Back to Journals » OncoTargets and Therapy » Volume 11
Prognostic and clinicopathological value of SIRT3 expression in various cancers: a systematic review and meta-analysis
Authors Zhou Y, Cheng S, Chen S, Zhao Y
Received 22 November 2017
Accepted for publication 5 March 2018
Published 13 April 2018 Volume 2018:11 Pages 2157—2167
DOI https://doi.org/10.2147/OTT.S157836
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ingrid Espinoza
Yongping Zhou,1 Sijin Cheng,2 Sinuo Chen,2 Yongzhao Zhao1,2
1Department of Hepatobiliary, Wuxi Second Hospital, Nanjing Medical University, Wuxi, People’s Republic of China; 2Tongji University School of Medicine, Shanghai, China
Background: Several studies have explored the prognostic value of sirtuin 3 (SIRT3) in various cancers, but obtained inconsistent results. The current systematic review and meta-analysis was conducted to investigate the association between SIRT3 expression and prognosis in various cancers.
Methods: PubMed, Embase, Web of Science and the Cochrane Library were comprehensively retrieved by the end of September 29, 2017. All the relevant studies were checked and included in the meta-analysis if they met the inclusion criteria.
Results: A total of 17 studies involving 2,865 patients were included in the systematic review and meta-analysis. The results indicated that SIRT3 expression was not significantly associated with overall survival (OS) (hazard ratio [HR]=0.87, 95% CI=0.59–1.29, P=0.50) and disease-free survival (HR=0.87, 95% CI=0.57–1.31, P=0.50) in total various cancers. However, significant relationship between SIRT3 expression and OS in specific cancers was detected, including chronic lymphocytic leukemia (CLL) (HR=0.48, 95% CI=0.26–0.89, P=0.019), hepatocellular carcinoma (HCC) (HR=0.56, 95% CI=0.42–0.74, P<0.001), pancreatic carcinoma (PC) (HR=0.55, 95% CI=0.30–1.00, P=0.049), renal cell carcinoma (RCC) (HR=0.13, 95% CI=0.02–0.98, P=0.048), breast cancer (BC) (HR=2.53, 95% CI=1.83–3.67, P<0.001), colon cancer (CC) (HR=1.87, 95% CI=1.12–3.26, P=0.022) and non-small-cell lung cancer (NSCLC) (HR=2.20, 95% CI=1.38–3.50, P=0.001). Moreover, SIRT3 expression was obviously associated with tumor size (odds ratio [OR]=1.41, 95% CI=1.02–1.94, P=0.04), tumor differentiation (OR=1.52, 95% CI=1.08–2.16, P=0.02) and clinical stage (OR=2.07, 95% CI=1.23–3.46, P=0.01) in HCC.
Conclusion: SIRT3 was distinctly related to the OS in specific cancers. SIRT3 was an unfavorable prognostic factor in BC, CC and NSCLC; however, it was also a favorable prognostic factor in CLL, HCC, PC and RCC, especially in HCC.
