia symptoms appear to mediate the association between PLEs and SI more than resilience. Specifically, insomnia symptoms explained greater variance between PLEs and SI. This may be due to the fact that adolescents’ sleep quality is more directly affected by negative life stress, and that most adolescents are able to seek help in time to protect their resilience from serious damage when faced with adverse situations. Another possibility is that insomnia symptoms as risk factors on resilience may also partially explain the effect of PLEs on resilience. Indeed, the current findings also observed a chain effect of insomnia symptoms and resilience that mediates the relationship between PLEs and SI (H4). This result can be explained by the fact that insomnia symptoms in adolescents also affect the development of resilience, a conclusion that has been presented in previous studies.37,38 It has been suggested that insomnia symptoms and resilience affect the brain by similar mechanisms.67 Evidence from neurological studies suggests that insomnia symptoms may cause over-reactivity in a person’s amygdala, which affects the ability to withstand or recover from stressors.68 By leveraging insomnia symptoms and resilience, this study explained the risk role of PLEs in catalyzing adolescent SI. Several implications were highlighted for adolescent with PLEs from an intervention and health‐enhancement perspective. First, early screening for PLEs and insomnia symptoms may be effective in identifying those at risk for SI. Moreover, more work could be done to improve sleep quality and facilitate resilience, such as cognitive behavioral therapy for insomnia (CBT-I)69 and resilience-promoting interventions.70
In addition, this study showed consistent mediating effects of insomnia symptoms and resilience in the relationship between DEs/ HEs and SI. Consistent with previous studies,71 all subtypes of PLEs are positively associated with SI. Studies by Saha et al,72 and participants were drawn from a large-scale cross-sectional survey, indicating that adolescents with delusional experiences were about two to four times as likely to report SI. Hielscher et al also have found that hallucinatory experience and its associated distress increase the risk of SI and suicide attempts in adolescents.73 These findings suggested that both delusional experiences and hallucinatory experience may directly or indirectly predict SI. In this study, delusional experiences seem to have a stronger effect on SI than hallucinatory experience. This result may be attributed to measurement differences, with delusional experiences examining six types of PLE, whereas hallucinatory experiences examining only two items (verbal auditory hallucinations and visual hallucinations). Previous studies have revealed that there may be a significant dose–response relation between the number of PLEs and suicide outcomes.19,74
Finally, there are several limitations of this study that need to be clarified. First, the survey was completed on a web-based platform and data on study variables were collected through self-report measures rather than clinical diagnosis, which may cause reporting bias and potentially threatens the validity of the results. Thus, future studies should use more rigorous methods to ensure data quality in self-report research that is conducted online. Future clinical interviews also should be conducted to determine the severity of PLEs, insomnia symptoms, and SI. Second, this study only measured PLEs, insomnia, and resilience at T1. Although this study involved a longitudinal design, future studies are needed to determine the causal nature among study variables. Third, despite our large sample, all the participants were originally from colleges/universities. It is uncertain whether our findings could be generalised to younger adolescents. Moreover, our study focused only on adolescents’ SI while suicide attempts and behaviors were not considered. Future research could further clarify the relationship between PLEs and comprehensive suicide indexes, and examining the role of more extensive risk factors in this association is also warranted. Additionally, participants with a history of psychiatric diagnosis were excluded from this study, which may have overlooked those who had clinical level of symptoms but did not yet have a definitive diagnosis. Finally, although students have resumed school normally during the investigation, they are still affected by the COVID-19. The pandemic related stress may have increased the risk of PLEs,75 insomnia,76 and SI24 among adolescents and therefore may have also contributed to the current results.
Conclusions
This study suggests that insomnia symptoms and resilience have chain-mediating effects on the association between PLEs and SI in adolescents. This indicates that adolescents who frequently experience PLEs can be considered a high-risk group for SI, which requires early intervention. When intervening, the effects of insomnia symptoms and resilience on adolescents’ SI should be comprehensively considered.
Data Sharing Statement
The data presented in this study are available on request from the corresponding authors (Dr. Dongfang Wang).
Ethics Statement
The investigation was carried out in accordance with the Helsinki Declaration as revised 1989 and approved by the Ethics Committees of Hunan Normal University. Informed consent was obtained from all subjects involved in the study.
