Back to Journals » Clinical Interventions in Aging » Volume 18
Prognostic Value of Systemic Immune-Inflammation Index and NT-proBNP in Patients with Acute ST-Elevation Myocardial Infarction
Authors Zhu Y , He H, Qiu H, Shen G, Wang Z, Li W
Received 15 December 2022
Accepted for publication 12 March 2023
Published 17 March 2023 Volume 2023:18 Pages 397—407
DOI https://doi.org/10.2147/CIA.S397614
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Yinghua Zhu,1,* Haiyan He,2,* Hang Qiu,1 Guoqi Shen,1 Zhen Wang,1 Wenhua Li1,3
1Institute of Cardiovascular Diseases, Xuzhou Medical University, Xuzhou, People’s Republic of China; 2Department of Cardiology, Xuzhou Municipal Hospital Affiliated to Xuzhou Medical University, Xuzhou, People’s Republic of China; 3Department of Cardiology, Affiliated Hospital of Xuzhou Medical University, Xuzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wenhua Li, Department of Cardiology, Affiliated Hospital of Xuzhou Medical University, Xuzhou, People’s Republic of China, Tel +86 18052268293, Email [email protected]
Objective: Our aim was to assess systemic immune-inflammation index (SII) and NT-proBNP value either in singly or in combination to predict acute ST-elevation myocardial infarction (STEMI) patient prognosis.
Methods: Analyzed retrospectively the clinical features and laboratory data of STEMI confirmed patients in our hospital from January to December 2020. The levels of SII and NT-proBNP were detected. The Kaplan-Meier approach and Spearman’s rank correlation coefficient were used to construct the overall major adverse cardiac event (MACE) curve. Multivariate Cox regression analysis was applied to detect MACE predictors. In addition, the Delong test and receiver operating characteristic (ROC) curve analyzed each factor performance on its own and composite multivariate index to predict MACEs.
Results: The MACE group showed statistically significant differences in SII, NT- proBNP in comparison to the non-MACE group (P=0.003, P < 0.001). Based on Kaplan-Meier analysis, SII and NT-proBNP showed positive correlation with MACE (log-rank P < 0.001). SII and NT-proBNP were independent predicting factors for long-term MACEs in multivariate Cox regression analysis (P < 0.001, HR: 2.952, 95% CI 1.565– 5.566; P < 0.001, HR: 2.112, 95% CI 1.662– 2.683). SII and NT-proBNP exhibited a positive correlation (R = 0.187, P < 0.001) in correlation analysis. According to the ROC statistical analysis, the combination exhibited 78.0% sensitivity and 88.0% specificity in the prediction of MACE. According to the results of the AUC and Delong test, the combined SII and NT-proBNP performed better as a prognostic index than each of the individual factor indexes separately (Z = 2.622, P = 0.009; Z = 3.173, P < 0.001).
Conclusion: SII and NT-proBNP were independent indicators of clinical prognosis in acute STEMI patients, and they correlated positively. These factors could be combined to improve clinical prognosis.
Keywords: systemic immune-inflammation index, NT-proBNP, STEMI, MACEs, risk assessment
Introduction
ST-segment elevation myocardial infarction (STEMI) has been recognized as the disease with the highest mortality and morbidity in the world for many years; ruptured atherosclerotic plaque is the most common cause of STEMI.1 As emergency intervene technology matures and gains acceptance in clinical practices, emergency intervention therapy has become the most appropriate treatment for acute STEMI. Percutaneous coronary intervention (PCI) showed clinical prognosis improvement by increasing of myocardial blood flow perfusion.2 However, STEMI patients are still at risk for long-term adverse cardiovascular events (MACEs).3 Studies have shown that current smoking, history of heart failure, and diabetes mellitus are independent predictors of MACEs after STEMI.4,5 SII and NT-proBNP levels are rarely reported to be associated with MACEs.