Keywords: SIRT3, cancer, prognostic, clinicopathological, overall survival, meta-analysis
Introduction
Cancer is a major public health problem and the second leading cause of death in the US. It is estimated that 1,688,780 Americans will be newly diagnosed with cancers and 600,920 Americans will die from cancers in 2017.1 Despite enormous progress has been made in the diagnosis and therapy, the ending of most cancer patients remains disappointing. In consideration of the current situation, the prognostic factors, able to predict the clinical outcomes and guide the therapy, are drawing a majority of researcher’s attention.2–9
Sirtuins, a family of NAD+-dependent deacetylases, regulate multiple signaling pathways’ cellular biology including cellular proliferation, metabolism, stress reaction and oxidation resistance.10–14 Seven isoforms of sirtuins (SIRT1–7) have been described in mammals. Among them, SIRT1 and SIRT2 are located preponderantly in the nucleus and cytosol, respectively. The remaining 3 sirtuins, SIRT3, SIRT4 and SIRT5, are located in the mitochondria.15 Among this deacetylase family, SIRT3 is of particular interest. SIRT3 is synthesized as a 44 kDa peptide with an N-terminal sequence, which is the primary mitochondrial deacetylase and modulates the acetylation level of multiple mitochondrial proteins.16 SIRT3 plays a critical role in various cellular activities, including cell proliferation, apoptosis and stress reaction.15,17 Owing to the important role of SIRT3 in cellular pathways, previous studies have testified that SIRT3 participated in the development of various diseases, such as diabetes18 and myocardial injury.19 In recent years, SIRT3 attracted researchers’ attention on account of its dual role in tumorigenesis.10,17,20,21 A great number of studies have been conducted to investigate the association between SIRT3 and tumorigenesis of various cancers, including hepatocellular carcinoma (HCC),22 lung cancer,23 gastric cancer (GC)24 and breast cancer (BC).25 However, the results were controversial. Zhang et al22 collected 248 primary HCC specimens and found the patients with high SIRT3 expression tended to have longer overall survival (OS) compared to patients with low SIRT3 expression (hazard ratio [HR]=0.56, 95% CI=0.34–0.90, P=0.016). Similarly, Jeh et al26 validated that renal cell carcinoma (RCC) patients with high SIRT3 expression had longer OS (HR=0.13, 95% CI=0.02–0.94, P=0.047). However, different observations were made in other studies. He et al27 performed a study comprising 308 patients with BC to explore the correlation between SIRT3 expression and prognosis and unexpectedly found that BC patients with high SIRT3 expression possessed shorter OS compared to patients with low SIRT3 expression, which indicated that SIRT3 might reduce OS and be a unfavorable prognostic biomarker (HR=2.53, 95% CI=1.83–3.67, P<0.001). Coincidentally, the results of Yang et al39 study reaffirmed the conclusion that SIRT3 might be a tumor promoter and could reduce the prognosis of cancer patients (HR=2.20, 95% CI=1.38–3.50, P=0.001). In view of the abovementioned controversial results, the dispute on the prognostic value of SIRT3 in various cancers spontaneously arises.
In view of the discrepancy, the current systematic review and meta-analysis was conducted to investigate the association between SIRT3 expression and prognosis in various cancers.
Materials and methods
Literature search strategy
PubMed, Embase, Web of Science and the Cochrane Library were comprehensively searched by the end of September 29, 2017. The search terms were as follows: “SIRT3”, “silent mating type information regulation 2 homolog 3”, “SIR2L3” OR “sirtuin 3” combining with “tumor”, “carcinoma” OR “cancer”. The references of the retrieved articles were also checked to avoid missing relevant studies.
Inclusion and exclusion criteria
The study would be included in this systematic review and meta-analysis if it met all the following criteria: 1) observational studies with cohorts; 2) investigating the relationship between SIRT3 expression and prognosis in various cancers; 3) covering treatment-free survival (TFS), recurrence-free survival (RFS), OS, disease-free survival (DFS), time to recurrence (TTR), cancer-specific survival (CSS) or clinicopathological parameters and 4) with full text. The exclusion criteria were as follows: duplicate publications, reviews, case reports, animal experiments, cell experiments and inefficient data.