Funding
This research was funded by the major project of National Social Science Fund of China (17ZDA326), and the youth project of Social Science Fund of Hunan Province (18YBQ069).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Centers for Disease Control and Prevention. National Center for Health Statistics. Underlying cause of death 1999–2018 on CDC WONDER online database, released in 2020. data are from the multiple cause of death files, 1999–2018, as compiled from data provided by the 57 vital statistics jurisdictions through the vital statistics cooperative program; 2018. Available from: http://wonder.cdc.gov/ucd-icd10.html.
2. Patton GC, Coffey C, Sawyer SM, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009;374(9693):881–892. doi:10.1016/S0140-6736(09)60741-8
3. Zhu X, Tian L, Huebner ES. Trajectories of suicidal ideation from middle childhood to early adolescence: risk and protective factors. J Youth Adolesc. 2019;48(9):1818–1834. doi:10.1007/s10964-019-01087-y
4. Baiden P, Tadeo SK. Investigating the association between bullying victimization and suicidal ideation among adolescents: evidence from the 2017 youth risk behavior survey. Child Abuse Negl. 2020;102:104417. doi:10.1016/j.chiabu.2020.104417
5. McKinnon B, Gariepy G, Sentenac M, Elgar FJ. Adolescent suicidal behaviours in 32 low- and middle-income countries. Bull World Health Organ. 2016;94(5):340–350. doi:10.2471/BLT.15.163295
6. Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol Med. 2011;41(1):1–6. doi:10.1017/S0033291710001005
7. Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43(6):1133–1149. doi:10.1017/S0033291712001626
8. Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. 2012;42(9):1857–1863. doi:10.1017/S0033291711002960
9. Sullivan SA, Kounali D, Cannon M, et al. A population-based cohort study examining the incidence and impact of psychotic experiences from childhood to adulthood, and prediction of psychotic disorder. Am J Psychiatry. 2020;177(4):308–317. doi:10.1176/appi.ajp.2019.19060654
10. Wang D, Chen H, Chen Z, et al. Current psychotic-like experiences among adolescents in China: identifying risk and protective factors. Schizophr Res. 2022;244:111–117. doi:10.1016/j.schres.2022.05.024
11. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness–persistence–impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–195. doi:10.1017/S0033291708003814
12. Dominguez MD, Wichers M, Lieb R, Wittchen HU, van Os J. Evidence that onset of clinical psychosis is an outcome of progressively more persistent subclinical psychotic experiences: an 8-year cohort study. Schizophr Bull. 2011;37(1):84–93. doi:10.1093/schbul/sbp022
13. Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57(11):1053. doi:10.1001/archpsyc.57.11.1053
14. Healy C, Brannigan R, Dooley N, et al. Childhood and adolescent psychotic experiences and risk of mental disorder: a systematic review and meta-analysis. Psychol Med. 2019;49(10):1589–1599. doi:10.1017/S0033291719000485
15. Rimvall MK, van Os J, Verhulst F, et al. Mental health service use and psychopharmacological treatment following psychotic experiences in preadolescence. Am J Psychiatry. 2020;177(4):318–326. doi:10.1176/appi.ajp.2019.19070724
16. DeVylder JE, Jahn DR, Doherty T, et al. Social and psychological contributions to the co-occurrence of sub-threshold psychotic experiences and suicidal behavior. Soc Psychiatry Psychiatr Epidemiol. 2015;50(12):1819–1830. doi:10.1007/s00127-015-1139-6
17. Nishida A, Shimodera S, Sasaki T, et al. Risk for suicidal problems in poor-help-seeking adolescents with psychotic-like experiences: findings from a cross-sectional survey of 16,131 adolescents. Schizophr Res. 2014;159(2–3):257–262. doi:10.1016/j.schres.2014.09.030
18. Yates K, Lång U, Cederlöf M, et al. Association of psychotic experiences with subsequent risk of suicidal ideation, suicide attempts, and suicide deaths: a systematic review and meta-analysis of longitudinal population studies. JAMA Psychiat. 2019;76(2):180–189. doi:10.1001/jamapsychiatry.2018.3514
