Back to Journals » Psychology Research and Behavior Management » Volume 15
Psychopathological Symptoms Among Chronically Ill Patients During SARS-CoV-2 Pandemic in Poland
Authors Pawłowski M, Fila-Witecka K , Rymaszewska JE, Kamińska D, Poznański P , Augustyniak-Bartosik H, Zielińska D, Krajewska M, Krajewski PK , Stefaniak A, Szepietowski JC , Pokryszko-Dragan A, Chojdak-Łukasiewicz J, Budrewicz S, Pawłowski T , Szcześniak D, Rymaszewska J
Received 19 February 2022
Accepted for publication 19 June 2022
Published 16 September 2022 Volume 2022:15 Pages 2659—2669
DOI https://doi.org/10.2147/PRBM.S362918
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Marcin Pawłowski,1 Karolina Fila-Witecka,1 Julia Ewa Rymaszewska,1 Dorota Kamińska,2 Paweł Poznański,2 Hanna Augustyniak-Bartosik,2 Dorota Zielińska,2 Magdalena Krajewska,2 Piotr K Krajewski,3 Aleksandra Stefaniak,3 Jacek C Szepietowski,3 Anna Pokryszko-Dragan,4 Justyna Chojdak-Łukasiewicz,4 Sławomir Budrewicz,4 Tomasz Pawłowski,1 Dorota Szcześniak,1 Joanna Rymaszewska1
1Psychiatry Department, Wroclaw Medical University, Wroclaw, Poland; 2Nephrology and Transplantology Department, Wroclaw Medical University, Wroclaw, Poland; 3Department of Dermatology, Venereology and Allergology, Wroclaw Medical University, Wroclaw, Poland; 4Department of Neurology, Wroclaw Medical University, Wroclaw, Poland
Correspondence: Marcin Pawłowski, Email [email protected]
Introduction: The global severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic had a drastic psychological and economic impact on the global population. Having a chronic disease during the pandemic is associated with numerous limitations and challenges like regular hospital visits, access to health-care units and getting specialized treatment. In addition, chronically ill patients are at great risk of acquiring the SARS-CoV-2 virus and at experiencing a more severe course of illness, due to comorbid conditions as well as more frequent encounters with health-care workers and other patients in medical facilities. The aim of this study was to examine the psychological disturbances, during the pandemic in chronically ill patients.
Methods: During the cross-sectional survey conducted between May and October 2020, 398 patients with four different chronic conditions (psoriasis, multiple sclerosis and patients who have undergone a kidney transplant or received dialysis). Study sample was examined regarding the occurrence of psychopathological symptoms (General Health Questionnaire 28) and their perceived stress levels (Perceived Stress Scale).
Results: The highest scores were found in the MS group and the lowest scores were found in the kidney transplantation group in every subscale of the GHQ-28. Close to half of the studied population (48.74%, n = 193) patients scored above the cut-off for psychopathology.
Conclusion: As the study was conducted during the SARS-CoV-2 pandemic in Poland, it stands to reason that the pandemic affected the psychological wellbeing of chronically ill patients. A COVID-19 infection, being quarantined and having had contact with a person who was infected, did not significantly affect the outcome measures; however, further research is needed to explore this topic.
