Back to Journals » Psychology Research and Behavior Management » Volume 15
Psychometric Properties and Factor Analysis of Family Accommodation Scale For Obsessive Compulsive Disorder-Interviewer-Rated-Thai Version (FAS-T)
Authors Tantrarungroj T , Saipanish R , Lotrakul M, Kusalaruk P, Wisajun P
Received 21 January 2022
Accepted for publication 12 June 2022
Published 28 June 2022 Volume 2022:15 Pages 1607—1615
DOI https://doi.org/10.2147/PRBM.S358251
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Thanita Tantrarungroj, Ratana Saipanish, Manote Lotrakul, Pichaya Kusalaruk, Pattarabhorn Wisajun
Department of Psychiatry, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Thanita Tantrarungroj, Department of Psychiatry, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, 270 Rama VI Road, Phayathai, Ratchathewee, Bangkok, 10400, Thailand, Tel +6622011929, Email [email protected]
Purpose: Obsessive compulsive disorder (OCD) is a longstanding and debilitating psychiatric disorder which is related to a level of distress in family members of patients who suffer from it. The Family Accommodation Scale (FAS) for OCD helps medical personnel have a clearer and deeper understanding of the pattern of family accommodation. This study aimed to translate FAS into Thai and examine its psychometric properties and factor analysis.
Patients and Methods: There were fifty participants who were relatives of OCD patients. Demographic data were collected along with completion of the FAS-T, the Patient Health Questionnaire (PHQ-9), the Pictorial Thai Quality of Life (PTQL), and the Thai Florida Obsessive Compulsive Inventory (FOCI-T), and then analyzed. The severity scales of FOCI-T from 44 OCD patients who had relatives participating in this study were collected from medical records and examined. Psychometric properties and factor analysis of FAS-T were tested.
Results: The average total score of FAS-T was 8.36± 8.77 ranging between 0 to 25. The mean scores of FOCI-severity scale in relatives, PHQ-9, PTQL, and FOCI-severity scale in OCD patients, were 1.04± 1.97, 4.04± 3.73, 52.31± 13.99, 8.95± 4.36, respectively. The Cronbach’s coefficient alpha of FAS-T was 0.84, which demonstrated good internal consistency. The item-level CVI and scale-level CVI were at an excellent level. The Spearman’s rho between the FAS and FOCI symptom checklist, FOCI severity score, and PHQ-9 PTQL, were weakly correlated which implied acceptable discriminant validity. Exploratory Factor Analysis (EFA) suggested a three-factor solution as participation, modification, and facilitation.
Conclusion: The Family Accommodation Scale for Obsessive–Compulsive Disorder—Interviewer-Rated - Thai version is a psychometrically reliable and valid measure for assessing accommodation in family members of OCD patients.
Keywords: family, accommodation, obsessive compulsive disorder, Thai
Introduction
Obsessive compulsive disorder (OCD) is a chronic psychiatric disorder1 which is severe and debilitating.2 Patients with obsession and/or compulsion waste a lot of time each day and have deteriorating functions in daily living.3 OCD affects patients in many aspects, such as time, money, study, work, and relationships with others.4 Differences in cultural identity of the person, cultural explanation of the disease, cultural interpretation of psychosocial stressors and the functioning level, and cultural elements of the doctor-patient relationship, have an influence on the manifestations, clinical course, severity, and treatment response in patients with OCD.5
OCD does not only affect patients, but also people around them, especially family members.6 The previous study manifested the positive correlation between the level of distress in family members of OCD patients and patients’ symptoms.7 The adaptation from family members to OCD symptoms place tremendous burden on caregivers and negatively impact their quality of life.8
Even though family members play a vital role in patients’ recovery journey by offering encouragement, promoting help-seeking, and offering housing and financial assistance,9 they might cause stress, more severe psychopathology and higher disability scores for the patients.10 For OCD patients, their family members might try to adjust in many ways. For instance, they change their daily activities in response to the patients’ symptoms or facilitate in compulsion or avoidance because of the patients’ OCD symptoms, this is called family accommodation.11 This is common in OCD and other anxiety disorders with similar characteristics.8 Moreover, the accommodation is prevalent in both childhood and adulthood.12 Studies of family accommodation revealed significant correlation between family accommodation and OCD symptom severity.13,14 This is associated with increasing OCD and anxiety symptoms in the parents of OCD patients. For patients that are undergoing behavioral and pharmacological treatment, levels of accommodation have been associated with treatment outcomes, as shown by the correlation between the significant improvement of OCD symptoms and the reductions in family accommodation.15 Therefore, systematic assessment and keeping track of family accommodation are crucial for therapy which focuses on decreasing family accommodation, to potentially enhance treatment outcome for OCD patients.
