Back to Journals » Risk Management and Healthcare Policy » Volume 11
Progress and challenges in improving maternal health in the Tibet Autonomous Region, China
Authors Labasangzhu , Bjertness E , McNeil EB , Deji, Guo Y, Songwathana P , Chongsuvivatwong V
Received 8 April 2018
Accepted for publication 11 July 2018
Published 14 November 2018 Volume 2018:11 Pages 221—231
DOI https://doi.org/10.2147/RMHP.S170445
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kent Rondeau
Labasangzhu,1,2 E Bjertness,3 EB McNeil,2 Deji,1 Y Guo,4 P Songwathana,5 V Chongsuvivatwong2
1Department of Preventive Medicine, Tibet University Medical College, Lhasa, Tibet, China; 2Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Hatyai, Songkhla, Thailand; 3Department of Community Medicine and Global Health, Institute of Health and Society, University of Oslo, Oslo, Norway; 4Department of Health Policies and Management, School of Public Health, Peking University Health and Science Center, Beijing, China; 5Department of Adult and Elderly Nursing, Faculty of Nursing, Prince of Songkla University, Hatyai, Songkhla, Thailand
Background: The maternal mortality ratio (MMR) of the Tibet Autonomous Region (hereinafter “Tibet”) is still five times higher than the national average. This study aims to identify the successes and pitfalls of the health system that might be related to the high mortality rate based on the WHO health system building blocks, focusing on human resources for health and health infrastructure and the impact on maternal health and outcomes.
Methods: Sources of information include China’s central government and Tibet’s local government policies and regulations, health statistical yearbooks, maternal and child health routine reporting system, and English and Chinese online research articles. Joinpoint analysis was applied for MMR and maternal health service trends, and correlation test was used to test the relationship between maternal health services and outcomes.
Results: Between 2000 and 2015, public health spending in Tibet increased 67-fold, the hospital delivery rate increased 70.1%, and the MMR dropped from 466.9 to 100.1 per 100,000 live births. However, the total number of health workers, qualified medical doctors, and registered nurses per 1,000 people were 4.4, 1.4, and 1.0, respectively, much lower than the national average (5.8, 1.8, and 2.4). In Tibet, there were 80 basic and 16 comprehensive emergency obstetric care (EOC) centers. On average, there were 12 basic and 2.5 comprehensive EOC centers per 500,000 of the population. Though it met the WHO’s recommendation, it might remain inadequate in the low population density of the area like Tibet.
Conclusion: The shortage of health professionals and EOC centers and health information in predominantly remote rural areas with a scattered population still needs to be rectified.
Keywords: health system, human resources for health, emergency obstetric care, Tibet
Introduction
Globally, about 1.15 women die every two minutes due to preventable pregnancy-related causes, and many suffer health problems in connection with pregnancy and birth.1 In 2016, China released a national plan on implementation of the Sustainable Development Goals. The plan aims to reduce maternal mortality ratio (MMR) to less than 12 per 100,000 live births by 2030;2 this goal cannot be achieved without improving health services in all remote areas including Tibet.3
Tibet constitutes the main part of the Tibetan plateau in south-west China. It is predominantly rural, with a scattered population estimated at 3.23 million people4 residing in remote areas (more details in Table S1). In 2015, Tibet’s MMR per 100,000 live births was 100.1, five times higher than the national average,5 much higher than neighboring provinces such as Xinjiang and Qinghai (Figure 1). Moreover, rebounds often happen in Tibet’s MMR trend, as seen in 2007 and 2011. It was reported that the MMR increased to 114.92 per 100,000 live births in 2017,6 which might indicate the weakness of the health system in providing continuing health service.
