Back to Journals » Patient Preference and Adherence » Volume 16
Psychometric Assessment of the Mandarin Version of the Decisional Conflict Scale with Pregnant Women Making Prenatal Test Decisions
Authors Xiang JM, Sun K, Zhao Q, Li HB, Gao LL
Received 3 November 2021
Accepted for publication 29 December 2021
Published 18 January 2022 Volume 2022:16 Pages 149—158
DOI https://doi.org/10.2147/PPA.S346017
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Jia-Ming Xiang,1 Ke Sun,2 Qian Zhao,1 Han-Bing Li,1 Ling-Ling Gao1
1School of Nursing, Sun Yat-sen University, Guangzhou, People’s Republic of China; 2The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, People’s Republic of China
Correspondence: Ling-Ling Gao, School of Nursing, Sun Yat-sen University, 74#, Zhongshan Road II, Guangzhou, 510089, People’s Republic of China, Tel +86-20-87335013, Fax +86-20-87333043, Email [email protected]
Purpose: Women with high-risk pregnancies are often required to make choices about further prenatal testing for Down syndrome, but the decisional conflict they face is poorly understood. This study aimed to test the validity and reliability of the Mandarin version of the decisional conflict scale (M-DCS) in Chinese women with high-risk pregnancies making choices about further prenatal testing for Down syndrome.
Patients and Methods: A methodological study was conducted to determine the psychometric properties of the M-DCS, specially, reliability and content, construct, and concurrent validity. The convenience sample comprised 240 pregnant women with high risk for Down syndrome attending the out-patient clinic of the study hospital in Guangzhou, China.
Results: The five-factor model of M-DCS was supported by confirmatory factor analysis with a satisfactory fit to the data (RMSEA < 0.08, RMR < 0.05, GFI, CFI, NFI, and IFI all > 0.90, except AGFI=0.88 PNFI = 0.76). The internal consistency of the M-DCS was high, with Cronbach’s ? of 0.94.
Conclusion: The reliability and validity (content, construct, and concurrent) of the M-DCS were all demonstrated as good. This instrument is an important tool for researchers and health-care providers working with women with high-risk pregnancies who need to make choices about further prenatal testing for Down syndrome.
Keywords: decisional conflict, prenatal testing, reliability, validity
Introduction
Down syndrome is the most common cause of intellectual disability around the world, affecting approximately 1:500 pregnancies and reported in 1:800 to 1:1000 live births.1 In addition to intellectual disability, individuals with Down syndrome typically experience other medical complications, including congenital heart disease, and degenerative changes in their joints.2 The economic burden of Down syndrome can be substantial for the families and society.3 Down syndrome can be prevented by screening and diagnostic tests available in many countries, including mainland China.4,5 In mainland China, all pregnant women are offered screening for Down syndrome.6 Women who book before 13+6 weeks and accept Down syndrome screening are offered the serum biomarkers (PPAP-A, and free β-HCG) to determine risk.6 Those between 15 and 20 weeks are offered the triple test based on serum markers (AFP, free β-HCG, and μE3) and maternal age.7
Women identified as having an increased risk for Down syndrome are offered a definitive diagnosis through invasive testing that carries a small risk of miscarriage (0.5%).8 Women with high risk can also choose non-invasive prenatal testing (NIPT) that sequences cell-free DNA (cf-DNA) in maternal plasma as a second-tier screening for Down syndrome. NIPT holds no risk of miscarriage and detects the presence of Down syndrome with high sensitivity (99.9%) and specificity (98%).9,10 However, NIPT is not covered by the publicly funded healthcare system and is not considered sufficiently accurate for a diagnosis.11 Furthermore, if the NIPT detection results are also positive, pregnant women will finally be faced with the options of invasive diagnostic testing.12
Faced with the decision-making choices about further prenatal testing for Down syndrome, pregnant women often worry the health of the fetus and are uncertain with various options and their associated advantages and disadvantages.13 Parents may be conflicted by their parental responsibilities and the quality of life their future children may experience, leading to great uncertainty in prenatal testing.14 Thus, women with high risk for Down syndrome face many difficult decisions and are likely to experience decisional conflict, exacerbated by the time constraints under which the decisions must be made.14,15 All the options carry some risk, are irreversible and emotionally laden.14,15
Decisional conflict is affected by many factors, including lack of knowledge of prenatal testing, perceived differences of opinion from partner/spouse, doctors’ decisional preferences, and being childless.14,16,17 In particular, a lack of social support or existing anxiety are the main determinants of increased decisional conflict.18–20 Lo et al found that over 50% of women experienced anxiety at the time of decision-making regarding receiving NIPT or not.18 Lee et al revealed that lower perceived social support resulted in more decisional conflict.20 Unresolved decisional conflict can adversely affect outcomes including decision quality and implementation.14–18 A careful assessment of women’s decisional conflict is, therefore, a prerequisite for developing the appropriate counselling services and decision support.
