Back to Journals » Risk Management and Healthcare Policy » Volume 15
Price, Availability and Affordability of Anti-Cancer Medicines in Addis Ababa, Ethiopia
Authors Alemu BA , Hailemariam FH
Received 8 November 2022
Accepted for publication 16 December 2022
Published 29 December 2022 Volume 2022:15 Pages 2421—2433
DOI https://doi.org/10.2147/RMHP.S395456
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jongwha Chang
Bemnet Atlaw Alemu, Fikreselam Habte Hailemariam
Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Fikreselam Habte Hailemariam, Tel +251 913 39 40 44, Email [email protected]
Introduction: Cytotoxic drugs are essential treatments available for patients with cancer. There are concerns that unavailability and high prices of cancer medicines may limit patient access. Since information on availability, prices and affordability for cancer medicine is lacking for several countries, particularly for lower income countries like Ethiopia, it will be difficult to know the real situation of those medications’ access.
Purpose: The purpose of this study was to assess availability, affordability and price of anti-cancer medications, in Addis Ababa, Ethiopia.
Methods: The study was cross-sectional using a modified form of the WHO/HAI methodology of measuring medicine price, availability and affordability in public, private, Kenema municipal and Red Cross Pharmacies found in Addis Ababa, Ethiopia. Data on the availability and price of 47 cytotoxic medications for both lowest priced generics and originator brands were collected in 3 public, 6 private and 2 NGO pharmacies which are expected to dispense cytotoxic medications in Addis Ababa. The data were entered and analyzed using WHO/HAI data entry and analysis form. Results were presented in tables and figures.
Results: The majority of the anti-cancer medications assessed were not available and the few available medicines were unaffordable. The lowest priced generic were relatively more available (34.8%) than the originator brand medications (2.8%) in the public sector. Generally, the availability of anti-cancer medicine differs when comparing the public, private and other sectors. The availability of cytotoxic medications was 18.8%, 5.3% and 8.8% in the public, private and other sectors. The prices of cytotoxic medications available in the private sector were higher than the public and other sectors. All of the medications except for anastrazole were unaffordable.
Conclusion: Medicines for cancer treatment are unavailable and the few available medicines are unaffordable in Addis Ababa, Ethiopia. Different interventions should be done to improve access to cytotoxic medications.
Keywords: access, cytotoxic, essential medicine, cancer in Ethiopia
Introduction
Cancer is the world’s second biggest cause of mortality.1 Cancer is responsible for around 1 in every 6 deaths worldwide, bearing over 80% of the burden in terms of disability-adjusted life-years (DALYs). With the aging of the population, the number of new cancer cases globally is expected to rise to 21.4 million by 2030. Unless more is done to change the path of the disease, this figure is likely to climb to over 30 million additional cases by 2040.2
In Low and Middle Income Countries (LMIC) the incidence of cancer is around 3 million with mortality of nearly 2 million and prevalence of more than 6 million.3 Currently, even though the incidence in LMIC is three times lower than developed countries, more than half of the mortality from cancer occurs in LMIC and it is expected to rise significantly in the next 50 years.4
In Ethiopia, the yearly incidence of cancer is estimated to be over 60,960 cases, with an annual death of over 44,000. Cancer accounts for around 5.8% of total national mortality.5 In the last decade the incidence, death and DALY from cancer increased by 32%, 29% and 19% respectively.6 The common types of cancer in females are breast, cervical and ovarian. Whereas, bone and soft tissue, colorectal and esophageal malignancies are common in males.5,7 Considerable numbers of the cancers are discovered at advanced stages, usually several months after symptoms first appear which require chemotherapy as a main treatment.5,8
According to international treaties access to health care is a fundamental human right.9 The basic right to health cannot be accomplished without equitable access to critical pharmaceuticals for priority diseases. Medicine cost and availability can be a barrier to patient treatment.9 Millions of people worldwide go without the treatment they require because of the increased cost and unavailability of pharmaceuticals to those in need.9