Several studies have demonstrated that inflammation contributes to the progress of atherosclerotic ischemic heart disease. Research showed that the systemic immune-inflammation index (SII), a combination of lymphocytes, neutrophils, and platelets, can predict the development of cancer.6 According to several recent studies, the SII is correlated with adverse consequences in patients with cardiovascular disease, including atrial fibrillation, chronic heart failure and cardiomyopathy.7,8
NT-proBNP is a prohormone released by cardiomyocytes, mainly in response to increased wall-filling stress in cardiac chambers, which then leaks into the peripheral circulation.9,10 NT-proBNP has also been identified as a strong independent prognostic marker in different cardiac patients. As a result of local stretch mechanisms in the area surrounding the ischemic region, NT-proBNP production increases after acute myocardial ischemia.11 It has been shown in recent years that elevated NT-proBNP is linked to a better outcome, and the most studied outcome is in-hospital/30-day mortality.12,13
Both SII and NT-proBNP may independently predict the severity and outcome of cardiovascular disease. This is conducive to early stratification and preventing the occurrence of MACEs. The objective of current study is to assess predictive valuableness of SII, NT-proBNP, alone and combined for the clinical outcomes of STEMI patients.
Materials and Methods
Design and Study Population
This is a retrospective observational cohort study of patients with STEMI diagnosed at a single center at Xuzhou Medical University’s Affiliated Hospital between January and December 2020.
The criteria for the early diagnosis of STEMI include the following: (I) typical angina and/or signs of ischemia at rest lasting more than 20 minutes; (ii) the occurrence of ST-segment elevation aligns with Myocardial Infarction of 2 mm or higher in adjacent chest leads and/or ST-segment elevation of ≥ 1 mm in 2 ≥ standard leads or the existence of a new (or probably new) left bundle branch block on electrocardiogram at admission; and (iii) positive indicators of myocardial injury.14
Patients excluded were those with chronic heart failure (New York Heart Association (NYHA) class 3 or higher), severe chronic renal failure or severe hepatic impairment, inflammation (including ongoing infection, systemic inflammation, or autoimmune disease), cancer, stroke, valvular heart disease, hematologic disorders, pregnant .
The study initially enrolled 389 patients. However, a sum of 34 patients were exempted from follow up and a sum of 355 patients were enrolled as a result, including 262 males (78.0%), with an average age of 63.40 ± 12.72 years. The study protocol was accepted by the Affiliate of Xuzhou Medical University’s Ethics Committee in compliance with the Helsinki Declaration. Participants provided written/oral informed consent. A combination of medical records and telephone interviews was used in the study to collect data. The flow chart for the study displayed in Figure 1.
 |
Figure 1 The flow chart of participants inclusion. |
Clinical and Demographic Characteristics
In the first 24 hours following admission, patient’s blood samples were collected. Medical records were reviewed for demographic and clinical characteristics, including gender, age, diabetes and hypertension histories, smoking status, and medication histories. Left ventricular ejection fraction (LVEF) values and Lab results were collected includes lipid profile, complete blood count, NT-proBNP, and fibrinogen, as well as fasting blood-glucose (FBG), alcohol consumption, glycated hemoglobin, uric acid, and urea nitrogen. The SII was calculated based on the absolute peripheral neutrophil count × platelet count/lymphocyte count.
Division of Patient Groups
From the medians of SII and NT-proBNP, patients were grouped into four groups (Group Q1, SII ≤1240.61 or NT-proBNP ≤280.53; Group Q2, SII>1240.61 and NT-proBNP >280.53). In Group Q1 (low SII/low NT-proBNP), n = 263; in Group Q2 (high SII + high NT-proBNP), n = 92. Subsequently, two groups of patients were formed (n = 100) and (n = 255) based on whether they experienced MACEs throughout follow up.
Clinical Endpoint and Follow Up
The MACEs occurred during the hospitalization or within 1 year after discharge were recorded, including deaths from all causes, not fatal MI, malignant arrhythmia, target vessel reconstruction, unstable angina, acute heart failure, and non-fatal stroke.
Statistical Analysis
For the analysis, SPSS 26.0 for Windows (SPSS Inc., Chicago, IL, USA) was used. Counts and percentages (%) are expressed for categorical variables, while mean ± standard deviations or medians and quartile intervals (%) are expressed for continuous variables. Independent sample t-tests were employed for comparison between parameter values among groups, Mann–Whitney U-tests were applied for comparison between non-parameter values across groups, and for comparing classified variables, the chi-square (χ2) test was carried out. Pearson correlation coefficient analysis was used to investigate correlation between SII and NT-proBNP. The prognosis predictive value throughout follow-up examined with Cox regression analysis. Kaplan-Meier analysis was used to calculate the cumulative incidence of long-term outcomes, and the Log rank test was used to compare between groups. P<0.05 was regarded as significant. Receivers operating characteristic (ROC) curves were created to examine the predictive value of risk variables. It was determined that the diagnostic effect was better when ROC curves were compared. The Delong test was applied to analyze the SII, NT-proBNP and combined indexes in predicting the efficacy of MACE.