Calvocoressi et al16 developed the Family Accommodation Scale for Obsessive Compulsive Disorder Interviewer-Rated (FAS-IR), published in 1999, which assists medical personnel to better understand the pattern of family accommodation. The scale is divided into 2 sections, the first part is regarding the patients’ current symptoms of OCD, which was modified from the Yale-Brown Obsessive-Compulsive Scale. The second section of the FAS-IR consists of the questions about the 12 accommodating behaviors from relatives of patients with OCD. The psychometric properties of FAS-IR demonstrated excellent inter-rater reliability (Intraclass Correlation Coefficient of each item ranges between 0.75–0.97) and good internal consistency (Cronbach’s alpha coefficient = 0.82). It also performed well on convergent, which was significantly correlated with the patients’ Y-BOCS scores and GAF scores. Moreover, it has acceptable discriminant validity with lack of association between FAS and financial stress, and stress associated with caring for non-OCD conditions.
In Thailand, however, we do not have a scale for accommodating behaviors from family members of OCD patients, which would allow healthcare providers to gain a better understanding on the characteristics and degree of accommodating behaviors. Therefore, the objective of this study was to translate FAS into the Thai language and test its psychometric properties.
Materials and Methods
Participants
Fifty participants were relatives of OCD patients who received treatment from the psychiatric outpatient department at Ramathibodi Hospital. Inclusion criteria were 1) relatives of OCD patients, 2) willingness to participate in the study, 3) capable of communicating. Exclusion criteria were having diagnosis of schizophrenia or other psychotic disorders, bipolar affective disorder, severe major depressive episodes, severe substances use disorder, and intellectual disability. In addition, data from 44 OCD patients who had relatives participating in this study were collected from medical records and examined. Information about this study was communicated to all participants, both the relatives and the patients, then informed consent was obtained.
Measures
The Family Accommodation Scale for Obsessive Compulsive Disorder-Thai Version (FAS-T)
The authors translated the Family Accommodation Scale for Obsessive Compulsive Disorder from English to Thai with permission from Dr. Lisa Calvocoressi, the owner of this scale. This study was approved by the ethics committee of Ramathibodi Hospital with document number 2559/703 and performed in compliance with the Declaration of Helsinki. Forward translation was performed by 3 independent translators, the authors then analyzed and discussed the result of translation to generate the preliminary Thai version. After which, the back translation was performed by an academic who is fluent in the English language and has never read the original FAS. The authors then compared the back translation with the original version, discussed and adjusted the Thai version of FAS to make it acceptable for the Thai culture. After that, the authors did a pilot study with a focus group of 10 participants, consequently the Thai version of FAS was finalized.
The Patient Health Questionnaire (PHQ-9)
The PHQ-9 is a self-report measure for depressive symptoms in the past 2 weeks. It consists of 9 questions which comply with the DSM-V criteria diagnosis of Major Depressive Disorder. The Thai version of PHQ-9 has good internal consistency with Cronbach’s alpha=0.79. It has moderate correlation with Hamilton Depression Rating Scale (r=0.56; P<0.001).17
The Pictorial Thai Quality of Life (PTQL)
The PTQL is composed of 25 pictorial-format questions which include 6 aspects as follows: physical, cognitive, affective, social function, economic, and self-esteem. Its alpha coefficient of total test is 0.88 and the six subscales range from 0.81 to 0.93. The level of concurrent validity association with WHOQOL-BREF is high and the Pearson correlation coefficient and Area Under ROC curve are 0.92 and 0.97, respectively.18
The Thai Florida Obsessive Compulsive Inventory (FOCI-T)
The FOCI is a self-report scale which comprises a symptom checklist and symptom severity. The symptom checklist scale assesses the presence of common obsessions (10 items) and compulsions (10 items), of which the total score ranges from 0 to 20. The total severity score ranges from 0 to 20.19 The Thai version of Florida Obsessive Compulsive Inventory (FOCI-T) has satisfactory internal consistency on both the symptom checklist (KR-20 = 0.86) and the severity scale (α = 0.92). The FOCI-T Severity Scale is strongly correlated with the YBOCS-II-T obsession, compulsion, and total score (rs>0.9), also, it has a high correlation with the CGI-S (r=0.76).20
Statistical Methods
The collected data were analyzed using SPSS software (V18.0). The general information is presented in percentage, mean±SD, minimum and maximum value of data.