Keywords: pandemic, SARS-CoV 2, chronic kidney disease, psychopathology, multiple sclerosis, psoriasis
Introduction
The global severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic constituted a vast and unexpected change in everybody’s lives. This sudden shift occurred in December 2019 in Wuhan, China, and continues to contribute to rapidly changing circumstances and uncertainty until this day. Since the beginning of the pandemic there have been drastic psychological and economic impacts on the global population.1 According to previous research not only infection risk, but also the self-isolation and quarantines that followed, contributed to an increased risk of depression and anxiety.2 The emergence of SARS-CoV-2 has also exceedingly impacted health-care systems around the world, with patients and health-care professionals alike having been subjected to a novel stressor affecting their everyday life and functioning. COVID-19, the disease caused by SARS-CoV-2, can manifest across a variety of systems, including respiratory, cardiovascular, gastrointestinal, hematological, kidney, skin, liver and endocrine symptoms. COVID-19 has also been found to affect the central nervous system,3 and the mechanisms behind neurological symptoms in COVID-19 have been described in two ways. The first addresses the effect of a systemic infection with vascular and infection-related secondary inflammatory tissue damage. The second explanation points to a direct neuroinvasion as a result of the infection.4,5
Patients with multiple comorbid conditions are principally vulnerable to developing a more severe COVID-19 infection course.6 The CDC reports that conditions like cancer, cerebrovascular diseases, diabetes, chronic obstructive pulmonary diseases, heart diseases and obesity are risk factors for a severe course of COVID-19.7,8 Having a chronic disease is associated with numerous limitations and challenges, including regular hospital visits, access to health-care units and receiving specialized treatment. These factors have been further exacerbated by infection threat and limited and restricted access during the pandemic. The implementation of preventive strategies is especially important in dialysis patients, who are at great risk of contracting the SARS-CoV-2 virus and experiencing a more severe course of illness, due to the increased interactions with medical workers and other patients in dialysis facilities. Furthermore, their illness is frequently associated with comorbidities like diabetes, hypertension or cardio-vascular diseases.9 Another group of patients who were exceptionally affected by the pandemic were kidney transplant patients, who frequently experienced delays and postponements of planned surgeries, even with negative SARS-CoV-2 tests, due to a risk of false-negative results.10 According to the research by Li et al, patients on dialysis (often suffering with multiple comorbid conditions) have an increased COVID-19 infection mortality rate compared to non-dialysis individuals. The mortality rate in the kidney transplant patients reaches up to 24.05% and 27.7% among hemodialysis population.11–13 Another group of patients exposed to the pandemics impact on mental health are multiple sclerosis (MS) patients, whose medication regimens require immunosuppressive or immunomodulating therapy, putting them at a higher risk of acquiring respiratory tract diseases and related complications.14 Highlighting the importance of the fact, that MS patients are exceptionally vulnerable to neuropsychiatric impacts of the SARS-CoV-2 pandemic is necessary, because these patients often already suffer from cognitive impairment, anxiety and depression.15
The impact of the pandemic can also be noted in other immunological diseases, such as psoriasis. Typically, a continuation of immunomodulating therapies is recommended for psoriasis patients, however those infected with the SARS-CoV-2 virus are advised to discontinue the treatment. Among patients with psoriasis and multiple comorbidities a switch to other, safer modalities such as retinoids or an at-home phototherapy has been reported.16 The fear of not being able to receive proper psoriasis treatment during the pandemic can negatively affect the mental state of already psychologically burdened patients. While health-care systems worldwide focus on taking care of COVID-19 infected patients, the amount of chronically ill patients has not decreased. COVID-19 patients are prioritized and planned procedures and treatments are continuously postponed.
During the first wave of the SARS-CoV-2 pandemic in Poland, visiting clinics and hospital emergency rooms was discouraged. The Polish government advised the population to avoid high-risk places due to an increased risk of infection. These recommendations, however necessary, may pose a risk of neglecting chronic illnesses.14,17 Of particular note is that only 6.3% of the Gross Domestic Product (GDP) in Poland was spent on healthcare in 2018,18 in comparison to France, who allocated almost twice this percentage to healthcare in the same year.19 This leaves the local health-care systems underpaid and poorly financed in face of the mounting additional burden created by the pandemic.
The aim of this cross-sectional observational study was to evaluate the psychopathological symptoms among four groups of chronically ill patients who are especially susceptible to SARS-CoV-2 infections, namely: psoriasis, multiple sclerosis and patients who have undergone a kidney transplant or received dialysis during the SARS -CoV-2 pandemic. Living with a chronic condition predisposes to mental disorders as does the SARS-CoV-2 pandemic.20–23 We hypothesized that chronically ill patients would be highly susceptible to the stress caused by the changing circumstances and restrictions as well as the global uncertainty that came with the pandemic, due to their unique circumstances of living with a chronic condition. A secondary aim of this study is to highlight the need for additional support and tailored, informed psychological interventions in the population of patients with chronic health conditions during the pandemic.