19. Bromet EJ, Nock MK, Saha S, et al.; World Health Organization World Mental Health Survey Collaborators. Association between psychotic experiences and subsequent suicidal thoughts and behaviors: a cross-national analysis from the World Health Organization world mental health surveys. JAMA Psychiat. 2017;74(11):1136–1144. doi:10.1001/jamapsychiatry.2017.2647
20. Jahn DR, DeVylder JE, Hilimire MR. Explanatory risk factors in the relations between schizotypy and indicators of suicide risk. Psychiatry Res. 2016;238:68–73. doi:10.1016/j.psychres.2016.02.021
21. Yuksel D, Kiss O, Prouty DE, Baker FC, de Zambotti M. Clinical characterization of insomnia in adolescents - an integrated approach to psychopathology. Sleep Med. 2022;93:26–38. doi:10.1016/j.sleep.2022.03.010
22. Wong MM, Brower KJ, Craun EA. Insomnia symptoms and suicidality in the national comorbidity survey - adolescent supplement. J Psychiatr Res. 2016;81:1–8. doi:10.1016/j.jpsychires.2016.06.004
23. Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res. 2011;45(4):505–511. doi:10.1016/j.jpsychires.2010.09.005
24. Wang D, Ross B, Zhou X, et al. Sleep disturbance predicts suicidal ideation during COVID-19 pandemic: a two-wave longitudinal survey. J Psychiatr Res. 2021;143:350–356. doi:10.1016/j.jpsychires.2021.09.038
25. Afonso P, Brissos S, Figueira ML, Paiva T. Schizophrenia patients with predominantly positive symptoms have more disturbed sleep-wake cycles measured by actigraphy. Psychiatry Res. 2011;189(1):62–66. doi:10.1016/j.psychres.2010.12.031
26. Ered A, Cooper S, Ellman LM. Sleep quality, psychological symptoms, and psychotic-like experiences. J Psychiatr Res. 2018;98:95–98. doi:10.1016/j.jpsychires.2017.12.016
27. Wang D, Zhou L, Wang J, Sun M. The bidirectional associations between insomnia and psychotic-like experiences before and during the COVID-19 pandemic. Nat Sci Sleep. 2021;13:2029–2037. doi:10.2147/NSS.S335508
28. American Psychological Association. Building your resilience; 2020. Available from: https://www.apa.org/topics/resilience/.
29. Masten AS, Best KM, Norman G. Resilience and development: contributions from the study of children who overcome adversity. Dev Psychopathol. 1990;2(4):425–444. doi:10.1017/S0954579400005812
30. Kumpfer KL. Factors and Processes Contributing to Resilience. Springer; 2002.
31. Liu WJ, Zhou L, Wang XQ, Yang BX, Wang Y, Jiang JF. Mediating role of resilience in relationship between negative life events and depression among Chinese adolescents. Arch Psychiatr Nurs. 2019;33(6):116–122. doi:10.1016/j.apnu.2019.10.004
32. Tang Y, Ma Y, Zhang J, Wang H. The relationship between negative life events and quality of life in adolescents: mediated by resilience and social support. Front Public Health. 2022;10:980104. doi:10.3389/fpubh.2022.980104
33. Laloyaux J, Collazzoni A, Hirnstein M, Kusztrits I, Laroi F. Personal resilience factors protect against distressing auditory hallucinations: a study comparing psychotic patients with auditory hallucinations, non-patients with auditory hallucinations, and healthy controls. Psychiatry Res. 2020;290:113058. doi:10.1016/j.psychres.2020.113058
34. Barahmand U, Heydari SAR. Psychotic-like experiences and psychological distress: the role of resilience. J Am Psychiatr Nurses Assoc. 2016;22(4):312–319. doi:10.1177/1078390316653802
35. Kim SM, Kim HR, Min KJ, et al. Resilience as a protective factor for suicidal ideation among Korean workers. Psychiatry Investig. 2020;17(2):147–156. doi:10.30773/pi.2019.0072
36. Chang LY, Chang YH, Wu CC, Chang JJ, Yen LL, Chang HY. Resilience buffers the effects of sleep problems on the trajectory of suicidal ideation from adolescence through young adulthood. Soc Sci Med. 2021;279:114020. doi:10.1016/j.socscimed.2021
37. Doi S, Fujiwara T, Ochi M, Isumi A, Kato T. Association of sleep habits with behavior problems and resilience of 6- to 7-year-old children: results from the A-CHILD study. Sleep Med. 2018;45:62–68. doi:10.1016/j.sleep.2017.12.015
38. Wong MM, Puttler LI, Nigg JT, Zucker RA. Sleep and behavioral control in earlier life predicted resilience in young adulthood: a prospective study of children of alcoholics and controls. Addict Behav. 2018;82:65–71. doi:10.1016/j.addbeh.2018.02.006