The reliability of FAS-T was calculated by Cronbach’s coefficient alpha in measuring internal consistency, with the assumption that the acceptable alpha values range from 0.70 to 0.95.21 Moreover, the inter-rater reliability was tested using intra-class correlation coefficient.22
The validity was completed with the Content Validity Index (CVI),23 which was assessed by three psychiatrists with expertise in obsessive compulsive disorder. The CVI can be computed using the Item-CVI (I-CVI) and the Scale-level-CVI (S-CVI).24 Discriminant validity was evaluated by the correlation between FAS-T, PHQ-9, and FOCI-T.
In order to analyze the factor structure of FAS-T, the authors reviewed past studies of FAS-Interviewer Rated (FAS-IR) and found two articles that contain factor analysis. The first one is the Brazilian-Portuguese version from Gomes et al25 whose Exploratory Factor Analysis (EFA) yielded 3 factors; participation, facilitation, and modification. The other is the Chinese version from Liao et al26 whose EFA included a two-factor structure; modification and facilitation, and participation. It is worth mentioning that the 12 items of FAS-IR from Calvocoressi et al16 in 1999 were not presented in the factor analysis.
The Confirmatory Factor Analysis (CFA) was then performed by R Lavaan package version 0.6–11. Several statistical methods were used in the consideration for model fit. It was decided that a nonsignificant Chi-squared value would indicate a good fit between the model and the data. A Comparative Fit Index (CFI) value of above 0.90 would be the indication of an adequate fit. The Root Mean-Square Error of Approximation (RMSEA) of less than 0.06 would be accepted as a model fit.27 After that, the Kaiser-Meyer-Olkin (KMO) and Bartlett Test of Sphericity28 were examined for suitability of data for factor analysis.
The Exploratory Factor Analysis (EFA) was then analyzed to identify the factor constructs of the FAS-T with principal component analysis and oblique rotation.29 The principal component analysis was selected to reduce data while preserving as much information as possible from the original data set. In addition, oblique rotation was chosen to allow for any relationship between the factors to be identified. After which, extraction of factors were based on the eigenvalues that were greater than 1.00 and scree plot.30 Items with a structure matrix value 0.4 or greater were considered as loading on a factor.31
Results
Demographic Data and Mean Scores of Measures
The mean age of participants was 54.36±11.50. Most of the participants were female (76.0%), married (72.9%), and more than half of them graduated with Bachelor’s degree or higher (60.9%). About three-quarters of them were employed (71.7%) and most of them (83.7%) had monthly income of more than 10,000 Bath. Around two thirds of participants were parents of OCD patients (63.8%), with hours per week spent caring for the patient having a mean of 59.74±67.49 and almost half of them (45.7%) had assistance from caregivers to care for the patients.
The mean scores of the FOCI-Severity Scale, PHQ-9, and PTQL were 1.04±1.97, 4.04±3.73, and 52.31±13.99, respectively. The OCD patients had a mean age of 34.42±16.41, being mostly young adults and seniors. The FOCI score of the patients included only the severity scale with a mean score of 8.95±4.36.