Data extraction and quality assessment
An extraction template was designed in advance, and then 2 reviewers extracted the following data independently: the family name of the first author, publication year, country, ethnicity, sample size, the percentage of the male, the percentage of the patients with high SIRT3 expression level, cutoff value, clinical outcomes, cancer type and analysis model and information needed to evaluate the quality of each study. Any discrepancies during study selection and data extraction were resolved by discussion with the third reviewer. The HRs along with 95% CI obtained directly from published articles were integrated in the meta-analysis according to the study conducted by Tierney et al.28 Two reviewers evaluated all the included studies independently after reading the full text of each study. The Newcastle–Ottawa scale (NOS) was utilized to assess the quality of the included studies.29
Statistical analysis
All pooled analyses were conducted using Review Manager 5.3 (Cochrane Collaboration; UK) and STATA 12.0 software (StataCorp LP, College Station, TX, USA). For prognostic index, eg, OS, HR and corresponding 95% CI were used as the summary measure. For clinical parameters, dichotomous, the odds ratio (OR) and corresponding 95% CI were used to analyze the results. Chi-square test and I2 statistic were utilized to evaluate the interstudy heterogeneity. I2 equal to or less than 50% indicated that the heterogeneity was not statistically obvious, and the fixed-effect model was employed. If not, the random-effect model was applied. Begg’s test and Egger’s test conducted by STATA 12.0 were applied to assess the publication bias among the included studies. Sensitivity analysis performed by STATA 12.0 was applied to confirm the robustness of the results.
Results
Selection and characteristics of the included studies
This study complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for reporting systemic review and meta-analysis.30 The process of literature search is shown in Figure 1. In total, 798 papers were initially retrieved. Then, 578 papers remained when 220 duplicates were removed. Regarding the remaining 578 papers, titles or abstracts of them were screened and 532 were directly excluded for not concerning this topic. The full text of the remaining 46 papers was carefully read, and 29 papers were abandoned for the following reasons: 22 papers not focusing on this topic and 7 papers for inefficient data. Ultimately, 17 studies involving 2,865 patients were included into this systematic review and meta-analysis.22–27,31–41
  | Figure 1 Flow diagram of study selection process. |
The characteristics of included studies are presented in Table 1. Throughout these studies, 15 and 2 studies were carried out in Asian people22–24,26,27,31–34,36–41 and Caucasian people,25,35 respectively. Additionally, the sample size varied a lot among the included studies, from 30 to 350. In total, 15 studies reported the percentage of male, from 0% to 88.71%.22–27,32–34,36–41 Moreover, 15 studies illustrated the percentage of patients with high SIRT3 expression, varying from 25.81% to 60.00%.22–27,31–34,36–40 With respect to prognostic outcomes, 14 studies reported clinicopathological parameters,22,23,25–27,31–34,36–40 11 studies covered OS,22,24,27,31–33,35–37,39,41 1 covered CSS,26 2 reported DFS,24,27 1 covered RFS,22 1 reported TFS and 1 covered TTR.36 Furthermore, as for cancer type, 9 cancers were investigated, including chronic lymphocytic leukemia (CLL),35 HCC,22,40 esophageal cancer (EC),37,41 GC,31,38 BC,25,27 colon cancer (CC),33 pancreatic carcinoma (PC),32 RCC26 and non-small-cell lung cancer (NSCLC).23,39 In terms of analysis model, OS was analyzed using multivariate analysis in 10 studies22,26,27,31–33,36,37,39,41 and using univariate analysis in 2 studies.24,35 NOS used for evaluating quality of included studies varied from 5 to 8.
Meta-analysis of OS
A total of 11 studies covered the OS and 1 study presented CSS; hence, 12 studies containing 2,352 patients were involved in the meta-analysis of OS. As shown in Figure 2, random-effect model was used for the evident heterogeneity (I2=89%). The results indicated that the SIRT3 expression was not significantly associated with OS (HR=0.87, 95% CI=0.59–1.29, P=0.50). The sensitivity analysis conducted by STATA 12.0 confirmed the robustness of the results (Figure 3). Moreover, as shown in Figure 4, no obvious publication bias was detected among included studies based on the results of Begg’s test (P=0.945) and Egger’s test (P=0.344).