39. Wang J, Zhang X, Simons SR, Sun J, Shao D, Cao F. Exploring the bi-directional relationship between sleep and resilience in adolescence. Sleep Med. 2020;73:63–69. doi:10.1016/j.sleep.2020.04.018
40. Jang JH, Lee YJ, Cho SJ, Cho IH, Shin NY, Kim SJ. Psychotic-like experiences and their relationship to suicidal ideation in adolescents. Psychiatry Res. 2014;215(3):641–645. doi:10.1016/j.psychres.2013
41. Thompson EC, Jay SY, Andorko ND, et al. Sleep quality moderates the association between psychotic-like experiences and suicidal ideation among help-seeking university students. Psychiatry Res. 2021;296:113668. doi:10.1016/j.psychres.2020
42. Hielscher E, DeVylder JE, Saha S, Connell M, Scott JG. Why are psychotic experiences associated with self-injurious thoughts and behaviours? A systematic review and critical appraisal of potential confounding and mediating factors. Psychol Med. 2018;48(9):1410–1426. doi:10.1017/S0033291717002677
43. Wang D, Sun M, Xi C, et al. Gender and longitudinal measurement invariance of the community assessment of psychic experiences-positive subscale. Chin J Clin Psych. 2020;28(1):41–45. doi:10.16128/j.cnki.1005-3611.2020.01.010
44. Wang D, Sun M, Ouyang X, Fang F. Validity and reliability of the simplified version of community assessment of psychic experiences in college students. Chin Ment Health J. 2022;36(1):172–178. doi:10.3969/j.issn.1000-6729.2022.02.014
45. Stefanis NC, Hanssen M, Smirnis NK, et al. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. 2002;32(2):347–358. doi:10.1017/s0033291701005141
46. Wang D, Ma Z, Zhai S, Sun M, Fan F. Sleep disturbance and psychotic-like experiences among urban adolescents with and without parental migration. Front Public Health. 2022;10:1037963. doi:10.3389/fpubh.2022.1037963
47. Wang D, Ma Z, Scherffius A, et al. Sleep disturbance is predictive of psychotic-like experiences among adolescents: a two-wave longitudinal survey. Sleep Med. 2023;101:296–304. doi:10.1016/j.sleep.2022.11.011
48. Liu X, Yang Y, Liu ZZ, Luo Y, Fan F, Jia CX. Psychometric properties of Youth Self-Rating Insomnia Scale (YSIS) in Chinese adolescents. Sleep Biol Rhyth. 2019;17(3):339–348. doi:10.1007/s41105-019-00222-3
49. Wang D, Chen H, Zhai S, et al. Is returning to school during the COVID-19 pandemic stressful? A study on immediate mental health status of Chinese college students. J Affect Disord. 2021;287:261–267. doi:10.1016/j.jad.2021.03.035
50. Cheng C, Dong D, He J, Zhong X, Yao S. Psychometric properties of the 10-item Connor-Davidson Resilience Scale (CD-RISC-10) in Chinese undergraduates and depressive patients. J Affect Disord. 2020;261:211–220. doi:10.1016/j.jad.2019.10.018
51. Xia CY, Wang DB, He HS, Ye HS. Study of self-rating idea of undergraduates in the mountain area of southern Zhejiang. Chin J Sch Health. 2012;33:144–146.
52. Xie P, Wu K, Zheng Y, et al. Prevalence of childhood trauma and correlations between childhood trauma, suicidal ideation, and social support in patients with depression, bipolar disorder, and schizophrenia in southern China. J Affect Disord. 2018;228:41–48. doi:10.1016/j.jad.2017.11.011
53. Chen C, He Z, Xu B, Shao J, Wang D. A latent profile analysis of sleep disturbance in relation to mental health among college students in China. Front Public Health. 2023;11:1107692. doi:10.3389/fpubh.2023.1107692
54. Johnson RE, Rosen CC, Djurdjevic E. Assessing the impact of common method variance on higher order multidimensional constructs. J Appl Psychol. 2011;96(4):744–761. doi:10.1037/a0021504
55. Hayes A. Introduction to mediation, moderation, and conditional process analysis. J Educ Meas. 2013;51(3):335–337. doi:10.1111/jedm.12050
56. Evans-Campbell T, Walters KL, Pearson CR, Campbell CD. Indian boarding school experience, substance use, and mental health among urban two-spirit American Indian/Alaska natives. Am J Drug Alcohol Abuse. 2012;38(5):421–427. doi:10.3109/00952990.2012.701358
