Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Psychosocial Factors Associated with Suicidal Ideation Among HIV/AIDS Patients on Follow-Up at Dessie Referral Hospital, Northeast Ethiopia: A Cross-Sectional Study
Authors Tamirat KS , Tesema GA , Tessema ZT
Received 6 January 2021
Accepted for publication 23 March 2021
Published 15 April 2021 Volume 2021:13 Pages 415—423
DOI https://doi.org/10.2147/HIV.S299538
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Koku Sisay Tamirat, Getayeneh Antehunegn Tesema, Zemenu Tadesse Tessema
Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Koku Sisay Tamirat
Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, P.O. Box 196, Gondar, Ethiopia
Email [email protected]
Background: Psychosocial and mental health problems are common among HIV/AIDS patients that affect sustained utilization of healthcare services. To date, information is scarce regarding the perceived stigma, level of social support, and suicidal ideation among HIV/AIDS patients in the study setting. Therefore, this study aimed to assess psychosocial factors associated with suicidal ideation among HIV/AIDS patients on follow-up in the study setting.
Methods: A hospital-based cross-sectional study was conducted among people living with HIV/AIDS (PLWH) on antiretroviral therapy follow-up for at least six months at a referral hospital in northeastern Ethiopia from November to January 2019. A total of 395 study participants of antiretroviral therapy clinic visitors were selected systematically. A binary logistic regression model was fitted to identify factors associated with suicidal ideation among PLWH. An adjusted odds ratio (AOR) with 95% confidence interval (CI) and variables having less than or equal 0.05 p-value used to declare statistical significant association.
Results: This study revealed that 45.3%, 56.5%, and 20%, had perceived stigma, poor social support, and depression, respectively. Moreover, the prevalence of suicidal ideation was 9.4% (95% CI: 6.7 to 12.7) of which, 3.3% had attempted to kill themselves. Low body mass index (AOR=4.11, 95% CI: 1.70 9.91), stages three and above illnesses (AOR=6.63, 95% CI: 1.30 33.79), depression (AOR=4.67, 95% CI: 4.67, 95% CI: 1.75 3.93), poor social support (AOR=4.18, 95% CI: 1.46 11.94), and fair and poor adherence (AOR=3.51, 95% CI: 1.14 10.85) were factors associated with suicidal ideation among PLWH.
Conclusion: This study showed that mental disorders and psychosocial problems were common among PLWH. The poor social support, depression, low body mass index, and poor adherence to ART medications were factors associated with suicidal ideation. This finding underscores the importance of regular screening for common mental health disorders and the strengthening of counseling services, nutritional, and psychosocial support programs.
Keywords: suicidal ideation, psychosocial factors, Ethiopia
Introduction
The world has made significant progress in the prevention and control of HIV/AIDS in the last three decades, however, the disease remains a major global public health issue. According to the World Health Organization (WHO) 2019 report, about 38 million peoples living with HIV/AIDS, of which 1.7 million were new cases, and about 690, 000 HIV/AIDS-related deaths occurred.1 The introduction of Highly Active Antiretroviral Therapy (HAART) saved millions of lives and significantly reduced the transmission of the virus in the population. Thus, HAART reduced new HIV infection by 39%, HIV-related death by 51%, and saved 15.3 million lives. However, only 68% of adults living with HIV received lifelong antiretroviral therapy (ART) in 2019 according to the WHO annual report.1,2
More than two-third (25.7 million) of peoples living with HIV/AIDS live in WHO Africa region and the diseases is more prevalent in the general population and number of new infections are increasing among the most vulnerable groups.1 Different interventions were made to realize the 90 90, 90 strategies of 2020 targets like by increasing the number of testing sites, implantation of test and treat strategies, and point of care (POC) approach. Point of care strategies of HIV care treatment is intended to provide accessible and affordable services like viral load, CD4 count measurement, and staging of the disease.3 According to UNAIDS 2020 report, 81% of peoples living with HIV/AIDS know their status, 67% were on ART and 59% had achieved viral suppression.2,4 In Ethiopia, there are about 690, 000 peoples living with HIV/AIDS, with 23, 000 are new infections, and 11,000 people died from an AIDS-related illness.1 Further interventions are needed to achieve the targets set; given that only 79% of peoples living with HIV/AIDS knew their status, of whom 65% were on HAART.4