Results
Baseline Clinical Characteristics of Patients
A sum of 355 individuals were enrolled in the research who were clinically diagnosed with STEMI and were followed for one year. Table 1 displays the clinical, ultrasonic cardiogram, and lab results for the study participants. Except for diuretics, there were no statistically significant differences between the two groups in terms of drug administration. Patients in Group Q2 were markedly older than those in Group Q1, and in Group Q2, SII, NT-proBNP, WBC count, neutrophil count, platelet count, CKMB were higher. In Group Q2, lymphocyte count, total cholesterol, and creatinine were lower than those of Group Q1.
 |
Table 1 Clinical and Laboratory Characteristics of Enrolled Patients According to SII and NT-proBNP |
Clinical Characteristics of Patients with and without MACEs
In this research, as a composite endpoint, 100 patients (28.2%) developed MACEs, with 39 cases (11.0%) of all-cause mortality and 22 cases (6.2%) of re-hospitalization for angina. 14 cases (3.9%) of nonfatal myocardial infraction; 7 cases (2.0%) of target vessel reconstruction; of which 16 cases (4.5%) of acute heart failure; and 2 cases (0.6%) of non-fatal stroke. MACE patients were noted to be older and diabetes was more prevalent. Furthermore, the neutrophil count, hemoglobin, CK-MB, creatinine, fibrinogen, SII, and NT-proBNP levels in the MACE group were greater than in the non-MACE group. Additionally, the lymphocyte count and the proportion of male and the history of diuretics and nitrates in MACE-free group was higher (Table 2).
 |
Table 2 Comparison of Clinical and Laboratory Characteristics of Enrolled Patients According to the Occurrence of MACEs |
Risk Factor Analysis for MACEs Development
Based on MACE occurrence as an endpoint indicator, under univariate Cox survival analysis, lymphocyte count, hemoglobin, red blood Cell distribution width (RDW), hypersensitive C-reactive protein (hs-CRP), fibrinogen (FIB), The multivariate Cox survival analysis included Ln(SII) and Ln(NT-proBNP) (P <0.01) and showed that Ln(SII) (HR = 2.952 P < 0.001, 95% CI 1.565–5.566) and Ln(NT-proBNP) (HR = 2.112 P < 0.001, 95% CI 1.662–2.683) independently predicted the development of MACE in STEMI patients (Table 3).
 |
Table 3 Univariate and Multivariate Cox Regression Analysis Results for MACEs |
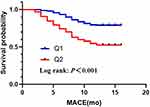
Long-term patient survival rates were assessed using the Kaplan-Meier survival analysis. As displayed in Figure 2, the MACEs at 1 year were significantly different between the two groups. In the group with high SII and high NT-proBNP, MACE incidence was greater (log rank: 29.67, P<0.001).
Correlation Between the SII and NT-proBNP
The Pearson correlation analysis was utilized to measure the correlation counts between SII and NT-proBNP. The findings revealed a positive correlation between SII and NT-proBNP (R = 0.187, P<0.001).
Effect of Combined SII and NT-proBNP on Development of MACE
ROC analysis was done to determine if the SII and NT-proBNP could enhance the prediction of long-term MACEs. The ROC curve analysis indicated that for the SII, the AUC was 0.649 (95% CI: 0.587–0.712, P<0.001), for the NT-proBNP, the AUC was 0.774 (95% CI: 0.710–0.835, P<0.001), and for the SII and NT-proBNP combined, the AUC was 0.840 (95% CI: 0.791–0.887, P<0.001) (Figure 3). Compared with the SII and NT-proBNP, and the SII combined with NT-proBNP, the combination predicted MACEs better than SII or NT-proBNP alone, and the variance between them was statistically significant. (Z = 2.622, P = 0.009; Z = 3.173, P <0.001).