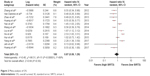  | Figure 2 Meta-analysis of OS. |
  | Figure 3 Influence analysis of OS. |
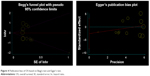  | Figure 4 Publication bias of OS based on Begg’s test and Egger’s test. |
In view of the distinct heterogeneity of OS, the subgroup analysis was conducted to further explore the relationship between SIRT3 expression and various cancers. As shown in Table 2, the subgroup analyses were implemented based on analysis model, ethnicity, sample size and cancer type. Regarding analysis model, no statistically evident correlation was detected between SIRT3 expression neither when using multivariate analysis model (P=0.657) nor when using univariate analysis model (P=0.404). Similarly, there was no obvious relationship between SIRT3 expression and OS in cancer patients whether the sample size was greater (P=0.526) or less than 200 (P=0.698). Regarding the ethnicity, the results presented that patients with high SIRT3 expression might have obviously longer OS compared to patients with low SIRT3 expression in Caucasian (P=0.019); however, no relationship between SIRT3 expression and OS was observed in Asian (P=0.685). Furthermore, the subgroup analyses classified by cancer type validated that high SIRT3 expression was a favorable prognostic factor in patients with CLL (P=0.019), HCC (P<0.001), PC (P=0.049) and RCC (P=0.048). Nevertheless, the results also indicated that high SIRT3 expression was also an unfavorable prognostic factor in BC (P<0.001), CC (P=0.022) and NSCLC (P=0.001). In addition, there was no significant association between SIRT3 expression and OS in patients with EC (P=0.806) and GC (P=0.347).
Meta-analysis of DFS
Among the 17 studies, 2 reported DFS, 1 covered RFS, 1 reported TFS and 1 covered TTR, and all these 5 studies were integrated into the meta-analysis of DFS. As shown in Figure 5, the random-effect model was used for the distinct heterogeneity (I2=83%). The results demonstrated that there was no relationship between SIRT3 expression and DFS in patients with various cancers (HR=0.87, 95% CI=0.57–1.31, P=0.50). The sensitivity analysis tested the robustness of the results (Figure 6). As shown in Figure 7, there was no obvious publication bias among included studies based on the results of Begg’s test (P=1.000) and Egger’s test (P=0.901).
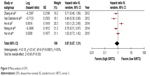  | Figure 5 Meta-analysis of DFS. |
  | Figure 6 Influence analysis of DFS. |
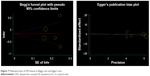  | Figure 7 Publication bias of DFS based on Begg’s test and Egger’s test. |
Meta-analysis of clinicopathological parameters
Among the included studies, 14 studies reported data about the relationship between SIRT3 expression and clinicopathological parameters, and the main clinicopathological parameters in this meta-analysis included age, sex, tumor size, tumor differentiation, clinical stage, vascular invasion, cirrhosis, alpha fetal protein (AFP) and hepatitis B virus (HBV) infection. As listed in Table 3, the results indicated that there was no significant relationship between SIRT3 expression and all abovementioned clinicopathological parameters. Now that significant association between SIRT3 expression and OS was observed in HCC patients, a subgroup analysis of clinicopathological parameters focusing on HCC patients was performed. The results demonstrated that HCC patients with high SIRT3 expression tended to be associated with smaller tumor size (OR=1.41, 95% CI=1.02–1.94, P=0.04; I2=46%), better tumor differentiation (OR=1.52, 95% CI=1.08–2.16, P=0.02; I2=50%) and earlier clinical stage (OR=2.07, 95% CI=1.23–3.46, P=0.01; I2=0%). However, no relationship was detected between SIRT3 expression and cirrhosis (P=0.71), and similar result was found in terms of AFP (P=0.48) and HBV infection (P=0.14) in HCC.
