Back to Journals » Advances in Medical Education and Practice » Volume 10
Problem-based learning: medical students’ perception toward their educational environment at Al-Imam Mohammad Ibn Saud Islamic University
Authors Aldayel AA , Alali AO, Altuwaim AA, Alhussain HA , Aljasser KA, Bin Abdulrahman KA , Alamri MO, Almutairi TA
Received 28 September 2018
Accepted for publication 23 January 2019
Published 26 February 2019 Volume 2019:10 Pages 95—104
DOI https://doi.org/10.2147/AMEP.S189062
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Abdulaziz Abdulrahman Aldayel, Abdulrahman Omar Alali, Ahmed Abdullah Altuwaim, Hamad Abdulaziz Alhussain, Khalid Ahmed Aljasser, Khalid A Bin Abdulrahman, Majed Obaid Alamri, Talal Ayidh Almutairi
College of Medicine, Al Imam Mohammad Ibn Saud Islamic University, Riyadh, Saudi Arabia
Background: Problem-based learning (PBL) is a student-centered innovating instructional approach in which students define their learning objectives by using triggers from the problem case or scenario.
Objectives: To assess undergraduate medical students’ perception toward PBL sessions and to compare their perceptions among different sex and grade point average (GPA) in the college of medicine, Al-Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Saudi Arabia.
Materials and methods: We conducted a cross-sectional study based on a self-administered anonymous online questionnaire during the first semester of the 2017–2018 academic year in IMSIU. The data were collected from male and female students of the second and third year, as well as male students of the fourth year.
Results: Out of 259 students, 152 (58.7%) completed the questionnaire. The students’ perception toward PBL was more positive than negative. Most of the students reported that PBL sessions increased their knowledge of basic sciences (P=0.03). Furthermore, most students agreed that PBL provided a better integration between basic and clinical sciences which differed significantly between the different GPA groups (P=0.02). Nevertheless, only 28.3% of the students agreed that the teaching staff is well prepared to run the sessions with significant statistical difference among different GPA groups (P=0.02). Moreover, only 26.3% of the students reported that there was proper student training before starting the PBL sessions with no significant difference. Additionally, only 34.2% and 28.9% of the students felt that they learn better and gain more knowledge thorough PBL than lectures respectively, with no significant difference.
Conclusion: This study showed that tutors should be trained to guide the process of PBL effectively to achieve its goals. Moreover, students should be securely introduced to PBL and experience the development of their clinical reasoning through PBL. Further improvements are needed to provide students with an effective favorable learning environment and to take the students recommendations into consideration.
Keywords: medical students, problem-based learning, education, perception, curriculum
Introduction
Problem-based learning (PBL) is a student-centered innovating instructional approach in which students define their own learning objectives by using triggers from the problem case or scenario.1 PBL in medical education was first developed and implemented in the 1960s at McMaster University in Canada by Howard Barrows.2–4 The implementation of the PBL is either as a pure or a hybrid model.5,6 A PBL hybrid model is adopted in many undergraduate medical schools in Saudi Arabia and most of the Gulf Cooperation Council countries.7 The College of Medicine at Al-Imam Mohammad Ibn Saud Islamic University (IMSIU) is one of the medical colleges in Saudi Arabia that introduced PBL into their Bachelor of Medicine, Bachelor of Surgery program as PBL hybrid model. In the pure PBL model, PBL is the chief instructional method in the curriculum and usually without any lectures or tutorial sessions.8 However, in the hybrid PBL model, PBL is introduced in the curriculum with the support of lectures and tutorial sessions.8,9 PBL tutorials consist of small group discussions under the supervision of a tutor.1 There are many reported advantages of this approach. These include increasing students’ knowledge retention, improvement of problem-solving skills, and also students are better able to integrate basic science and clinical knowledge.1,3,10–12 In addition, it contributes to the development and promotion of self-directed and lifelong learning, communication and teamwork skills, presentation skills, and enhances students’ motivation and enthusiasm.1,13–15 However, there are a few studies reporting that PBL is time-consuming and does not help in knowledge acquisition.16,17 Many factors influence effectiveness and quality of the PBL tutorials. There are four critical factors which include the duration of the PBL sessions, the structure of cases, tutors, and assessment in PBL.18 In IMSIU, the PBL system is directed by two sessions weekly. There are two sessions per week for the first year students lasting for 2 hours, and one combined session per week for the second and third year students scheduled to last 3 hours. There is an allocated self-directed learning space to search in various authentic resources between these separated sessions. The seven steps of PBL govern both sessions. In the first session, the students meet and perform brainstorming for problem analysis, where they read through the case and ask for clarification of terms and concepts not readily comprehensible, then assemble their opinions and work together to define and