Frequency of Patients’ OCD Symptoms from FAS-T
The obsessive symptoms the OCD patients had were contamination (34.0%), somatic obsession (20.0%), other obsessions (20.0%), symmetry obsession (18.0%), hoarding obsession (12.0%), religious obsession (8.0%), harm (8.0%), and sexual obsession (4.0%). Meanwhile, the compulsive symptoms were cleaning (42.0%), checking (34.0%), repeating (18.0%), counting, ordering, hoarding, and other compulsions (9.8%). The OCD patients also had avoidance symptom (39%), doubt (24.4%), indecisiveness (22.0%), slowness (19.5%), and over-responsibility (9.8%).
Scoring of Measures
The average total score of FAS-T was 8.36±8.77 and ranged from 0 to 25. The highest and lowest mean score were “providing reassurance” (1.54±1.63) and “taking on patient’s responsibility” (0.32±0.77), respectively. Table 1 describes the mean scores and frequencies of each item. In addition, the mean score of FOCI-Severity Scale in OCD patients did not significantly correlate with FAS-T (spearman’ rho=0.17,p=0.28).
 |
Table 1 Mean Score and Frequency of Each Item in FAS-T |
Reliability
The internal consistency (Cronbach’s coefficient alpha) of FAS-T was 0.84 which is considered a good internal consistency.21 Cronbach’s coefficient alpha if items deleted are shown in Table 2 and the results suggested that all items should be retained. The inter-rater reliability from Intraclass Correlation Coefficients (ICCs) was 1.0, which was indicative of excellent reliability.32
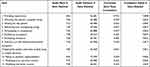 |
Table 2 The Cronbach’s Coefficient Alpha if Item Deleted of Items in Family Accommodation Scale |
Validity
According to the CVI, the Item-CVI (I-CVI) of each item and the Scale-level CVI (S-CVI) were 1.0. The Spearman’s rho between FAS and the FOCI symptom checklist, the FOCI severity score, and PHQ-9 PTQL were weakly correlated at 0.06, 0.17, and 0.27, respectively, which implies acceptable discriminant validity.
Confirmatory Factor Analysis (CFA)
According to the CFA, the three-factor structure which consists of participation, facilitation, and modification from Gomes study25 was examined. Items 5, 6, and 8 are indicated to load on the participation factor; items 1, 2, 3, 9, 10 are indicated to load on the facilitation factor; and items 4, 7, 11, 12 are indicated to load on the modification factor. Results revealed that the covariance matrix of latent variables in this three-factor model is not positively definite.
After that, the Liao’s26 model which consists of two factors; 1) modification and facilitation, and 2) participation, was studied. Items 3, 6, 7, 10, 11, and 12 are indicated to load on the modification and facilitation factor; items 1, 2, 4, 5, 8, and 9 are indicated to load on the participation factor. Results revealed that the model was a poor fit to meet established guidelines (Chi-squared=148.12, degrees of freedom=53, P-value=0.00; CFI=0.61; RMSEA=0.19).
Exploratory Factor Analysis (EFA)
Next, the EFA was examined. The KMO test was 0.70 and Bartlett Test of Sphericity had a significant value (p=0.00), which imply that the data were suitable for factor analysis. The principal component analysis and oblique rotation yielded three factors which accounted for 62.86% of the variance. The factors were categorized as “Participation”, “Modification”, and “Facilitation”. The structure matrix for each item on three factors are presented in Table 3.
 |
Table 3 Factor Loadings of Three-Factor Model Exploratory Factor Analysis with Oblique Rotations |
Discussion
The Family Accommodation Scale for Obsessive Compulsive Disorder Interviewer-Rated (FAS-IR) was proposed in 1999 which allowed healthcare providers in understanding the pattern of family accommodation. However, there is still no measurement for accommodating behaviors in family members of patients with OCD in Thailand. To our knowledge, this is the first study to assess the psychometric properties of the Family Accommodation Scale for Obsessive–Compulsive Disorder—Thai version (FAS-T).