Despite the increase in prevalence, cancer treatment is usually inaccessible and expensive especially in developing countries. In the southern part of Ethiopia, among 1298 patients diagnosed with cancer only 1.4% were able to access medication for their treatment; even though most of the patients had advanced stage which require chemotherapy as primary therapy.10 Low and Middle Income Countries (LMICs) are assigned a budget less than 5% of global cancer-fighting resources.11 In LMICs up to 90% patients must bear the cost of treatment in the absence of government reimbursements, insurance or exclusive access schemes.12,13 Cancer patients and governments throughout the world face a difficulty due to the high cost of cancer therapy.12,14 Additionally, indirect costs associated with the disease like loss of production because of the disease, transportation, symptomatic drug use, other inputs and so on results in financial strain.12 As a result, patients are forced into hardship and poverty, leading to treatment abandonment and early death.12,14 Essential cancer drugs that are unavailable and/or costly may result in inferior and/or interrupted treatment regimens, worse health outcomes and fewer odds of survival.15 As a result, fair access to essential medications at reasonable prices is a critical component of comprehensive cancer treatment.15
One of the most significant barriers to access is high drug pricing. In Ethiopia three fourths of patients with cancer experience catastrophic health expenditure majorly because of unaffordability of treatment.12 Also most patients were required to cover their expense out of pocket.12
To guarantee that medications are affordable, efficient and effective national policies, drug pricing and procurement methods are essential. The difficulty in obtaining trustworthy information on pharmaceutical costs and availability impedes governments’ capacity to develop appropriate medicine pricing policies or assess their impact. To create effective and transparent pricing strategies in LMICs there should be adequate data on the cost and affordability of the medications. Furthermore, people in charge of acquiring drugs are unable to negotiate lower prices since they lack a solid foundation on which to base their negotiations.16 Even in nations where consumers and patients have greater purchasing power, governments, insurance funds and hospitals frequently find it difficult to choose drugs due to a lack of information.11 Systems for generating reliable and quality data to guide the selection of the most appropriate pricing model for cancer medicines should be put in place to ensure fair and transparent pricing of cancer medicines.16,17
This study assessed the price of anti-cancer medicines and how many of the drugs are available in different sectors in Addis Ababa, Ethiopia. And thus, it could enable to assess if the medicines are affordable or not.
Methods
Study Settings
Ethiopia is a landlocked country found in East sub-Saharan Africa. Addis Ababa is capital city of Ethiopia, where the Africa Union and different international organizations are located. It is the largest city in the country with a population of around 5.2 million. In Addis Ababa there are 13 public hospitals, around 100 health centers and several private ones. Until recent years cancer treatment was provided in Addis Ababa only, currently it is provided in a few regional teaching hospitals in Ethiopia.16 Cancer therapy is provided in three of those public teaching and tertiary hospitals in Addis Ababa, these are Tikur Anbessa Specialized Hospital, St. Paul Specialized Hospital, and Yekatit 12 Hospital. Additionally, palliative care is provided in Woreda 08 health center. Even though cancer therapy is initiated at different regions of Ethiopia other than Addis Ababa, the majority of the patients are referred to Addis Ababa for better management and monitoring.10 This study was conducted at those three public hospitals, and at private, and other sector pharmacies found around those hospitals. Procurement price was assessed from Ethiopian Central Pharmaceutical Supply Agency.
Study Design and Period
The study was a cross-sectional study held from May 16 to 30, 2022 GC.
Study Population and Sample Size
Outpatient department (OPD) pharmacies of three public hospitals which provide cancer therapy (Tikur Anbessa Specialized Hospital, Yekatit 12 Hospital and St. Paulos Specialized Hospital); six private pharmacies found around those public hospitals, three Addis Ababa city administration/ municipal pharmacies called Kenema Pharmacies and one Red Cross Pharmacy found near to those public hospitals were surveyed. The medication procurement price was collected from the Ethiopian Pharmaceutical Supply Agency located in Addis Ababa, the agency majorly supply lowest priced generic (LPG) medications for public health facilities. Therefore, data were collected from 13 medicine outlets and one central procurement agency. The study includes 47 cytotoxic medications which are listed as essential medicine on the Ethiopian essential medicine list (EML),18 and a few medications used in Ethiopia but not included in the EML.
