Back to Journals » OncoTargets and Therapy » Volume 11
Prognostic value of selected preoperative inflammation-based scores in patients with high-risk localized prostate cancer who underwent radical prostatectomy
Authors Shu K, Zheng Y, Chen J, Li W, Jiang K
Received 10 September 2017
Accepted for publication 28 February 2018
Published 3 August 2018 Volume 2018:11 Pages 4551—4558
DOI https://doi.org/10.2147/OTT.S151314
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ingrid Espinoza
Kunpeng Shu,1,* Yu Zheng,2,* Junru Chen,1 Wenbin Li,3 Ke Jiang4
1Department of Urology, Institute of Urology, 2Department of Thoracic Surgery, 3Huaxi MR Research Center (HMRRC), Department of Radiology, 4Thyroid and Parathyroid Surgery Center, West China Hospital of Sichuan University, Chengdu, Sichuan, People’s Republic of China
*These authors contributed equally to this work
Background: This study investigated the prognostic value of inflammation-based scores in patients with high-risk localized prostate cancer who underwent radical prostatectomy with or without neoadjuvant androgen deprivation therapy (ADT).
Methods: Inflammation-based scores included the neutrophil-to-lymphocyte ratio (NLR), derived NLR (dNLR), platelet-to-lymphocyte ratio (PLR), prognostic nutritional index (PNI), and plasma fibrinogen. A total of 440 patients (380 patients treated without neoadjuvant ADT and 60 patients treated with neoadjuvant ADT) were retrospectively evaluated in our medical center. Receiver operating characteristic (ROC) curves and Kaplan–Meier analyses were performed to compare the prognostic value of these scores. Univariate and multivariate Cox regression analyses were also performed.
Results: For all patients, dNLR and PNI were predictive of biochemical recurrence (P=0.041 and <0.001, respectively). Subgroup analysis of neoadjuvant strategies was also performed. For patients treated with neoadjuvant ADT, no selected inflammation-based scores were significantly correlated with biochemical recurrence (P>0.05). In contrast, for patients treated without neoadjuvant ADT, NLR (area under the ROC curve [AUC] =0.576, P=0.033), dNLR (P=0.585 and 0.017), PLR (AUC =0.582, P=0.024), and PNI (AUC =0.622, P<0.001) were predictive of biochemical recurrence. Kaplan–Meier analyses showed that dNLR (P=0.044), PLR (P=0.028), and PNI (P=0.004) were significantly associated with biochemical recurrence. Based on multivariable models, PNI was an independent predictor of biochemical recurrence (hazard ratio: 0.56, 95% confidence interval: 0.35–0.90, P=0.016).
Conclusion: High dNLR, high PLR, and low PNI were associated with poor biochemical recurrence-free survival in patients undergoing radical prostatectomy for high-risk localized prostate cancer not treated with neoadjuvant ADT. In particular, PNI was an independent prognostic factor for biochemical recurrence.