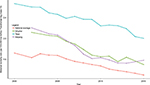  | Figure 1 Maternal mortality in Tibet, Xinjiang Autonomous Region, Qinghai province, and the national average between 2000 and 2015. |
Postpartum hemorrhage and maternal hypertensive disorder are the two major causes of maternal death in Tibet, followed by amniotic fluid embolism.7,8 Therefore, achievement of high coverage of maternal health service (MHS) is the main strategy to reduce MMR.9,10 To that end, the hospital delivery subsidy program was introduced in 2006 by both the government of central China and Tibet11 and revised in 2012 to have total fee exemption, transportation, and cash subsidies for rural residents.12 Consequently, the hospital delivery rate increased by about 52% over a decade (2006–2015);13,14 the MMR reduced over this period but has not substantially decreased further. The aim of this study was to identify pitfalls in the health system and describe the progress of maternal health care between 2000 and 2015, focusing on human resources for health (HRH) and health infrastructure and the impact on maternal health and outcomes.
Methods
This study applied an impact-based health system evaluation framework used in countdown case studies15–18 and WHO’s health system six building blocks for a review of the health system19 (see Figure S1). Health system was reviewed with emphasis on maternal health policy, service package and organization, HRH, health facility and infrastructure, health information, health finance, and progress of maternal health between 2000 and 2015. Joinpoint analysis (Joinpoint Regression Program, version 4.5.0.1 - June 2017; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute) was applied to document the progress of maternal health outcome and tendency.20 Pearson correlation coefficient was used to test the relationship between MMR, hospital delivery rate, antenatal care (ANC), and postpartum visit (PPV) coverage.
Sources of information included government policy announcements, health-related laws and regulations pertaining to the health system and governance, National Health Statistical Yearbooks (2001–2016), and Tibet’s Health Statistics (2013), which cover the whole of Tibet reflecting changing trend in maternal health indices and health expenditure. Online databases were also utilized including PubMed and China National Knowledge Infrastructure for all original research articles (English or Chinese) published between January 1, 2000, and December 31, 2017, using the search term “([maternal health]) AND (Tibet or Tibetan)”. All data access was freely available, and this study was approved by the Ethical Review Committee of the Faculty of Medicine, Prince of Songkla University, Hatyai, Thailand (REC number: 58-314-18-5).
The results and discussion of the study are detailed below.
Results and discussion
The maternal health organization and governance
Administration and governance
Similar to the national health administration structure, under the National Health and Family Planning Commission (NHFPC), Tibet’s health administration is a three-level hierarchy: Tibet’s Health and Family Planning Commission (HFPC) is at the top, followed by prefecture (city), and the county (district) HFPC. The HFPC at each level has a maternal and child health (MCH) service and family planning division as the main MCH policy maker and administrator. Township health care centers and village clinics are under county (district) HFPC and township governments’ administration. The Working Committee for Women and Child and the Women’s Federation as independent government sections work closely with HFPC in terms of MCH care and oversee MCH-related work. The Tibet Maternal and Child Association and other stakeholders, such as nongovernmental bodies, are also invited to participate in MCH policy making and talent training programs.21
All government sections are included in the campaign to reduce the MMR. Particularly in rural areas, advocating hospital childbirth and sending near-to-labor pregnant women to hospital have been a daily duty of village cadres since 2015. If childbirth and maternal death happen at home, it will be the direct responsibility of the village cadres.22
MHS organization
Following the national system, Tibet’s current MHS delivery is a five-tier hierarchy. As shown in Figure S2, regional tertiary referral hospitals are at the top. Each prefecture or city has its own MCH hospital and a comprehensive western medical hospital (People’s Hospital, PH) with an obstetrics and gynecology (O&G) section. These act as secondary referral health care facilities. Accordingly, at the third level, each county (district) also has its own PH and MCH station. County, township, and village health facilities, a three-tier primary health care network, are the third to fifth level of the health system. Due to geographic inaccessibility, township health care centers play the role of a multifunctional service center for first MHS visits. At the county level, with a serious shortage of trained personnel, similar types of service are shared among the county PH, Traditional Tibetan Medicine (TTM) hospital, Center for Disease control (CDC), MCH, and family planning section, all these facilities have been set up in a so-called “4 in 1” health service center since the late 1980s.23 The county health service center provides first referral service for rural communities including childbirth service. Nevertheless, there is no strict gatekeeper system between the different levels of hospitals.24 Pregnant women and their family often bypass the primary care center for the referral hospital, particularly for childbirth. The most common reason is that they perceive a poor quality of service at primary care centers, and they are expecting a higher level of health worker competency at the referral hospital. Besides government-run health facilities, there are private hospitals also providing basic obstetric services in major cities.