analyze what they think is the problem, without interventions by the tutor. The students also attempt to draw a systematic inventory of the explanations inferred from previous steps in order to formulate and identify their learning objectives by consensus between students and facilitators. This is followed by a personal study done individually to read the literature, collect additional information outside the group, and prepare answers for the formulated learning objectives. In the second session, the students meet to report and discussing their answers, compare results, and exchange arguments. They then problem-solve by synthesizing and testing the newly acquired knowledge while the facilitator evaluates and assesses whether the learning objectives have met the requirements or not. Subsequently, students are provided with feedback summarizing their work through the learning process, including participation in definitions and clarifications, analysis and discussion capabilities, review and formation of the objectives, self-study and reporting. In regard to the tutor competency framework, not all tutors who run the process are subject experts, but a tutor to run PBL sessions in IMSIU has to undergo facilitation in PBL environment courses and training held by the college, in which the applicant is exposed to different strategies in PBL moderation. This tutor training role in PBL involves helping to prioritize issues, encouraging all members to participate, preventing sidetracking, checking understanding, and assessing performance. There are many studies worldwide that suggest a positive impact of PBL on learning. However, there are some studies done in Saudi Arabia and Malaysia on students’ perception of the PBL session, and there was a contradiction between the findings in Saudi Arabia and Malaysia. In Saudi Arabia, they found that students who learned through PBL had better interpersonal skills and knowledge, as well as a better attitude toward patients.19 In Malaysia, they found that PBL was time-consuming and it can be replaced or substituted by other instructional methods.16 Therefore, there is controversy in the students’ impression of the PBL session. Thus, the current study was designed to investigate the students’ perception of PBL sessions and to compare their perceptions among different sex and grade point average (GPA) in the College of Medicine, IMSIU, Riyadh, Saudi Arabia.
Material and methods
Study subjects
A cross-sectional study was carried out to assess the students’ perception of PBL sessions and to compare their perceptions among different sex and GPA in the College of Medicine, IMSIU, Riyadh, Saudi Arabia. The study was conducted during the first semester of the 2017–2018 academic year. The data were collected from male and female medical students of the second and third year, as well as male medical students of the fourth year. Male and female students of the first year were excluded from the study since they did not have GPA at the time of the conduction of this study. All the students of the specified years were included in the study. Uncompleted questionnaires were excluded.
Data collection tool
Data collection was done through self-administered anonymous online questionnaire. The questionnaire was adopted from previous studies, and it was modified to achieve the aim of the study.20–22 The questionnaire was divided into five parts. The first part (Table 1) was dedicated for demographic profile of participants which was answered by multiple choices. The second part (Table 2) consisted of 14 items to measure the students’ perception of the PBL sessions’ benefits. The third part (Table 3) consisted of 12 items to measure the students’ perception toward the PBL conduction and processes. The fourth part (Table 4) consisted of three items to measure the students’ perception of the PBL tutors’ facilitation and their fairness. These items were answered on a three-point Likert scale as agree, neutral/not sure, and disagree. The fifth part (Table 5) consisted of three items, of which two items were answered by checkboxes, and one item was answered by multiple choices. It was designated to evaluate the utilization of self-directed learning resources, duration, and preferred places for preparation of PBL sessions.
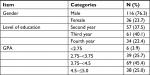  | Table 1 Demographic profile of participants Abbreviation: GPA, grade point average. |
  | Table 2 Students’ perception to problem-based learning (PBL) session benefits Abbreviation: GPA, grade point average. |
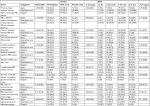  | Table 3 Students’ perception toward the problem-based learning (PBL) conduction and processes |
  | Table 4 Tutors’ facilitation of the problem-based learning (PBL) sessions and their fairness on students’ evaluation |
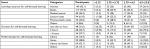  | Table 5 Utilization of self-directed learning resources, duration, and preferred places |
Data analysis
Data were coded and entered into the computer, Microsoft Excel Software (Microsoft Corporation, Redmond, WA, USA) and analyzed using SPSS version 21.0 (IBM Corporation, Armonk, NY, USA) statistical software. The average score for each student was calculated on a five-point Likert scale. The five-point Likert scale responses were combined into three different categorical variables: “agree” (strongly agree plus agree), “neutral/not sure”, and “disagree” (strongly disagree plus disagree). The chi-squared test of independence was used to measure the associations between the different categorical outcome variables (agree, neutral/not sure, and disagree).