Keywords: biochemical recurrence, prostate cancer, derived neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, prognostic nutritional index
Introduction
Prostate cancer is the most common solid cancer and is the second highest leading cause of death in American men.1 It is also associated with the highest cancer incidence among Chinese men, and this incidence has been increasing over the last decade.2 The high prevalence of chronic inflammation in histopathological samples from prostate needle biopsies, transurethral resections of the prostate, and radical prostatectomies (RPs) implies a possible relationship between local inflammation and prostate cancer initiation and progression. This relationship has also been confirmed by epidemiologic3,4 and cellular/molecular studies.5,6 Several possible consequences of local inflammation during prostate cancer include genomic and cellular damage, the stimulation of new cell turnover, and the creation of an inflammation-associated microenvironment.5,6
Currently, tumor-associated inflammation, including both local and systemic, is considered as a key factor for tumor invasion, migration, and metastasis.7,8 The tumor microenvironment, which is mostly orchestrated by inflammatory cells, is now widely recognized as a key determinant of the neoplastic process, fostering proliferation, migration, and survival.8 Systemic inflammation has a substantial effect on survival outcomes in patients with various malignancies,9–13 including those with predominantly low- and intermediate-risk localized prostate cancer who underwent RP.4,14 Systemic inflammatory responses are found to be associated with the progression of cancer,8,15 and this can be measured by blood-based parameters, such as circulating inflammatory blood cells. The neutrophil-to-lymphocyte ratio (NLR), derived NLR (dNLR), platelet-to-lymphocyte ratio (PLR), prognostic nutritional index (PNI), and serum fibrinogen are significant markers of systemic inflammation.16
Many studies have shown that NLR and dNLR have prognostic value for metastatic castration-resistant prostate cancer with systemic therapy.3,17–21 Some studies demonstrated that high preoperative NLR is associated with poor survival in patients with localized prostate cancer who underwent RP.4,14,22 A few studies reported that PLR and fibrinogen have prognostic significance in terms of survival in patients with prostate cancer with androgen deprivation therapy (ADT) or radiotherapy.23–26
However, the prognostic significance of dNLR, PLR, PNI, and fibrinogen has not been previously investigated for patients with prostate cancer treated with RP and especially those in the high-risk group. A comparison of the prognostic value of selected inflammation-based scores has also never been explored for prostate cancer. Therefore, the present study aimed to evaluate and compare the prognostic value of selected inflammation-based scores with respect to biochemical recurrence in patients with high-risk localized prostate cancer treated with RP with/without neoadjuvant ADT.
Patients and methods
Ethics and patients
A total of 440 patients (380 patients treated without neoadjuvant ADT and 60 patients treated with neoadjuvant ADT) were included in this study from January 2009 to June 2016 in our center. The 60 patients received standard neoadjuvant ADT for 3–6 months before RP. These patients were treated with maximal androgen blockade (goserelin plus bicalutamide; 24 patients, 40.0%), antiandrogen therapy (bicalutamide; 12, 20.0%), medical castration only (goserelin; 20, 33.3%), and orchiectomy only (4, 6.7%). Included participants were male older than 18 years with pathologically proven high-risk localized prostate cancer (≥T3a or prostate-specific antigen [PSA] >20 ng/mL or Gleason score ≥8, according to the National Comprehensive Cancer Network [NCCN] classification system).27 All patients underwent RP, including open (163 patients, 37.0%), laparoscopic (167, 38%), and robot assisted (110, 25%). Peripheral blood cell counts were performed within 1 week before RP. The inclusion criteria were applied postoperatively. Patients with unavailable preoperative complete blood counts (n=3), other tumors (n=23), and a history of clinical systemic inflammatory diseases such as sarcoidosis, systemic lupus erythematosus, and rheumatoid arthritis (n=15) were excluded. The study received approval from the Ethics Committee of West China Hospital of Sichuan University, and written informed consent was obtained from all study participants.
Management of prostate cancer
Preoperative diagnosis was confirmed through ultrasound-guided transperineal needle prostate biopsy for all cases. Histopathological evaluation of needle samples was performed separately by two urological pathologists from our medical center. Baseline demographic, clinical, pathological, and biochemical data, which included PSA levels, were collected to ensure consistent data collection, through the use of uniform electronic templates, which could be obtained from the hospital information system of our center. The disease was staged according to the TNM staging system of 7th edition of the AJCC/UICC Cancer Staging Handbook.28
Follow-up
After initial pathological diagnosis, some patients received ADT due to high tumor burden prior to RP, whereas others did not. Therefore, patients were separated into the following two subgroups: patients with neoadjuvant ADT and patients without neoadjuvant ADT. After initial RP, all patients received regular follow-up visits. Patients with positive surgical margins or extracapsular extension received adjuvant therapy. PSA values were detected every month during the first 3 years, every 3 or 6 months for the next 5 years, and once per year thereafter. If disease progression was confirmed due to biochemical relapse or radiological progression using Response Evaluation Criteria in Solid Tumors (RECIST),29 adjuvant or salvage ADT or external beam radiotherapy was performed when necessary.