Mental health and psychosocial problems are common among HIV/AIDS patients that affect sustained utilization of healthcare and adherence to the medications.5 Some of the mental health impairments are mood disorder, elevated depressive symptoms, and suicidal ideations. The trends of mental health problems are increasing worldwide and caused 1 in 5 years lived with disability.6 In addition, there has been a 13% rise in mental health conditions and substance use disorders in the last decade (to 2017).7 Around 20% of the world’s children and adolescents have a mental health condition, with suicide the second leading cause of death among 15–29-year.7 Approximately one in five people in post-conflict settings have a mental health condition. About 79% of global suicides occur in low- and middle-income countries and close to 800, 000 people die due to suicide every year.8,9 Many mental health conditions can be effectively treated at a relatively low cost, yet the gap between people needing care and those with access to care remains substantial. Effective treatment coverage remains extremely low. According to a study in low-income countries about 36.6%, 22.5%, 43.9% of HIV/AIDS patients had depression, suicidal ideation, and faced perceived stigma, respectively.10–12 Moreover, advanced disease conditions, prior mental disorder, substance use and treatment failure, and intractable social support are determinants of depression and suicidal ideation among HIV/AIDS patients.10,12–16 The integration of HIV care and treatment with counseling and psychosocial support programs are helpful for the reduction of mental disorder and psychosocial concerns among PLWH. Besides, the involvement of HIV/AIDS patients in income-generating activities showed a promising effect on the improvement of social networks and alleviating financial hardships.17 To date there is a scarcity of information regarding the perceived stigma, level of social support, and suicidal ideation in the study setting.
Therefore, this study aimed at the psychosocial factors associated with suicidal ideation among HIV/AIDS patients on follow-up in the study setting. The findings of this study could help for the evaluation of psychosocial supports at HIV/AIDS programs. In addition, the results of this study could help to integrate mental health services with HIV/AIDS treatment programs.
Methods
Study Design, Setting, and Period
An institution-based cross-sectional study was undertaken at Dessie referral hospital from November to January 2019. The hospital is the largest hospital serving millions of people in the region of Amhara and neighboring Afar, situated 401 kilometers away from Addis Ababa, the capital of Ethiopia. In addition to general care, the hospital has also offered more than 6, 763 HIV/AIDS (6279 adults and 484 pediatric) patients with antiretroviral therapy since the launch of the program.
Study Participants and Sampling Procedures
The study population consisted of adult HIV/AIDS patients who had been followed up on for at least six months. Patients aged 18 and up who had been on ART for at least 6 months and were available at the ART clinic during the data collection period were also eligible. The sample size was estimated using the single proportion formula with the assumptions of prevalence (P) suicidal ideation among HIV-positive adults (33.6%) obtained from a study conducted in Ethiopia, 95% confidence level, a margin of error of 5%, and a 10% non-response rate, resulting in a sample size of 378.10 Finally, 395 HIV/AIDS patients on follow-up were chosen from ART clinic visitors using a systematic random sampling technique.
Data Collection Procedure
After reviewing various literature, questionnaires were prepared in English, then translated into the local Amharic language, and then translated back to ensure its consistency. There are socio-demographic, clinical, psychosocial, and mental health elements of the questionnaire. Two data collectors and one supervisor were hired before the initial data collection, and they received one-day training on the target and how to interview participants and collect data from medical records.
The nine-item structured Patient Health Questionnaire (PHQ-9) and the suicide manual of the Composite International Diagnostic Interview were used to collect data on depression and suicidal ideation and attempt (CIDI). In addition, using the Oslo Social Support Scale (OSS) and HIV-stigma scale, the level of social support and perceived stigma was measured. Suicidal ideation was the response variable, while socio-demographic (age, sex, education level), clinical (ART routine, recent CD4 count, opportunistic infection, WHO stage, and adherence to ART medication) and psychosocial (depression, social support, and level of stigma) variables were independent variables.