The mean score of FAS-T was 8.36±8.77, which is lower than the other FAS-IR studies, including Calvocoressi’s (12.1±9.79),16 Gomes’s (15.6 ± 10.1),25 and Liao’s (13.99 ± 9.10).26 This might be explained by the relatives’ understanding of the OCD symptoms, the treatments, and ways to help OCD patients.33 Also, the OCD symptoms in the patients were not severe, so, the family members might not need to highly accommodate the patients.34
The most frequently chosen accommodating behaviors were providing reassurance (54%), and tolerating odd behaviors/household disruption (38%). In regards to the responses with extreme or daily basis (endorsement with 4-scored), the two most frequent endorsements were providing reassurance (22%), and refraining from saying/doing things (16%). All the aforementioned accommodating behaviors are passive and do not directly involve the patients. In contrast, the two least frequently chosen items were facilitating compulsion (18%), and taking on patients’ responsibilities (20%), which are similar to the results from Liao’s study.26 These two accommodating behaviors are more active and devoted.
According to the association between accommodating behaviors and the patients’ severity of OCD symptoms, this study found no significant correlation which is not consistent with previous FAS studies.34,35 This could be due to the small sample size, and the patients’ concealment of their symptoms to the family members because many OCD patients still suffer the stigma attached to mental illness.36,37 Also, in Thai culture, the patients might not want to be a burden to their relatives, for example, the cost of treatment and the relatives’ time spent on caring.38 On the other hand, some of the OCD patients did not come to the hospital for many reasons, for example, they are seniors and have difficulties leaving their houses, they avoid coming to the hospital because of their illnesses, and a few patients were unable to take the day off for their appointment. Therefore, their relatives visit the doctor on the patients’ behalf to receive medications, making the number of OCD patients less than the number of relatives (44 versus 50). In addition, most of the relatives were parents of OCD patients, which suggests difficulty in living independently for OCD patients, as they have to live with their parents to receive support in many aspects, such as dwelling, financial, etc.
Regarding the psychometric properties, the result demonstrated acceptable psychometric properties of FAS-T. It revealed a good internal consistency,21 which resembles the original paper of Calvocoressi et al,16 the Brazilian-Portuguese version of Gomes et al,25 and the Chinese version of Liao et al.26 The Cronbach’s coefficient alpha if items deleted in FAS-T suggested that all items should be maintained. According to discriminant validity, the FAS-T demonstrated excellent content validity in both the item and scale levels, which is similar in comparison with the original version.16 The result suggested that FAS-T is relevant to, and representative of, the accommodation from family.39
According to the factor analysis, the CFA was performed and the results showed the inconsistencies with models from Gomes et al25 and Liao et al.26 The outcome implies that the factor structure of FAS was still unsettled. The EFA was applied and the data yielded three factors; participation, modification, and facilitation. However, some items tend to conform to more than one factor. For instance, item 5 which is regarding the relatives’ participation in compulsion, belongs to both participation and modification factors. Also, the question about helping patients with the tasks of daily living or simple decisions (item 9) took part in both participation and facilitation factors. For this reason, it is difficult to clearly differentiate the group of items in each factor. In comparison with studies of FAS-IR in the past, the three-factor solution is similar to the results from Gomes et al’s study.25 However, the items in each factor in the FAS-Thai version might be modestly different from the Brazilian-Portuguese’s version. For example, Question 8 which asks the relative about tolerating odd behaviors and household disruption, showed high factor loading in modification factor in this study. From the authors’ perspective about item 8, the relatives of OCD patients have adapted their usual lifestyles to endure the patients’ odd behaviors or household disruptions.
The factor structure of this study is different from the FAS-Chinese version,25 which contained 2 components; modification and facilitation, and participation. However, there are many items which loaded on the same factor. For example, items 1, 2, 4, and 9 of the Chinese and the Thai versions were loaded on the “participation” factor.
Limitation
This study has several limitations which should be addressed. First, it contained a small sample size, which might result in inadequate statistical power. However, it is worth considering that many OCD patients come to receive treatment at the hospital on their own without their relatives being by their side, moreover, others do not want their family members to know about their illness. On the other hand, some OCD patients avoid leaving their homes and request their relatives to see doctors on their behalf. Secondly, we did not perform test-retest reliability in this study. Thirdly, the severity of OCD patients’ conditions was measured with the FOCI, which is reported by the patients and might contain social desirability bias. In the future, it will be vital to utilize this family accommodation scale in order to assess the effectiveness of family intervention, as well as to encourage family members to be involved in treating OCD patients.