 |
Figure 3 Receiver operating characteristic curves of SII, NT-proBNP, SII combined with NT-proBNP for 1-year MACEs prediction. |
Discussion
STEMI is a type of coronary heart disease that is seriously life-threatening. It refers to the plaque rupture in these coronary arteries that contain unstable atherosclerotic plaques due to lack of blood supply and oxygen, thereby leading to coronary micro thrombosis, making myocardial tissue cell swelling, degeneration and necrosis. Clinical manifestations consist of persistent chest tightness and chest pain, gastrointestinal symptoms, palpitations caused by arrhythmia.15 Once myocardial infarction occurs, cardiomyocytes cannot regenerate at the infarct site and the necrotic myocardial tissue becomes thinning. It may cause heart rupture, papillary muscle rupture, abnormal heart conduction pathway, heart failure and other complications. These complications seriously affect the prognosis of patients.16 STEMI is one of the most prevalent types of myocardial infarction. Moreover, it is common among the middle-aged and elderly individuals.17 In recent years, STEMI incidence and mortality have been increasing year by year. Recently, it is not unusual for many young patients to have an acute coronary syndrome.18 Therefore, it is extremely important to pay clinical attention to the follow-ups on the treatment of patients with STEMI whilst also effectively assessing poor outcomes risk of in STEMI patients, as well as timely formulating the corresponding individualized intervention measures, so as to reduce the mortality of STEMI patients and provide better patients prognostic quality of life.
SII is a systemic immune inflammation index, which integrates more inflammation and immune indicators that reflect the body state. It can better reflect the inflammation and immune system status of patients.19 After the inflammation occurs in the human body, it may promote the abnormal rise of platelets. Abnormally aggregated platelets also adhere to the surface of the endothelial cells of the body, thus inducing local ischemia, hypoxia, micro thrombosis and then blocking blood vessels, causing ischemic MI, stroke, peripheral vascular diseases and other malignant clinical events.20 Serum levels of SII are linked to a greater chance of developing ischemic heart disease, ACS, cardiovascular events, and stroke.21,22 An abnormal decrease in lymphocyte count indicates excessive lymphocyte apoptosis, which reduces the immune system capacity and immune dysfunction. It is then easy to promote the endothelial dysfunction, resulting in abnormal aggregation and thrombosis after platelet activation.23 While neutrophils can also activate and induce inflammatory reactions in the body, promote the abnormal coronary plaques, induce the atherosclerotic plaque rupture and thrombosis,24,25 and then increase cardiovascular complications risk. Dziedzic et al have reported26 that after SII is applied to patients with STEMI. In the short-term prognosis, SII levels are significantly higher in the poor prognosis group than in the good prognosis group.
NT-proBNP is the remaining other half of the product when the BNP precursor (pro BNP) cleaves into BNP. It is mainly a hormone secreted by ventricular cells that has many biological effects, such as vasodilation, balancing water and sodium metabolism, inhibiting renin-angiotensin and sympathetic nervous system, etc. When the ventricular volume and pressure load increase, or the left heart function is impaired, it can be greatly expressed in a short time and reflect the cardiac function.27,28 Some studies report that NT-proBNP can be used as an early warning and diagnostic indicator for STEMI.29
The current study assessed the ability of SII and NT-proBNP alone and jointly to predict MACE in a cohort of patients with STEMI. Compared to other biomarkers, SII and NT-proBNP can better respond to inflammatory conditions and ventricular load and wall pressure in STEMI patients.30 The outcomes of univariate and multivariate Cox survival analysis show that SII and NT-proBNP are both independent predictors of MACE in STEMI patients. MACE incidence is significantly higher in the patients with higher values of SII and NT-proBNP. Moreover, SII is also correlated with NT-proBNP to some extent. SII combined with NT-proBNP may improve the predictive power of cardiovascular complications in STEMI patients.
Limitations
This research has some limitations. Firstly, this is a single-center retrospective research, and the inseparable limitations of these investigations will invariably result in selection bias. Secondly, the follow-up period is short and the sample size is small; therefore, multicenter and larger sample sizes are required to establish clinical relevance.
Conclusion
This study demonstrated that SII and NT-proBNP in STEMI patients may be used for prediction of MACEs development, and SII had a positive correlation with NT-proBNP. A combination of the SII and NT-proBNP might improve clinical outcome predictions in these patients.
Data Sharing Statement
The corresponding author can provide the Data upon appropriate request.