The atomic formulas of selected inflammation-based scores
As a part of clinical routine, fasting blood samples were collected within 7 days prior to RP or 3 days before prostate needle biopsy. NLR was the ratio of neutrophils to lymphocytes. dNLR was calculated as the absolute neutrophil count divided by (white blood cell − neutrophil count). PLR was the ratio of platelet to lymphocytes. PNI was calculated using the following equation: albumin (g/L) + (5× total lymphocyte count ×103/μL) or 10× serum albumin (g/dL) +0.005× total lymphocyte count (per mm3). The primary outcome was biochemical recurrence-free survival (BFS), which was defined as the time from prostatectomy to a serum PSA level of ≥0.2 ng/mL, as confirmed by repeat measurements.
Statistical analysis
To evaluate the prognostic values, we calculated receiver operating characteristic (ROC) curves and compared the area under the ROC curve (AUC) with a 95% confidence interval (CI). An AUC value of 0.5 indicated no predictive ability for the outcomes, and a value of 1.0 showed perfect discrimination. Cutoff points with the highest sensitivity and specificity were calculated. We generated BFS curves by the Kaplan–Meier method. Differences between the two curves were analyzed via the log-rank test. Univariate and multivariate Cox regression analyses also were performed. A two-sided P-value of <0.05 was considered statistically significant. We used MedCalc Statistical software (version 15.6; MedCalc Software, Ostend, Belgium), GraphPad Prism software (version 7.0; GraphPad Software, Inc., San Diego, CA, USA), SPSS software (version 22; IBM Corporation, Armonk, NY, USA), and R software (version 3.3.3; R Foundation for Statistical Computing, Vienna, Austria) for the statistical analyses.
Results
Patient and disease characteristics (n=440), both for the entire cohort and separated by neoadjuvant ADT, are presented in Table 1. A total of 134 (30.5%) patients had seminal vesicle invasion, and 185 (42%) patients had positive surgical margins. A pathological diagnosis of intraductal carcinoma of the prostate (IDC-P) occurred in 34 (7.7%) patients. Furthermore, 165 (37.5%) cases were classified as very high-risk disease according to the current NCCN recommendation.27 The mean levels of NLR, dNLR, PLR, PNI, and fibrinogen were 2.9 (standard deviation [SD]: 3.1, range: 0.6–26.5), 1.9 (SD: 1.6, range: 0.5–17.4), 104.3 (SD: 45.1, range: 21.3–304.0), 4.5 (SD: 2.1, range: 0.7–19.1), 49.8 (SD: 7.3, range: 3.75–85.2), and 290.4 mg/dL (SD: 73.5 mg/dL, range: 144–821 mg/dL), respectively. The median follow-up time was 31.0 months (interquartile range: 17.4–51.1 months). In total, biochemical recurrence occurred in 73 (19.2%) cases.
A total of 60 patients (13.6%) were treated with neoadjuvant ADT before RP. Patients treated with neoadjuvant ADT were significantly correlated with advanced T stage (T3) (P=0.014), higher incidence of extracapsular extension (P=0.011), higher PNI (P<0.0001), lower NLR (P=0.014), lower dNLR (P=0.001), and lower PLR (P=0.017).