Conclusion
In conclusion, the FAS-T has excellent psychometric properties. The instrument would be useful for mental healthcare providers in assessing OCD patients’ family accommodation, and in planning suitable intervention for family members, which will be advantageous for patients and their families.
Acknowledgment
The authors in this study would like to express sincere gratitude toward all the participants in this study. The authors also would like to express great appreciation to Asst.Prof. Thanavadee Prachason, Ph.D. for the valuable and constructive suggestions in statistical analysis.
Disclosure
The authors report no conflicts of interest in this study.
References
1. Visser HA, van Oppen P, van Megen HJ, Eikelenboom M, van Balkom AJ. Obsessive-compulsive disorder; chronic versus non-chronic symptoms. J Affect Disord. 2014;152:169–174. doi:10.1016/j.jad.2013.09.004
2. Masellis M, Rector NA, Richter MA. Quality of life in OCD: differential impact of obsessions, compulsions, and depression comorbidity. Can J Psychiatry. 2003;48(2):72–77. doi:10.1177/070674370304800202
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. VA: American Psychiatric Publishing; 2013.
4. Challacombe F, Oldfield VB, Salkovskis P. Break Free from OCD. London: Vermilion; 2011.
5. Nicolini H, Salin-Pascual R, Cabrera B, Lanzagorta N. Influence of culture in obsessive-compulsive disorder and its treatment. Curr Psychiatry Rev. 2017;13(4):285–292. doi:10.2174/2211556007666180115105935
6. Albert U, Balla A, Maina G. Family accommodation in adult obsessive compulsive disorder: clinical perspectives. Psychol Res Behav Manag. 2017;10:293–304. doi:10.2147/PRBM.S124359
7. Amir N, Freshman M, Foa EB. Family distress and involvement in relatives of obsessive-compulsive disorder patients. J Anxiety Disord. 2000;14(3):209–217. doi:10.1016/S0887-6185(99)00032-8
8. Lebowitz ER, Panza KE, Bloch MH. Family accommodation in obsessive-compulsive and anxiety disorders: a five-year update. Expert Rev Neurother. 2016;16(1):45–53. doi:10.1586/14737175.2016.1126181
9. Waller S, Reupert A, Ward B, McCormick F, Kidd S. Family-focused recovery: perspectives from individuals with a mental illness. Int J Mental Health Nurs. 2019;28:247–255.
10. Mahapatra A, Kuppili PP, Gupta R, Deep R, Khandelwal SK. Prevalence and predictors of family accommodation in obsessive-compulsive disorder in an Indian setting. Indian J Psychiatry. 2020;62(1):43–50. doi:10.4103/psychiatry.IndianJPsychiatry_299_17
11. Gomes JB, Cordioli AV, Bortoncello CF, Braga DT, Gonçalves F, Heldt E. Impact of cognitive-behavioral group therapy for obsessive-compulsive disorder on family accommodation: a randomized clinical trial. Psychiatry Res. 2016;246:70–76. doi:10.1016/j.psychres.2016.09.019
12. Lebowitz ER, Scharfstein LA, Jones J. Comparing family accommodation in pediatric obsessive-compulsive disorder, anxiety disorders, and nonanxious children. Depress Anxiety. 2014;31(12):1018–1025. doi:10.1002/da.22251
13. Strauss C, Hale L, Stobie B. A meta-analytic review of the relationship between family accommodation and OCD symptom severity. J Anxiety Disord. 2015;33:95–102. doi:10.1016/j.janxdis.2015.05.006
14. Stewart KE, Sumantry D, Malivoire BL. Family and couple integrated cognitive-behavioural therapy for adults with OCD: a meta-analysis. J Affect Disord. 2020;277:159–168. doi:10.1016/j.jad.2020.07.140
15. Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother. 2012;12(2):229–238. doi:10.1586/ern.11.200
16. Calvocoressi L, Mazure CM, Kasl SV, et al. Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family behavior. J Nerv Ment Dis. 1999;187(10):636–642. doi:10.1097/00005053-199910000-00008
17. Lotrakul M, Sumrithe S, Saipanish R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry. 2008;8(1):1–7. doi:10.1186/1471-244X-8-46
18. Phattharayuttawat S, Ngamthipwatthana T, Pitiyawaranun B. The development of the pictorial Thai quality of life. J Med Assoc Thai. 2005;88(11):1605–1618.