Materials and Methods
Study Design and Settings
During the cross-sectional survey conducted between May and October 2020, patients with four different chronic conditions (psoriasis, multiple sclerosis and patients who have undergone a kidney transplant or received dialysis) were examined regarding the occurrence of psychopathological symptoms and their perceived stress levels. Demographic variables, as well as data related to having been quarantined, infected with the SARS-CoV-2 virus, or having relatives who were infected with the virus were also included in the survey. The survey was conducted using both online and print formats, due to the imposed restrictions on direct contact as well as patient safety. The online questionnaire was based on Computer-Assisted Web Interviewing (CAWI) and distributed among patients via websites and social media profiles of Polish Psoriasis and MS Societies. The printed version of the questionnaire was distributed among patients of the University Hospital in Wroclaw, Poland. Psoriasis and multiple sclerosis patients were examined using online and paper questionnaires. Patients in the dialysis and kidney transplantation groups were exclusively taking part in the pen-and-paper version of the questionnaire. The data collected via online questionnaires was downloaded in excel format and the pen-and-paper version was transferred to the same format manually.
Participants
A total of 398 respondents, recruited among patients of the University Hospital in Wroclaw (Poland) as well as psoriasis and MS societies members were included in the study. The respondents were invited to participate in a survey that was distributed through social media as well as directly to the patients in the hospitals. The inclusion criteria were: a diagnosis of psoriasis (P), multiple sclerosis (MS), currently receiving dialysis treatments (D) and having received a kidney transplant in the past (KT), age over 18 years. No formal confirmation of the diagnosis has been required for either of the groups. In the KT and D groups, however, patients were recruited by medical personnel on the base of hospital databases which ensured the reliability of medical data. Due to the recruitment process (partially online) some of the diagnoses in the P and MS groups could not be verified by requesting medical documents for data protection reasons, the reliability of the medical data relies on the distribution channels (hospital network and member-only online societies). The exclusion criteria were limited to patients who were of age and able to give informed consent. Incomplete datasets were also excluded from the analysis. The final number of participants was: P group n = 95, MS group; n = 128, KT group n = 102 and D group n = 73. The gender ratio in the groups presented as follows: 238 (60%) female and 160 (40%) male. The mean age of the participants was 45.75. Information on a history of psychiatric treatment was taken but did not constitute an excluding factor. The study was approved by the local Bioethical Committee at the Wroclaw Medical University (KB-468/2020; KB-469/2020; KB-470/2020; KB-417/2020). Participation in the survey was voluntary and without any financial compensation. Anonymity of the responses was maintained throughout the collection and storage of data. An informed consent form to participate in the study and allow the processing of data for research purposes was provided in the initial part of the questionnaire. Confirmation of informed consent on the online version was necessary to proceed with responding and submitting the questionnaire. On the printed version, informed consent was confirmed by signing the form and by the completion of the questionnaire. This research was funded by Wroclaw Medical University, grant number SUBZ.C230.22.062; SUBZ.C160.22.051; SUBZ.C260.22.056.
Measurements and Outcomes Measures
The psychometric tool selection in the study was based on relevant literature by a team of specialists from different fields (psychiatry, psychology, neurology, dermatology and nephrology). The following questionnaires were included in the survey:
- Sociodemographic information and COVID-19 exposure data section.
- The General Health Questionnaire (GHQ-28; Makowska, Z.; Merecz, D. Polish adaptation of David Goldberg’s general health questionnaire: GHQ-28)24 is a self-administered screening tool designed to detect and measure the presence of psychopathological symptoms. It consists of 28 items. The questionnaire was validated in the Polish population and deemed satisfactory with validity scores (Cronbach’s alpha) around 0.8. On the basis of previous literature, the cut-off score was established at 24 points.24,25
- The Perceived Stress Scale 10 (PSS-10; Cohen et al, 1983; Polish adaptation: Juczyński & Ogińska-Bulik, 2009) assess the level of experienced stress. It contains 10 questions designed to measure the subjective level of stress. The general result reflects the intensity of perceived stress. Participants indicate their answers on a 5-point scale ranging from 0 (never) to 4 (very often). The PSS-10 score is calculated by summing up the item scores. The questionnaire was validated in the Polish population and deemed satisfactory with validity scores (Cronbach’s alpha) around 0.8.26,27
A detailed description of the study design can be found in Figure 1.
 |
Figure 1 Flow diagram of study design. |
Statistical Analysis
The statistical analysis of the obtained results was performed with the use of IBM SPSS Statistics v. 26 (SPSS INC., Chicago, USA) software. All data were assessed for parametric or non-parametric distribution. The minimum, maximum, mean and standard deviation were calculated. Analyzed quantitative variables were evaluated using the Mann–Whitney U-test and Spearman and Pearson correlations, while for qualitative data the Chi-squared test was used. Differences between several groups were assessed by Kruskal–Wallis 1-way analysis of variance on ranks. A 2-sided P value ≤0.05 was considered to be statistically significant. All of the analyzed datasets were complete and no missing data was encountered.