Ethical approval
All participants were informed of the objectives of the study, participation was voluntary, and the informed consent was embedded at the beginning of the online questionnaire. Participant anonymity was guaranteed by assigning each questionnaire with a code number for the analysis. Ethical approval for carrying out the present study was obtained by the Research Ethical Committee, College of Medicine, IMSIU, Riyadh, Saudi Arabia.
Results
A total of 259 medical students enrolled in the study. The overall response rate was 58.7%, which represents 152 students. Male students constituted 76.3%, and female students constituted 23.7% of the sample. Details of other characteristics of the sample are shown in Table 1. Table 2 portrays the students’ perception of the PBL sessions’ benefits, which included 14 items. Most of the students reported that PBL sessions increased their knowledge of basic sciences (61.2% of the males, and 58.3% of the females; P=0.03). There were statistically significant differences between the responses of different GPA groups (P=0.05). Furthermore, most students (72.2% of the females, and 59.5% of the males) agreed that PBL provided better integration between basic and clinical sciences which differed significantly between the different GPA groups (P=0.02). Of the students, 44.1% stated that PBL made them more satisfied about their academic progress with the presence of statistically significant differences between the different GPA groups (P=0.01). A majority reported that PBL was helpful in understanding basic sciences knowledge (54.6%); motivated them to learn (59.9%); made them discuss information in a professional way (54.6%); encouraged self-directed lifelong learning (67.8%); helped them to develop problem-solving skills (60.5%); helped them to develop communication skills (75.0%); helped them to identify their strengths and weaknesses throughout the learning process (65.8%); improved their decision-making skills (61.2% of the males, and 50% of the females; P=0.01); and helped them develop their leadership skills (71.5% of the males, and 55.6% of the females; P=0.03). Conversely, only 34.2% of the students felt that they learn better in PBL than lectures. Moreover, only 28.9% of the students agreed that the knowledge is gained more thorough PBL than lectures. However, no significant differences were observed in both variables. Table 3 summarizes the students’ perception toward the PBL conduction and processes, which included 12 items. Most of the students reported that they attended PBL sessions on time (84.2%); the duration of the PBL session was enough (76.3%); the members of PBL contributed equally in PBL session (65.1%); the members of PBL know their roles (58.6%); they felt comfortable with PBL tutorials (43.4%). By way of contrast, only 26.3% of the students disclosed that there was proper students’ training before starting the PBL session with no statistical differences between the groups. Additionally, only 23.7% agreed that they contributed actively in group discussions. However, no significant difference was observed. A majority of the students did not agree with the substitution of lectures by PBL sessions (75% of the females, and 46.6% of the males; P=0.01). Of the students, 44.7% agreed that there is repetition between PBL and lectures with the presence of statistically significant differences between the different GPA groups (P=0.01). Regarding the structure of PBL cases, the students reported that the PBL cases are well written and understandable (45.4%); have a realistic and interesting clinical trigger (55.9%); and have an appropriate level of difficulty/challenge (55.3%). Table 4 shows the students’ perception of the PBL tutors’ facilitation and their fairness, which included three items. Only 28.3% of the students agreed that the teaching staff is well prepared to run the sessions (41.7% of the females, and 24.1% of the males; P=0.11) and there was a statistical difference among students who have different GPA (P=0.02). On top of this, only 26.3% of the students stated that they have been evaluated by the tutors fairly. However, no significant difference was observed. Of the students, 45.4% reported that tutors’ feedbacks were helpful to improve their performance, which differed significantly among students who have different GPA (P=0.001). Table 5 demonstrates the utilization of self-directed learning resources, duration, and preferred places for preparation of PBL sessions. The Internet was the most used resource among the students (92.1%), followed by books (77%), lecture notes (61.8%), medical journals (26.3%), and previous batch notes (23%). A majority (44.7%) reported that they spent 2 hours in the preparation of PBL, and 31.6% of the students spent only <1 hour. Preparation for PBL sessions at both home and library is the leading preferred places (42.1%). The library was used alone by 16.4% of the students.