Study Variables
The study variables were:
- Availability.
- Affordability.
- Price.
Data Collection and Analysis
A structured questionnaire was developed by modifying WHO and HAI standard methodology to assess price, availability and affordability of medicines for treatment of cancer. The study included all cytotoxic/anti-cancer medications found in the EML of Ethiopia, and also a few medicines which are registered and used in the country, but not found in the EML.
For each medicine in the survey, data on availability and price were collected for two products: the originator brand (OB), and the lowest-priced generic (LPG) equivalent found at each medicine outlet.
Data were collected by one pharmacist who was well trained about the data collection. Supervision was done by the investigator, examining data collection forms at the conclusion of each day of fieldwork to guarantee data quality and follow up on any incomplete, erroneous, or illegible data.
Data entry personnel (pharmacist) entered the data into the automated WHO/HAI Medicine Price and Availability Workbook – Part I, which is a Microsoft Excel (V 15.0)-customized program to enter and analyze the data collected.
To ensure the quality of the data collected, pre-test was done at one private pharmacy to ensure that the questionnaire is clear and understandable. Random check was done by the supervisor to ensure the quality of the data collected.
To avoid mistakes during data entry, data were entered twice by the pharmacists and cross-checked (double entry). The data-checker function of the workbook was used to indicate dubious data that had to be verified.
The WHO/HAI Medicine Price and Availability Workbook – Part I, which is Microsoft Excel V 15.0, was used for data analysis. It is a programmed workbook to consolidate and summarize results. Individual medicine availability is provided as a percentage (%) and prices discovered during the survey were given as ratios relative to a standard set of worldwide reference prices, known as the median price ratio or MPR, to simplify international comparisons. The ratio expresses how much higher or lower the median local medication price is than the international reference price;19 for example, an MPR of 2 indicates that the local medicine price is twice as high as the international reference price.
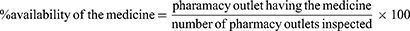
Availability
The availability of survey medicines was assessed by inspecting the lowest priced generic and originator brand medicine in the pharmacy outlet. Medicine availability was calculated as the percentage of pharmacy outlets where a given medicine was available on the day of survey for public, private and Kenema Pharmacy and also for all sectors. Percent availability was calculated as:
Price
In Ethiopia most patients acquire medicine by purchasing out of pocket. There are few patients who have a letter stating they cannot afford the medicines, for such patients medicines are free.
Price of the medicine was obtained from the price list in the pharmacy outlet. Pharmacies in private mostly write the local price on the medicine package. The local price was changed to US dollars using the exchange rate on the first date of the data collection. On first day of data collection 1US$=51.52 ETB. THe median price ratio (MPR) was calculated as:
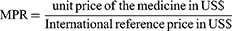
Affordability
Affordability was calculated as the number of working days necessary for the lowest-paid unskilled government worker to purchase the specific anti-cancer medication for one course of therapy.11 It was calculated as:
Ethical Considerations
An official letter stating the purpose of the study was written by Addis Ababa University, School of Pharmacy Ethical Review board with reference number (ERB/SOP/454/14/2022). The letter was presented to the responsible authorities of the pharmacies. In addition, verbal and written consent was asked from each manager of the pharmacy outlets after explaining the purpose of the study. The managers of the pharmacist were told that the data obtained from the outlets was used only for research purpose.
Operational Definition
Availability: in this study refers to anti-cancer medication was present for the patients in the pharmacy outlet on the day of data collection.
Price of the medicine: the payment required to purchase the medicine without including other service charges if present on the day of data collection.
Affordability: if less than one day's wage was required to purchase the medication, then it is affordable. If more than one day is required to purchase the medicine, it is unaffordable.11 Other sector in this study was Kenema and Red Cross Pharmacies.