Maternal health policy
China promulgated its first national law on MCH in 1994.25 Subsequently, interventions to improve MCH have been included in the national economic and social development plan since then. Tibet adapted the national law on MCH later with an emphasis on hospital delivery and medical birth attendance in rural areas. Since 1996, Tibet has launched four rounds of Women’s Development Plans,26 with maternal health as one of the main parts. These plans aimed to raise the hospital delivery rate, reduce MMR, and improve obstetrics care quality. The most recent Tibet women’s development plan was released in 2017 aimed at an MMR reduction to 80 per 100,000 live births and a hospital delivery above 95% by 2020.
Overall, a top-down, multidimensional, integrated safe motherhood policy is currently in practice in Tibet. However, the acceptability, accessibility, and adaptability of this health system policy have rarely been studied.
Health workforce and training system
Planning and distribution
In 2015, Tibet had 29,094 health workers in total.5 Among them, 49.3% (14,341) were health professionals: 6,213 qualified medical doctors (including physician assistants), 3,190 registered nurses, 636 pharmaceutists, 627 technicians, and 3,675 not holding any qualified certification. As shown in Table 1, the total number of rural health workers, qualified medical doctors (including physician assistants), qualified medical doctors only, and registered nurses per 1,000 people were much lower than national average and all indices lower than neighboring provinces such as Qinghai and Xinjiang.5 Tibetan government aims to have an average number of HRH per 1,000 people equal to national average by 2020.27
  | Table 1 Comparison of human resources for health Note: “–” Data were not available. Abbreviations: HRDI, Health Resource Density Index; TAR, Tibet Autonomous Region. |
The disparity is much bigger within Tibet: the number of health workers per 1,000 people in urban areas was about three times more than that in rural areas, and the number of qualified medical doctors per 1,000 people in urban areas was four times and registered nurses approximately seven times that in rural areas. Taking into account the geographic considerations and low population density, according to the Chinese scholar’s Health Resource Density Index (HRDI),28 Tibet’s HRDI in 2015 was the lowest and lower than other western provinces’ average of 1.34.29
The maternal health workforce mainly refers to doctors and nurses in the O&G sector. Like most other parts of China, there is no specific midwife occupation in Tibet. Although nurses or O&G doctors in the delivery room have a skill mix as midwives, real midwifery is neither encouraged nor common according to current hospital delivery policy.30,31 The health workers of MCH hospitals and stations are the main component of maternal health workforce. Although the number of HRH in prefecture MCH hospitals is gradually increasing, there is still an average of about 11 job vacancies.32 In 2015, Tibet had 520 MCH hospital/station health workers; among them 447 were health professionals (including 203 physicians and 105 registered nurses). The number in the MCH workforce was the lowest in China, with about 31% of MCH professionals not holding a qualified certification or were interns. In addition, the doctor:nurse ratio (2:1) was much higher than national average33 and Chinese national standard (1:2).34
Training and recruitment
China’s central government launched the Tibetan modern medical doctor and nurse training program in the 1960s.35 A secondary level modern medical education program was also initiated in Tibet and other Chinese mainland cities for Tibetan students in the 1970s. All qualified graduating students were assigned jobs. Since 1978, Tibet Autonomous Region Medical College has enrolled bachelor degree modern medical students.35 In 1989, the Tibet Autonomous Region (TAR) government re-established the Tibetan Traditional Medicine University for training TTM professionals.35 In the 1990s, the TAR government developed a 3-year secondary high school level MCH professionals program in health vocational schools in mainland China for Tibet’s MCH centers and stations. Since 2010, like other parts of China, the Rural Medical Students Scholarship Scheme has also been implemented in Tibet. Based on the scheme, an MCH class was designed with an MCH-based curriculum in Tibet University Medical College. Currently, Tibet has three university level medical education centers.35 There were 530 and 427 graduate medical college students (including nurses and preventive medicine students) in Tibet in 2014 and 2015, respectively.4,36 However, the number of local graduates could not meet the shortage and the increasing demand of Tibet’s health workforce. Health professional recruitment and retention policy is still not a success and a brain drain is common, particularly in rural areas.37,38