Discussion
Medical education in Saudi Arabia is in need of continuous improvements in order to keep up with the changing demands of the present time. The reported advantages of the PBL lead most of the medical colleges locally and regionally to shift their curricula to this instructional strategy.23 Assessment of the educational environment of the local institutions that adopted PBL into their curriculum is essential to evaluate the benefits of the new instructional method and to identify areas of weakness for improvement. The present study was undertaken to assess the students’ perception toward PBL sessions and to compare their perceptions among different sex and GPA. The literature showed that students in PBL find learning more motivating and engaging.23 Moreover, students in PBL often report greater satisfaction with their experiences than non-PBL students.23 On the other hand, some of the students in other study reported a negative perception toward PBL and the reason was that some students dominate while others are passive in the PBL discussion.24 In regard to the students’ perception toward the PBL sessions benefits, our study revealed that PBL was a helpful tool for most of the students to increase their knowledge of basic science. This is in agreement with a local study which showed that most students reported that the PBL sessions were helpful in understanding basic sciences concepts.20 Also, it was found in another local study that PBL sessions help in the development of student skills, including problem-solving skills.19 Moreover, it was revealed in a local study that the majority of the students (75%) were satisfied with the PBL method and it improved their problem-solving skills, which is in line with our results.22 Furthermore, Abraham et al25 reported that >75% of students had a strong feeling that their communication skills and self-confidence have improved because of their involvement in PBL.25 In our study, 75% of students reported that PBL improved their communication skills. Also, our study showed that 54.6% of students reported that PBL made them discuss the cases in a professional way which favorably affects their self-confidence. Regarding the knowledge acquisition by PBL and traditional lectures, our study showed that only 34.2% and 28.9% of the students felt that they learn better and gain more knowledge through PBL than lectures respectively. Nevertheless, no significant differences were observed in both variables. Moreover, a local study showed that there is no statistically significant difference observed between both methods regarding the amount of recalled knowledge or provision of a large quantity of information within a shorter time.22 It has been found in a previous study that there are factors that may affect group interactions which include students’ and tutors’ perceptions, tutors’ background, tutors’ group dynamics, students’ training, and the characteristics of the problem that has been used.26 Furthermore, poor participation of some students during PBL sessions could be attributed to many factors including students’ prior knowledge of the content of the scenario, English proficiency, the facilitator not ensuring effective participation of all the students, and poor communication between the group members.27 In the current study, students reported that tutors’ feedbacks were helpful to improve their performance, which is consistent with the results of previous studies where it has been reported that tutors’ feedbacks were essential in the process of PBL and helpful in the development of students’ performance.19,28,29 In the present study, only 26.3% of the students stated that they have been evaluated fairly by the tutors. Similar results were also found in a local study where they reported that only 39% of the students (mostly males) agreed that the tutors fairly evaluated them in the PBL sessions.20 Moreover, in another local study, they found that only 29.2% and 18.4% of students are satisfied with the tutor’s role in PBL session and tutor evaluation, respectively.19 Therefore, according to the result we have obtained, more intensive training for tutors is required to run the PBL process more effectively, focus on students’ difficulties, encourage students to participate despite their prior knowledge or English proficiency, give effective feedbacks, and evaluate the objectives. Similarly, previous local studies have also recommended similar training for tutors.20,30 Previous studies in Vietnam showed that students who were exposed to PBL methods more consistently perceived that they were better prepared for a public health job than those who had not been widely exposed to PBL.31,32 Our results agree with the results of Callis et al,33 who reported that students who enrolled in a hybrid PBL curriculum demonstrated a greater ability to apply basic science principles to a clinical scenario when compared to traditional lecture-based students, which resulted in an increase in the student’s skills in the areas of communication and hypothesis generation. These are necessary skills for interaction of students with other health professionals.33 A recent study reported that students who enrolled in a PBL-based curriculum performed significantly better than students who enrolled in a traditional lecture-based curriculum.34 Similar findings were also reported in other studies.35–37 Our study showed that the Internet was the most used learning resource during SDL to prepare for PBL sessions. This could be attributed to easy access and abundance of information on the Internet. Home and the library are the preferred places (42.1%) for preparation for PBL sessions. However, the library was poorly utilized alone. Consequently, working hours and available resources in the library have to be considered. In addition, an important finding in this study is that only 26.3% of the students reported that there was proper student training before starting the PBL sessions. The lack of proper training may explain the poor contribution of students in group discussions and indicate that training provided to the students in the learning skills course was not enough. Thus, proper student training is essential before starting the PBL sessions, and it should include information on the utilizing of different available resources for seeking information, and making decisions by assessing, interpreting, evaluating, comparing, and weighing evidence.38,39
Study limitations
This is a cross-sectional study which was based on a convenient sampling method and conducted in one medical college which cannot be generalized. Moreover, there was a low response rate from the female section, and there were no fourth-year female students, which is due to the fact that the program of females at IMSIU started recently in 2014–2015 academic year. Furthermore, the male and female students are on separate campuses with different facilitators and thus they may not go through a similar experience in PBL. Therefore, further longitudinal studies must be carried out in medical colleges all over Saudi Arabia to conclude more valid outcomes.