57. Janiri D, Doucet GE, Pompili M, et al. Risk and protective factors for childhood suicidality: a US population-based study. Lancet Psychiat. 2020;7(4):317–326. doi:10.1016/S2215-0366(20)30049-3
58. Capra C, Kavanagh DJ, Hides L, Scott JG. Subtypes of psychotic-like experiences are differentially associated with suicidal ideation, plans and attempts in young adults. Psychiatry Res. 2015;228(3):894–898. doi:10.1016/j.psychres.2015.05.002
59. Lataster T, Wichers M, Jacobs N, et al. Does reactivity to stress cosegregate with subclinical psychosis? A general population twin study. Acta Psychiatr Scand. 2009;119(1):45–53. doi:10.1111/j.1600-0447.2008.01263.x
60. Lin A, Wigman JT, Nelson B, et al. The relationship between coping and subclinical psychotic experiences in adolescents from the general population--a longitudinal study. Psychol Med. 2011;41(12):2535–2546. doi:10.1017/S0033291711000560
61. Andorko ND, Mittal V, Thompson E, et al. The association between sleep dysfunction and psychosis-like experiences among college students. Psychiatry Res. 2017;248:6–12. doi:10.1016/j.psychres.2016.12.009
62. Wu R, Wang CY, Wang F, et al. Association between sleep and suicidal ideation in Chinese undergraduate students. Int J Environ Res Public Health. 2022;19(23):15433. doi:10.3390/ijerph192315433
63. McCall WV, Benca RM, Rosenquist PB, et al. Reducing Suicidal Ideation Through Insomnia Treatment (REST-IT): a randomized clinical trial. Am J Psychiatry. 2019;176(11):957–965. doi:10.1176/appi.ajp.2019.19030267
64. Perlis ML, Grandner MA, Chakravorty S, Bernert RA, Brown GK, Thase ME. Suicide and sleep: is it a bad thing to be awake when reason sleeps? Sleep Med Rev. 2016;29:101–107. doi:10.1016/j.smrv.2015.10.003
65. Baruth KE, Carroll JJ. A formal assessment of resilience: the Baruth protective factors inventory. J Indiv Psych. 2002;58(3):235–244.
66. Werner E. Risk, resilience, and recovery: perspectives from the Kauai longitudinal 600 study. Dev Psychopathol. 1993;5:503–515. doi:10.1017/S095457940000612X
67. Maier SF, Watkins LR. Role of the medial prefrontal cortex in coping and resilience. Brain Res. 2010;1355:52–60. doi:10.1016/j.brainres.2010.08.039
68. Mignot E, Taheri S, Nishino S. Sleeping with the hypothalamus: emerging therapeutic targets for sleep disorders. Nat Neurosci. 2002;5:
69. Alimoradi Z, Jafari E, Broström A, et al. Effects of cognitive behavioral therapy for insomnia (CBT-I) on quality of life: a systematic review and meta-analysis. Sleep Med Rev. 2022;64:101646. doi:10.1016/j.smrv.2022.101646
70. Liu J, Ein N, Gervasio J, Battaion M, Reed M, Vickers K. Comprehensive meta-analysis of resilience interventions. Clin Psychol Rev. 2020;82:101919. doi:10.1016/j.cpr.2020.101919
71. Jay SY, DeVylder J, Schiffman J, et al. Exploring the relation between psychosis-like experiences and suicidal ideation, plans, and attempts among college students in the United States. Early Interv Psychiatry. 2022;17(3):272–280. doi:10.1111/eip.13325
72. Saha S, Scott JG, Johnston AK, et al. The association between delusional-like experiences and suicidal thoughts and behaviour. Schizophr Res. 2011;132(2–3):197–202. doi:10.1016/j.schres.2011.07.012
73. Hielscher E, DeVylder J, Connell M, Hasking P, Martin G, Scott JG. Investigating the role of hallucinatory experiences in the transition from suicidal thoughts to attempts. Acta Psychiatr Scand. 2020;141(3):241–253. doi:10.1111/acps.13128
74. Cederlöf M, Kuja-Halkola R, Larsson H, et al. A longitudinal study of adolescent psychotic experiences and later development of substance use disorder and suicidal behavior. Schizophr Res. 2017;181:13–16. doi:10.1016/j.schres.2016.08.029
75. Wang D, Zhou L, Chen C, Sun M. Psychotic-like experiences during COVID-19 lockdown among adolescents: prevalence, risk and protective factors. Schizophr Res. 2023;252:309–316. doi:10.1016/j.schres.2023.01.027
76. Wang D, Zhao J, Zhai S, et al. Longitudinal trajectories of insomnia symptoms among college students during the COVID-19 lockdown in China. J Psychosom Res. 2022;157:110795. doi:10.1016/j.jpsychores.2022.110795
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

