Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Prevalence of unrecognized depression and associated factors among patients attending medical outpatient department in Adare Hospital, Hawassa, Ethiopia
Authors Tilahune AB , Bekele G, Mekonnen N, Tamiru E
Received 28 July 2016
Accepted for publication 15 September 2016
Published 25 October 2016 Volume 2016:12 Pages 2723—2729
DOI https://doi.org/10.2147/NDT.S118384
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Asres Bedaso Tilahune,1 Gezahegn Bekele,1 Nibretie Mekonnen,2 Eyerusalem Tamiru2
1School of Nursing and Midwifery, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia; 2Department of Medical Case Team, Hawassa University Comprehensive Specialized Hospital, Hawassa, Ethiopia
Abstract: Depression is an illness that involves the body, mood, and thoughts and that affects the way a person eats, sleeps, feels about him or herself and thinks about things. Depression is one of the most common mental disorders affecting 121 million people in the world, and it frequently goes unrecognized among patients. It is estimated that 5%–10% of the population at any given time is suffering from identifiable depression needing psychiatric or psychosocial intervention. An institution-based cross-sectional study design was implemented to determine the magnitude and associated factors of unrecognized depression among patients attending the adult medical outpatient department in Adare Hospital, Hawassa, Southern Nations, Nationalities, and Peoples’ Region, Ethiopia, among 326 patients selected using systematic random sampling technique. Data were collected using the interviewer-administered technique. A structured questionnaire was used to collect data on sociodemographic characteristics and other independent variables. Depression was assessed using the Patient Health Questionnaire 9. Data were entered and analyzed using SPSS 20. The level of significance was determined at P<0.05. About 326 patients were interviewed, of whom 186 (57.1%) were males. The mean age of participant was 34 with standard deviation of ±13.1 years. Current substance users accounted for 106 (32.5%) of the total participants. Of 326 respondents, 80 (24.5%) had significant depressive symptoms, while the detection rate of depression by the clinician was 0%. Depression was associated with female sex (adjusted odds ratio [AOR] =1.63 [1.14–2.34]), age >60 years (AOR =4.14 [1.87–9.14]), being divorced (AOR =3.13 [1.70–5.76]), and having an average monthly income <750 ETB (AOR =1.92 [1.119–3.195]). The findings of this study revealed that the prevalence of depression among patients attending general medical outpatient department was highly underrecognized and unmanaged. On the basis of these results, we recommended that health-care providers perform a thorough assessment to address common mental disorders, especially depression, and suggest that training to recognize and manage depression appropriately be given.
Keywords: depression, outpatient, Adare Hospital, unrecognized, institution-based cross-sectional study
Introduction
Depression is a common mental disorder that is characterized by loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration.1 Depression often occurs as a result of adverse life events, such as the loss of a significant person–object relationship or loss of health. However, it can also occur due to no apparent cause. These problems can become chronic or recurrent and lead to substantial impairment in an individual’s ability to take care of their everyday responsibility.2
Depression is associated with a combination of genetic, psychological, environmental, and biological factors.3 The risk factors associated with depression include stress, impulsive behavior, alcohol or substance abuse, and family history of depression or suicide. Other factors such as poverty, severe or chronic medical conditions, insomnia, female sex, intimate partner violence, sexual abuse, and tobacco use are also associated with depression.4
The review of research evidence available indicates that the primary health-care clinician’s ability to detect depressive disorders is important to prevent suicide and reduce health-care cost because patients with depression visit health facilities frequently.5 However, the clinician’s ability to detect depression is sometimes affected by the presence of comorbidities. Literature has indicated that comorbidity between physical illness and depression often complicates the recognition, treatment, and prognosis of depression.6
More than 150 million people suffer from depression at any point of time in the world.7 Also, the World Health Organization (WHO) estimated that depression is the fourth most important contributor to the global burden of disease and comprised 4.4% of the total disability-adjusted life years in the year 2004.8
The WHO estimated that nearly 15% of the global population on average suffered from depression at least once in their lives. Also, the WHO estimated that neuropsychiatric disorders account for a total of 28% of the global burden of disease, of which more than one-third are accounted for by depression.8 In North America, the probability of having a major depression episode within a 1-year period of time is 3%–5% for males and 8%–10% for females.9