Results
Participants
The study participants were divided into four groups based on their medical condition, as described in the participants section. The study groups had dissimilar sociodemographic profiles in terms of sex, age, marital status, average amount of children, psychiatric treatment, psychotherapy and duration of illness. There were no significant differences between groups in COVID-19 status and infection or quarantine of a close one. The average age of the participants was 45.75 years (SD: 17.05). 52% of participants were married and 18% were single. 28% of the study participants had received psychological intervention and 18% psychiatric treatment in the past. 6% of respondents reported having someone close who had been infected with the SARS COV-2 virus or quarantined, 2% admitted to having a COVID-19 infection at the time of data collection, 5% were quarantined and 2% had contact with a person infected with SARS-CoV-2. Detailed demographic data are presented in Table 1.
 |
Table 1 Detailed Sociodemographic Data |
Psychopathological Symptoms
The average GHQ-28 total score in all groups was 26.53 points (p = 0.01), where 48.74% (n = 193) (p < 0.05) of patients scored above the cut-off for psychopathology, which was set at >24 points, based on previous research by Goldberg and Hillier.17 Eighty-seven of those patients were in the MS group and forty-eight in the psoriasis group (Figure 2). The highest score was found in the MS group and the lowest scores were found in the kidney transplantation group in every scale subscale. Significant differences between the MS and three other groups in terms of GHQ-28 total score, somatic symptoms, anxiety and insomnia and severe depression were found (p < 0.05). In the GHQ subscale social dysfunction and PSS perceived stress levels significant differences were found between the MS and KT (p < 0.001) and between the MS and P (p < 0.01) groups. A significant difference in the GHQ subscale severe depression was found for the P and KT (p < 0.05) groups. Detailed results can be found in Table 2.
 |
Table 2 PSS, and GHQ 28 Scores in Chronically Ill Patients by Type of Illness |
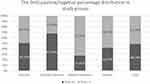 |
Figure 2 The GHQ positive/negative percentage distribution in study groups. |
The Relationship Between Psychopathological Symptoms, Sociodemographic Factors and Perceived Levels of Stress
There was a significant difference in GHQ total score found between patients with a different marital status and between genders. Those who were in separation tended to score significantly higher on the GHQ than those who were married (p < 0.05), and women had significantly higher GHQ total score than men (p > 0.001). A weak but significant negative correlation between the GHQ total score and the number of children (r=−0.111, p < 0.05), a significant negative correlation between the GHQ total score and age of participant (r = −0.229465, p < 0.001) and a significant negative correlation between the GHQ total score and illness duration among the psoriasis group (r = −0.320793, p > 0.01) were found. We noted that people who had received psychiatric or psychological treatment had significantly lower GHQ total scores than those with no history of treatment (p < 0.001 and p < 0.001, respectively). No significant relationships in GHQ total scores were found between people who had contact with COVID, a COVID infection, were quarantined, or had a close one quarantined or infected. A strong significant positive correlation between the PSS score and the GHQ total score (r = 0.631146, p < 0.001) was found.
Discussion
The results of this study describe the levels of psychopathological symptoms in four groups of patients with chronic health conditions: psoriasis, multiple sclerosis and patients who have undergone a kidney transplant or received dialysis. This is the first study comparing the mental health of different chronically ill patients during the COVID-19 pandemic. Over 48% of respondents from the study sample presented clinically relevant psychopathological symptoms. The crucial finding is that the highest psychopathological symptoms were observed in the group of MS patients and the lowest in patients who have undergone kidney transplants during the SARS-CoV2 pandemic.