Discussion
SIRT3, an arresting member of the sirtuins family located in mitochondria, plays a critical role in multiple cellular activities such as energy metabolism, cell proliferation and cell apoptosis.11–13,15–17 Recently, SIRT3 is gaining attention from more and more researchers due to its dual role in tumorigenesis.22–24,26,33–41
In the current study, we validated that SIRT3 expression might not be related to the prognosis in various cancers, which was in accordance with the previous meta-analysis.42 Regarding the subgroup analyses of OS, we found the high SIRT3 expression might be a favorable factor in Caucasian. However, it should be noted that only 1 study focusing on CLL was included into these subgroups; therefore, the conclusion was not quite unconvincing. It is worth mentioning that we noticed significant correlation between SIRT3 expression and prognosis in several specific cancers. The results manifested that SIRT3 might be a tumor suppressor in CLL, HCC, PC and RCC. Conversely, the results also indicated that SIRT3 might promote the cancer development and decrease the OS in patients with BC, CC or NSCLC. Meanwhile, no obvious relationship between SIRT3 expression and clinicopathological parameters in total various cancers was detected in the current study.
Yu et al42 previously performed a meta-analysis involving 15 studies to explore the prognostic value of SIRT3 in various cancers and found no distinct relationship between SIRT3 expression and OS. Despite similar results, there were several differences between the current study and the previous meta-analysis.42 First, in the previous meta-analysis, although the authors declared that 15 studies were included in the previous study, only 7 studies were analyzed in the meta-analysis of OS. The small population certainly reduced the convincing of the conclusion and restricted its clinical application. However, in the current study, 12 studies comprising 2,352 patients were involved in the meta-analysis of OS, and the results were clear and convincing. Second, Chinese databases such as China National Knowledge Infrastructure and Wanfang Data were searched in the previous studies, which might increase the selection bias in the previous meta-analysis. More importantly, 2 dissertations without peer-reviewed process were included into the previous meta-analysis, which decreases the persuasion of the conclusion to a great extent. Third, the quality assessment by NOS, the meta-analysis of DFS and the publication bias based on Begg’s test and Egger’s test were performed in the current meta-analysis, which was not reported in the previous meta-analysis. Hence, the methodology of the current study was more normative, and the conclusion could be drawn for enough credibility.
In spite of the numerous relative studies focusing on the prognostic role of SIRT3 in cancers, the underlying mechanism remains unclear. The complex mechanism might be on account of multiple biological roles of SIRT3 in cellular pathways, including cell proliferation, apoptosis and metabolism.12,17,18,43 In the current study, we discovered that SIRT3 functioned as a tumor suppressor or a tumor promoter in specific cancers, which indicated that SIRT3 might be involved with different signaling pathways in specific cancers. Regarding BC, Wei et al44 focused on the association between cell metabolism and cancers, and they discovered that SIRT3 played a vital role in the BC cell proliferation, and the results indicated that oroxylin A inhibits glycolysis-dependent proliferation of BC cells through the suppression of HIF1α stabilization via SIRT3 activation. In addition, SIRT3 is absolutely necessary in the regulation of reactive oxygen species (ROS) production. Torrens-Mas et al45 discovered that SIRT3 could be a therapeutic target for BC and improve the effectiveness of cisplatin (CDDP) and tamoxifen (TAM) treatments based on the ROS production. With regard to HCC, the study conducted by Liu et al found that the expression of SIRT3 was lower in HCC tissue than in non-HCC tissue, which manifested that SIRT3 was involved in the development of HCC and that SIRT3 acted as a tumor suppressor in HCC. Further in vitro experiments indicated that SIRT3 could inhibit the growth and proliferation of HepG2 cells and induce cell apoptosis,46 which was consistent with our results. Similarly, Song et al34 analyzed 60 HCC specimens and discovered that high SIRT3 expression was an unfavorable factor, and their further research validated that SIRT3 inhibited cell growth through the glycogen synthase kinase-3β/BCL2-associated X protein-dependent apoptotic pathway, which was in accordance with the viewpoint that the prognostic value of SIRT3 in specific cancers might be associated with the regulation of metabolism. In the current study, we also detected that HCC patients with high SIRT3 expression had longer OS, smaller tumor size, better tumor differentiation and earlier clinical stage compared to those with low SIRT3 expression. In view of the limited population, more studies should be carried out to ascertain the prognostic value of SIRT3 in HCC. Furthermore, other researchers testified that SIRT3 also acted as a tumor suppressor in RCC by regulating glutamine-derived mitochondrial respiration.26,47 Conversely, Liu et al33 analyzed 127 patients with CC and discovered that patients with high SIRT3 expression had a better OS, which suggested that high SIRT3 expression was an unfavorable factor in CC, and similar result was observed in a study by Yan et al,37 which found that high SIRT3 expression was associated with worse prognosis in EC. Taken together, despite the discrepancy, extensive studies have demonstrated that SIRT3 expression was significantly related to OS in specific cancers.