The decisional conflict scale (DCS) was developed to measure the level of decisional conflict and has been used worldwide for multiple decision types, clinical contexts, and populations, demonstrating its value as a decision-making evaluation measure.21 Adaptations of the DCS into numerous languages have demonstrated good psychometric properties.22–24 Legare et al conducted a systematic review of decision-support interventions and shared decision-making in healthcare and indicated that the DCS is the most commonly used measure related to decision-making, used for a variety of purposes.25
However, prior to this study, an appropriate version of the DCS was not available in Mandarin, and the DCS had not been validated in high-risk pregnant women making choices about further prenatal testing for Down syndrome in mainland China. Therefore, this study aimed to evaluate the reliability and validity of the Mandarin version of the DCS with women with high-risk pregnancies making choices about further prenatal testing for Down syndrome.
Materials and Methods
Design, Setting and Participants
A methodological study was conducted in Guangzhou, China, from September 2020 to July 2021. Guangzhou, located in the southeast of China, is the provincial capital of Guangdong Province, with a population of 16 million. Participants in this study were recruited from one of the affiliated hospitals of Sun Yat-sen University, where more than 4000 babies are born every year. The inclusion criteria were: (a) identified as having an increased risk (≧1:270) for Down syndrome in the first trimester by the serum biomarkers (PPAP-A, and free β-HCG) or in the second trimester of pregnancy by the triple test (AFP, free β-HCG, and μE3) and maternal age,6,7 (b) Singleton pregnancy, and (c) aged ≥18 years. The exclusion criteria were: (a) not able to understand and read Chinese, and (b) having other fetal abnormalities, including surface malformations or in vivo malformation by prenatal combined testing.
Some authors recommend that 10 participants per item is an acceptable sample size for factor analysis,26,27 while others suggest that a sample size of 200 is adequate for most factor analysis.28 We recruited a convenience sample of 255 pregnant women with high risk for Down syndrome attending the out-patient clinic of the study hospital. Fifteen participants did not complete the entire assessment and were excluded. A total of 240 women (response rate: 94.1%) completed the questionnaire.
Measures
The DCS was used to measure the decisional conflict in women with high-risk pregnancies making choices about further prenatal testing for Down syndrome.29 O’Connor developed the DCS in 1995 to measure individuals’ perceptions of their uncertainty in making a choice about health-care options, the modifiable factors contributing to uncertainty, and the quality of the decision made.29 The DCS is a 16-item scale comprising five dimensions: uncertainty (3 items), feeling informed (3 items), clarity related to personal values (3 items), feeling supported (3 items), and effective decision-making (4 items).30 Responses to each item are recorded on a 5-point scale ranging from 0 (strongly agree) to 4 (strongly disagree). The total score is calculated by dividing the score of 16 items by 16 and multiplying by 25. Total scores range from 0 (no decisional conflict) to 100 (high decisional conflict). A score of <25 indicates an effective decision, while a score of ≥37.5 is associated with decision delay or feeling uncertain about the decision.30 A higher score means a higher level of decisional conflict. The original version of the DCS provided by the original author was adapted into Mandarin for this study. The DCS was translated into Mandarin by one bilingual team member and then back-translated into English by a second independent team member. Original and back-translated versions were compared. Discrepancies were identified and resolved by discussion, and the translation procedure was reiterated until satisfactory semantic equivalence was found. Then the Mandarin version of the DCS was reviewed by six experts, including two nursing professors, two obstetricians and two midwives, all first-language speakers of Mandarin. They were requested to provide a quantitative rating for each item. The content validity ratio (CVR) and content validity index (CVI) of each item were examined.