19. Storch EA, Bagner DA, Merlo LJ, et al. Florida obsessive-compulsive inventory: development, reliability, and validity. J Clin Psychol. 2007;63(9):851–859. doi:10.1002/jclp.20382
20. Saipanish R, Hiranyatheb T, Lotrakul M. Reliability and validity of the Thai version of the Florida obsessive-compulsive inventory. Sci World J. 2015; 2015:240787.
21. Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. doi:10.5116/ijme.4dfb.8dfd
22. Bobak CA, Barr PJ, O’Malley AJ. Estimation of an inter-rater intra-class correlation coefficient that overcomes common assumption violations in the assessment of health measurement scales. BMC Med Res Methodol. 2018;18(1):93. doi:10.1186/s12874-018-0550-6
23. Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006;29(5):489–497. doi:10.1002/nur.20147
24. Rodrigues IB, Adachi JD, Beattie KA, MacDermid JC. Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis. BMC Musculoskelet Disord. 2017;18(1):540. doi:10.1186/s12891-017-1914-5
25. Gomes JB, Cordioli A, Van Noppen B, et al. Family accommodation scale for obsessive-compulsive disorder-interviewer-rated (FAS-IR), Brazilian Portuguese version: internal consistency, reliability, and exploratory factor analysis. Compr Psychiatry. 2015;57:155–159. doi:10.1016/j.comppsych.2014.11.017
26. Liao Z, You C, Chen Y, Zhang J, Ding L. Psychometric properties of the Chinese version of the family accommodation scale for obsessive-compulsive disorder interviewer-rated. Compr Psychiatry. 2021;105:152220. doi:10.1016/j.comppsych.2020.152220
27. Byrne BM. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming.
28. Dziuban CD, Shirkey EC. When is a correlation matrix appropriate for factor analysis? Some decision rules. Psychol Bull. 1974;81(6):358–361. doi:10.1037/h0036316
29. Jung S, Lee S. Exploratory factor analysis for small samples. Behav Res. 2011;43:701–709. doi:10.3758/s13428-011-0077-9
30. Streiner DL. Figuring out factors: the use and misuse of factor analysis. Can J Psychiatry. 1994;39(3):135–140. doi:10.1177/070674379403900303
31. Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess. 1995;7(3):286–299. doi:10.1037/1040-3590.7.3.286
32. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012
33. Pedley R, Bee P, Berry K, Wearden A. Separating obsessive-compulsive disorder from the self. A qualitative study of family member perceptions. BMC Psychiatry. 2017;17:326. doi:10.1186/s12888-017-1470-4
34. Wu MS, McGuire JF, Martino C, Phares V, Selles RR, Storch EA. A meta-analysis of family accommodation and OCD symptom severity. Clin Psychol Rev. 2016;45:34–44. doi:10.1016/j.cpr.2016.03.003
35. Steketee G, Van Noppen B. Family approaches to treatment for obsessive compulsive disorder. Braz J Psychiatry. 2003;25(1):43–50. doi:10.1590/S1516-44462003000100009
36. Burnard P, Naiyapatana W, Lloyd G. Views of mental illness and mental health care in Thailand: a report of an ethnographic study. J Psychiatr Ment Health Nurs. 2007;13(6):742–749.
37. Wong-Anuchit C, Mills AC, Schneider JK, Rujkorakarn D, Kerdpongbunchote C, Panyayong B. Internalized stigma of mental illness scale - Thai version: translation and assessment of psychometric properties among psychiatric outpatients in central Thailand. Arch Psychiatr Nurs. 2016;30(4):450–456. doi:10.1016/j.apnu.2016.01.012
38. Pitakchinnapong N, Rhein D. Exploration of the causation of stigmatization of mental illness in Thailand: perceptions of Thai University Students. Comput Hum Behav. 2019;2:24.
39. Rusticus S. Content validity. In: Michalos AC, editor. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer Netherlands; 2014:1261–1262.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