Operational Definition
Depression: Participants who were interviewed and scored five and above using patient health questioner 9 (PHQ-9) were considered depressed.18
Good adherence: If the average adherence level (95% or more adherence = missing ≤ 2 doses of 30 doses or ≤3 doses of 60 doses).19
Fair adherence: (85–94% or 4–8 doses missed per month).19
Poor adherence: (less than 85% or ≥9 doses missed per month).
Perceived stigma: Participants who scored above the median score ≥ 24 were perceived stigma and those who scored below the median score (<24) were not perceived stigma measured by using the HIV stigma scale.20
Social support: The OSS-3 scores ranged from 3–14 with a score of 3–8 = poor support; 9–11 = moderate support; and 12–14 = strong support.21
Body Mass Index: based on Nutritional assessment classification underweight <18.5 kg/m2, Normal=18.5–24.9 kg/m2, over weight ≥25kg/m2.22
Data Processing and Analysis
Initially, the completed questionnaire was reviewed manually for completeness and coding, entered in EpiData version 3.1, and exported to STATA version 14 for further data management and analysis. Frequencies and percentages of socio-demographic, clinical, and psychosocial features are computed and displayed in charts, graphs, and texts. The binary logistic regression analysis was developed to classify factors associated with suicidal ideation. Crude and adjusted odds ratio of 95% CI estimated to see the presence and severity of the correlation between independent variables and depression.
In the multivariable logistic model, variables with a p-value of 0.05 or less were considered significantly correlated with suicidal ideation. Using the Hosmer and Lemeshow goodness of fit test, the model adequacy was tested and revealed that the p-value of 0.222 is insignificant suggested that the model matches the data better. Moreover, after running the null and full models, the area under the curve (AUC) was compared, and the full model had the highest AUC value of 0.8534, suggesting that it better explained the data over the null model (Figure 1).
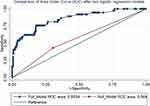 |
Figure 1 Receiver Operative Curve (ROC) of model comparison after logistic regression model. |
Result
Socio-Demographic and Behavioral Characteristics
A total of 395 patients were included in the final analysis of the study. The median age was 38 years with an Interquartile range (IQR) of 10 years, about 47.1% % of them aged between 35–44 years. Two hundred forty-two (61.3%) patients were females, 44.6% were single, and the majority (90.4%) of them were urban dwellers. Regarding behavioral characteristics, about 94.7% disclosed their HIV Status, 30.9% ever consumed alcohol, 3% smoked a cigarette, and 10.1% chewed Khat. About 45.6% of respondent’s partners were HIV positive, of which 96.1% of them were on ART (Table 1).
 |
Table 1 Socio-Demographic and Behavioral Characteristics HIV/AIDS Patients in Ethiopia |
Clinical Conditions of the Participants
The duration of illnesses for the majority (93.9%) of patients were above 12 months, 83.5% had stage one diseases, about 88.4% of patients were on first-line antiretroviral therapy (ART) of which, and 92.2% of patients took ART for more than 12 months and more than two-thirds of patients were on Efavirenz (EFV) based regimen. Meanwhile, 5.8% had chronic illnesses, of which Diabetes mellitus and Hypertension were common comorbid conditions, 7.8% had opportunistic infections in the past six months, and 13.9% had Anemia (Hg<12gm/dl). The majority (81.3%) had a recent CD4 count above 200 cells/mm3, and 70.6% of undetected viral load on recent follow-up measurements (Table 2).
 |
Table 2 Clinical Characteristics of HIV/AIDS Patients in Ethiopia (N=395) |
Perceived Stigma, Social Support, and Suicidal Ideation
Of the overall participants, 45.3%, 56.5%, and 20% were viewed as a stigma, low social support, and depression. Whilst, the prevalence of suicidal ideation was between 9.4% (95% CI: 6.7 to 12.7) and 3.3% attempted suicide. More specifically, the prevalence of suicidal ideation among depressed, stigma-ridden, and inadequate social support was 29.1%, 10.6%, and 12.6%, respectively (Figure 1). Of those who wanted to kill themselves, chemical substances such as Berekina, Merz, and hanged were widely used materials (Figure 2).
