Back to Journals » Clinical Ophthalmology » Volume 13
Prospective randomized comparative study between venturi and peristaltic pumps in WhiteStar Signature® phacoemulsification machine
Authors Hida WT , de Medeiros AL, de Araujo Rolim AG, Motta AFP, Kniggendorf DV, de Queiroz RLF, Chaves MAPD , Carricondo PC , Nakano CT, Nosé W
Received 22 June 2018
Accepted for publication 14 September 2018
Published 27 December 2018 Volume 2019:13 Pages 49—52
DOI https://doi.org/10.2147/OPTH.S177978
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wilson Takashi Hida,1–3 André Lins de Medeiros,1,2 André Gustavo de Araújo Rolim,1,2 Antonio Francisco Pimenta Motta,2,3 Danilo Varela Kniggendorf,1,2 Rodrigo Lafetá Franco de Queiroz,1,2 Mário Augusto Pereira Dias Chaves,1,2 Pedro Carlos Carricondo,1,2 Celso Takashi Nakano,2,4 Walton Nosé5
1Cataract Sector, Hospital Oftalmológico de Brasília, Brasília, Federal District, Brazil; 2Cataract Sector, Centro de Estudos Oftalmológicos Renato Ambrósio, Brasília, Brazil; 3Cataract Sector, Universidade de São Paulo, São Paulo, Brazil; 4Cataract Sector, Hospital Santa Cruz, São Paulo, Brazil; 5Cataract Sector, Universidade Federal de São Paulo, São Paulo, Brazil
Purpose: To compare intraoperative parameters between venturi and peristaltic pump in WhiteStar Signature® phacoemulsification machine using the bevel-down technique.
Setting: Hospital Oftalmológico de Brasília, Brasília, Federal District, Brazil.
Design: Prospective, comparative, patient-masked study.
Methods: Three hundred eyes were randomly assigned to have a phacoemulsification procedure with WhiteStar Signature® using either peristaltic (n=150 eyes) or venturi (n=150 eyes) pumps by a single surgeon (WTH). Elliptical ultrasound setting and prefracture (prechop or preslice) techniques were used in all cases. Cataract nucleus density was graded using lens opacities classification system III and Pentacam Nucleus Staging classification. Clinical measurements included preoperative- and postoperative- corrected visual acuity, preoperative and 2-month postoperative endothelial cell counts, and preoperative and 1-day postoperative central corneal thickness. Intraoperative measurements at the end of the case were phaco time, fluid used, total case time, and Efx energy.
Results: There were no statistically significant differences between groups regarding age, cataract density, and phaco time (P>0.05). Intraoperatively, we observed significantly less ultrasound energy (P=0.011), case time (P=0.0001), and balanced saline solution (P=0.001) usage in the venturi group. Clinically, both fluidic settings can provide similar clinical outcomes and visual recovery, regarding corrected distance visual acuity, endothelial cell count, and central corneal thickness.
Conclusion: Our data show that to minimize fluid use, case time, and energy with the prefracture technique, the venturi pump was the most efficient system and was statistically superior to peristaltic pump.
Keywords: venturi, peristaltic, phacoemulsification, cataract surgery, vacuum efficiency
Introduction
Phacoemulsification is the preferred technique for cataract surgery worldwide.1 Surgical efficiency may vary depending on the surgeon’s skills and the machine settings. A good clinical outcome utterly depends on the combination of both.2–4
Some studies have shown that change in one single parameter can significantly alter the nucleus emulsification. Fluidics is a key factor to achieve good surgical efficiency, as it will determine how fragments will move toward the phaco-tip for emulsification. Phaco-machine pumps work mainly on two different ways to control fluidics: flow-based (or peristaltic) and vacuum-based (or venturi).5,6
Peristaltic pumps use rollers to create flow by compressing the tube and moving the fluid in one direction. Vacuum is formed depending on flow restriction, and the maximum preset vacuum levels can only be achieved with full occlusion of the tip. Venturi pumps use vacuum to create flow. Therefore, no tip occlusion is necessary to achieve high vacuum levels. Experimental studies have already demonstrated superior efficiency of vacuum-based over flow-based pumps depending on the vacuum levels and nucleus density.5 However, there is a lack of clinical studies to demonstrate these data.
The WhiteStar Signature® (J&J Vision, Santa Ana, CA, USA) is capable of operating with either venturi or peristaltic pumps depending on the surgeon prefer and machine configuration. The two pumps coexist in the same cassette and can be switched on the fly.5
The purpose of this study was to compare intraoperative parameters in phacoemulsification using either venturi or peristaltic pumps.