Depression was the leading cause of disability as measured by years lived with disability and the fourth leading contributor to the global burden of disease in 2000.9 By the year 2020, depression is projected to reach second place in the ranking of the major causes of disability-adjusted life years calculated for all ages and both sexes.10 Depression accounts for 5% of the total burden of diseases from all causes.11
Mental disorders are more common in clinical than in community setting as evidenced by the study conducted in Kenya (n=2,770) among inpatient and outpatient clients. This study showed that 42% of the subjects had symptoms of mild and severe depression. Only 114 (4.1%) of subjects had a file or working diagnosis of a psychiatric condition.12
Literature from high-income countries suggest that almost 20% of adults will have a mood disorder requiring treatment during their lifetime and that about 8% of adults will have a major depressive disorder during their lives.13
In Ethiopia, depression contributes to about 6.5% of the burden of diseases.14 The prevalence of depression in Ethiopia was reported to be 5%.15
The World Health Organization report on mental health suggests that undiagnosed depression places a significant socioeconomic burden on individuals, families and community in terms of increased service needs, lost employment, reduced productivity, poor parental care with the risk of transgenerational effect, and an increased burden on caregivers.16
The average annual health cost for depressed patients, including medical, pharmaceutical, and disabling costs, was 4.2 times higher than that of the general population.17
Studies carried out so far in different countries of the world5,18–26 have shown that symptoms of depression among medical patients were common and were associated with various factors. However, little is known about the prevalence of depression among medical patients. Therefore, this study was performed to determine the prevalence of depression and factors associated with it among patients attending the medical outpatient department (OPD).
Materials and methods
An institution-based cross-sectional study design was conducted from March 1 to March 30, 2016 in Adare Hospital’s adult medical OPD. Adare Hospital was established in Hawassa town in 1954 as a health center and attained General Hospital status on February 1, 2003. The hospital is 273 km away from Addis Ababa. Currently, the hospital is serving about 126,458 people in different outpatient and inpatient departments.
All patients who attended adult medical OPD at Adare Hospital were the source population, and those who were attending adult medical OPD at Adare Hospital during the study period and who fulfilled inclusion criteria were considered as study population. Clients who were already diagnosed with mental illness and unable to communicate during the interview as a result of critical illness were excluded from this study.
The sample size was determined using a single population proportion formula considering the following assumptions: standard normal distribution with confidence interval (CI) of 95% (Z=1.96), absolute precision or tolerable margin of error (d=0.05), and anticipated proportion of patients who experience depression =30.3% (P) taken from the study conducted in Malawi.27 Since the source population was <10,000, we used a correction formula and added 10% nonresponse rate; so, the final sample size was 326.
A systematic random sampling technique was used to select the respondents for interview. A total of 43,200 and 3,600 clients attend the medical OPD annually and monthly, respectively. The sampling fraction (K) was obtained by dividing monthly average number of patients attending outpatient department for the sample size, 3,600/326 which is 11. The first individual was selected using a lottery method, and the rest were selected at a regular interval using systematic random sampling method.
The Patient Health Questionnaire 9 (PHQ-9) was used to assess whether the respondents had experienced symptoms associated with depression within 2 weeks before the interview. The PHQ-9 has demonstrated acceptable reliability and validity. Sensitivity and specificity of PHQ-9 score was 88% for major depression. The PHQ-9 was translated and validated for use in Ethiopia. Depression was measured using PHQ-9 with a 3-point severity scale over the last 2 weeks. Based on the instrument standard, a PHQ-9 score ≥5 was considered as significant for meeting the symptoms of depression. The PHQ-9 incorporates the Diagnostic and Statistical Manual for Mental Disorder Version IV depression criteria along with other leading depression symptoms into a brief self-report tool.28
The Amharic version of “PHQ-9” for screening of depression was utilized. Semistructured questionnaires were used to collect sociodemographic, substance use, and clinical factors. Current use of a substance was defined as substance use in the last 3 months.