 |
Figure 2 A graph showing common psychosocial problems of HIV/AIDS patients in Ethiopia. |
Factors Associated with Suicidal Ideation
In those patients who had poor social support, the odds of suicidal thought was 3.64 times higher compared to those who had moderate and strong social support (AOR=4.18, 95% CI: 1.46 11.94). Similarly, those patients who had a low body mass index (BMI<18.5 kg/m2) associated with 4.46 times higher than those who had normal BMI (AOR=4.11, 95% CI: 1.70 9.91). Moreover, in patients who had depression, the odds of suicidal ideation were 4.28 times than higher those who had not depression (AOR=4.67, 95% CI: 1.75 12.39). For those patients who had poor adherence the odds of suicidal ideation was 4.11 times than those who had good adherence to ART medications (AOR=3.51, 95% CI: 1.14 10.85). Those patients on the first-line ART regimen had 4.69 times higher odds of suicidal ideation than those on the second-line regimen (AOR=4.69, 95% CI: 1.05 2085). Patients who had the second stage of diseases were associated with 6.13 times higher odds of suicidal ideation than those asymptomatic individuals (AOR=6.13, 95% CI: 1.30 33.79) (Table 3).
 |
Table 3 Binary Logistic Regression Analysis to Identify Factors Associated with Suicidal Ideation Among PLWH |
Discussion
This research found that common mental illnesses were more common, with around 56.5%, 45.3%, 20%, 9.4%, and 3.3% having inadequate social support, perceived stigma, depression, suicidal thoughts, and attempts, respectively. Common mental health issues such as depression, suicidal ideation, stigma, and discrimination are major health problems among HIV/AIDS patients. Especially stigma and poor social support for HIV/AIDS patients, which can impede care and good clinical prediction. The completion of this research was consistent with studies in Ethiopia and Nigeria.10,23
In addition, this research also found that poor social support, low BMI, depression, disease stage, ART regimen, and poor adherence to ART drugs were variables associated with suicidal ideation. In contrast to other Ethiopian studies, the magnitude of suicidal ideation in this sample was relatively poor. This may be because the research participants took ART for at least six months, resulting in clinical recovery and emotional relaxation for the majority of the patients.
Thus, those patients who had insufficient social support were associated with increased self-murder thoughts. This result was in line with results from Ethiopian studies.10,11,24 This may be because social support plays a critical role in the psychosocial adaptation to the living conditions of patients. In addition, social support is the social health determinant (SDH) that affects the quality of life of the patient and the use of health care networks.
Depression was similarly associated with higher suicidal ideation odds. This result was consistent with prior results from the report.11 This may be because extreme depressive symptoms are related to suicidal risk and thoughts. Depression affects everyday activities, social interactions, and low self-esteem can cause increased suicidal thoughts. Similarly, relative to asymptomatic people, patients with stage two HIV/AIDS following treatment had a higher risk of suicidal ideation. This result was in line with previous research.11,12,16 This may be because the progression of the disease leads to a compromised quality of life of a patient who has progressed. This research also showed that patients on a first-line ART regimen were associated with increased suicidal ideation odds. This result was in line with previous results from the report. The Efavirenz-containing first-line antiretroviral therapy (ART) has been linked to an increased risk of psychiatric complications.25 This research also found that higher chances of suicidal thoughts were correlated with the low body mass index of HV/AIDS patients. This may be attributable to the fact that unexplained weight loss is a symptom of advanced disease that affects patients’ physical, mental, and psychological well-being. This result was in line with the results of a systematic review and meta-analysis.26
Poor adherence to ART drugs has been related to a rise in suicidal thoughts. This result was in line with previous research findings. This may be due to inadequate adherence to ART drugs, which leads to rapid disease development and treatment failures. Furthermore, psychiatric conditions such as depression, suicidal ideation, and attempts can affect their medication adherence.
This study indicates that mental health concerns have been prevalent in patients with HIV/AIDS that can impact the quality of life and clinical results of the patient. In addition, frequent screening and therapy for mental wellbeing and strengthening psychosocial care for HIV/AIDS patients is of vital importance.
Strength and Limitation of the Study
This research has the power to evaluate common psychosocial and mental illnesses in patients with HIV/AIDS. This research could help improve mental and psychosocial support interventions and be used as an entry point for further screening of mental health status. However, due to the cross-sectional study design and the fact that study participants are clinically healthy, the frequency of suicidal ideation could be underestimated.