The Self-rating Anxiety Scale (SAS) was used to measure participants’ anxiety symptoms.31 The SAS includes 20 items, with each item scored on a 4-point Likert scale where 1 = none or a little of the time and 4 = most or all of the time. The final standardized score is the sum of item scores multiplied by 1.25, ranging from 25 to 100. A SAS standard score ≧50 is considered to indicate anxiety symptoms in the general adult population.32 The scale has been widely used to measure the anxiety symptoms of pregnant Chinese women, and has good reliability and validity.33,34 Cronbach’s alpha was 0.80 in the present study.
The Social Support Rating Scale (SSRS) was used to measure the social support available to the pregnant women.35 The 10-item SSRS yields scores ranging from 12 to 66, where higher scores refer to higher levels of social support. The SSRS has been widely used with different populations in different areas, and proved to have good reliability and validity for pregnant Chinese women.36 In the current study, Cronbach’s alpha was 0.64.
Socio-demographic and obstetric questionnaires were used to collect additional data, including age, education, occupation, monthly household income, number of previous miscarriages/abortions, gestational age, parity, and decision about further prenatal testing.
Procedure and Ethical Considerations
Ethical approval was obtained from the Institutional Review Boards (IRB) of the Third Affiliated Hospital of Sun Yat-sen University. As the present study was a survey, the IRB of the hospital fast-tracked the review without assigning IRB numbers. The research conforms to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh in 2000). The data were collected by the first author, who worked in the study hospital as a research assistant. All eligible women waiting for their genetic counselling at the hospital out-patient clinic were invited to participate in the study. They were informed about the purpose and procedures of the study, and signed a consent form before inclusion. If a woman obtained a SAS score ≥50, this score was shared with their medical doctor at the clinic with their consent. In that event, a referral was also made to a psychiatrist at the hospital for further clinical assessment and/or treatment. This study did not envisage further follow-up of these women.
Statistical Analysis
Data were analyzed with IBM SPSS Statistics version 22.0, and LISREL version 8.80. Descriptive statistics were used to present demographic and antenatal characteristics. The internal consistency of the Mandarin version of the DCS was assessed using Cronbach’s alpha.
The validity of the scale was tested for content, construct, and concurrent validity. In this study, confirmatory factor analysis (CFA) was used to evaluate the construct validity of the scale. Bartlett’s tests were performed to examine the adequacy of the data for factor analysis. The maximum likelihood method was chosen for parameter estimation to test the five-factor structure of the DCS. Several fit indices, such as, χ2/df, root mean square error of approximation (RMSEA), root mean square residual (RMR), the goodness-of-fit index (GFI), the adjusted goodness-of-fit index (AGFI), the comparative fit index (CFI), the normed fit index (NFI), the parsimony normed fit index (PNFI) and the incremental fit index (IFI) were used to assess how well the tested models fitted the data.37 χ2/df values of <3, GFI, AGFI, CFI, NFI, PNFI and IFI values of >0.90, RMSEA values of <0.08 and RMR values of <0.05 were taken as indicating good fit.37 GFI, AGFI, CFI, NFI, PNFI and IFI values of >0.80 suggested a mediocre fit.37
Women who underwent invasive diagnosis testing and non-invasive prenatal testing were both included in the study. The participants were divided according to their decisions about further prenatal testing into the invasive diagnosis testing group and the NIPT group. An independent t-test was used to compare the difference in the DCS scores between the invasive diagnosis testing group and the NIPT group. The concurrent validity of the M-DCS was examined by calculating the correlation coefficients of the DCS with the SAS and SSRS.
