Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Psoriasis and COVID-19 Infection Negatively Impact Each Other: An Analysis of 3581 Cases
Authors Wang X, Yuan L, Qiu X, Yang B, Man MQ
Received 15 May 2023
Accepted for publication 19 July 2023
Published 25 July 2023 Volume 2023:16 Pages 1933—1936
DOI https://doi.org/10.2147/CCID.S421394
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Xiaohua Wang,* Liyan Yuan,* Xiaoyu Qiu, Bin Yang, Mao-Qiang Man
Dermatology Hospital, Southern Medical University, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Mao-Qiang Man; Bin Yang, Dermatology Hospital, Southern Medical University, No. 2 Lujing Road, Guangzhou, 510095, People’s Republic of China, Tel +86-20-87255286, Email [email protected]; [email protected]
Objective: To determine whether COVID-19 infection and psoriasis impact each other.
Methods: WeChat app was used to carry out a questionnaire survey in individuals aged 18 years and over.
Results: A total of 3581 individuals, including 2515 individuals without psoriasis and 1066 psoriatic patients completed the survey. The rate of COVID-19 infection was significantly higher in psoriatic patients than in those without psoriasis (89.59% vs 77.93%, p < 0.0001). Moreover, the rate of relapse and/or worsening of psoriasis was higher in psoriatic patients with COVID-19 infection than in that without COVID-19 infection (75.29% vs 47.75%, p < 0.0001).
Conclusion: COVID-19 infection and psoriasis negatively impact each other.
Keywords: COVID-19, psoriasis, infection
Introduction
Psoriasis, an immune-mediated inflammatory dermatosis, can be triggered or exacerbated by a variety of factors, including infections and psychological stress.1,2 COVID-19 infection can dramatically impact mental health, with up to 35% of individuals with COVID-19 infection exhibiting depression and anxiety,3 whereas psoriasis can also increase the risk of infections.4 Whether COVID-19 infection and psoriasis impact each other is not clear yet. Here, we compared the incidence and symptoms of COVID-19 infection in individuals with vs without psoriasis.
Materials and Methods
WeChat app was used to carry out questionnaire survey in individuals aged ≥18 years old from January 17 to February 4, 2023. COVID-19 infection rates were compared between individuals with and without psoriasis. Moreover, the rates of psoriasis worsening and relapse were compared in psoriatic subjects with vs without COVID-19 infection. Either Chi square or Fisher exact test was applied to assess the significance between the qualitative data, while unpaired student test was used to determine the significance between the quantitative data. The protocol of this survey was reviewed and approved by Institutional Review Board of Dermatology Hospital of Southern Medical University (#2023020). And this work was carried out in accordance with Declaration of Helsinki.
Results
Out of 5748 individuals who clicked the questionnaire link, 3581 individuals, including 2515 individuals without psoriasis and 1066 psoriatic patients, completed the questionnaire. Overall, the subjects’ age was comparable between individuals with or without psoriasis (Table 1). Neither age nor overall BMI differed significantly in psoriatic patients with vs without COVID-19 infection (age: 48.23 ± 0.59 vs 48.14 ± 1.67; BMI: 22.32 ± 0.12 vs 21.97 ± 0.36). The rates of COVID-19 infection were similar between males and females in individuals with or without psoriasis. However, the incidence of COVID-19 infection was significantly higher in individuals with psoriasis than in those without psoriasis (89.59% vs 77.93%, p<0.0001) although the rate of COVID-19 vaccination did not differ between psoriatic patients and non-psoriatic individuals (88.09% vs 86.72%). Proportions of individuals with lower fever, coughing and headache were lower in psoriatic patients than in non-psoriatic individuals after COVID-19 infection. In contrast, more psoriatic patients had high fever and shortness of breath than non-psoriatic individuals did (Table 2). Moreover, 47.75% (53/111) of psoriatic patients without COVID-19 infection experienced relapse and/or worsening of psoriasis, while 75.29% (719/955) of psoriatic patients with COVID-19 infection claimed relapse and/or worsening of psoriasis, with relative risk of 1.577 (95% CI 1.136–1.952) (p<0.0001) (Table 3). The overall rates of receiving biologics were comparable in psoriatic patients with vs without COVID-19 infection (74.97% vs 75.68%). The proportion of subjects receiving anti-IL-23 antibody was slightly higher in psoriatic patients without COVID-19 infection than those with COVID-19 infection (3.60% vs 1.05%, p=0.0490). Collectively, these results demonstrate that psoriasis predisposes the risk for COVID-19 infection while COVID-19 infection exacerbates psoriasis.