Results
Availability of Anti-Cancer Medicines
The overall availability of anti-cancer medication at all sectors was found to be extremely low. The availability of LPGs and OBs was 34.8% and 2.8% at public sector, 9.9% and 0.7% at private sector and 16% and 2.1% in other sector (Kenema Pharmacies) respectively. Anti-cancer medications were totally unavailable in Red Cross Pharmacies.
Relatively, LPGs medicines were available better than OB; 20.21% and 1.89% respectively (Table 1). The most available medication in both OBs and LPGs form in the public sector was tamoxifen, with 100% availability. In the private sector the highest availability of OBs and LPGs were 16.7% and 83.3% respectively while the average availability were 0.71% and 9.93% respectively. In other sector the highest availability of OBs and LPGs were 100% while the average availability were 2.13% for OB and 15.96% for LPGs.
 |
Table 1 Overall Availability of Lowest Priced Generic Anti-Cancer Medicines on the Day of Survey at Public, Private and Other Sectors in Addis Ababa, Ethiopia 2022 |
Methotrexate 50 mg injection and tamoxifen 20 mg were the only OB medicines available in the public hospital pharmacy with 33.3% and 100% availability respectively.
Across sectors, the public sector had the highest relative mean availability of cytotoxic medication in OBs and LPGs (2.8% and 34.8%). Regarding the availability of individual drugs, tamoxifen was the most widely available, with a mean availability of 63.9% in all sectors. The overall availability of arsenic trioxide, asparaginase, carboplatin, cisplatin, cytarabine, dacarbazine, dactinomycin, docetaxel, gemcitabine, irinotecan, mercaptopurine and thalidomide was very low in all the sectors. Vinblastine and vincristine, which are recommended for prostate cancer and leukemia treatment, was available in the public sector but not in private and other sectors (Table 1).
Bendamustine, bleomycin, chlorambucil, epirubicin, fludarabine and paclitaxel which are recommended for ovarian, cervical, breast cancer, leukemia, and Hodgkin’s and non-Hodgkin’s lymphoma (common cancer in Ethiopia) were not available in all medicine outlets. Also the following anti-cancer medicines were totally unavailable in any of the outlets, Whether OBs or LPGs form, during the study period, even though included in the EML of Ethiopia; bendamustine 100 mg/mL injection, bleomycin 15 IU injection, calcium folinate 50 mg mg/mL injection, calcium folinate 3 mg/mL injection, chlorambucil 2 mg tab, daunorubicin 50 mg injection, epirubicin 100 mg injection, fludarabine 50 mg injection, exemestane 25 mg tab, ifosfamide 1000 mg injection, ifosfamide + mesna 1000 mg + 400 mg/mL injection, melphalan 2 mg tab, methotrexate 1000 mg injection, oxaliplatin 50 mg/10 mL injection, oxaliplatin 100 mg/20 mL injection, paclitaxel 100 mg injection, paclitaxel 300 mg injection, procarbazine 50 mg cap, vinorelbine, 10 mg/mL injection.
Generally, the availability of cytotoxic medicines differs when comparing the public, private and other sectors. The availability of cytotoxic medications was 18.8%, 5.3% and 8.8% in the public, private and other sectors.
Anti-Cancer Medication Prices
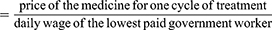
Public Sector Procurement Prices
Most of the LPG medicines being purchased were at prices approximately equal to international prices. The maximum MPR found in this study is 1.15, which is comparable to the international procurement price (Table 2).
 |
Table 2 MPR for All Cytotoxic Medication in Public Sector Procurement Agency, Addis Ababa, Ethiopia 2022 |
Public Sector Patient Prices
The medications with the maximum and minimum average price from the available medications were cyclophosphamide and anastrazole with a price of ETB 753.9 and 2.455 respectively.
The average price of the available drugs is listed in Table 3.