Results
Participant Characteristics
Table 1 presents the socio-demographic and antenatal characteristics of the study participants. The mean age of the participants was 33.9 (SD = 4.6, range = 22–45) years. The majority of the women (72.5%) had attained at least a tertiary education. Most (81.6%) had a full-time job. Over two-thirds of the women (70.0%) had a monthly household income of more than ¥6000 (US$938) per person, above the average monthly household income in Guangzhou.38 The mean gestational age was 16.1 (SD = 2.0, range = 12–20) weeks. Sixty percent of the women were multiparous. About half of the women had suffered one or more miscarriages. Nearly two-thirds (67.5%) of the sample opted for invasive diagnostic testing.
 |
Table 1 Socio-Demographic and Obstetric Characteristics (n = 240) |
Content Validity
Content validity refers to the theoretical basis and practical experience to judge the extent to which the items in the research tool reflect the measured content.39 Experts were required to review the items with respect to being necessary, beneficial, or unnecessary. Then, the questionnaires were collected, and the content validity ratio (CVR) was calculated for each item.40 Thereafter, experts evaluated the concept to be measured based on the relevance of each item, using a 4-point Likert scale ranging from 1 (not relevant at all) to 4 (very relevant). In this study, six experts were invited to quantify the content validity of the Mandarin version of the DCS. Based on the Lawshe table, the acceptable CVR for the six experts was 1.40 CVR for all the items met the criterion. The I-CVI of each item exceeded 0.8 and S-CVI was 0.99, suggesting the content validity of DCS is good.
Construct Validity
Bartlett’s test (χ2=2532.50, df=120, p < 0.001) and the Kaiser-Meyer-Olkin (0.94) indicated that the M-DCS was appropriate for factor analysis. The five-factor model was supported by CFA with a satisfactory fit to the data (RMSEA <0.08, RMR <0.05, GFI, CFI, NFI, IFI all >0.90, except AGFI = 0.88 and PNFI = 0.76; Table 2), which reflected a good construct validity. The values of factor loadings indicated that the items had significant loadings on the five-factor model, as shown in Figure 1. Factor loadings ranged from 0.71 to 0.84 on “Feeling informed”; 0.81 to 0.85 on “Clarity related to personal values”; 0.74 to 0.76 on “Feeling supported”; 0.63 to 0.86 on “Uncertainty,” and 0.78 to 0.83 on “Effective decision-making,” showing that the item corresponding to each latent variable was highly representative. The statistical significance of the five-factor correlations supported the hypothesis that the five factors (feeling informed, clarity related to personal values, feeling supported, uncertainty and effective decision-making) were highly related dimensions of decisional conflict (p < 0.001; Figure 1).
 |
Table 2 Goodness of Fit Indices of Confirmatory Factor Analysis of the M-DCS |
 |
Figure 1 Confirmatory factor analysis of the M-DCS. Abbreviation: DCS, decisional conflict scale. Note: Error is represented by “e.” |
Concurrent Validity
The M-DCS score correlated positively with the SAS and negatively with the SSRS. Each subscale correlated positively with the SAS and correlated negatively with the SSRS, supporting the construct validity of the M-DCS. These values are provided in Table 3.
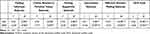 |
Table 3 Correlation Matrix for Concurrent Validity of the M-DCS |
Comparison of Mean DCS Scores Between Different Groups
As shown in Table 4, the women in the NIPT group reported higher levels of decisional conflict than the women in the invasive diagnosis testing group, providing evidence supporting the construct validity of the M-DCS.
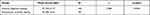 |
Table 4 Comparison of Mean M-DCS Scores Between Different Groups |
Reliability
The internal consistency of the M-DCS was high, with Cronbach’s α = 0.94. As Table 5 shows, each subscale demonstrated good internal consistency, with Cronbach’s α over 0.80. The correlation between each subscale and the total scale exceeded 0.80 (p < 0.001), and the correlation coefficients of the subscales were significantly correlated (p < 0.001), indicating significant overlap among the five subscales (Table 6).