There are some highlights in the current study. First, a total of 2,865 patients were finally included into the meta-analysis and the conclusion was convincing enough. Second, comprehensive subgroup analyses of OS and clinicopathological parameters were performed to elucidate this issue, which increased clinical application value of the conclusion. Nevertheless, the current study was not without drawbacks. The cutoff values of SIRT3 expression varied a lot in some included studies. Hence, the clinical applicability of the conclusion was affected. In addition, the sample size of some subgroup analyses was relatively small, which might lower the influence of the results. Last but not least, the previous report did not show the detailed characteristics of various cancers, which might affect the reliability of the conclusion. Despite the abovementioned shortcomings, the current meta-analysis still gave more convincing evidence on the prognostic role of SIRT3 in various cancers and could help researchers to catch the important development in this filed.
Conclusion
There was no evident relationship between the SIRT3 expression and prognosis in total cancers. However, SIRT3 expression might be a critical prognostic factor in specific cancers, including CLL, HCC, BC, CC, PC, NSCLC and RCC, especially in HCC. More clinical cohort studies with large population size and strict methodology should be carried out to clarify the issues in future.
Acknowledgment
The study was supported by Science and Technology Development Fund of Nanjing Medical University (Key Project) (No 2017NJMUZD117).
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. | ||
Chen S, Zhang L, Yan G, et al. Neutrophil-to-lymphocyte ratio is a potential prognostic biomarker in patients with ovarian cancer: a meta-analysis. Biomed Res Int. 2017;2017:7943467. | ||
Wang J, Zhao Y, Qi R, et al. Prognostic role of podocalyxin-like protein expression in various cancers: a systematic review and meta-analysis. Oncotarget. 2016;8(32):52457–52464. | ||
Zhao Y, Si G, Zhu F, et al. Prognostic role of platelet to lymphocyte ratio in hepatocellular carcinoma: a systematic review and meta-analysis. Oncotarget. 2017;8(14):22854–22862. | ||
Kim HM, Lee J, Koo JS. Clinicopathological and prognostic significance of programmed death ligand-1 expression in breast cancer: a meta-analysis. BMC Cancer. 2017;17(1):690. | ||
Li N, Shi K, Kang X, Li W. Prognostic value of long non-coding RNA TUG1 in various tumors. Oncotarget. 2017;8(39):65659–65667. | ||
Wang C, Yang W, Dong F, et al. The prognostic role of Sirt1 expression in solid malignancies: a meta-analysis. Oncotarget. 2017;8(39):66343–66351. | ||
Wang J, Liu Y, Zhang N, et al. Prognostic role of pretreatment platelet to lymphocyte ratio in urologic cancer. Oncotarget. 2017;8(41):70874–70882. | ||
Zhou Q, Hong L, Zuo MZ, He Z. Prognostic significance of neutrophil to lymphocyte ratio in ovarian cancer: evidence from 4,910 patients. Oncotarget. 2017;8(40):68938–68949. | ||
Chen Y, Fu LL, Wen X, et al. Sirtuin-3 (SIRT3), a therapeutic target with oncogenic and tumor-suppressive function in cancer. Cell Death Dis. 2014;5:e1047. | ||