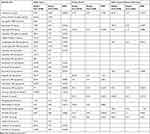 |
Table 3 Unit Price and MPR of Anti-Cancer Medicines Available in Addis Ababa, Ethiopia, 2022 |
The median MPR of LPG for public sector was 0.55. The minimum and maximum MPR was 0.05 and 2.23 respectively (Table 3).
Private Sector Patient Prices
The lowest-priced generic medicines found had median MPR of 2.08, with minimum and maximum MPR of 1.37 and 5.33 respectively (Table 3).
The unit price of the medications available at private sector had higher price when compared to the public and other sectors (Table 3).
Other Sector Patient Prices
The median price of LPG cytotoxic medicines available at other sectors was lower than private sectors but higher than the public sector. The median MPR was 0.85 with minimum and maximum MPR of 0.49 and 6.61 respectively (Table 3).
When the prices of medicines available in more than one sector are compared, the price in the public sector is always less than the private and other sector price, except for doxorubicin 50 mg injection (Table 3).
Affordability of the Medications
The affordability of cancer treatment was estimated as the number of days necessary at the existing wage that the lowest-paid, unskilled government worker needed to purchase anti-cancer medicines prescribed at a standard dose. In Ethiopia, the daily wage of the lowest paid, unskilled government worker used in the analysis was ETB 36.7, which is equivalent to ETB 1101 per month.20
All the available cytotoxic medications surveyed were unaffordable except for anastrazole in the public sector. The unaffordability was much higher in the private sector (Table 4).
 |
Table 4 Number of Days’ Wages of the Lowest-Paid Government Worker Needed to Purchase Standard Treatments of Common Cancer in Addis Ababa, Ethiopia, 2022 |
For an adult woman patient with breast cancer prescribed cyclophosphamide 600 mg/m2 combined with doxorubicin 60 mg/m2 for 4 cycles and subsequent docetaxel for 12 cycles21 required 249 days of wages to purchase the medicine in the public sector.
Discussion
This study showed that anti-cancer medicine availability was 18.8% in the public sector, 5.3% in the private sector and 8.8% in the other sector. Most of the essential medicines for the treatment of cancer are not available in Addis Ababa; even though medications in the essential list are expected to be available all the time. Cytotoxic medications are core in the treatment of cancer, unavailability means the patient is counting the number of days left before dying. In Ethiopia cancer treatment is in the infant stage. In Addis Ababa there are only three public hospitals which provide cancer treatment, and were included in this study. These three hospitals are expected to treat patients referred from every corner of the country, since most of the regional hospitals started the service recently and are suffering from a shortage of the necessary supply for the treatment service.16 Additionally the Ethiopian population number is rising at an alarming rate and also the life expectancy is also rising, in the near future it is expected that the number of cancer cases will rise as the aging population are increasing. Overall, the availability of cytotoxic pharmaceuticals falls short of the WHO’s target of 80% availability of the necessary medicines to treat non-communicable disease (NCDs).22 The overall and each sector availability was also lower than New Delhi, India23 and Ghana24 availability. The low availability is likely to be the effect of multiple factors, such as interrupted and inefficient supply chain management system, inadequate investment in the area, less attention given to the area and lack of research which indicates the real figure of the situation.
When comparing the general availability in public, private and other sectors, the medicines were more available in the public sector in this study. This finding was similar with the Indian, New Delhi finding23 but different from Ghana,24 and Mexico, which was 61.2% in public and 67.5% in private.25 And the overall availability was also lower than Ghana and Mexico countries.23–25 The availability of cytotoxic drugs in this study was also lower than other LMICs such as Tanzania and Pakistan.26,27 Pakistan and Tanzania reported 50% availability of cytotoxic medicine in the public sector. In Pakistan, the private sector had a better availability of drugs than the public sector.26 Additionally, private sectors in Pakistan are more focused on having OBs, whilst private sectors in Addis Ababa have more access to generic cytotoxic drugs. Different countries have different preference for private and public sector involvement in availing the medication. The study also showed that cytotoxic medicines were more available in public than other sector/Kenema, but still other sector had better availability than the private sector. The difference in availability between public and private sectors could be because different countries have different policies and preference. In Addis Ababa, the less availability in the private sector may be because private sectors have limited knowledge about the burden of the disease and the needs of the medication, also private sectors may not have adequate information source about availability of those medications. Low availability in the private sector may also be due to low demand for anti-cancer drugs in private facilities because of the limited health facilities providing cancer management. It is common to see that private sectors in Ethiopia do not prefer to avail medication which they think the service is not well established because of economic scale value when used by few and the fear of expiry. This study indicates there is serious unavailability of medicines, and the public sector are primarily involved in availing the medicines The healthcare policy of Ethiopia should encourage private, NGO and other sector involvement in better availing anti-cancer medications, so the burden of this catastrophic disease could be reduced.