Two nurses with diplomas who received a 2-day intensive training on data collection techniques were involved in data collection. The pretest was done at Melkaoda Hospital on 5% of sample, and Cronbach’s α was used to check the reliability of the tool. The value of Cronbach’s α was >0.71 for the entire tool. Data collection was supervised, and each questionnaire was checked for completeness by the supervisor on a daily basis.
Collected data were entered and analyzed using SPSS version 20 (IBM Corporation, Armonk, NY, USA). Descriptive statistics was used to identify the distribution of sociodemographic characteristics of the study participants. The prevalence estimates of depression were calculated. The distribution of PHQ-9 scores among men and women as well as the prevalence of each specific symptom was also estimated. Both bivariate and multivariate logistic regression analyses with 95% CI were used to see the association between each independent variables and depression. Finally, those variables that showed statistical significance at P<0.05 and 95% CI in the final model were reported as being independently associated with depression.
Ethical clearance was obtained from the ethical review board of Hawassa University, College of Medicine and Health Science. Ethical issues of the participants were addressed throughout the study. All participants of the study were provided with an informed consent form, clearly stating the objectives of the study and their right to refuse; the form also stated that if they did not want to answer any question, they had the right to do so. All participants were randomly selected without any discrimination on any ground. Filled out questionnaires were carefully handled, and all access to results was kept strictly within the members of the group.
Results
Three hundred and twenty-six clients were contacted, and 326 respondents gave a complete response with a response rate of 100%. The mean age of the clients was 34±13.1 years. The majority of participants were men (57.1%), married (53.1%), Protestant (50.9%), employed (34.9%), and Sidama by ethnicity (58.9%), and 8.9% of the respondents had no formal education. About 13.2% of clients were reported to have a family history of mental illness (Table 1).
Substance use status of study participants
About 32.1% of respondents were current substance users, and of this, current users of khat, alcohol, and tobacco were 16.3%, 26.1%, and 8.6%, respectively.
Current chronic medical illness of study participants
Of all respondents, 158 (48.1%) had chronic medical illness (Figure 1).
The prevalence of depression
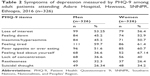
According to PHQ-9, 80 (24.5%) of study subjects were identified as having a depressive episode in the 2 weeks preceding the survey, while detection rate of depression by the clinician was 0%. Women had higher prevalence (26.4%) of all depression symptoms compared with men (23.1%). From the total of nine items, loss of interest (56.4%) and feelings of tiredness (61.4%) were the most common symptoms reported among women, whereas restlessness was more common symptoms experienced by men (Table 2).
Factors associated with depression
Determinants that had significant associations on bivariate analysis at P-value <0.2 were then entered for multivariate analysis. The following variables were associated (P<0.05) with increased odds of depressive symptoms: depressive symptomatology was associated with female sex, age >60 years, being divorced, and having an income <750 ETB.
Women were 1.6 times as likely as men to exhibit symptoms of depression (adjusted odds ratio [AOR] =1.63 [1.14–2.34]), and respondents who were aged >60 years were more likely to develop depression (AOR =4.14 [1.87–9.14]). The likelihood of having depression symptoms was higher in those who were divorced (AOR =3.13 [1.70–5.76]). Respondents who had an average monthly income <750 ETB were 1.9 times more likely (AOR =1.92 [1.119–3.195]) to exhibit depression symptoms (Table 3).
Discussion
The overall prevalence of depression among patients attending Adare Hospital was 24.5%. This finding is similar to the results of studies carried out in India (23.8%),18 Malawi (30.3%),27 France (25%), and the USA (19.2%),29 but demonstrates a higher prevalence than that reported in South Korea primary care setting (14.1%).19 The higher prevalence in the current study might reflect the particular psychosocial stresses experienced by this group of patients.