Bordo D. Structure and evolution of human sirtuins. Curr Drug Targets. 2013;14(6):662–665. | ||
Choi JE, Mostoslavsky R. Sirtuins, metabolism, and DNA repair. Curr Opin Genet Dev. 2014;26:24–32. | ||
Li Y, Liu T, Liao S, et al. A mini-review on sirtuin activity assays. Biochem Biophys Res Commun. 2015;467(3):459–466. | ||
Pirinen E, Lo Sasso G, Auwerx J. Mitochondrial sirtuins and metabolic homeostasis. Best Pract Res Clin Endocrinol Metab. 2012;26(6):759–770. | ||
Alhazzazi TY, Kamarajan P, Verdin E, Kapila YL. SIRT3 and cancer: tumor promoter or suppressor? Biochim Biophys Acta. 2011;1816(1):80–88. | ||
Ahn BH, Kim HS, Song S, et al. A role for the mitochondrial deacetylase Sirt3 in regulating energy homeostasis. Proc Natl Acad Sci U S A. 2008;105(38):14447–14452. | ||
Xiong Y, Wang M, Zhao J, Han Y, Jia L. Sirtuin 3: a Janus face in cancer (Review). Int J Oncol. 2016;49(6):2227–2235. | ||
Jing E, Emanuelli B, Hirschey MD, et al. Sirtuin-3 (Sirt3) regulates skeletal muscle metabolism and insulin signaling via altered mitochondrial oxidation and reactive oxygen species production. Proc Natl Acad Sci U S A. 2011;108(35):14608–14613. | ||
Sundaresan NR, Samant SA, Pillai VB, Rajamohan SB, Gupta MP. SIRT3 is a stress-responsive deacetylase in cardiomyocytes that protects cells from stress-mediated cell death by deacetylation of Ku70. Mol Cell Biol. 2008;28(20):6384–6401. | ||
Lee DY, Jung DE, Yu SS, Lee YS, Choi BK, Lee YC. Regulation of SIRT3 signal related metabolic reprogramming in gastric cancer by Helicobacter pylori oncoprotein CagA. Oncotarget. 2017;8(45):78365–78378. | ||
Alhazzazi TY, Kamarajan P, Joo N, et al. Sirtuin-3 (SIRT3), a novel potential therapeutic target for oral cancer. Cancer. 2011;117(8):1670–1678. | ||
Zhang CZ, Liu L, Cai M, et al. Low SIRT3 expression correlates with poor differentiation and unfavorable prognosis in primary hepatocellular carcinoma. PLoS One. 2012;7(12):e51703. | ||
Xiong Y, Wang M, Zhao J, et al. SIRT3 is correlated with the malignancy of non-small cell lung cancer. Int J Oncol. 2017;50(3):903–910. | ||
Hur H, Kim YB, Ham IH, Lee D. Loss of ACSS2 expression predicts poor prognosis in patients with gastric cancer. J Surg Oncol. 2015;112(6):585–591. | ||
Desouki MM, Doubinskaia I, Gius D, Abdulkadir SA. Decreased mitochondrial SIRT3 expression is a potential molecular biomarker associated with poor outcome in breast cancer. Hum Pathol. 2014;45(5):1071–1077. | ||
Jeh SU, Park JJ, Lee JS, et al. Differential expression of the sirtuin family in renal cell carcinoma: aspects of carcinogenesis and prognostic significance. Urol Oncol. 2017;35(12):675.e9–675.e15. | ||
He S, He C, Yuan H, Xiong S, Xiao Z, Chen L. The SIRT 3 expression profile is associated with pathological and clinical outcomes in human breast cancer patients. Cell Physiol Biochem. 2014;34(6):2061–2069. | ||
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. | ||
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. | ||
Huang KH, Hsu CC, Fang WL, et al. SIRT3 expression as a biomarker for better prognosis in gastric cancer. World J Surg. 2014;38(4):910–917. | ||