When comparing the availability of OBs and LPGs, LPGs were more available than the OBs in all of the sectors assessed. This study finding was contrary to the research done in Pakistan that showed better availability of OBs than LPGs in both public and private facilities.26 The preference for LPG may help to reduce the cost of the medications28 as long as quality of the medication is kept. The more availability of LPG than OB has paramount importance for the patient purchasing the medication out of pocket like in Ethiopia.
This study also analyzed the price of the selected cytotoxic medications and also compared among sectors with OB and LPG. The price of cytotoxic medications in the public procurement sector was comparable with the international reference prices. This shows the central procurement has a good procurement process. Even though studies indicate that African countries had a higher procurement price than Latin Americans, this study found the price to be comparable to or less than the international reference price.29 In this study it was difficult to compare price between OB and LPG because the availability of OB was very low, but still the price variation between OB and LPG was very high for the two OB available medicines, similarly with other country studies.30,31 However, the cost of the medications for the patient was very high. This could be because the added costs to the final medication price reaching the patient could be very high relative to central procurement cost.
The results indicated that it was not only prices of the medications were high, but also there was a large difference between the price found in public and private sectors. The price at public and other sectors were more or less similar but the price at the private sector was very high. This result is similar with a study done in South Africa.27 But different from India,31 having lesser MPR than this study, even less than one in Ghana. The difference could be because retail pharmacies have different cost of acquiring the drug and also different profit margin in different countries. There was also a difference of the price between OBs and LPGs. The price of the OBs was very higher than the LPGs. High costs could be attributed to a lack of generic competition, high manufacturer profit margins and an inefficient supply system.
Among the entire 47 anti-cancer medications assessed, except one, all others were unaffordable. Furthermore, the majority of cancer treatment regimens require more than one drug at a time for one course of treatment, making the treatment even more expensive. This result was similar with the studies done in India,23 Ghana24 and Mexico.25 Other studies in Tanzania and Pakistan also found that purchasing anti-cancer drugs takes more than one working day for a single cycle.26,27 Systematic reviews also indicated that essential cytotoxic medicines are often unaffordable in low-income countries.27 In addition to anti-cancer medications, medications for prevention and treatment of side effects increase the overall medication cost for the disease. This indicates the need to develop policy to reduce the cost and also to reimburse the patient on the cost of medication.
All anti-cancer medicines for the treatment of most common cancers in Ethiopia were unaffordable. A patient with early stage breast cancer and estrogen positive required 286 days of wages to purchase the medicine. Similar with other studies when OB medications were used the unaffordability was even more increased.30,32 In reality many of the cancer treatments may require more cycle and combination of medicines treatment, which may result in increased price and unaffordability. This shows in Ethiopia treatment of cancer is allowed only for the few rich people, It is leisure for the other many population. The healthcare policy of Ethiopia should urgently find a solution to cover for such costs.
Therapy availability, price and affordability are determinant factors for treatment of cancer. In Ethiopia, access to cancer drugs is a serious concern. Also lack of pricing and affordability data to design efficient and transparent pricing policies, a lack of insurance coverage and the ensuing financially prohibitive cost to patients had paramount negative effect on patient treatment outcome.