Conclusion
Perception of medical students regarding their educational environment at IMSIU College of medicine which adopted PBL into their curriculum was more positive than negative. However, the study showed that tutors should be trained to guide the process of PBL in order to achieve its goals. Moreover, students should be securely introduced to PBL and experience the development of their clinical reasoning through PBL. Further improvements are needed to provide students with an effective favorable learning environment and to take the students recommendations into consideration.
Author contributions
Alphabetical order was used to determine the order of co-authors. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Wood DF. ABC of learning and teaching in medicine: problem based learning. BMJ. 2003;326(7384):328–330. | ||
Barrows HS, Tamblyn RM. An evaluation of problem-based learning in a small groups utilizing a simulated patient. J Med Educ. 1976;51(1):52–54. | ||
Barrows H. How to Design a Problem-Based Curriculum for the Preclinical Years. Vol. 8. New York: Springer Pub Co.; 1985. | ||
Olson JO. The McMaster philosophy: a student’s perspective on implementation. Med Educ. 1987;21(4):293–296. | ||
Lee Y-M, Mann KV, Frank BW. What drives students’ self-directed learning in a hybrid PBL curriculum. Adv in Health Sci Educ. 2010;15(3):425–437. | ||
Telang A. Problem-based learning in health professions education: an overview. Arch Med Health Sci. 2014;2(2):243. | ||
Khalid BA. The current status of medical education in the Gulf Cooperation Council countries. Ann Saudi Med. 2008;28(2):83–88. | ||
Masek A, Yamin S. Problem based learning model: a collection from literature. Asian Soc Sci. 2010;6(8):148–156. | ||
Azer SA. What makes a great lecture? Use of lectures in a hybrid PBL curriculum. Kaohsiung J Med Sci. 2009;25(3):109–115. | ||
Dolmans D, Schmidt H. The advantages of problem-based curricula. Postgrad Med J. 1996;72(851):535–538. | ||
Patel VL, Groen gJ, Norman GR. Two modes of thought: a comparison of conventional and problem-based curricula. Acad Med. 1991;66:380–389. | ||
Kaufman DM, Mann KV. Comparing students’ attitudes in problem-based and conventional curricula. Acad Med. 1996;71(10):1096–1099. | ||
Barrows Hs TR. Problem-Based Learning: An Approach to Medical Education. Vol 1. New York: Springer Pub Co.; 1980. | ||
Ehj Y, Schmidt HG. Evidence for constructive, self-regulatory, and collaborative processes in problem-based learning. Adv Heal Sci Educ. 2009;14(2):251–273. | ||
Chan EA. Reflecting on the essence of our problem-based learning discussions: the importance of faculty development and our continuous quest for applications of problem-based learning. Kaohsiung J Med Sci. 2009;25(5):276–281. | ||
Emerald NM, Aung PP, Han TZ, Yee KT, Myint MH, Soe TT, Oo SS. Students’ perception of problem-based learning conducted in Phase 1 medical program. SE Asia J Med Educ. 2013;7(2):45–48. | ||
Hartling L, Spooner C, Tjosvold L, Oswald A. Problem-based learning in pre-clinical medical education: 22 years of outcome research. Med Teach. 2010;32(1):28–35. | ||
Chan LC. Factors affecting the quality of problem-based learning in a hybrid medical curriculum. Kaohsiung J Med Sci. 2009;25(5):254–257. | ||
Shamsan B, Syed AT. Evaluation of problem based learning course at College of medicine, Qassim university. Int J Health Sci (Qassim). 2009;3(2):249–258. | ||
Al-Drees AA, Khalil MS, Irshad M, Abdulghani HM. Students’ perception towards the problem based learning tutorial session in a system-based hybrid curriculum. Saudi Med J. 2015;36(3):341–348. | ||