Huang S, Chen X, Zheng J, et al. Low SIRT3 expression contributes to tumor progression, development and poor prognosis in human pancreatic carcinoma. Pathol Res Pract. 2017;213(11):1419–1423. | ||
Liu C, Huang Z, Jiang H, Shi F. The sirtuin 3 expression profile is associated with pathological and clinical outcomes in colon cancer patients. Biomed Res Int. 2014;2014:871263. | ||
Song CL, Tang H, Ran LK, et al. Sirtuin 3 inhibits hepatocellular carcinoma growth through the glycogen synthase kinase-3β/BCL2-associated X protein-dependent apoptotic pathway. Oncogene. 2016;35(5):631–641. | ||
Van Damme M, Crompot E, Meuleman N, et al. HDAC isoenzyme expression is deregulated in chronic lymphocytic leukemia B-cells and has a complex prognostic significance. Epigenetics. 2012;7(12):1403–1412. | ||
Wang JX, Yi Y, Li YW, et al. Down-regulation of sirtuin 3 is associated with poor prognosis in hepatocellular carcinoma after resection. BMC Cancer. 2014;14:297. | ||
Yan SM, Han X, Han PJ, Chen HM, Huang LY, Li Y. SIRT3 is a novel prognostic biomarker for esophageal squamous cell carcinoma. Med Oncol. 2014;31(8):103. | ||
Yang B, Fu X, Shao L, Ding Y, Zeng D. Aberrant expression of SIRT3 is conversely correlated with the progression and prognosis of human gastric cancer. Biochem Biophys Res Commun. 2014;443(1):156–160. | ||
Yang GC, Fu BC, Zhang DY, et al. The expression and related clinical significance of SIRT3 in non-small-cell lung cancer. Dis Markers. 2017;2017:8241953. | ||
Zhang B, Qin L, Zhou CJ, Liu YL, Qian HX, He SB. SIRT3 expression in hepatocellular carcinoma and its impact on proliferation and invasion of hepatoma cells. Asian Pac J Trop Med. 2013;6(8):649–652. | ||
Zhao Y, Yang H, Wang X, Zhang R, Wang C, Guo Z. Sirtuin-3 (SIRT3) expression is associated with overall survival in esophageal cancer. Ann Diagn Pathol. 2013;17(6):483–485. | ||
Yu FY, Xu Q, Wu DD, Lau AT, Xu YM. The prognostic and clinicopathological roles of sirtuin-3 in various cancers. PLoS One. 2016;11(8):e0159801. | ||
Haigis MC, Deng CX, Finley LW, Kim HS, Gius D. SIRT3 is a mitochondrial tumor suppressor: a scientific tale that connects aberrant cellular ROS, the Warburg effect, and carcinogenesis. Cancer Res. 2012;72(10):2468–2472. | ||
Wei L, Zhou Y, Qiao C, et al. Oroxylin A inhibits glycolysis-dependent proliferation of human breast cancer via promoting SIRT3-mediated SOD2 transcription and HIF1α destabilization. Cell Death Dis. 2015;6:e1714. | ||
Torrens-Mas M, Pons DG, Sastre-Serra J, Oliver J, Roca P. SIRT3 silencing sensitizes breast cancer cells to cytotoxic treatments through an increment in ROS production. J Cell Biochem. 2017;118(2):397–406. | ||
Liu Y, Liu YL, Cheng W, Yin XM, Jiang B. The expression of SIRT3 in primary hepatocellular carcinoma and the mechanism of its tumor suppressing effects. Eur Rev Med Pharmacol Sci. 2017;21(5):978–998. | ||
Choi J, Koh E, Lee YS, et al. Mitochondrial Sirt3 supports cell proliferation by regulating glutamine-dependent oxidation in renal cell carcinoma. Biochem Biophys Res Commun. 2016;474(3):547–553. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