 |
Table 1 Demographic Characteristics of Subjects |
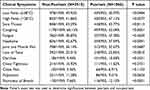 |
Table 2 Characterization of COVID Infection in Subjects with vs without Psoriasis |
 |
Table 3 Comparison of Psoriatic Individuals with vs without COVID Infection |
Discussion
Previous study suggested a risk of psoriasis for COVID-19 infection.4 Correspondingly, we showed here that the incidence of COVID-19 infection was higher in psoriatic patients than in non-psoriatic individuals, consistent with previous finding that psoriasis increases risk for infections.5 Although anti-IL-17 antibody can possibly lower the risk for COVID-19 infection,6 the rates of COVID-19 infection were similar between psoriatic patients with vs without IL-17a treatment, consistent with findings by the others.7 The higher incidence of COVID-19 infection in psoriatic patients is unlikely due to the use of anti-TNFα antibody, a risk factor for infections,8 because proportion of patients who used anti-TNFα antibody did not differ between individuals with and without COVID-19 infection (24.44% vs 26.13%). These results are consistent with previous studies.9 Although a study showed that COVID-infection is not a risk factor for exacerbation of psoriasis,10 other studies revealed that either COVID-infection or COVID-19 vaccination induces new-onset or flares of psoriasis in both adults and children.11–13 Likewise, the present study demonstrates exacerbation of psoriasis by COVID-19 infection. The exacerbation of psoriasis can be attributable to COVID-19 induced production of IL-17 and IL-23,4,14 key cytokines in the pathogenesis of psoriasis. Moreover, COVID-19 infection increases the number of circulating neutrophils, and cytokines and chemokines,15 leading to relapse or exacerbation of psoriasis. Furthermore, COVID-19 infection can induce psychological stress, which is a known trigger factor for psoriasis. Especially, the COVID-zero policy isolated individuals infected with COVID-19 and those contacted with COVID-positive individuals, making them subject to extra psychological stress. Thus, COVID-19 infection-induced inflammation and psychological stress can contribute to relapse and exacerbation of psoriasis. Collectively, the present study clearly demonstrated that psoriasis and COVID-19 infection negatively impact each other. Biologics do not increase risk for COVID-19 infection. In contrast, biologics are effective for psoriatic patients with COVID-19 infection.10,12,16
In summary, psoriasis and COVID-19 infection affect each other. Successful management of one condition could possibly benefit the other one. The underlying mechanisms by which psoriasis and COVID-19 infection negatively impact each other remain to be determined.
Data Sharing Statement
All data are available from the Xiaohua Wang ([email protected]) upon reasonable request, with privacy restriction.
Ethics Statement
This work was reviewed and approved by ethics committee of Dermatology Hospital, Southern Medical University (#2023020).
Informed Consent
Written informed consent was obtained from all participants.
Funding
There is no funding to report.
Disclosure
The authors have no conflicts of interest.
References
1. Zhou S, Yao Z. Roles of infection in psoriasis. Int J Mol Sci. 2022;23(13):6955. doi:10.3390/ijms23136955
2. Yang H, Zheng J. Influence of stress on the development of psoriasis. Clin Exp Dermatol. 2020;45(3):284–288. doi:10.1111/ced.14105
3. Penninx BW, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. 2022;28(10):2027–2037. doi:10.1038/s41591-022-02028-2
4. De Simone C, Fargnoli MC, Amerio P, et al. Risk of infections in psoriasis: assessment and challenges in daily management. Expert Rev Clin Immunol. 2021;17(11):1211–1220. doi:10.1080/1744666X.2021.1997592
5. Loft N, Skov L, Richardson C, Trivedi V, Alarcon I, Egeberg A. A nationwide population‐based cohort study of the incidence of severe and rare infections among adults with psoriasis in Denmark. Br J Dermatol. 2022;187(3):353–363. doi:10.1111/bjd.21595
6. Peng G, Okumura K, Ogawa H, Ikeda S, Niyonsaba F. Psoriatic lesional expression of SARS-CoV-2 receptor ACE2 is reduced by blockade of IL-17 signaling but not by other biologic treatments. J Am Acad Dermatol. 2022;87(3):714–715. doi:10.1016/j.jaad.2022.01.041
7. Kridin K, Schonmann Y, Solomon A, et al. Risk of COVID-19 infection, hospitalization, and mortality in patients with psoriasis treated by interleukin-17 inhibitors. J Dermatolog Treat. 2022;33(4):2014–2020. doi:10.1080/09546634.2021.1905766
8. Scheinfeld N. Adalimumab: a review of side effects. Expert Opin Drug Saf. 2005;4(4):637–641. doi:10.1517/14740338.4.4.637
9. Jones ME, Kohn AH, Pourali SP, et al. The use of biologics during the COVID-19 pandemic. Dermatol Clin. 2021;39(4):545–553. doi:10.1016/j.det.2021.05.010
10. Topaloğlu Demir F, Polat Ekinci A, Aytekin S, et al. Clinical course of psoriasis patients that discontinued biologics during the COVID-19 pandemic. J Cosmet Dermatol. 2023;22(3):722–731. doi:10.1111/jocd.15638
11. Shah H, Busquets AC. Psoriasis flares in patients with COVID-19 infection or vaccination: a case series. Cureus. 2022;14(6):e25987. doi:10.7759/cureus.25987
12. Zitouni J, Bursztejn AC, Belloni Fortina A, et al. Children with psoriasis and COVID-19: factors associated with an unfavourable COVID-19 course, and the impact of infection on disease progression (Chi-PsoCov registry). J Eur Acad Dermatol Venereol. 2022;36(11):2076–2086. doi:10.1111/jdv.18361
13. Ständer S, Zirpel H, Bujoreanu F, Tatu AL, Ludwig RJ, Thaçi D. Case report: clinical features of COVID-19 vaccine-induced exacerbation of psoriasis-a case series and mini review. Front Med. 2022;9:995150. doi:10.3389/fmed.2022.995150
14. Ling Y, Puel A. IL-17 and infections. Actas Dermosifiliogr. 2014;105(Suppl 1):34–40. doi:10.1016/S0001-7310(14)70016-X
15. Schett G, Sticherling M, Neurath MF. COVID-19: risk for cytokine targeting in chronic inflammatory diseases? Nat Rev Immunol. 2020;20:271–272. doi:10.1038/s41577-020-0312-7
16. Gargiulo L, Ibba L, Vignoli CA, et al. New-onset and flares of psoriasis after COVID-19 infection or vaccination successfully treated with biologics: a case series. J Dermatolog Treat. 2023;34(1):2198050. doi:10.1080/09546634.2023.2198050
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
