Back to Journals » Psychology Research and Behavior Management » Volume 16
Psychometric Properties of the Moral Injury Symptom Scale Among Indian Healthcare Professionals
Authors Singhal K , Chukkali S
Received 9 January 2023
Accepted for publication 12 April 2023
Published 24 April 2023 Volume 2023:16 Pages 1439—1444
DOI https://doi.org/10.2147/PRBM.S404094
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Kirti Singhal, Surekha Chukkali
Department of Psychology, CHRIST (Deemed to be University), Ghaziabad, Delhi NCR, India
Correspondence: Surekha Chukkali, Department of Psychology, CHRIST (Deemed to be University), Mariam Nagar, Meerut Road, Ghaziabad, Delhi NCR, 201003, India, Tel +91 9901775477, Email [email protected]
Abstract: The spread of the novel coronavirus has led to a rise in morally conflicting situations for healthcare professionals. Doctors and nurses who were serving as frontline workers, require special attention to alleviate the long-lasting impact of the potentially morally injurious events. The current study aims to validate the Moral Injury Symptom Scale-Healthcare Professionals (MISS- HP) among Indian healthcare workers. The 10-item MISS was administered to 150 doctors and 150 nurses using the purposive sampling method. Firstly, reliability was assessed using internal consistency measure. Secondly, item discrimination index was assessed by calculating the point biserial correlation for each item. Cronbach alpha indicated high internal consistency (0.77). The point biserial correlation value for each item indicated good discrimination. Finally, confirmatory factor analysis (CFA) was performed to replicate the factor structure. CFA results suggested a good fit to the data. In conclusion, MISS-HP is a reliable and valid tool to assess moral injury among Indian healthcare professionals in India.
Keywords: pandemic, moral conflict, moral dilemma, frontline workers
Introduction
Doctors and nurses deployed in essential healthcare during the COVID-19 pandemic have been exposed to an upsurge in unprecedented challenges and continuous traumatic events. They were heavily burdened with enforced changes like not allowing any visitors, while witnessing patients dying alone in the intensive care unit. In addition to the magnitude of mortality, the allocation of limited resources forced them to make ethically difficult decisions. Moreover, while constantly bearing the burden of unattended people waiting for care, they were clouded with uncertainties in treatment protocols, accompanied by mortality trajectories.1 This was furthered by the scarcity of intensive care equipment, posing a long-lasting threat to their physical, psychological, and moral well-being.2 Such ethically difficult situations have the potential to become morally injurious. Studies indicate a direct association of events like these with clinician burnout, and psychological distress.3 With the fear of infection gripping in as the pandemic progressed, healthcare workers had to deal with reported abuse and discrimination. The reality of this pandemic has resulted in profound feelings of helplessness, emotional burden, and moral injury in them.
The term “moral injury” was first introduced by Shay as a violation of what is right in military context by oneself or by someone holding a legitimate authority.4 Since then, significant work has been done to understand how moral injury exists among military personnel. Beyond the reported relationship between combat trauma and moral injury, studies have begun to examine moral injury outside the battlefield. Recently, the scope has been expanded to understand the moral dimension of traumatic experiences among civilians. This pandemic led to an influx of challenges and people have witnessed the difficulties advancing from the first wave to the second wave and further. Healthcare workers across the globe were serving the heavy inflow of patients with unrecognizable variants. Adjusting to the increased work volume and intensity accompanied by high transmission rates has challenged them to a large extent. Even though they are prepared to see people suffer and die, yet, witnessing an overwhelming number of deaths has the potential to become morally injurious.5
Moral injury is a concern that remains relevant not just until the pandemic, but long after that. Middle and low-income countries were not prepared to deal with the challenges mediated by the outbreak. India’s healthcare system was brought to the brink of collapse multiple times during the second wave. Thus, it becomes essential for any nation to protect its frontline worker population, especially, the healthcare workers who have been the most critical resource during the pandemic.6 These resources cannot be replenished if immediate actions are not taken to mitigate the distress associated with moral injury.7 Taken together, the COVID-19 pandemic has highlighted and affirmed the importance of having more empirically robust research on such issues. To date, there is a lack of empirical research on moral injury among healthcare professionals in India. Hence, a dire need for more evidence-based research emerges to curtail the compounded effect of these morally injurious events.
Moral injury among healthcare professionals has been increasingly assessed in various studies using narrative analysis and thematic analysis.3 Beyond the qualitative attempts, some studies offer empirical perspectives using the modified versions of already existing tools like the Moral Injury Events Scale. This scale was originally established to assess moral injury in ground combat marines.8 Nonetheless, moral injury remains a concern to objectively assess in India. Thus, to overcome the existing insufficiencies in moral injury assessment for Indian healthcare professionals, it becomes crucial to devise or adapt a psychometrically sound tool.