Methods
This study was approved by the institutional review board of University of São Paulo, Brazil and complied with the ethical principles of the Declaration of Helsinki. All patients signed informed consent before the surgery.
It was a prospective, comparative, patient-masked study. Three hundred eyes were randomly and consecutively assigned to have phacoemulsification with WhiteStar Signature® using either peristaltic (n=150 eyes) or venturi (n=150 eyes) pumps by a single surgeon (WTH), between February 2011 and February 2012.
The surgical technique was also equal in all cases. After a 2.4 mm clear cornea incision positioned on the steepest axis, dispersive and cohesive viscoelastic material were delivered inside the anterior chamber in a soft-shell technique. Continuous curvilinear capsulorrhexis was made with forceps, followed by hydrodissection and hydrodelineation. A prefracture (prechop or preslice) technique was used in all cases, followed by phacoemulsification with a bevel-down technique. Elliptical ultrasonic modulation was used with the Ellips FX handpiece (Abbot Medical Optics, Inc.). For the peristaltic group, the flow rate was set at 45 cm3/min when unoccluded and 55 cm3/min when occluded by a nucleus fragment. Maximum vacuum level were set at 450 mmHg when unoccluded and 400 mmHg when occluded for peristaltic and 350 mmHg for venturi.
Clinical measurements included preoperative and 3-month postoperative corrected visual acuity (CDVA), preoperative and 3-month postoperative endothelial cell counts (ECC), and preoperative and 1-day postoperative central corneal thickness (CCT). Cataract nucleus density was graded using lens opacities classification system III and Pentacam Nucleus Staging classification. Intraoperative measurements at the end of phacoemulsification were phaco time, aspiration time, fluid used, case time, Efx energy, and infusion fluid use.
All data were gathered on an Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet, and statistical analysis was performed using SPSS for Windows (Microsoft Corporation); significance was tested using the Tukey, Wilcoxon, Kruskal–Wallis, analysis of variance, and chi-squared tests by adjusting to a level of significance of 5% (P<0.05).
Results
There were no intraoperative complications. Groups were statistically equivalent in age and cataract density (Table 1).
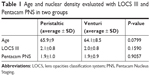  | Table 1 Age and nuclear density evaluated with LOCS III and Pentacam PNS in two groups |
Total ultrasound (US) time and average US power were not statistically different between groups (Table 2). Venturi group presented less elliptical Efx energy, BSS usage, and total case time than the peristaltic group (Figures 1–3). There was no statistical significance regarding visual acuity, ECC, and CCT. Median preoperative CCT (preCCT) was 535.12 μm and 1-day postoperative CCT (postCCT) was 576.34 μm in the peristaltic group; in the venturi group, the preCCT was 541.14 μm and the postCCT was 568.45 μm. Regarding the median preoperative ECC (preECC), the peristaltic group had a value of 2,572.06, while it was 2,578.77 in the venturi group; the postoperative ECC (postECC) was 2,413.52 and 2,434.70, respectively. The median preoperative CDVA (preCDVA) was 0.3630 logMAR in the peristaltic group, while in the venturi group it was 0.365 logMAR;e the postoperative CDVA was 0.0271 logMAR and 0.0281 logMAR, respectively.
  | Table 2 Elliptical Efx time and average US power compared between two groups |
  | Figure 1 Comparison of elliptical Efx energy between peristaltic and venturi pump in Signature phacoemulsification machine. |
  | Figure 2 Comparison of fluid usage time in cubic centimeters (cm3) between peristaltic and venturi pump in Signature phacoemulsification machine. |
  | Figure 3 Comparison case time in minutes between peristaltic and venturi pumps in Signature phacoemulsification machine. |
Discussion
Despite the recent technological advances in cataract surgery, such as femtosecond platforms and improved anterior chamber stability with mitigating postvacuum surge, US energy for phacoemulsification is still necessary, mainly in moderate and harder nucleus. One should strive to use as less US energy as possible as it can cause damage to adjacent structures if used carelessly.7–9
Preslice and prechop techniques use US-free maneuvers to divide the nucleus into quadrants, therefore lowering US energy delivered inside the anterior chamber. The bevel-down tip approach demonstrated increase phacoemulsification speed and followability, with the benefit of directing the energy away from the cornea. Combining both strategies may result in a more endothelial friendly procedure.3,9,10 All surgeries in both groups were performed using these combined techniques (prechop or preslice and bevel-down phacoemulsification) by the same surgeon, therefore avoiding bias regarding surgical technique. If the same phaco machine is used, a peristaltic pump could mimic the high flow rate of venturi with the same maximum vacuum, and the vacuum at the peristaltic tip without occlusion would be the same for both systems; so, they would function exactly the same.