Ethics Approval and Consent Participate
The study was approved by the Medical Ethics Committee of Xuzhou Medical University’s Affiliated Hospital in compliance with the Helsinki Declaration. Due to the retroactive nature of the investigation, the review committee relaxed the necessity for written informed consent. We eliminated all private patient data before examining the data.
Consent for Publication
All participants and/or their legal guardians given permission for the publishing of their information.
Acknowledgments
We want to appreciate all participants and colleagues who took part in the study. Yinghua Zhu and Haiyan He are co-first authors on this work.
Funding
There was no funding provided to the authors for this work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Bajaj A, Sethi A, Rathor P, Suppogu N, Sethi A. Acute complications of myocardial infarction in the current era: diagnosis and management. J Investig Med. 2015;63(7):844–855. doi:10.1097/jim.0000000000000232
2. Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO) the task force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39:763–816. doi:10.1093/eurheartj/ehx095
3. Radwan H, Hussein EM, Refaat H. Short- and long-term prognostic value of right ventricular function in patients with first acute ST elevation myocardial infarction treated by primary angioplasty. Echocardiography. 2021;38(2):249–260. doi:10.1111/echo.14974
4. Lemkes JS, Janssens GN, van der Hoeven NW, et al. Coronary angiography after cardiac arrest without ST segment elevation: one-year outcomes of the COACT randomized clinical trial. JAMA Cardiol. 2020;5(12):1358–1365. doi:10.1001/jamacardio.2020.3670
5. Otero-García O, Cid-álvarez AB, Juskova M, et al. Prognostic impact of left ventricular ejection fraction recovery in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: analysis of an 11-year all-comers registry. Eur Heart J Acute Cardiovasc Care. 2021;10:898–908. doi:10.1093/ehjacc/zuab058
6. Huang H, Liu Q, Zhu L, et al. Prognostic value of preoperative systemic immune-inflammation index in patients with cervical cancer. Sci Rep. 2019;9(1):3284. doi:10.1038/s41598-019-39150-0
7. Han Y-C, Yang T-H, Kim D-I, et al. Neutrophil to lymphocyte ratio predicts long-term clinical outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean Circ J. 2013;43(2):93–99. doi:10.4070/kcj.2013.43.2.93
8. Chen H, Li M, Liu L, Dang X, Zhu D, Tian G. Monocyte/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients with non-ST-elevation myocardial infarction. Medicine. 2019;98(26):e16267. doi:10.1097/md.0000000000016267
9. Clerico A, Vittorini S, Passino C. Measurement of the pro-hormone of brain type natriuretic peptide (proBNP): methodological considerations and pathophysiological relevance. Clin Chem Lab Med. 2011;49(12):1949–1954. doi:10.1515/cclm.2011.686
10. Yamashita T, Seino Y, Ogawa A, et al. N-terminal pro-BNP is a novel biomarker for integrated cardio-renal burden and early risk stratification in patients admitted for cardiac emergency. J Cardiol. 2010;55(3):377–383. doi:10.1016/j.jjcc.2010.01.008
11. Emdin M, Passino C, Prontera C, et al. Comparison of brain natriuretic peptide (BNP) and amino-terminal ProBNP for early diagnosis of heart failure. Clin Chem. 2007;53(7):1289–1297. doi:10.1373/clinchem.2006.080234
12. Schellings DA, Adiyaman A, Dambrink JE, et al. Predictive value of NT-proBNP for 30-day mortality in patients with non-ST-elevation acute coronary syndromes: a comparison with the GRACE and TIMI risk scores. Vasc Health Risk Manag. 2016;12:471–476. doi:10.2147/vhrm.S117204
13. Scirica BM, Kadakia MB, de Lemos JA, et al. Association between natriuretic peptides and mortality among patients admitted with myocardial infarction: a report from the ACTION registry(R)-GWTG™. Clin Chem. 2013;59:1205–1214. doi:10.1373/clinchem.2012.198556