Internal aid
Providing health professionals’ internal aid is another strategy to help remote, less developed area in China. The Aid Tibet Cadres (“yuan zang gan bu” in Chinese) Program includes health supports to Tibet. This program through the Paring-Aid Province (“dui kou yuan zang sheng” in Chinese) has sent Chinese medical professionals to work in Tibet for a 1- to 3-year period since 1950s.39 The Medical Professional Delegation Aid Tibet Program (“zu tuan shi yi liao yuan zang” in Chinese) was specially designed by the Chinese Central Communist Party Organization Department and launched in 2015.6 About 322 doctors from the 94 best hospitals in mainland China were grouped as delegations and sent to aid Tibet in 2015 and 2016, staying in Tibet for at least 1 year and working with local doctors and training local health workers. Tibet PH and seven prefecture (city) hospitals (“1+7”) were the main target support hospitals for this program. It was reported that the average number of outpatient, inpatient, and surgical operations in those hospitals has increased by 19.59%, 17.60%, and 17.83%, respectively.40 This program had a positive effect on service delivery and local health workers development, but the challenge to make it sustainable remains. Thus, developing an effective mechanism to develop and benefit local professionals is an important issue that needs to be studied and evaluated.
Deployment
Tibet ended its undergraduate job assignment policy in 2006 and introduced a two-way selection employment policy under open recruitment testing. Medical graduates mainly flow to primary health care centers, but there has not been a solid continuing education for these inexperienced graduates. For referral hospitals at prefectural level, specialist doctors are mostly recruited from other provinces, with very few new graduates or locally experienced doctors recruited each year. This universal broad-brush solution for HRH has been greatly criticized.32,37,38
Maternal child health infrastructures
Facility and technology
Tibet has developed MCH health facility infrastructure from scratch since 1979 when the first county MCH facility was built. The first prefectural MCH hospital was established in 1984 in Lhasa and later in Nagchu and other prefectures. The Tibet TTM hospital has also established a traditional medicine and modern medicine combined O&G department. Private MCH hospitals and some obstetric clinics have also appeared in Lhasa since 2000. Overall, the total bed number in Tibet hospital’s O&G section increased from 434 in 2007 to 835 in 2013. Subsequently, township health care centers have been developed rapidly since 200335 to serve basic ANC, natural delivery, and to receive referrals from primary health care centers. All county (district) hospitals are equipped with a functional ambulance. Each administrative village and township health care center have also been given at least one vehicle responsible to transport emergency pregnancy cases to health facilities. Telemedicine and air transportation were initially developed in Tibet in 2015 and 2017, respectively. These services can potentially be a great model for supplementary assistance in MCH care in remote areas, as practiced in Mongolia and Australia.41,42 The utilization and effectiveness of each model need to be evaluated.
Emergency obstetric care
According to emergency obstetric care (EOC) criteria, Tibet’s 74 county hospitals barely meet the standard of basic EOC. The prefecture (city) hospital and referral hospitals provide comprehensive EOC. Thus, there are about 12 EOC facilities and two comprehensive EOC for every 500,000 population, which merely meets the WHO’s minimum standard for EOC43 (Table 2). However, this number is apparently inadequate in a low density population like Tibet. Tibet’s cesarean section rate was <5%, which is lower than WHO’s recommendation and much lower than China’s average.43 This may indicate low utilization rate of emergency care and a great shortage of EOC centers.
  | Table 2 Emergency obstetric care facilities in Tibet in 2015 |
Maternal health information
Tibet follows the national health information system and the vital MCH-related information collecting systems. The National MCH surveillance system of the National Office for Maternal and Child Health Surveillance (NOMCHS) and Death Surveillance Center (DSC) of China CDC were the two most relevant systems to MMR. There were six NOMCHS counties and eight CDC DSC project counties, which provide maternal care data in the region. However, this vital system is limited by the shortage of human resources. The project sample counties are mostly located in central Tibet, whereas rural information is lacking.