In our study, the highest level of psychopathological symptoms and perceived stress levels were found in patients diagnosed with MS. These findings may be attributable to disease progression and prognosis in MS. MS is an inflammatory disorder of the brain and spinal cord, resulting in the damage of myelin and axons in the central nervous system, which could be a predisposing factor for mental health problems.20,28 The typical course of MS also includes numerous exacerbations and remissions, which could create an additional stress factor. The relationship between stress and disease progression in MS has been reported in previous research.29 On the other hand, patients who underwent kidney transplants in the past reported the lowest GHQ and PSS scores in our study. Although both groups are undoubtedly highly burdened, patients who underwent a kidney transplant from a living donor face a variety of restrictions and inconveniences, however the transplant procedure offers them a chance to live with a higher quality of life than before the operation.30
In the study conducted by Petrie et al, in New Zealand, the researchers examined dialysis, kidney transplant and general practice (GP) groups of patients using GHQ-30, with a cut-off point of 13 or above for psychological distress. The results showed that 43% dialysis patients, 27% transplant patients and 30% GP achieved a total score above cut-off.31 In comparison, in our study 27.45% of dialysis patients and 41.67% of patients after kidney transplantation reached a total score above cut-off (24 points) for psychopathology. Although no direct comparison is possible due to differences in the instruments used and cut-off scores, similar results under almost twice the points needed for cut-off, could suggest a detrimental influence of the pandemic on mental wellbeing in these two groups. Dialysis patients must attend a hospital unit a few times a week in person to receive treatment, which has posed a higher risk of infection for these patients during the pandemic.
In our study 50.53% of psoriasis patients scored above the cut off for psychopathology. Comparatively, in the study by Finzi et al, 1580 patients with psoriasis completed the GHQ-12, and minor psychological distress was present in 46% of respondents and major psychological distress in 10%. Furthermore, similarly to our study, female sex was related to a significantly worse outcome than male sex.32 Neuropsychiatric comorbidities such as cognitive impairment, anxiety, or mood disorders, are also observed in other dermatological or dysmetabolic disorders, such as prurigo nodularis and Wilson’s disease, respectively.33,34 Interestingly, patients with Wilson’s disease did not experience an exacerbation of their neuropsychiatric symptoms during the SARS-CoV-2 pandemic, as recently proposed by Lanza et al.33
The outcomes addressing a poor psychological wellbeing during the pandemic could be explained by the fact that all participants had already suffered from a chronic illness, thus can be considered both high-risk and susceptible to infection. Various disease-related symptoms experienced by the participants, a fear for their already strained health and regular obligatory control visits to hospital settings where COVID-19 infections are spreading, may account for higher perceived stress levels in the studied population. Additionally, a greater impact of the SARS-CoV-2 pandemic on the mental health of the participants may be related to an easier access to a large amount of quickly-spreading news distributed by mass media and the internet, which seems to have played a less substantial role during the SARS outbreak in 2003 or other similar events.8,35
A significant correlation between perceived stress levels as well as psychopathology and having received psychotherapy and psychiatric treatment in the past was observed in all groups. Having undergone treatment for mental disorders seems to beneficially influence mental health, which could be due to numerous causes. The first interpretation would indicate that successful treatment allows patients to start from a better position in regards to mental health, which may constitute a protective factor in itself. The second interpretation implies that having received treatment may have reinforced or shaped coping strategies, that then allow individuals to better adapt to changing circumstances, therefore resulting in lower stress levels and better mental health. The last interpretation points to the fact that individuals who actively decide to seek help for their problems may be considered more pro-active in the face of challenging circumstances, and therefore better equipped to cope with the present situation (if only through seeking the help of an appropriate specialist).
According to Cohen & Williamson (1988) the PSS median score for the healthy population is 16.62. In comparison to the data in our study – only the KD group scored slightly lower (16.22). The authors also explored stress levels in patients with chronic health conditions, and found the highest scores for patients who experienced a heart attack in the past (21.48), followed by ischemic heart disease (18.84), diabetes (17.50) and dialyzed patients (16.87). In our study, only the MS group scored higher than the heart attack group. The outcomes for the dialysis group in our study, however, were higher than the scores noted by Cohen & Williamson. This could imply that the circumstances of the pandemic could have contributed to increased stress levels in patients having received dialysis.36
The comparison of sociodemographic data and psychopathological symptoms demonstrated that factors like age, sex, marital status and the number of children were significant, however the sociodemographic profile of this study was dissimilar. In the study by Pieh et al 2021 a higher incidence of mental health problems in adults younger than 35 years, women, unemployment, and low income were observed during the SARS-CoV 2 pandemic.37 Worse outcomes noted among young respondents may be explained by the easier access to a variety of information sources, like social media, where a lot of fear-inducing news is presented. In our study, women had a significantly higher GHQ total score than men. This phenomenon was studied by Almeida et al 2020 with the conclusion that women who were pregnant, postpartum, had a miscarriage or experienced partner violence are at a higher risk for developing mental health problems during the pandemic. A protective factor was found to be social support, which was difficult to acquire at the time due to the restrictions on social contact enforced during the pandemic.38 Our results suggest that better outcomes were found among married people and respondents with more children, which can be explained in the context of available social support, by the presence of loved ones at home during the pandemic isolation and not being alone in those hard times.