Conclusion
This study showed that among HIV/AIDS patients, psychiatric illnesses and psychosocial issues were widespread. Suicide ideation was related to a lack of social support, depression, a low BMI, and a lack of adherence to ART medications. This result highlights the importance of frequent screening for common mental illnesses as well as the improvement of therapy, nutritional, and psychosocial support services.
Data Sharing Statement
The datasets used during the current study are available from the corresponding author up on request.
Ethical Consideration
Ethical acceptance letter to conduct this study obtained from the University of Gondar College of medicine and health sciences ethical review committee before the actual data collection process. For this study verbal informed consent was approved by the ethical review committee, and that this study was conducted in accordance with the Declaration of Helsinki. An additional official permission letter was also obtained from the chief clinical director of the hospital. Verbal informed consent was taken from after briefing about the objective of the study each of the study participants. Moreover, all the study participants were assured to leave the study at any time of the study. Moreover, filled questionnaires keep in locked cabinets for the attainment of confidentiality of patients’ information. Patients who had depression, suicidal ideation, and attempts during data collection time were linked to the psychiatry clinic for further treatment and follow-ups.
Consent for Publication
Not applicable as there is no image or other confidentiality-related issues.
Acknowledgment
We would like to acknowledge data collectors, hospital administrators, and Microbiology department staff for their support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
We didn’t receive external funds for this research.
Disclosure
The authors declared that they have no competing interests.
References
1. UNAIDS LP. Global AIDS response progress country report. Available from: https://www.unaids.org/sites/default/files/country/documents/LAO_narrative_report_2016.pdf.
2. Bain LE, Nkoke C, Noubiap JJN. UNAIDS 90–90–90 targets to end the AIDS epidemic by 2020 are not realistic: comment on “Can the UNAIDS 90–90–90 target be achieved? A systematic analysis of national HIV treatment cascades”. BMJ Global Health. 2017;2:2. doi:10.1136/bmjgh-2016-000227
3. Drain PK, Dorward J, Bender A, et al. Point-of-care HIV viral load testing: an essential tool for a sustainable global HIV/AIDS response. Clin Microbiol Rev. 2019;32(3). doi:10.1128/CMR.00097-18
4. Gesesew HA, Ward P, Woldemichael K, Mwanri L. HIV Care continuum Outcomes: can Ethiopia Meet the UNAIDS 90- 90-90Targets? Ethiop J Health Sci. 2020;30(2):179. doi:10.4314/ejhs.v30i2.5
5. Remien RH, Stirratt MJ, Nguyen N, Robbins RN, Pala AN, Mellins CA. Mental health and HIV/AIDS: the need for an integrated response. AIDS. 2019;33(9):1411. doi:10.1097/QAD.0000000000002227
6. Campisi SC, Carducci B, Akseer N, Zasowski C, Szatmari P, Bhutta ZA. Suicidal behaviours among adolescents from 90 countries: a pooled analysis of the global school-based student health survey. BMC Public Health. 2020;20(1):1–11. doi:10.1186/s12889-020-09209-z
7. Kessler RC, Üstün TB. The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):93–121. doi:10.1002/mpr.168
8. Abas M, Ali GC, Nakimuli‐Mpungu E, Chibanda D. Depression in people living with HIV in sub‐Saharan Africa: time to act. Trop Med Int Health. 2014;19(12):1392–1396. doi:10.1111/tmi.12382
9. World Health Organization. Global Burden of Mental Disorders and the Need for a Comprehensive, Coordinated Response from Health and Social Sectors at the Country Level. World Health Organization; 2012.