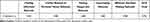 |
Table 5 Reliability of the M-DCS |
 |
Table 6 Correlation Matrix for Each Subscale and Total Scale of the M-DCS |
Discussion
This study evaluated the validity and reliability of the M-DCS in Chinese women with high-risk pregnancies required to make choices about further prenatal testing for Down syndrome. Consistent with previous studies,22–24 the findings of the present research demonstrated that the M-DCS is a valid and reliable tool for the assessment of decisional conflict. The M-DCS and its five subscales have good internal consistency, with Cronbach’s alpha exceeding 0.80 for the each subscale and total scale. These five subscales correlated strongly with each other showing satisfactory homogeneity among all items.
CFA showed that the original five-factor model fitted the data of the M-DCS in our sample. However, the high correlations (r = 0.58~0.90, p < 0.001) among five dimensions may reflect duplication of the variables in the five subscales.41 The homogeneity within and distinctiveness among the five factors of the M-DCS need further research. Studies in other regions such as Hong Kong22 and the Netherlands23 failed to clearly distinguish “Feeling informed” and “Clarity related to personal values.” Studies in Japan found “Uncertainty” and “Effective decision-making” were loaded on the same dimension.24
There are several potential reasons for the different study results. First, the population selected for study here differed from previous research which focused mainly on cancer patients. The population selected in this study was relatively free of life-threatening conditions. In a different decision-making context, the way patients cope with stressful events will also change. Women’s decisions about prenatal testing for Down syndrome may largely reflect personal values and considerations within a unique socio-cultural context. In Chinese tradition, the family occupies a valued position and it is important to have healthy offspring to continue the family name.33 Aside from cultural norms, in mainland China, raising a child currently involves a great financial burden. This increased difficulty is creating a social norm where children are more valued, and having a “perfect” baby is an unspoken expectation among pregnant couples.
Second, differences in the time points at which decisions are made may influence the process of decision-making. Under China’s new three-child policy, health-care providers’ workloads will continue to increase, leading to inadequate treatment and communication.42 Meanwhile, patients often lack a comprehensive understanding of the content of decision-making because of inaccurate medical information, leading to decisional conflict.43,44 Compared to those diagnosed with cancer, pregnant women screened as high risk had relatively little time to make a decision. Typically, most women have to make their decision about which test to undergo on the same day they receive counseling. The time available for patients to search for and receive information is very limited. The findings of the present study are partly consistent with the previous work.24 Kawaguchi et al also confirmed that the results of the cluster analysis of DCS may be affected by the timing.24 Essentially, the difference in factor structure across studies may be due to the heterogeneity of samples regarding medical decision-making types and cultures.
The CVI scores of all items were greater than 0.80, demonstrating that all items in the scale reflect the conflict of pregnant women’s reproductive decision-making. Concurrent validity was good, as indicated by a positive relationship with measures of anxiety and a negative relationship with social support measures. The M-DCS demonstrated expected patterns for known-group comparisons regarding decisions about further prenatal testing. The women in the NIPT group reported greater levels of decisional conflict compared to the women in the invasive diagnosis testing group. These results are consistent with Tanja,15 who found that choosing NIPT was associated with high decisional conflict.
This study has several limitations. First, a convenience sampling method was used for sampling. Second, most of the participants were well educated, married, and middle-class. Thus, generalization of the results is limited. In further studies, the psychometric properties of the M-DCS should be explored in a less literate, more rural and varied socio-economic sample.
Conclusion
In this study, reliability and validity (including content, construct and concurrent validity) of the M-DCS were all demonstrated to be good. The M-DCS provides health professionals with a useful tool for the early identification of pregnant women with high risk for Down syndrome who have difficulty in decision-making. It may also be used in identifying women with high decisional conflict who need extra support during prenatal genetic counseling. Furthermore, the tool may facilitate the development of culturally appropriate interventions to promote the quality of decision-making.