14. Frampton J, Devries JT, Welch TD, Gersh BJ. Modern management of ST-segment elevation myocardial infarction. Curr Probl Cardiol. 2020;45(3):100393. doi:10.1016/j.cpcardiol.2018.08.005
15. Blondheim DS, Kleiner-Shochat M, Asif A, et al. Characteristics, management, and outcome of transient ST-elevation versus persistent ST-elevation and non-ST-elevation myocardial infarction. Am J Cardiol. 2018;121:1449–1455. doi:10.1016/j.amjcard.2018.02.029
16. Urbinati S, Tonet E. Cardiac rehabilitation after STEMI. Minerva Cardioangiol. 2018;66:464–470. doi:10.23736/s0026-4725.18.04674-1
17. Otten AM, Ottervanger JP, Timmer JR, et al. Age-dependent differences in diabetes and acute hyperglycemia between men and women with ST-elevation myocardial infarction: a cohort study. Diabetol Metab Syndr. 2013;5(1):34. doi:10.1186/1758-5996-5-34
18. Lichtman JH, Leifheit EC, Safdar B, et al. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: evidence from the VIRGO study (variation in recovery: role of gender on outcomes of young AMI patients). Circulation. 2018;137(8):781–790. doi:10.1161/circulationaha.117.031650
19. Candemir M, Kiziltunç E, Nurkoç S, Şahinarslan A. Relationship between Systemic Immune-Inflammation Index (SII) and the severity of stable coronary artery disease. Angiology. 2021;72(6):575–581. doi:10.1177/0003319720987743
20. Hally KE, La Flamme AC, Larsen PD, Harding SA. Platelet toll-like receptor (TLR) expression and TLR-mediated platelet activation in acute myocardial infarction. Thromb Res. 2017;158:8–15. doi:10.1016/j.thromres.2017.07.031
21. Hou D, Wang C, Luo Y, et al. Systemic immune-inflammation index (SII) but not platelet-albumin-bilirubin (PALBI) grade is associated with severity of acute ischemic stroke (AIS). Int J Neurosci. 2021;131(12):1203–1208. doi:10.1080/00207454.2020.1784166
22. Su G, Zhang Y, Xiao R, Zhang T, Gong B. Systemic immune-inflammation index as a promising predictor of mortality in patients with acute coronary syndrome: a real-world study. J Int Med Res. 2021;49(5):3000605211016274. doi:10.1177/03000605211016274
23. Harm T, Bild A, Dittrich K, et al. Acute coronary syndrome is associated with a substantial change in the platelet lipidome. Cardiovasc Res. 2022;118(8):1904–1916. doi:10.1093/cvr/cvab238
24. Klopf J, Brostjan C, Eilenberg W, Neumayer C. Neutrophil extracellular traps and their implications in cardiovascular and inflammatory disease. Int J Mol Sci. 2021;22(2):559. doi:10.3390/ijms22020559
25. Petzold T, Zhang Z, Ballesteros I, et al. Neutrophil “plucking” on megakaryocytes drives platelet production and boosts cardiovascular disease. Immunity. 2022;55(12):2285–2299.e7. doi:10.1016/j.immuni.2022.10.001
26. Dziedzic EA, Gąsior JS, Tuzimek A, et al. Investigation of the associations of novel inflammatory biomarkers-Systemic Inflammatory Index (SII) and Systemic Inflammatory Response Index (SIRI)-with the severity of coronary artery disease and acute coronary syndrome occurrence. Int J Mol Sci. 2022;23(17):9553. doi:10.3390/ijms23179553
27. Cordero A, Martínez Rey-Rañal E, Moreno MJ, et al. Predictive value of Pro-BNP for heart failure readmission after an acute coronary syndrome. J Clin Med. 2021;10(8):1653. doi:10.3390/jcm10081653
28. Schellings DA, Adiyaman A, Giannitsis E, et al. Early discharge after primary percutaneous coronary intervention: the added value of N-terminal pro-brain natriuretic peptide to the Zwolle risk score. J Am Heart Assoc. 2014;3(6):e001089. doi:10.1161/jaha.114.001089
29. Shanmuganathan M, Masi A, Burrage MK, et al. Acute response in the noninfarcted myocardium predicts long-term major adverse cardiac events after STEMI. JACC Cardiovascular Imaging. 2023;16(1):46–59. doi:10.1016/j.jcmg.2022.09.015
30. Çinar T, Hayiroğlu M, Şeker M, et al. The predictive value of age, creatinine, ejection fraction score for in-hospital mortality in patients with cardiogenic shock. Coron Artery Dis. 2019;30(8):569–574. doi:10.1097/mca.0000000000000776
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.