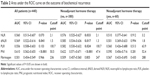
As shown in Figure 1, ROC curve analyses were performed to predict biochemical recurrence in patients with high-risk localized prostate cancer treated with RP with/without neoadjuvant ADT and then AUC measurements were compared (Table 2). First, for all included patients treated with or without neoadjuvant ADT, the AUC of dNLR for predicting biochemical recurrence was 0.569 (95% CI: 0.522–0.616; P=0.041). Furthermore, the AUC of PNI was 0.610 (95% CI: 0.562–0.655; P<0.001). For patients treated without neoadjuvant ADT, the AUC of NLR was 0.576 (95% CI: 0.525–0.627; P=0.033). The best cutoff value for NLR was 2.1, with a sensitivity of 64.4% and a specificity of 50.5%. Similarly, the AUC of dNLR was 0.585 (95% CI: 0.534–0.636; P=0.017), with a sensitivity of 87.7% and a specificity of 29.6%, based on a cut-off value of 1.3. The AUC of PLR was 0.582 (95% CI: 0.530–0.632; P=0.024). Based on a cut off value of 100.7 for PLR, the sensitivity was 64.4%, and the specificity was 55.4%. The area under the PNI ROC curve for predicting biochemical recurrence was 0.622 (95% CI: 0.571–0.671; P<0.001). When using a cutoff point of 47.4, the sensitivity was 41.1% and the specificity was 79.2%, with a Youden’s index of 0.203. Next, 94 (24.7%) patients with PNI ≤47.4 and 286 (75.3%) patients with PNI >47.4 were, respectively, classified into PNI-high and PNI-low groups. For this, the AUC measurement for fibrinogen to distinguish biochemical recurrence was 0.509 (P=0.805). Lastly, for patients treated with neoadjuvant ADT, there was no statistically significant difference between the AUC values of the selected inflammation-based scores (0.5).
Kaplan–Meier survival analyses of patients with high-risk prostate cancer who were treated with RP and neoadjuvant ADT are presented in Figure 2. dNLR, PLR, and PNI did not relate to BFS. However, when evaluating these parameters in patients treated without ADT, increased dNLR, increased PLR, and decreased PNI were found to be associated with poorer BFS. A significant difference in terms of BFS was found between the dNLR-low (26.3%, 100/380) and dNLR-high (73.6%, 280/380) groups (P=0.044). The PLR-low group (48.4%, 184/380) had a higher BFS than the PLR-high group (51.6%, 196/380; P=0.028). The BFS was significantly poorer in the PNI-low group (24.7%, 94/380) than in the PNI-high group (75.3%, 286/380; P=0.004), which revealed that PNI is a protective factor.
As shown in Table 3, for patients with high-risk localized prostate cancer treated with RP without neoadjuvant ADT, high PSA level, increased Gleason score, advanced pathological T stage, extracapsular extension, seminal vesicle invasion, positive surgical margin, perineural invasion, pathological subtype of IDC-P, high dNLR, high PLR, and low PNI were related to poorer BFS based on univariate models. Extracapsular extension, seminal vesicle invasion, positive surgical margin, and low PNI were also related to poorer BFS based on multivariable models. Furthermore, PNI was an independent predictor of BFS (hazard ratio: 0.56; 95% CI: 0.35–0.90, P=0.016).
Discussion
Our results demonstrated that dNLR, PLR, and PNI are predictive of biochemical recurrence in patients with high-risk localized prostate cancer who underwent RP and who were treated without neoadjuvant ADT. Furthermore, increased dNLR, increased PLR, and decreased PNI were associated with poor BFS in these patients. Particularly, low PNI was an independent prognostic risk factor for biochemical recurrence after adjusting for the effects of PSA levels and advanced pathological factors. To the best of our knowledge, this is the first study to show that dNLR and PLR are significantly associated with biochemical recurrence in patients with high-risk prostate cancer who underwent RP. More importantly, the present study represents the first attempt to evaluate the value of PNI as a predictor of biochemical recurrence in the same group of patients. Preoperative PNI values could become key complementary markers, in addition to TNM staging and PSA levels, for the selection of optimal treatment strategies. Thus, we recommend adding PNI to the traditional prognostic model to improve predictive accuracy.