High inflation, low per capita income and associated rising living costs are only a few of the obstacles that prevent individuals from obtaining anti-cancer drugs. Long-term sustainability requires differential pricing, insurance schemes, drug discounts, patient-access schemes, tax breaks, collaborative public–private ventures, patent amendments, national health plans and replication of key governance models. The link between price and healthcare results should be strengthened through arrangements that promote innovation while preserving the long-term viability of a low-cost healthcare system.
Limitations of the study were: the study was restricted to Addis Ababa only, which may not indicate the whole country situation which could be worse than this finding; the availability result works only for the day of the assessment, it does not show the situation for extended period; also it was difficult to find updated international reference price, the study compared the price with a previously published MSH price which might have some drawbacks but still able to show some insight about the situation.
Conclusion
Cancer medications were extremely unavailable and the few available medications were unaffordable. Different sectors have different availability and cost of medication. This could impose serious harm to patients with such debilitating disease.
Abbreviations
DALYs, disability-adjusted life-years; Cap, capsule; EML, essential medicine list; ETB, Ethiopian birr; HAI, Health Action International; LMICs, low- and middle-income countries; LPGs, lowest-priced generics; MPR, median price rationale; MSH, Management Science for Health; NGOs, non-governmental organizations; OB, originator brands; Tab, tablet; USD, United States dollars; WHO, World Health Organization; WHO/HAI, World Health Organization/Health Action International.
Acknowledgments
We would like to thank Addis Ababa University, College of Health Science, School of Pharmacy for giving us this opportunity to undertake the study by covering transport cost to the facilities.
Funding
The author received no funding for this study.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Mattke S, Haims MC, Ayivi-Guedehoussou N, et al. Improving access to medicines for non-communicable diseases in the developing world. Rand Health Quart. 2011;1(3):115.
2. World Health Organization. International agency for research on cancer; 2022. Available from: https://gco.iarc.fr/.
3. International Agency for Research on Cancer, World Health Organization. Cancer Statistics for Low and Middle Income Countries. International Agency for Research on Cancer, World Health Organization; 2020.
4. International Agency for Research on Cancer, World Health Organization. Global cancer statistics, cancer tomorrow. Available from: https://gco.iarc.fr/tomorrow/en.
5. Federal Ministry of Health, Ethiopia. National cancer control plan 2016–2020 of Ethiopia. Prev Control Dir. 2015;2015(10):83.
6. Awedew AF, Asefa Z, Belay WB. National burden and trend of cancer in Ethiopia, 2010–2019: a systemic analysis for Global burden of disease study. Sci Rep. 2022;12(1):1. doi:10.1038/s41598-022-17128-9
7. International Agency for Research on Cancer, World Health Organization. Ethiopian Cancer Statistics. International Agency for Research on Cancer, World Health Organization; 2020.
8. Solomon S, Mulugeta W. Diagnosis and risk factors of advanced cancers in Ethiopia. J Cancer Prev. 2019;24(3):163. doi:10.15430/JCP.2019.24.3.163
9. Howard DH, Bach PB, Berndt ER, Conti RM. Pricing in the market for anticancer drugs. J Econ Perspect. 2015;29(1):139–162. doi:10.1257/jep.29.1.139
10. Wondimagegnehu A, Negash Bereded F, Assefa M, et al. Burden of cancer and utilization of local surgical treatment services in rural hospitals of Ethiopia: a retrospective assessment from 2014 to 2019. Oncologist. 2022;27(11):e889–98. doi:10.1093/oncolo/oyac127
11. World Health Organization. Measuring Medicine Prices, Availability, Affordability and Price Components. World Health Organization; 2008.
12. Kasahun GG, Gebretekle GB, Hailemichael Y, Woldemariam AA, Fenta TG. Catastrophic healthcare expenditure and coping strategies among patients attending cancer treatment services in Addis Ababa, Ethiopia. BMC Public Health. 2020;20(1):1. doi:10.1186/s12889-020-09137-y
13. World Health Organization. Assessing National Capacity for the Prevention and Control of Noncommunicable Diseases: Report of the 2019 Global Survey. Geneva: World Health Organization; 2020.
14. Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi:10.1016/S0140-6736(19)30427-1
15. Ruff P, Al-Sukhun S, Blanchard C, Shulman LN. Access to cancer therapeutics in low-and middle-income countries. Am Soc Clin Oncol Educ Book. 2016;36:58–65. doi:10.1200/EDBK_155975
16. Tegegn HG, Reda HL, Tilahun Y. Access to cancer medicine issues: implication for policy and practice in Ethiopia. J Global Oncol. 2018;4:21s–21s. doi:10.1200/jgo.18.14000
17. Stewart BW, Wild CP. International agency for research on cancer. World cancer report. 2014.
18. Minister of Health/Ethiopian Food and Drug Authority. Ethiopian Essential Medicines List.
19. Management Sciences for Health. International Medical Products Price Guide. Management Sciences for Health; 2015.
20. Ministers of Council. Federal civil servants position rating, grading and salary scale council of ministers regulation number 455/2019. Federal negarit Gazette. 2019:11862 and 11863.
21. Anderson BO. NCCN harmonized guidelines for sub-Saharan Africa: a collaborative methodology for translating resource-adapted guidelines into actionable in-country Cancer control plans. JCO Global Oncol. 2020;6:111.
22. Assembly SWH, World TS. General assembly on September, 21, 1996. Strahlentherapie Und Onkol. 1997;173(2):122.
23. Faruqui N, Martiniuk A, Sharma A, et al. Evaluating access to essential medicines for treating childhood cancers: a medicines availability, price and affordability study in New Delhi, India. BMJ Global Health. 2019;4(2):e001379. doi:10.1136/bmjgh-2018-001379
24. Mensah KB, Mensah AB, Bangalee V, Padayachee N, Oosthuizen F. Evaluating essential medicines for treating childhood cancers: availability, price and affordability study in Ghana. BMC Cancer. 2021;21(1):1–9. doi:10.1186/s12885-021-08435-x
25. Moye-Holz D, Ewen M, Dreser A, et al. Availability, prices, and affordability of selected essential cancer medicines in a middle-income country–the case of Mexico. BMC Health Serv Res. 2020;20(1):1. doi:10.1186/s12913-020-05167-9
26. Sarwar MR, Iftikhar S, Saqib A. Availability of anticancer medicines in public and private sectors, and their affordability by low, middle and high-income class patients in Pakistan. BMC Cancer. 2018;18(1):1. doi:10.1186/s12885-017-3980-3
27. Ocran Mattila P, Ahmad R, Hasan SS, Babar ZU. Availability, affordability, access, and pricing of anti-cancer medicines in low-and middle-income countries: a systematic review of literature. Front Public Health. 2021;2021:462.
28. Shrestha S, Poudel RS, Kc B, et al. Price variation among different brands of anticancer medicines available in hospital pharmacies of Nepal. J Pharm Policy Pract. 2020;13(1). doi:10.1186/s40545-020-0203-0
29. Cuomo RE, Seidman RL, Mackey TK. Country and regional variations in purchase prices for essential cancer medications. BMC Cancer. 2017;17(1):1. doi:10.1186/s12885-017-3553-5
30. Shrestha S, Poudel RS, Kc B, et al. Price variation among different brands of anticancer medicines available in hospital pharmacies of Nepal. J Pharma Policy Pract. 2020;13(1):1.
31. Kolasani BP, Malathi DC, Ponnaluri RR. Variation of cost among anti-cancer drugs available in Indian market. J Clin Diagn Res. 2016;10(11):FC17. doi:10.7860/JCDR/2016/22384.8918
32. Kizub DA, Naik S, Abogan AA, et al. Access to and affordability of world health organization essential medicines for cancer in Sub-Saharan Africa: examples from Kenya, Rwanda, and Uganda. Oncologist. 2022;27(11):958–970. doi:10.1093/oncolo/oyac143
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.