Women were 1.6 times more likely to experience depression compared with men. This finding is consistent with reports from Pakistan,30 Nigeria,31 and India.18 It has been shown that mental health problems, particularly depression, affect women to a greater extent than men, and this finding is consistent across diverse societies and social contexts.32 Proportionally, symptoms of depression were more common in women compared with men across all age groups. The reason might be the pressure created by their multiple roles and responsibilities, sex discrimination, and associated factors such as sex-based violence that contribute to women’s poor mental health.33
Depression was significantly associated with age. Study subjects aged >60 years were 4.1 times more likely to develop depression as compared with those aged 18–30 years. The finding in this study was consistent with the study conducted in Debre Berhan.34 The possible reason might be that aging leads to neurotransmitter level decline, which affects communication in nerve cells, which leads to common mental disorder33 and increased prevalence of physical comorbidity with advancing age.
The finding reveals that being divorced was positively associated with depression. Respondents who were divorced were 3.1 times more likely to develop depression. This finding was in line with the study conducted in India,18 which showed that being divorced is a consistent risk factor for depression. The finding implies the unstable marital relationship and the loss of partner increase the risk of having depression episodes.
Low income was significantly associated with depression. Subjects who earned <750 ETB were 1.9 times more likely to develop depression as compared to those who earned >1,200 ETB. This finding is consistent with the study done in Harar35 and Debre Berhan.34 This might be because an insufficient income leads to a feeling of being in a stressful and unsafe situation, which may trigger depression. People experiencing poverty face difficulties to fulfill basic needs and are unable to afford the treatment, and this interferes with their ability to participate in the productive activity. Higher levels of hopelessness toward the present rather than the future and lower level of satisfaction with life are some of the psychological impacts of low socioeconomic status.36
Conclusion
Unrecognized depression is common in nonpsychiatric OPDs in Adare Hospital. This study found that the prevalence rate of depression was 24.5% among the patient sample tested. The results revealed the magnitude of depression that is prevalent in the health-care service that goes undiagnosed and unmanaged. Age, sex, marital status, and monthly income were the most important risk factors for depressive episodes.
We recommended that health-care providers do through assessment to address common mental disorders, especially depression, and suggest that training to recognize and manage depression appropriately be given. There is a need to screen patients presenting in medical OPDs for depression. Health-care service and health personnel need to recognize this as an important entity and focus on the detection of unrecognized forms of depression, which may be perhaps due to lack of awareness among patients and providers.
Acknowledgment
We thank School of Nursing and Midwifery, College of Medicine and Health Sciences, Hawassa University for supporting the research on different ways. Also, we extend our heartfelt thanks to Adare Hospital Outpatient case team members and study participants for providing us necessary information.
Author contributions
NM and ET designed and supervised the study, carried out analysis, and interpreted the data; ABT and GB assisted in the design, analysis, and interpretation of the data; and ABT wrote the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
National Institute for Health and Clinical Excellence. Depression: The Treatment and Management of Depression in Adults (Updated Edition). London, UK: NICE; 2009:6–11. | ||
World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Geneva, Switzerland: World Health Organization; 2010:240–261. | ||
National Institute of Mental Health. Depression. Bethesda, MD: National Institute of Mental Health; 2013:81–86. | ||
University of Maryland Medical Center. Depression – Risk Factors. Baltimore, MD: University of Maryland Medical Center; 2013:140–157. | ||