10. Bitew H, Andargie G, Tadesse A, Belete A, Fekadu W, Mekonen T. Suicidal ideation, attempt, and determining factors among HIV/AIDS patients, Ethiopia. Depress Res Treat. 2016;2016:1–6. doi:10.1155/2016/8913160
11. Gebremariam EH, Reta MM, Nasir Z, Amdie FZ. Prevalence and associated factors of suicidal ideation and attempt among people living with HIV/AIDS at Zewditu Memorial Hospital, Addis Ababa, Ethiopia: a cross-sectional study. Psychiatry j. 2017;2017:1–8. doi:10.1155/2017/2301524
12. Duko B, Geja E, Zewude M, Mekonen S. Prevalence and associated factors of depression among patients with HIV/AIDS in Hawassa, Ethiopia, cross-sectional study. Ann Gen Psychiatry. 2018;17(1):45. doi:10.1186/s12991-018-0215-1
13. Amare T, Getinet W, Shumet S, Asrat B. Prevalence and associated factors of depression among PLHIV in Ethiopia: systematic review and meta-analysis, 2017. AIDS Res Treat. 2018;2018:1–9. doi:10.1155/2018/5462959
14. Anlay DZ. Strong Association between Stigma and Depression among Adults People Living with HIV/AIDS in Ethiopia: a systematic review and Meta-analysis.
15. Casale M, Boyes M, Pantelic M, Toska E, Cluver L. Suicidal thoughts and behaviour among South African adolescents living with HIV: can social support buffer the impact of stigma? J Affect Disord. 2019;245:82–90. doi:10.1016/j.jad.2018.10.102
16. Wang W, Xiao C, Yao X, Yang Y, Yan H, Li S. Psychosocial health and suicidal ideation among people living with HIV/AIDS: a cross-sectional study in Nanjing, China. PLoS One. 2018;13(2):e0192940. doi:10.1371/journal.pone.0192940
17. Kabore I, Bloem J, Etheredge G, et al. The effect of community-based support services on clinical efficacy and health-related quality of life in HIV/AIDS patients in resource-limited settings in sub-Saharan Africa. AIDS Patient Care STDS. 2010;24(9):581–594. doi:10.1089/apc.2009.0307
18. Chibanda D, Verhey R, Gibson LJ, et al. Validation of screening tools for depression and anxiety disorders in a primary care population with high HIV prevalence in Zimbabwe. J Affect Disord. 2016;198:50–55. doi:10.1016/j.jad.2016.03.006
19. Tiyou A, Belachew T, Alemseged F, Biadgilign S. Predictors of adherence to antiretroviral therapy among people living with HIV/AIDS in resource-limited setting of southwest ethiopia. AIDS Res Ther. 2010;7(1):39. doi:10.1186/1742-6405-7-39
20. Melis T, Fikadu Y, Lemma L. Perceived Stigma and Associated Factors Among HIV Positive Adult Patients Attending Antiretroviral Therapy Clinics at Public Facilities of Butajira Town, Southern Ethiopia, 2020. HIV/AIDS. 2020;12:717.
21. Kocalevent R-D, Berg L, Beutel ME, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychology. 2018;6(1):31. doi:10.1186/s40359-018-0249-9
22. Jumare J, El-Kamary SS, Magder L, et al. Body Mass Index and Cognitive Function among HIV-1 Infected Individuals in China, India and Nigeria. J Acquir Immune Defic Syndr. 2019;80(2):e30. doi:10.1097/QAI.0000000000001906
23. Egbe CO, Dakum PS, Ekong E, Kohrt BA, Minto JG, Ticao CJ. Depression, suicidality, and alcohol use disorder among people living with HIV/AIDS in Nigeria. BMC Public Health. 2017;17(1):542. doi:10.1186/s12889-017-4467-5
24. Kindaya GG, Demoze CK. Lifetime prevalence and determinants of suicidal ideation and attempt among all patients living with HIV/AIDS in Hiwot Fana Specialized Hospital, Harar, Ethiopia, 2020. HIV/AIDS. 2020;12:331.
25. Jones DL, Rodriguez VJ, Alcaide ML, Weiss SM, Peltzer K. The use of efavirenz during pregnancy is associated with suicidal ideation in postpartum women in rural South Africa. AIDS Behav. 2019;23(1):126–131. doi:10.1007/s10461-018-2213-3
26. Perera S, Eisen RB, Dennis BB, et al. Body mass index is an important predictor for suicide: results from a systematic review and Meta‐Analysis. Suicide Life Threatening Behav. 2016;46(6):697–736. doi:10.1111/sltb.12244
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