Emerging evidence suggests that systemic inflammation plays an important role in the neoplastic process and survival in many types of solid tumors.10–13 Tumor cells release cytokines and chemokines that circulate and trigger a systemic inflammatory response.30 As a result, changes in neutrophils, lymphocytes, and platelets (among others) occur. Neutrophils play defined roles in the regulation of tumor cell proliferation and angiogenesis.31,32 Lymphocytes play a critical role in the control and integration of the systemic immune response.33,34 Platelets assist tumor cells in arresting at the endothelium of blood vessels and protect them from elimination, which contributes to tumor cell survival and spread.35,36
PNI is calculated based on the serum albumin and lymphocyte counts from peripheral blood samples. Serum albumin levels were found to be highly correlated with patient nutritional status, and low albumin indicated poorer nutritional status.37 Lymphocytes are responsible for immune responses,33,38 and play important roles in the systemic inflammatory response in patients with cancer.8 PNI values are closely related to the preoperative nutritional status, immune state of the body, and systemic inflammation, which could explain why low PNI was a risk factor for some extent.
In 1984, Onodera et al initially designed PNI to evaluate nutritional statuses and surgical risk prior to gastrointestinal surgery and regarded low PNI as a risk factor for survival.39,40 Recently, low PNI was found to be an independent risk factor for survival in patients with various types of solid tumors.41 In 2017, Fan et al42 first reported the value of PNI in the prostate cancer. They found that low PNI predicted poor overall survival and was an independent risk factor in metastatic castration-resistant prostate cancer treated with abiraterone, which is similar to the conclusion of our study. However, they explored the value of PNI in metastatic prostate cancer and not localized prostate cancer.
Many studies have shown that NLR is a poor risk factor for patients with prostate cancer.4,14,17–22 Some studies revealed that fibrinogen is associated with poor survival in prostate cancer patients treated with ADT or radiotherapy.25,26 In the present study, we observed that NLR is predictive of biochemical recurrence, but it was neither significantly associated with poorer biochemical recurrence nor an independent prognostic factor for biochemical recurrence. Meanwhile, fibrinogen was not found to be predictive of biochemical recurrence, associated with poorer biochemical recurrence, or an independent prognostic factor for biochemical recurrence. These results might be associated with the specific subgroup of prostate cancer patients, the high-risk group.
In this study, we focused on high-risk prostate cancer. The rates of positive surgical margin and extracapsular extension were similar to those of previous studies.43–45 In addition, our results revealed that all selected inflammation-based scores were not associated with biochemical recurrence in patients with high-risk localized prostate cancer treated with RP and ADT, which was confirmed by both ROC curve and Kaplan–Meier analyses. Thus, it might be not suitable to treat the inflammation-based scores as prognostic factors in patients treated with neoadjuvant therapy. This treatment likely has an impact on peripheral blood parameters. Therefore, inflammation-based scores calculated from the peripheral blood parameters prior to surgery failed to predict cancer survival.
There are some limitations of the study. First, it is a retrospective study. In addition, we determined the BFS and not metastasis-free survival or overall survival as the outcome due to a short follow-up duration. Moreover, we could not adjust for or analyze other baseline factors that might affect BFS. The sample size of the subgroup of patients treated with neoadjuvant ADT was also limited. Thus, additional large-scale and controlled clinical trials are required to confirm these results.
Conclusion
High dNLR, high PLR, and low PNI were associated with poor BFS in patients undergoing RP for high-risk localized prostate cancer not treated with neoadjuvant ADT. Particularly, PNI was an independent prognostic factor for biochemical recurrence in the same group of patients. Further prospective studies are needed to confirm whether improved PNI is associated with a long-term survival benefit.