Acknowledgments
We would like to thank all the experts involved in the scale translation and cross-cultural cultural adaptation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Greydanus DE, Pratt HD. Syndromes and disorders associated with mental retardation. Indian J Pediatr. 2005;72(10):859–864. doi:10.1007/BF02731116
2. Roizen NJ, Patterson D. Down’s syndrome. Lancet. 2003;361(9365):1281–1289. doi:10.1016/S0140-6736(03)12987-X
3. Chen Y, Qian X, Zhang J, Li J, Chu A, Schweitzer SO. Preliminary study into the economic burden of Down syndrome in China. Birth Defects Res A Clin Mol Teratol. 2008;82(1):25–33. doi:10.1002/bdra.20409
4. Agarwal GN, Kabra M. Diagnosis and management of down syndrome. Indian J Pediatr. 2014;81(6):560–567. doi:10.1007/s12098-013-1249-7
5. Wang R, Yu Y, Xi Q, et al. Analysis of prenatal diagnosis before and after implementation of the two-child policy in northeastern China. Medicine. 2019;98(38):e17200. doi:10.1097/MD.0000000000017200
6. Ministry of Public Health of China. Measures for administration of health care during pregnancy and child and standardization for health care during pregnancy and child; 2021. Available from: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=52320.
7. Alldred SK, Deeks JJ, Guo B, Neilson JP, Alfirevic Z. Second trimester serum tests for down’s syndrome screening. Cochrane Database Syst Rev. 2012;2012(6):D9925.
8. Akolekar R, Beta J, Picciarelli G, Ogilvie C, D’Antonio F. Procedure-related risk of miscarriage following amniocentesis and chorionic villus sampling: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2015;45(1):16–26. doi:10.1002/uog.14636
9. Metcalfe SA. Genetic counselling, patient education, and informed decision-making in the genomic era. Semin Fetal Neonatal Med. 2018;23(2):142–149. doi:10.1016/j.siny.2017.11.010
10. Norton ME, Brar H, Weiss J, et al. Non-Invasive Chromosomal Evaluation (NICE) Study: results of a multicenter prospective cohort study for detection of fetal trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;207(2):131–137. doi:10.1016/j.ajog.2012.05.021
11. Xu Y, Wei Y, Ming J, et al. Cost-effectiveness analysis of non-invasive prenatal testing for Down syndrome in China. Int J Technol Assess Health Care. 2019;35(3):237–242. doi:10.1017/S0266462319000308
12. Renga B. Non invasive prenatal diagnosis of fetal aneuploidy using cell free fetal DNA. Eur J Obstet Gynecol Reprod Biol. 2018;225:5–8. doi:10.1016/j.ejogrb.2018.03.033
13. Jun M, Thongpriwan V, Choi KS. Experiences of prenatal genetic screening and diagnostic testing among pregnant Korean women of advanced maternal age. J Transcult Nurs. 2017;28(6):550–557. doi:10.1177/1043659616662913
14. Muller C, Cameron LD. It’s complicated – factors predicting decisional conflict in prenatal diagnostic testing. Health Expect. 2016;19(2):388–402. doi:10.1111/hex.12363
15. Hartwig TS, Borregaard MC, Malmgren CI, Tabor A, Jørgensen FS. High risk – what’s next? A survey study on decisional conflict, regret, and satisfaction among high-risk pregnant women making choices about further prenatal testing for fetal aneuploidy. Prenat Diagn. 2019;39(8):635–642. doi:10.1002/pd.5476
16. Berger AM, Buzalko RJ, Kupzyk KA, Gardner BJ, Djalilova DM, Otte JL. Preferences and actual chemotherapy decision-making in the greater plains collaborative breast cancer study. Acta Oncol. 2017;56(12):1690–1697. doi:10.1080/0284186X.2017.1374555
17. Hickman RJ, Daly BJ, Lee E. Decisional conflict and regret: consequences of surrogate decision making for the chronically critically ill. Appl Nurs Res. 2012;25(4):271–275. doi:10.1016/j.apnr.2011.03.003
18. Lo TK, Chan KY, Kan AS, et al. Decision outcomes in women offered noninvasive prenatal test (NIPT) for positive Down screening results. J Matern Fetal Neonatal Med. 2019;32(2):348–350. doi:10.1080/14767058.2017.1378323
19. Riffin C, Pillemer K, Reid MC, Tung J, Ckenhoff L. Decision support for joint replacement: implications for decisional conflict and willingness to undergo surgery. J Gerontol B Psychol Sci Soc Sci. 2018;73(3):387–398. doi:10.1093/geronb/gbw023