During the pandemic, the Moral Injury Symptom Scale was recently validated among healthcare professionals in the South-eastern USA.9 It has also been translated and validated into languages like Chinese and Turkish.10,11 To use this scale among healthcare professionals in India, it is important to validate the scale and replicate its factor structure. This will ensure its usefulness in the specific population of Indian healthcare professionals.12
Materials and Methods
Participants
The sample size in validation studies recommends the use of a respondent-to-item ratio of at least 10:1. This suggests an absolute minimum of 100 respondents.13 The present study was carried out among 300 healthcare professionals from various healthcare sectors using the purposive sampling method. The data collection process was completed within 2 months of its initiation. Respondents included 150 doctors and 150 nurses from India’s North and South regions. Healthcare professionals who worked in private clinics or visited the hospital only for emergency treatment were excluded from the study. Those who had suffered a loss of life in their family due to COVID-19 were also excluded. Only those who had worked rotational shifts in hospitals during the COVID-19 pandemic were included.
Measures
All the study participants were administered the 10-item Moral Injury Symptom Scale- Health Professionals (MISS-HP) developed by Mantri et al.9 The responses for each item range from 1 to 10 on the basis of agreement and disagreement. The dimensions that are measured by the MISS-HP include guilt, shame, betrayal, moral concerns, self-condemnation, loss of trust, loss of meaning, difficulty forgiving, and religious struggle with a loss of religious faith. In addition, demographic correlates of the participants were also gathered. This included information about age, gender, and profession. Furthermore, data on whether or not the participants witnessed COVID-related death, and whether or not they themselves got infected by COVID-19 was also collected.
Data Analysis
Descriptive statistics were conducted on all participants depending on whether the variables were continuous or categorical to study the demographic variables. Cronbach alpha was calculated for reliability analysis. For item analysis, point biserial correlation was calculated. For assessing the stability of the factor structure of the MISS-HP in the Indian setting, confirmatory factor analysis (CFA) was performed. To determine the model fit, the comparative fit index (CFI), normed fit index (NFI), incremental fit index (IFI), and root mean square error of approximation (RMSEA) were assessed.14
Results
Demographic Characteristics
Among all the participants, 57.4% belonged to the age group 30–40 years, 29.7% were of the age group 20–30 years, 11.9% were of the age group 40–50 years, and 1% were of the age group 50–60 years. As indicated in Table 1, of these, 35.2% were males, 64.5% were females, and 0.3% belonged to the other categories, given the increased female representation in the healthcare system of India.15 The respondents included 50% doctors and 50% nurses. Nearly two third of the participants witnessed COVID-related death in the workplace (67.3%) and 42.6% of the overall sample were themselves infected by COVID-19.
 |
Table 1 Demographic Characteristics of the Participants |
Reliability and Validity
When calculated in the overall sample, the Cronbach alpha for the MISS-HP turned out to be 0.77. As indicated in Table 2, the CFA analysis resulted in a three-factor model of MISS-HP (RMSEA- 0.073, CFI- 0.98, NFI- 0.96, IFI- 0.98). The three factors were identified (Figure 1) were guilt/shame factor (Q2, Q3, Q4), mistrust factor (Q5, Q6, Q10), and forgiveness factor (Q1, Q7, Q8, Q9). The point biserial correlation for each item is greater than 0.3 (Table 3), indicating that all the items are performing well on the MISS-HP scale.
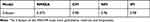 |
Table 2 Fit Indices Resulting from Confirmatory Analysis of the Default Model |
 |
Table 3 Point Biserial Correlation Coefficient (PBCC) Matrix |
 |
Figure 1 The confirmatory factor analysis model. |
Discussion
The current study aimed to validate the already existing MISS-HP in the Indian context. The 10-item MISS-HP was developed by Mantri et al in order to study the clinically significant moral injury symptoms among healthcare professionals, and was used for the study.9 The results from the present study conducted among 300 healthcare professionals (150 doctors and 150 nurses) indicated that MISS-HP is a reliable and valid measure to assess moral injury among healthcare professionals in India. The internal consistency of the MISS-HP indicates good reliability with Cronbach alpha value of 0.77.16 The CFA results are consistent with the findings of Mantri et al (2020) and verify the three-factor model of MISS-HP. Consequently, the construct validity and the model fit of MISS-HP are also acceptable. It is noteworthy that these findings are consistent with the work of Zhizhong et al who validated the MISS-HP among Chinese health professionals during the COVID-19 pandemic.10 Point biserial correlation (>.3 for each item) calculated for item analysis indicated an acceptable discrimination quality of the items and their usefulness in the scale.17
The strength of this study is that the MISS-HP Indian Version can be used as an effective tool to assess moral injury and also monitor the treatment progress among Indian healthcare professionals. However, the study follows certain limitations for its generalizability due to the sample taken such as small and a convenient sample. Despite the limitations, the reliability and validity of the MISS-HP are quite acceptable.