Alkhuwaiter SS, Aljuailan RI, Banabilh SM. Problem-based learning: dental student’s perception of their education environments at Qassim university. J Int Soc Prev Community Dent. 2016;6(6):575. | ||
Ibrahim NK, Banjar S, Al-Ghamdi A, et al. Medical students preference of problem-based learning or traditional lectures in King Abdulaziz University, Jeddah, Saudi Arabia. Ann Saudi Med. 2014;34(2):128–133. | ||
Maxwell NL, Bellisimo Y, Mergendoller J. Problem-based learning: modifying the medical school model for teaching high school economics. Soc Stud. 2001;92(2):73–78. | ||
P Dube DS, S Ghadlinge DM, Su DM, Tamboli DSB, B Kulkarni DM. Students perception towards problem based learning. J Dent Med Sci. 2014;13(5):49–53. | ||
Abraham R, Ramnarayan K, George B, et al. Effects of problem-based learning along with other active learning strategies on short-term learning outcomes of students in an Indian medical school. Int J Health Allied Sci. 2012;1(2):98. | ||
Rankin JA. Problem-based medical education: effect on library use. Bull Med Libr Assoc. 1992;80(1):36–43. | ||
Barman A, Jaafar R, Ismail NM. Problem-based learning as perceived by dental students in universiti sains Malaysia. Malays J Med Sci. 2006;13(1):63–67. | ||
Al-Haqwi AI, Al-Wahbi AM, Abdulghani HM, van der Molen HT. Barriers to feedback in undergraduate medical education. Male students’ perspective in central Saudi Arabia. Saudi Med J. 2012;33(5):557–561. | ||
Alhaqwi AI. Importance and process of feedback in undergraduate medical education in Saudi Arabia. Saudi J Kidney Dis Transpl. 2012;23(5):1051–1055. | ||
Al-Shawwa LAF. Preparing faculty members as PBL tutors in King Abdul Aziz University, Jeddah Saudi Arabia, L. Med J Cairo Univ. 2011;79(2):185–191. | ||
Grisham JW, Alc M, Negin J, Wright EP. Problem-based learning (PBL) and public health: an initial exploration of perceptions of PBL in Vietnam. Asia Pacific J Public Health. 2015;27(2):NP2019–NP2027. | ||
Hoat LN, Yen NB, Wright EP. Participatory identification of learning objectives in eight medical schools in Vietnam. Med Teach. 2007;29(7):683–690. | ||
Callis AN, McCann AL, Schneiderman ED, Babler WJ, Lacy ES, Hale DS. Application of basic science to clinical problems: traditional vs hybrid problem-based learning. J Dent Educ. 2010;74(10):1113–1124. | ||
Zahid MA, Varghese R, Mohammed AM, Ayed AK. Comparison of the problem based learning-driven with the traditional didactic-lecture-based curricula. Int J Med Educ. 2016;7:181–187. | ||
Al-Damegh SA, Baig LA. Comparison of an integrated problem-based learning curriculum with the traditional discipline-based curriculum in KSA. J Coll Physicians Surg Pak. 2005;15(10):605–608. | ||
Faisal R, Khalil-ur-Rehman, Bahadur S, Shinwari L. Problem-based learning in comparison with lecture-based learning among medical students. J Pak Med Assoc. 2016;66(6):650–653. | ||
Guven Y, Bal F, Issever H, Can Trosala S. A proposal for a problem-oriented pharmacobiochemistry course in dental education. Eur J Dent Educ. 2014;18(1):2–6. | ||
Dalrymple KR, Wuenschell C, Rosenblum A, et al. PBL core skills faculty development workshop 1: an experiential exercise with the PBL process. J Dent Educ. 2007;71(2):249–259. | ||
El Aziz El Naggar MAA, Maklady FAH, Hamam AM, Omar AS. Effectiveness of implementing a tutor training workshop for problem based learning class tutors at the Faculty of Medicine, Suez Canal University. Intel Prop Rights. 2013;1(1):2. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