Health system finance and insurance system
Health expenditure
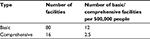
Tibet’s health finance is dominantly dependent on the central government. Although the amount of total expenditure on health (TEH) is small, the TEH and public health spending in Tibet have increased on a yearly basis as the Chinese economy continued to grow with the resulting increment of financial input. The TEH has increased from 7.383 billion in 20135 to 8.193 billion in 2014,13 and total public health spending has sharply increased 67-fold rising from 71.534 million to 4801.83 million CNY in the last two decades (1990–2013)44 (Figure 2). Government expenditure comprises about two thirds, while individual out-of-pocket (OOP) contributions in Tibet were much smaller than the national average5,13 (Table 3). Tibet also had the highest proportion of total expenditure of GDP in the country. However, the TEH per capita was lower than in neighboring autonomous regions and provinces such as Xinjiang and Qinghai13 (Table 3). The proportion of public health spending in total government spending has decreased and has remained between 4% and 7% since 1990.44
  | Figure 2 Government total spending and public health spending in Tibet Autonomous Region of China during the year 1990–2013. |
  | Table 3 Total expenditure on health (TEH) by different domains in Tibet and neighbor provinces in 2013 and 2014 |
Health insurance and subsidy
Similar to other parts of China, Urban Employees’ Basic Medical Insurance (UEBMI) and Urban Residents’ Basic Medical Insurance (URBMI) cover the urban population. The New Rural Cooperative Medical Scheme, which in Tibet is named “Free Medical Fee Based TAR Farmer and Herdsman Medical Scheme (FHMS),” covers the rural population.24 The Medical Financial Assistance Scheme supports people living below the poverty line in both urban and rural areas. Due to the majority of population (72.26% in 2016) living in rural areas, the Tibet health insurance system places more emphasis on the FHMS, which has evolved over three stages: the free medical services era (1959–1996), rural cooperative medical scheme (1997–2002), and the present period of the free fee-based Tibet FHMS (since 2003). The current scheme is a voluntary insurance scheme with a mix of flat-rate household contributions and subsides from the central and the Tibet governments. Although project-based transportation and living subsidy were initiated in the early 2000s, hospital child delivery and subsidy for transportation were first included in the FHMS from 2006 with a maximum reimbursement limit. After 2012, the institutional childbirth fee exemption policy was universally implemented for all rural residents.
In October 2015, Tibet HFPC launched a new regulation to promote hospital delivery in rural Tibet. According to the regulation, every rural woman who gives birth at an appointed hospital receives 1,000 CNY as a living subsidy and 30 CNY per day if admitted to the hospital before the beginning of labor pain and 50 CNY for transportation. However, due to the limitation of sickbeds in most referral hospitals, the length of hospital stay is shortened, and pregnant women who have not yet experienced labor pain are not allowed to be admitted to the hospital too early by most hospitals, especially in a referral hospital. Even though county or township hospitals allow pregnant women to stay there in advance of the labor pain, the poor living conditions inside the hospital deter many families from being admitted. Thus, rural pregnant women who are determined go through child labor in a hospital in the city need to rent a room nearby the hospital or live in a relative’s or friend’s home with subsequent expenditure, but without receiving any subsidy during that time.
There is no restriction to visit any hospital in Tibet. However, pregnant women who bypass the referral hospital without receiving a referral need to have an amount about of 4,000–5,000 CNY deposited in their account in advance. The hospital child delivery fee is not directly reimbursed from the hospital at the time of discharge, but the woman needs to apply for it from the government office located at the place of house registration. The health insurance electronic transaction might be a solution for this, but this has not yet been put into practice in Tibet.