Conclusion
The present article aimed to validate the Moral Injury Symptom Scale-Healthcare Professionals (MISS- HP) among healthcare workers in India. The findings highlighted that MISS-HP is a reliable and valid tool to screen and assess moral injury among healthcare professionals in the Indian setting. Further research on moral injury will help better understand symptoms and the resulting impairments. Considering the ongoing pandemic and the rate of its spread, it is necessary to establish the psychometric properties of the existing tools to assess, reduce, and prevent moral injury symptoms among healthcare professionals for specific populations.
Ethics Declaration
The authors hereby declare that this research involving human participants adheres to the ICMJE guidelines on the Protection of Research Participants. Formal and prospective approval from The Research Conduct and Ethics Committee, Center for Research CHRIST (Deemed to be University), Bengaluru, was obtained. All the participants have provided appropriate informed consent through google forms as a pre-requisite to the main questionnaires.
Acknowledgments
The authors would like to acknowledge the contribution of all the healthcare professionals who participated in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chakma T, Thomas BE, Kohli S, et al. Psychosocial impact of COVID-19 pandemic on healthcare workers in India & their perceptions on the way forward - a qualitative study. Indian J Med Res. 2021;153(5&6):637–648. doi:10.4103/ijmr.ijmr_2204_21
2. Choudhary V, Balhara YPS, Lal R. How could I do something so wrong? Restirring concept of moral injury & healing within health care context of COVID-19 pandemic. Asian J Psychiatr. 2022;70:103017. doi:10.1016/j.ajp.2022.103017
3. Song YK, Mantri S, Lawson JM, Berger EJ, Koenig HG. Morally injurious experiences and emotions of health care professionals during the COVID-19 pandemic before vaccine availability. JAMA Netw Open. 2021;4(11):e2136150. doi:10.1001/jamanetworkopen.2021.36150
4. Shale S. Moral injury and the COVID-19 pandemic: reframing what it is, who it affects and how care leaders can manage it. BMJ Leader. 2020;4(4):224–227. doi:10.1136/leader-2020-000295
5. Watson P, Norman SB, Maguen S, Hamblen J. Moral injury in health care workers. Available from: https://www.ptsd.va.gov/professional/treat/cooccurring/moral_injury_hcw.asp.
6. Behera D, Praveen D, Behera MR. Protecting Indian health workforce during the COVID-19 pandemic. J Family Med Prim Care. 2020;9(9):4541–4546. doi:10.4103/jfmpc.jfmpc_925_20
7. Gupta S, Sahoo S. Pandemic and mental health of the front-line healthcare workers: a review and implications in the Indian context amidst COVID-19. Gen Psychiatr. 2020;33(5):e100284. doi:10.1136/gpsych-2020-100284
8. Amsalem D, Lazarov A, Markowitz JC, et al. Psychiatric symptoms and moral injury among US healthcare workers in the COVID-19 era. BMC Psychiatry. 2021;21(1). doi:10.1186/s12888-021-03565-9
9. Mantri S, Lawson JM, Wang Z, Koenig HG. Identifying moral injury in healthcare professionals: the moral injury symptom scale-HP. J Relig Health. 2020;59(5):2323–2340. doi:10.1007/s10943-020-01065-w
10. Zhizhong W, Koenig HG, Yan T, et al. Psychometric properties of the moral injury symptom scale among Chinese health professionals during the COVID-19 pandemic. BMC Psychiatry. 2020;20:556. doi:10.1186/s12888-020-02954-w
11. Üstün G. Psychometric properties of the Turkish version of the moral injury symptom scale- healthcare professional. J Psy Nurs. 2022;13(1):67–75.
12. Wren TA, Sheng M, Bowen RE, et al. Concurrent and discriminant validity of Spanish language instruments for measuring functional health status. J Pediatr Orthop. 2008;28(2):199–212. doi:10.1097/BPO.0b013e318165216d
13. Anthoine E, Moret L, Regnault A, Sébille V, Hardouin JB. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. 2014;12:176. doi:10.1186/s12955-014-0176-2
14. Hayashi K, Bentler PM, Yuan KH. Structural equation modeling. In: Essential Statistical Methods for Medical Statistics. Elsevier; 2011:202–234. doi:10.1016/b978-0-444-53737-9.50010-4
15. Berlin G, Chen J, Groh R, Sharma M. Women in healthcare and life sciences: the ongoing stress of COVID-19. McKinsey & Company; 2022. Available from: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/women-in-healthcare-and-life-sciences-The-ongoing-stress-of-covid-19.
16. Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. doi:10.5116/ijme.4dfb.8dfd
17. Quaigrain K, Arhin AK, King Fai Hui S. Using reliability and item analysis to evaluate a teacher-developed test in educational measurement and evaluation. Cogent Educ. 2017;4:1301013. doi:10.1080/2331186X.2017.1301013
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