Acknowledgments
No funding was received to support this research. We thank all patients enrolled in this study. KS and YZ were co-first authors.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. | ||
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. | ||
Van Soest RJ, Templeton AJ, Vera-Badillo FE, et al. Neutrophil-to-lymphocyte ratio as a prognostic biomarker for men with metastatic castration-resistant prostate cancer receiving first-line chemotherapy: Data from two randomized phase III trials. Ann Oncol. 2015;26(4):743–749. | ||
Jang WS, Cho KS, Kim KH, et al. Prognostic impact of preoperative neutrophil-to-lymphocyte ratio after radical prostatectomy in localized prostate cancer. Prostate Cancer Prostatic Dis. 2016;19(3):298–304. | ||
Klein EA, Silverman R. Inflammation, infection, and prostate cancer. Curr Opin Urol. 2008;18(3):315–319. | ||
Caruso C, Balistreri CR, Candore G, et al. Polymorphisms of pro-inflammatory genes and prostate cancer risk: a pharmacogenomic approach. Cancer Immunol Immun. 2009;58(12):1919–1933. | ||
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–545. | ||
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. | ||
Deans C, Wigmore SJ. Systemic inflammation, cachexia and prognosis in patients with cancer. Curr Opin Clin Nutr. 2005;8(3):265–269. | ||
Templeton AJ, McNamara MG, Seruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):124. | ||
Song A, Eo W, Lee S. Comparison of selected inflammation-based prognostic markers in relapsed or refractory metastatic colorectal cancer patients. World J Gastroenterol. 2015;21(43):12410–12420. | ||
Crumley AB, McMillan DC, McKernan M, McDonald AC, Stuart RC. Evaluation of an inflammation-based prognostic score in patients with inoperable gastro-oesophageal cancer. Br J Cancer. 2006;94(5):637–641. | ||
Roxburgh CS, Salmond JM, Horgan PG, Oien KA, McMillan DC. Comparison of the prognostic value of inflammation-based pathologic and biochemical criteria in patients undergoing potentially curative resection for colorectal cancer. Ann Surg. 2009;249(5):788–793. | ||
Lee H, Jeong SJ, Hong SK, Byun SS, Lee SE, Oh JJ. High preoperative neutrophil-lymphocyte ratio predicts biochemical recurrence in patients with localized prostate cancer after radical prostatectomy. World J Urol. 2016;34(6):821–827. | ||
Mantovani A. Cancer: inflaming metastasis. Nature. 2009;457(7225):36–37. | ||
Sciarra A, Gentilucci A, Salciccia S, et al. Prognostic value of inflammation in prostate cancer progression and response to therapeutic: a critical review. J Inflamm (Lond). 2016;13(1):35. | ||
Keizman D, Gottfried M, Ish-Shalom M, et al. Pretreatment neutrophil-to-lymphocyte ratio in metastatic castration-resistant prostate cancer patients treated with ketoconazole: association with outcome and predictive nomogram. Oncologist. 2012;17(12):1508–1514. | ||
Nuhn P, Vaghasia AM, Goyal J, et al. Association of pretreatment neutrophil-to-lymphocyte ratio (NLR) and overall survival (OS) in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with first-line docetaxel. BJU Int. 2014;114(6b):E11–E17. | ||
Sonpavde G, Pond GR, Armstrong AJ, et al. Prognostic impact of the neutrophil-to-lymphocyte ratio in men with metastatic castration-resistant prostate cancer. Clin Genitourin Cancer. 2014;12(5):317–324. | ||
Templeton AJ, Pezaro C, Omlin A, et al. Simple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratio. Cancer. 2014;120(21):3346–3352. | ||
Boegemann M, Schlack K, Thomes S, et al. The role of the neutrophil to lymphocyte ratio for survival outcomes in patients with metastatic castration-resistant prostate cancer treated with Abiraterone. Int J Mol Sci. 2017;18(2):380. | ||
Gazel E, Tastemur S, Acikgoz O, et al. Importance of neutrophil/lymphocyte ratio in prediction of PSA recurrence after radical prostatectomy. Asian Pac J Cancer Prev. 2015;16(5):1813–1816. | ||