Our results suggest that venturi pump is more efficient than the peristaltic, considering less total US use, case time, and fluid usage. Cahoon et al5 showed in experimental models that the vacuum-based system is more efficient at lower vacuum levels and reduces chattering even with US linear power at 100% at all vacuum levels, compared to the flow-based system. In our study, the maximum vacuum level for both groups was set considerably high, according to the surgeon’s preference. Therefore, we believe that we have confirmed the in vitro study results.5
There were no surgical complications, and we believe that the two pump configurations are equally safe when an experienced surgeon performs the procedure. Other experimental and clinical papers in the literature have confirmed these findings.5,11,12
Karaguzel et al12 compared venturi and peristaltic pumps in bimanual microincision cataract surgery, with sleeveless tips, using two different phacoemulsification machines. They found venturi pump to be more efficient, safer, and less prone to create surge and thermal burns. Although using different technique and machines, the results were similar to our study.12
Patrício et al11 compared venturi and peristaltic pumps with different nucleus density. They found no differences of US energy usage between the pump modes for any given Pentacam Nucleus Staging, but a shorter case time with venturi mode in denser nucleus. In our study, there was no statistical significance in nuclear density between groups, with the venturi mode evidencing better overall performance.11
Conclusion
Our data shows that the venturi mode excels peristaltic mode in WhiteStar Signature® in surgical efficiency and that both are equally safe when used by experienced surgeons. The surgeon must adjust surgical parameters according to his preference, technique, and skills.
Disclosure
The authors report no conflicts of interest in this work.
References
Vision 2020: the cataract challenge. Community Eye Health Int Cent Eye Health. 2000;13(34):17–19. | ||
Christakis PG, Braga-Mele RM. Intraoperative performance and postoperative outcome comparison of longitudinal, torsional, and transversal phacoemulsification machines. J Cataract Refract Surg. 2012;38(2):234–241. | ||
Park J, Yum HR, Kim MS, Harrison AR, Kim EC. Comparison of phaco-chop, divide-and-conquer, and stop-and-chop phaco techniques in microincision coaxial cataract surgery. J Cataract Refract Surg. 2013;39(10):1463–1469. | ||
Georgescu D, Kuo AF, Kinard KI, Olson RJ. A fluidics comparison of Alcon Infiniti, Bausch & Lomb Stellaris, and Advanced Medical Optics Signature phacoemulsification machines. Am J Ophthalmol. 2008;145(6):1014–1017. | ||
Cahoon JM, Gupta I, Gardiner G, et al. Comparison of venturi and peristaltic vacuum in phacoemulsification. J Cataract Refract Surg. 2015;41(2):428–432. | ||
Sharif-Kashani P, Fanney D, Injev V. Comparison of occlusion break responses and vacuum rise times of phacoemulsification systems. BMC Ophthalmol. 2014;14:96. | ||
Baradaran-Rafii A, Rahmati-Kamel M, Eslani M, Kiavash V, Karimian F. Effect of hydrodynamic parameters on corneal endothelial cell loss after phacoemulsification. J Cataract Refract Surg. 2009;35(4):732–737. | ||
Han YK, Miller KM. Heat production: longitudinal versus torsional phacoemulsification. J Cataract Refract Surg. 2009;35(10):1799–1805. | ||
Pereira AC, Porfírio F, Freitas LL, Belfort R. Ultrasound energy and endothelial cell loss with stop-and-chop and nuclear preslice phacoemulsification. J Cataract Refract Surg. 2006;32(10):1661–1666. | ||
Fine IH. Advantages of bevel-down technique. J Cataract Refract Surg. 2012;38(5):925–926. | ||
Patrício MS, Almeida AC, Rodrigues MP, Guedes ME, Ferreira TB. Correlation between cataract grading by Scheimpflug imaging and phaco time in phacoemulsification using peristaltic and venturi pumps. Eur J Ophthalmol. 2013;23(6):789–792. | ||
Karaguzel H, Karalezli A, Aslan BS. Comparison of peristaltic and Venturi pumps in bimanual microincisional cataract surgery. Int Ophthalmol. 2009;29(6):471–475. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