20. Lee J, Jung D, Choi M. Relationship of social support and decisional conflict to advance directives attitude in Korean older adults: a community-based cross-sectional study. Jpn J Nurs Sci. 2016;13(1):29–37. doi:10.1111/jjns.12081
21. Garvelink MM, Boland L, Klein K, et al. Decisional conflict scale use over 20 years: the anniversary review. Med Decis Making. 2019;39(4):301–314. doi:10.1177/0272989X19851345
22. Lam WW, Kwok M, Liao Q, et al. Psychometric assessment of the Chinese version of the decisional conflict scale in Chinese women making decision for breast cancer surgery. Health Expect. 2015;18(2):210–220. doi:10.1111/hex.12021
23. Koedoot N, Molenaar S, Oosterveld P, et al. The decisional conflict scale: further validation in two samples of Dutch oncology patients. Patient Educ Couns. 2001;45(3):187–193. doi:10.1016/S0738-3991(01)00120-3
24. Kawaguchi T, Azuma K, Yamaguchi T, et al. Development and validation of the Japanese version of the decisional conflict scale to investigate the value of pharmacists’ information: a before and after study. BMC Med Inform Decis Mak. 2013;13(1):50. doi:10.1186/1472-6947-13-50
25. Légaré F, Stacey D, Turcotte S, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2014;2014(9):D6732.
26. Bryant FB, Yarnold PR. Principal components analysis and exploratory and confirmatory factor analysis. In: Grimm LG, Yarnold RR, editors. Reading and Understanding Multivariate Statistics. Washington, DC: American Psychological Association; 1995:99–136.
27. Gorsuch RL. Factor Analysis.
28. Devellis RF. Scale Development: Theory and Application.
29. O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi:10.1177/0272989X9501500105
30. O’Connor AM. User manual-decisional conflict scale; 2021. Available from: https://decisionaid.ohri.ca/eval_dcs.html.
31. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi:10.1016/S0033-3182(71)71479-0
32. Zung WW. The measurement of affects: depression and anxiety. Mod Probl Pharmacopsychiatry. 1974;7:170–188.
33. Gao L, Qu J, Wang AY. Anxiety, depression and social support in pregnant women with a history of recurrent miscarriage: a cross-sectional study. J Reprod Infant Psychol. 2020;38(5):497–508. doi:10.1080/02646838.2019.1652730
34. Zhang Y, Muyiduli X, Wang S, et al. Prevalence and relevant factors of anxiety and depression among pregnant women in a cohort study from south-east China. J Reprod Infant Psychol. 2018;36(5):519–529. doi:10.1080/02646838.2018.1492098
35. Xiao SY. Theoretical basis and application in research of social support rating scale. J Clin Psychiatry. 1994;4(2):98–100.
36. Yue C, Liu C, Wang J, et al. Association between social support and anxiety among pregnant women in the third trimester during the coronavirus disease 2019 (COVID-19) epidemic in Qingdao, China: the mediating effect of risk perception. Int J Soc Psychiatry. 2021;67(2):120–127. doi:10.1177/0020764020941567
37. Clayton MF, Pett MA. AMOS versus LISREL: one data set, two analyses. Nurs Res. 2008;57(4):283–292. doi:10.1097/01.NNR.0000313487.64412.be
38. Guangzhou Statistic Bureau. Average annual income of non-private and private employees in Urban areas of Guangzhou in 2020; 2021. Available from: http://tjj.gz.gov.cn/tjgb/qtgb/content/post_7319136.html.
39. Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–385. doi:10.1097/00006199-198611000-00017
40. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–575. doi:10.1111/j.1744-6570.1975.tb01393.x
41. Stevens JP. Applied Multivariate Statistics for the Social Sciences.
42. Kong X, Ai B, Kong Y, et al. Artificial intelligence: a key to relieve China’s insufficient and unequally-distributed medical resources. Am J Transl Res. 2019;11(5):2632–2640.
43. Sim JA, Shin JS, Park SM, et al. Association between information provision and decisional conflict in cancer patients. Ann Oncol. 2015;26(9):1974–1980. doi:10.1093/annonc/mdv275
44. Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):D1431.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