Langsenlehner T, Pichler M, Thurner EM, et al. Evaluation of the platelet-to-lymphocyte ratio as a prognostic indicator in a European cohort of patients with prostate cancer treated with radiotherapy. Urol Oncol. 2015;33(5):9–16. | ||
Wang Y, Xu F, Pan J, et al. Platelet to lymphocyte ratio as an independent prognostic indicator for prostate cancer patients receiving androgen deprivation therapy. BMC Cancer. 2016;16:329. | ||
Thurner EM, Krenn-Pilko S, Langsenlehner U, et al. The association of an elevated plasma fibrinogen level with cancer-specific and overall survival in prostate cancer patients. World J Urol. 2015;33(10):1467–1473. | ||
Wang Y, Yin W, Wang Z, et al. Pretreatment plasma fibrinogen as an independent prognostic indicator of prostate cancer patients treated with androgen deprivation therapy. Prostate Cancer Prostatic Dis. 2016;19(2):209–215. | ||
National Comprehensive Cancer Network. (NCCN). Clinical Practice Guidelines in Oncology. Prostate Cancer, Version 2; 2017. Available from: https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed April 17, 2017. | ||
Edge S, Byrd D, Compton C. AJCC Cancer Staging Handbook. 7th ed. New York, NY: Springer; 2010. | ||
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. | ||
Salazar-Onfray F, Lopez MN, Mendoza-Naranjo A. Paradoxical effects of cytokines in tumor immune surveillance and tumor immune escape. Cytokine Growth Factor Rev. 2007;18(1–2):171–182. | ||
Gregory AD, Houghton AM. Tumor-associated neutrophils: new targets for cancer therapy. Cancer Res. 2011;71(7):2411–2416. | ||
Cools-Lartigue J, Spicer J, McDonald B, et al. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J Clin Invest. Epub 2013 Jul 1. | ||
Butcher EC, Picker LJ. Lymphocyte homing and homeostasis. Science. 1996;272(5258):60–66. | ||
Stulting RD, Berke G. Nature of lymphocyte-tumor interaction. A general method for cellular immunoabsorption. J Exp Med. 1973;137(4):932–942. | ||
Battinelli EM, Markens BA, Italiano JE Jr. Release of angiogenesis regulatory proteins from platelet alpha granules: modulation of physiologic and pathologic angiogenesis. Blood. 2011;118(5):1359–1369. | ||
Gay LJ, Felding-Habermann B. Contribution of platelets to tumour metastasis. Nat Rev Cancer. 2011;11(2):123–134. | ||
Bistrian BR, Blackburn GL, Hallowell E, Heddle R. Protein status of general surgical patients. JAMA. 1974;230(6):858–860. | ||
Gowans JL, Mc GD, Cowen DM. Initiation of immune responses by small lymphocytes. Nature. 1962;196:651–655. | ||
Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139(1):160–167. | ||
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai zasshi. 1984;85(9):1001–1005. | ||
Sun K, Chen S, Xu J, Li G, He Y. The prognostic significance of the prognostic nutritional index in cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2014;140(9):1537–1549. | ||
Fan L, Wang X, Chi C, et al. Prognostic nutritional index predicts initial response to treatment and prognosis in metastatic castration-resistant prostate cancer patients treated with abiraterone. Prostate. 2017;77(12):1233–1241. | ||
Ku JH, Jeong CW, Park YH, Cho MC, Kwak C, Kim HH. Biochemical recurrence after radical prostatectomy with or without pelvic lymphadenectomy in Korean men with high-risk prostate cancer. Jpn J Clin Oncol. 2011;41(5):656–662. | ||
Harty NJ, Kozinn SI, Canes D, Sorcini A, Moinzadeh A. Comparison of positive surgical margin rates in high risk prostate cancer: open versus minimally invasive radical prostatectomy. Int Braz J Urol. 2009;39(5):639–646. | ||
Hussain M, Tangen CM, Thompson IM Jr, et al. Phase III intergroup trial of adjuvant androgen deprivation with or without mitoxantrone plus prednisone in patients with high-risk prostate cancer after radical prostatectomy: SWOG S9921. J Clin Oncol. Epub April 6, 2018. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.