OOP for MHS
Although free hospital delivery care has been implemented, ANC and PPV are listed in the essential public health service scheme but not included in the reimbursement package as hospital delivery. In addition, due to the poor quality of health services in rural hospitals, people are more likely to bypass the referral hospital. Women from remote areas need to stay near a hospital until experiencing labor pain. The hidden cost for a maternity waiting period, ANC, and PPV has not yet been studied in Tibet.
Progress in maternal health
In the early 1960s, maternal health care service was initiated in the Lhasa municipal hospital35 and has been practiced in Tibet since then, although progress almost stopped during the Cultural Revolution era, as elsewhere in China.45 From the late 1970s to early 1990s, the MHS service system grew into MCH stations and hospitals in all seven prefectures (cities)35 and improved after 2000.
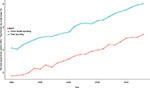
Figure 3 illustrates the change in MMR, hospital delivery rate, ANC, and PPV coverage between 2000 and 2015. The lines were derived from joinpoint analysis. It is clear that there were sharp increases in ANC and PPV coverage after 2012. The hospital delivery rate has stably increased by 70.4% during the period. The MMR is in declining trend. The rate of reduction was 8.32/100,000 per year between 2000 and 2013. One small turning point was also observed in 2013, when the rate of decline was 19.93/100,000 per year. This could be a direct result of free delivery care introduced in 2012. In addition, the correlation test showed that there was a negative high correlation (r=−0.9) between hospital delivery and the MMR and positive strong correlation between ANC and PPV (r=0.86).
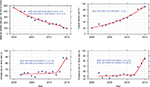  | Figure 3 Maternal health data in Tibet Autonomous Region of China between 2000 and 2015. Abbreviation: APC, annual percent change. |
Summary and implications
In summary, with continuous financial investment, there has been remarkable progress in maternal survival and MHS in Tibet, particularly after 2012 where government resources were more available. However, the relative stagnation of MMR reduction after 2015 needs further exploration. The shortage of health professionals and EOC centers and sound maternal health information for the predominantly rural and scattered population in remote areas still need improvement.
Acknowledgments
This study is part of the first author’s thesis in partial fulfillment of the requirements for a PhD at Prince of Songkla University, Thailand, and the China Medical Board (CMB) under the project of “Join Research Capacity Strengthening of the Western Rural Health Network, China”, CMB#11-086 and Zhu Feng Scholar Program of Tibet University provided the financial support. The authors are grateful to Tibet University Medical College and CMB for its support during the study period at Prince of Songkla University. Special thanks to Dr Walaiporn Patcharanarumol, Ms Sangay Wangmo, and Nongnuch Jaichuen from International Health Policy Program, and Mr Surichai Bilheem from the Epidemiology Unit, Prince of Songkla University, Thailand, who provided valuable suggestions and support for developing the study.
Author contributions
LS and VC designed the study. LS analyzed and drafted the manuscript. EM provided expert statistical advice. EB, PS, DJ, and GY provided professional advice and technical support. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization [webpage on the Internet]. Maternal mortality. WHO; 2017. Available from: http://www.who.int/gho/maternal_health/mortality/maternal_mortality_text/en/. Accessed September 5, 2018. | ||
Ministry of Foreign Affairs of the People’s Republic of China. China’s National Plan on Implementation of the 2030 Agenda for Sustainable Development; 2016. Available from: http://www.fmprc.gov.cn/web/ziliao_674904/zt_674979/dnzt_674981/qtzt/2030kcxfzyc_686343/P020170414689023442403.pdf. Accessed September 5, 2018. | ||