Surprisingly, factors such as contact with COVID-19, a COVID-19 infection, being quarantined, having a close person quarantined or infected did not significantly influence the outcomes of the study. However, the number of participants who reported having a close person or themselves infected, being quarantined or having contact with COVID-19 was insubstantial and hence lacked statistical power (n = 22). It stands to reason that samples collected further into the pandemic would be more prone to have been infected themselves or have a family member infected, as well as contact with the virus. This result should therefore be treated with caution and compared with more recent research conducted deeper into the pandemic. If direct contact with the pathogen is indeed not significant, a possible explanation could be that people who suffer from chronic diseases may experience higher levels of perceived stress at baseline due to their illness and new stressors, which could have little to a negligible influence on their mental health. This result would benefit from further investigation in future studies. The factor influencing stress levels could also be indirectly related to COVID-19, as opposed to a direct infection or contact. A plethora of restrictions, rumors, misinformation and lifestyle changes resulting from lockdown serve as additional significant stressors during the pandemic and may underlie worse outcomes observed in our study group in a synergistic way.39 Taking this, and moreover the fact that this research was performed in the early stages of the pandemic in Poland into consideration, future studies need to explore this topic in order to prepare suitable guidelines for the management of patients with chronic diseases during future pandemics.
Limitations
The present study has several limitations, including:
- The design of the study, as well as the circumstances surrounding the pandemic, did not allow for any means to compare outcomes, eg, the simultaneous recruitment of a control group who would not have been affected by the pandemic, a pre- or post-pandemic assessment.
- In the dialysis and kidney transplant groups data regarding having had contact with an infected individual, being quarantined or being infected with SARS-CoV-2 were lacking, therefore no conclusions as to the impact of exposure could be drawn.
- The groups were not uniform. The aim of the study was to evaluate the prevalence of psychopathological symptoms among chronically ill patients. In the analysis, we had to choose patients from multiple departments and they would vary in terms of age etc.
- The study was performed in the early stages of the pandemic in Poland. Hence, the number of participants who have undergone COVID-19, had contact with an infected individual or been quarantined was limited. Future studies should account for the influence of a prolonged pandemic on stress levels and in chronically ill patients with an emphasis on COVID-19 convalescents.
- As there was no response rate calculated in this study, sampling and participation biases are of concern.
- The data collection methodology was inconsistent throughout the study. Due to pandemic restrictions questionnaires were collected in both online as well as pen-and-paper format.
- Although the stages and severity of chronic diseases may be a significant factor, influencing mental health and therefore the scores on the instruments used, these variables were not taken into consideration in this study, due to the diversity of the studied patient population (MS, P,KT,D).
Conclusions
As the study was conducted during the SARS-CoV-2 pandemic in Poland, it stands to reason that the pandemic affected the psychopathology among chronically ill patients of the four conditions explored in the study. The highest psychopathological symptoms were observed in the group of MS patients and the lowest in patients who have undergone a kidney transplantation. A COVID-19 infection, being quarantined and having had contact with a person who was infected did not significantly affect the outcome measures, however further research is needed to explore this topic. Despite the differences between groups and diagnoses and the limited generalizability of including only four chronic conditions, the results demonstrate the presence of psychopathological symptoms and psychological distress in these patient groups. The findings of this study highlight the need for additional support and tailored, informed psychological interventions in populations of patients with chronic health conditions in times where all eyes are turned to COVID-19.