Ministry of Foreign Affairs of the People’s Republic of China. China Releases National Plan on Implementation of the 2030 Agenda for Sustainable Development; 2016. Available from: http://www.fmprc.gov.cn/mfa_eng/zxxx_662805/t1405596.shtml. Accessed October 24, 2018. | ||
Duoji Z. [Tibet Statistical Yearbook 2015]. Beijing: China Statistics Press; 2015. Chinese. | ||
National Health and Family Planning Commission. [China’s Health and Family Planning Statistical Yearbook 2015]. Beijing: Peking Union Medical College Press; 2015. Chinese. | ||
Zeng W. [Medical professional delegation aid Tibet Program boosts Tibet’s healthcare development]. China Health. 2017;9:58–59. Chinese. | ||
Bianba. [Analysis of 98 maternal death in Lhasa, Tibet]. Tibetan Medical. 2012;33(4). Chinese. | ||
Cui Y, Li Y, Lei W, Kuangshi W, Yi M. [Analysis of cause on 19 maternal deaths in project area of Tibet]. Chin J Maternal Child Health. 2006;1:7–9. Chinese. | ||
Banke-Thomas OE, Banke-Thomas AO, Ameh CA. Factors influencing utilisation of maternal health services by adolescent mothers in low-and middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2017;17(1):65. | ||
Campbell OMR, Graham WJ; Lancet Maternal Survival Series steering Group. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):1284–1299. | ||
People’s Government of Tibet Autonomous Region. [Tibet Autonomous Region Rural Medical Management Program Interim Measures. Lhasa, Tibet; 2006]. Chinese. | ||
People’s Government of Tibet Autonomous Region of P. R. China. [Tibet Autonomous Region Rural Medical Management Program]. Lhasa, Tibet; 2012. Chinese. | ||
National Health and Family Planning Commission. [China’s Health and Family Planning Statistical Yearbook 2015]. Beijing: Peking Union Medical College Press; 2015. Chinese. | ||
Ministry of Health. [China’s Health Statistical Yearbook 2007]. Beijing: Peking Union Medical College Press; 2007. Chinese. | ||
Gao Y, Zhou H, Singh NS, et al. Progress and challenges in maternal health in western China: a Countdown to 2015 national case study. Lancet Glob Health. 2017;5(5):e523–e536. | ||
Bryce J, Jh R, Lh M, Ram M, Re B. Population Health Implementation and Training-Africa Health Initiative Data Collaborative: a common evaluation framework for the African Health Initiative. BMC Health Services Research. 2013;13(Suppl 2):S10. | ||
Moucheraud C, Owen H, Singh NS, et al; Countdown Case Study Collaboration Group. Countdown to 2015 country case studies: what have we learned about processes and progress towards MDGs 4 and 5? BMC Public Health. 2016;16(Suppl 2):794. | ||
Bryce J, Requejo JH, Moulton LH, et al. A common evaluation framework for the African Health Initiative. BMC Health Serv Res. 2013;13(Suppl 2):S10. | ||
World Health Organization. Everybody’s Business - Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action. Geneva: World Health Organization; 2007. | ||
Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. | ||
Tibet Autonomous Region People’s Government. Maternal healthcare training for village doctors hold by Tibet maternal and child association; 2017. Available from: http://www.xizang.gov.cn/xwzx/qnyw/201706/t20170630_137800.html. Accessed October 24, 2018. Chinese. | ||
Interim Measures to Enhance Hospital Delivery in Rural Tibet Autonomous Region of P. R. China. Tibet Autonomous Region Health and Family Planning Commission File no.2015-262. Lhasa: 2015. Chinese. | ||
Lai Y, Jian W, Dawa Z, Yinchuan J, Xuejiao C. Operation status and problems of county disease control center in Tibet under the “Four in One” management model. Chin Rural Health Serv Admin. 2016;9:1144–1145. | ||
Wang W, Shi L, Yin A, et al. Primary care quality among different health care structures in Tibet, China. Biomed Res Int. 2015;2015:1–8. | ||