Ethics Approval and Consent to Participate
The study was approved by the local Bioethical Committee at the Wroclaw Medical University (KB-468/2020; KB-469/2020; KB-470/2020; KB-417/2020). Participation in the survey was voluntary and without any financial compensation. Anonymity of the responses was maintained throughout the collection and storage of data. Informed consent form to participate in the study and allow procession of data for research purposes was provided in the initial part of the questionnaire. Its confirmation in online version was necessary to proceed with responding and submitting the questionnaire. In printed version the consent was confirmed by signing the form and completion of the questionnaire. Our study complies with the Declaration of Helsinki.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Funding
This research was funded by Wroclaw Medical University, grant number SUBZ.C230.22.062; SUBZ.C160.22.051; SUBZ.C260.22.056.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Romano CM, Chebabo A, Levi JE. Past, present, and future of COVID-19: a review. Brazilian J Med Biol Res. 2020;53(9):1–8. doi:10.1590/1414-431X202010475
2. Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824. doi:10.1016/S2215-0366(20)30307-2
3. Gavriatopoulou M, Korompoki E, Fotiou D, et al. Organ-specific manifestations of COVID-19 infection. Clin Exp Med. 2020;20(4):493–506. doi:10.1007/S10238-020-00648-X
4. Sarubbo F, El Haji K, Vidal-Balle A, Bargay Lleonart J. Neurological consequences of COVID-19 and brain related pathogenic mechanisms: a new challenge for neuroscience. Brain Behav Immun Heal. 2022;19:100399. doi:10.1016/J.BBIH.2021.100399
5. Fisicaro F, Di Napoli M, Liberto A, et al. Neurological sequelae in patients with COVID-19: a histopathological perspective. Int J Environ Res Public Heal. 2021;18(4):1415. doi:10.3390/IJERPH18041415
6. Khoo BZE, See YP, Koh TJK, Yeo SC. Coronavirus disease 2019 (COVID-19) and dialysis: the experience in Singapore. Kidney Med. 2020;2(4):381. doi:10.1016/j.xkme.2020.05.002
7. Centers for Disease Control and Prevention. CDC. Coronavirus (COVID-19): symptoms of coronavirus. Centers for Disease Control and Prevention; 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
8. Anwar A, Malik M, Raees V, Anwar A. Role of mass media and public health communications in the COVID-19 pandemic. Cureus. 2020;12(9). doi:10.7759/cureus.10453
9. Lano G, Braconnier A, Bataille S, et al. Risk factors for severity of COVID-19 in chronic dialysis patients from a multicentre French cohort. Clin Kidney J. 2020;13(5):878–888. doi:10.1093/CKJ/SFAA199
10. Hassanein M, Radhakrishnan Y, Sedor J, et al. COVID-19 and the kidney. Cleve Clin J Med. 2020;87(10):619–631. doi:10.3949/CCJM.87A.20072
11. Li S-Y, Tang Y-S, Chan Y-J, Tarng D-C. Impact of the COVID-19 pandemic on the management of patients with end-stage renal disease. Journal of the Chinese Medical Association. 2020;83(7):628–633. doi:10.1097/JCMA.0000000000000356
12. Pio-Abreu A, Do Nascimento MM, Vieira MA, de Menezes Neves PDM, Lugon JR, Sesso R. High mortality of CKD patients on hemodialysis with Covid-19 in Brazil. J Nephrol. 2020;33(5):875–877. doi:10.1007/s40620-020-00823-z
13. Elias M, Pievani D, Randoux C, et al. COVID-19 infection in kidney transplant recipients: disease incidence and clinical outcomes. J Am Soc Nephrol. 2020;31(10):2413–2423. doi:10.1681/ASN.2020050639
14. Zheng C, Kar I, Chen CK, et al. Multiple sclerosis disease-modifying therapy and the COVID-19 pandemic: implications on the risk of infection and future vaccination. CNS Drugs. 2020;34(9):879–896. doi:10.1007/s40263-020-00756-y
15. Haji Akhoundi F, Sahraian MA, Naser Moghadasi A. Neuropsychiatric and cognitive effects of the COVID-19 outbreak on multiple sclerosis patients. Mult Scler Relat Disord. 2020;41:102164. doi:10.1016/j.msard.2020.102164
16. Sadeghinia A, Daneshpazhooh M. Immunosuppressive drugs for patients with psoriasis during the COVID-19 pandemic era. A Rev Dermatol Ther. 2021;34:1. doi:10.1111/dth.14498
17. gov.pl. Pacjent w czasie koronawirusa; 2020. Available from: https://pacjent.gov.pl/aktualnosc/pacjent-w-czasie-koronawirusa.
18. Statista. Healthcare expenditure as a share of gross domestic product in Poland 1990–2019. Adriana Sas; 2019. Available from: https://www.statista.com/statistics/429697/healthcare-expenditure-as-a-share-of-gdp-in-poland/.
19. Healthcare expenditure statistics. Statistics explained. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Healthcare_expenditure_statistics.
20. Siegert RJ. Depression in multiple sclerosis: a review. J Neurol Neurosurg Psychiatry. 2005;76:469–475. doi:10.1136/jnnp.2004.054635
21. King-wing TM, Kam-tao PL, Li PK, Carol C, Yu R. Depression in dialysis patients. Curr Opin Nephrol Hypertens. 2016;30. doi:10.1111/nep.12742
22. Mahil SK, Yates M, Yiu ZZN, et al. Describing the burden of the COVID-19 pandemic in people with psoriasis: findings from a global cross-sectional study. J Eur Acad Dermatology Venereol. 2021;35:e636–e640. doi:10.1111/JDV.17450
23. Motolese F, Rossi M, Albergo G, et al. The psychological impact of COVID-19 pandemic on people with multiple sclerosis. Front Neurol. 2020;11:1255. doi:10.3389/FNEUR.2020.580507/BIBTEX
24. Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. 1979;9(1):139–145. doi:10.1017/S0033291700021644
25. Makowska Z, Merecz D, Mościcka A, Kolasa W. The validity of general health question-naires, GHQ-12 and GHQ-28, in mental health studies of working people. Int J Occup Med Environ Health. 2002;15:353–362.
26. PSS-10 - Skala Odczuwanego Stresu. Pracownia Testów Psychologicznych. Available from: https://www.practest.com.pl/pss-10-skala-odczuwanego-stresu.
27. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi:10.2307/2136404
28. Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372(9648):1502–1517. doi:10.1016/S0140-6736(08)61620-7
29. Bonavita S, Sparaco M, Russo A, Borriello G, Lavorgna L. Perceived stress and social support in a large population of people with multiple sclerosis recruited online through the COVID‐19 pandemic. Eur J Neurol. 2021;2021:14697. doi:10.1111/ene.14697
30. Pawłowski M, Fila-Witecka K, Rymaszewska JE, Łuc M, Kamińska D, Rymaszewska J. Quality of life, depression and anxiety in living donor kidney transplantation. Transplant Rev. 2020;34(4). doi:10.1016/j.trre.2020.100572
31. Petrie K. Psychological well‐being and psychiatric disturbance in dialysis and renal transplant patients. Br J Med Psychol. 1989;62(1):91–96. doi:10.1111/J.2044-8341.1989.TB02814.X
32. Finzi A, Colombo D, Caputo A, et al. Psychological distress and coping strategies in patients with psoriasis: the PSYCHAE Study. J Eur Acad Dermatol Venereol. 2007;21(9):1161–1169. doi:10.1111/J.1468-3083.2007.02079.X
33. Lanza G, Godani M, Ferri R, Raggi A. Impact of COVID-19 pandemic on the neuropsychiatric status of Wilson’s disease. World J Gastroenterol. 2021;27(39):6733–6736. doi:10.3748/wjg.v27.i39.6733
34. Lanza G, Cosentino FII, Ferri R, et al. Cognitive impairment in inpatients with prurigo nodularis and psychiatric comorbidities. Int J Environ Res Public Health. 2021;18:6265. doi:10.3390/ijerph18126265
35. Su Z, McDonnell D, Wen J, et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Glob Heal. 2021;17(1):1–8. doi:10.1186/S12992-020-00654-4
36. Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Newbury Park, CA: Sage: Claremont Symposium on Applied Social Psychology; 1988:31–67.
37. Pieh C, Budimir S, Delgadillo J, Barkham M, Fontaine JRJ, Probst T. Mental health during COVID-19 lockdown in the United Kingdom. Psychosom Med. 2021;83(4):328–337. doi:10.1097/PSY.0000000000000871
38. Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Heal. 2020;23(6):741–748. doi:10.1007/S00737-020-01092-2
39. Usher K, Durkin J, Bhullar N. The COVID-19 pandemic and mental health impacts. Int J Ment Health Nurs. 2020;29(3):315–318. doi:10.1111/inm.12726
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