The State Council of the People’s Republic of China. Law of the People’s Republic of China on maternal and infant health care. Beijing; 1994. Available from: http://www.ilo.org/dyn/natlex/docs/ELECTRONIC/38702/108046/F-2064760163/CHN38702%20Eng.pdf. Accessed September 5, 2018. | ||
People’s Government of Tibet Autonomous Region [webpage on the Internet]. Tibet Autonomous Region’s plan of action for women (1996–2000). Lhasa; 1996. Available from: http://www.people.com.cn/GB/99013/99041/100696/100820/6186976.html. Accessed September 5, 2018. | ||
People’s Government of Tibet Autonomous Region of P. R. China. Tibet Autonomous Region Health Workforce Development Plan (2013–2020). Lhasa, Tibet; 2013. Chinese. | ||
Fang Y, Siliang, Zheng X, Li M, Liu S, Zhang R. [Density index of human resource health]. China Healthcare Management. 2000;4:253–254. Chinese. | ||
Liu H. Prediction of Human Resource for Health and Intensive Factors of Primary Healthcare in West China [PHD]. Shandong University; 2017. Available from: http://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CDFD&dbname=CDFDLAST2017&filename=1017079837.nh&v=MTQ5OTlMVkYyNkdiTy9GOW5QcUpFYlBJUjhlWDFMdXhZUzdEaDFUM3FUcldNMUZyQ1VSTEtlWitWdUZDcmhVcnI=. Accessed November 1, 2018. Chinese. | ||
Cheung NF. Chinese midwifery: the history and modernity. Midwifery. 2009;25(3):228–241. | ||
Feng XL, Xu L, Guo Y, et al. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull World Health Organ. 2012;90(1):30–39. | ||
Zhaxi D, Hua C, Zhen W, Wenhua W, Yangli G, Luobu O. [Analysis on the allocation and utilization of health human resources in Tibet Autonomous Region]. Chin Health Econ. 2016;6:51–54. Chinese. | ||
Crisp N, Chen L, Lincoln C. Global supply of health professionals. N Engl J Med. 2014;370(10):950–957. | ||
[China’s Nursing Management Standard and Assessment Approach (For Trial Implementation)]. 2013. Available from: http://chisc.net/CIOjulebu/wsbmwj/2013-09-30/2323.html. Accesed Novemebr 1, 2018. Chinese. | ||
Tibet Autonomous Region Local History Codification Committee. [Tibet Autonomous Region Health Annals]. Beijing: China Tibetology Press. Chinese. | ||
Duoji Z. [Tibet Statistical Yearbook 2016]. Beijing: China Statistics Press; 2016. Chinese. | ||
Lamu Deji LX. [An analysis on human resource for health in Tibet Autonomous Region]. Modern Med Health. 2015;23:3671–3673. Chinese. | ||
Lai Y, Zhaxi Dawa LS. [A study of health human resources in Tibet]. Chin Health Econ. 2012;8:16–18. Chinese. | ||
Guo R. China’s Regional Development and Tibet. Singapore: Springer; 2015. | ||
Tibet Autonomous, RegionHealth Family Planning, Committee. [Exploration and practice of Medical Professional Delegation Aid Tibet Program]. China Health Hum Resour. 2017;10:14–18. Chinese. | ||
Baatar T, Suldsuren N, Bayanbileg S, Seded K. Telemedicine support of maternal and newborn health to remote provinces of Mongolia. Stud Health Technol Inform. 2012;182:27–35. | ||
Akl N, Coghlan EA, Nathan EA, et al. Aeromedical transfer of women at risk of preterm delivery in remote and rural Western Australia: why are there no births in flight? Aust N Z J Obstet Gynaecol. 2012;52(4):327–333. | ||
Maine D. Monitoring Emergency Obstetric Care: A Handbook. Geneva: World Health Organization; 2009. | ||
Center of Health Statistics of Tibet Autonomous Region Health and Family Planning Commission. [Tibet Health Statistics Annual Report 2013]. Lhasa: Health and Family Planning Commission of Tibet Autonomous Region; 2013. Chinese. | ||
Guo Y, Bai J, Na H. The history of China’s maternal and child health care development. Semin Fetal Neonatal Med. 2015;20(5):309–314. |
Supplementary materials
  | Table S1 Tibet autonomous region’s statistical profile in 2000, 2010, and 2015 Note: “–” represents data were not available. |
  | Figure S1 Maternal health system review framework. |
  | Figure S2 Health system and its organisation structure and health service delivery system in Tibet. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