Al-Otaibi B, Al-Wegayyan A, Taher H, et al. Depressive symptoms among Kuwaiti population attending primary healthcare setting: prevalence and influence of sociodemographic factors. Med Princ Pract. 2007;16(5):3484–3488. | ||
Muhwezi W, Agren H, Musisi S. Detection of major depression in Uganda primary healthcare settings using simple questions from a subjective well-being subscales. Soc Psychiatry Psychiatr Epidemiol. 2007;42:61–69. | ||
World Health Organization. Mental Health and a State of Well-Being. Geneva, Switzerland: World Health Organization; 2011:24–39. | ||
Kastrup MC, Ramos AB. Global mental health – secondary publication. Dan Med Bull. 2007;54(1):42–43. | ||
Andrade L, Caraveo-Anduaga JJ, Berglund P, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res. 2003;12(1):3–21. | ||
World Health Organization. Mental Health and a State of Well-Being. Geneva, Switzerland: World Health Organization; 2012:41–59. | ||
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global Burden of Disease and Risk Factors. Washington, DC: The International Bank for Reconstruction and Development/The World Bank Group, Oxford University Press; 2006:978–991. | ||
Ndetei DM, Khasakhala LI, Kuria MW, Mutiso VN, Ongecha-Owuor FA, Kokonya DA. The prevalence of mental disorders in adults in different level general medical facilities in Kenya. Ann Gen Psychiatry. 2009; 8(1):1–8. | ||
Remick RA. Diagnosis and management of depression in primary care: a clinical update and review. CMAJ. 2002;167(11):1253–1260. | ||
Bitew T. Prevalence and risk factor of depression in Ethiopia: a review. Ethiop J Health Science. 2014;24(2):161–169. | ||
Marcus M, Taghi Yasami M, van Ommeren O, Chisholm D, Saxena S. Depression: A Global Public Health Concern. Geneva, Switzerland: World Health Organization; 2012. Available from: http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf?ua=1. Accessed January 23, 2015. | ||
Okello ES, Neema S. Explanatory models and help-seeking behavior: pathways to psychiatric care among patients admitted for depression in Mulago hospital, Kampala, Uganda. Qual Health Res. 2007;17(1):14–25. | ||
World Health Organization. Investigating Mental Health. Geneva, Switzerland: World Health Organization; 2013:123–131. | ||
Kohli C, Kishore J, Agarwal P, Singh SV. Prevalence of unrecognized depression among outpatient department attending a rural Hospital, Delhi. J Clin Diagn Res. 2013;7(9):1921–1925. | ||
Jo SJ, Yim HW, Jeong H, et al. Prevalence of depressive disorder of outpatients visiting two primary care settings. J Prev Med Public Health. 2015;48(5):257–263. | ||
Hailemariaum S, Tessema F, Asefa M, Tadesse H, Tenkolu G. The prevalence of depression and associated factors in Ethiopia: findings from the National Health Survey. Int J Ment Health Syst. 2012;6:1–16. | ||
Roy T, Lloyd CE, Parvin M, Mohiuddin GK, Rahman M. Prevalence of comorbid depression in out-patients with type 2 diabetes mellitus in Bangladesh. BMC Psychiatry. 2012;12:123. | ||
Amit R, Ethirag D, Anil B, Sandeep G, Pramil T. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary health center. Indian J Med Res. 2010;132:195–200. | ||
Obadeji A, Oluwole LO, Dada MU, Ajiboye AS, Kumolalo BF. Assessment of depression in primary care setting in Nigeria using the PHQ-9. J Family Med Prim Care. 2015;4(1):30–34. | ||
Neupane D, Panthi B, McLachlan CS, Mishra SR, Kohrt BA, Kallestrup P. Prevalence of undiagnosed depression among person with hypertension and associated factors: a cross-sectional study in urban Nepal. PLoS One. 2015;10(2):e0117329. | ||
Worku DK, Yifru YM, Postels DG, Gashe FE. Prevalence of depression in Parkinson’s disease patient in Ethiopia. J Clin Mov Disord. 2014;5(1):10–25. | ||
Bifftu BB, Dachew BA, Tiruneh BT, Tebeje NB. Depressions among people with epilepsy in Northwest Ethiopia: a cross-sectional institution based study. BMC Res Notes. 2015;8:585. | ||
Udedi M. The prevalence of depression among patients and its detection by Primary Health Care Workers at Matawale Health Center (Zomba). Malawi Med J. 2014;26(2):34–37. | ||
Akena D, Joska J, Obuku EA, Amos T, Musisi S, Stein DJ. Comparing the accuracy of brief versus long depression screening instruments which have been validated in low and middle income countries: a systematic review. BMC Psychiatry. 2012;12(1):187. | ||
World Health Organization. The World Mental Health Report – Health Systems: Improving Performance. Geneva, Switzerland: World Health Organization; 2000:14–17. | ||
Dogar IA, Azeem MW, Kiran M, Hussain I, Mehmood K, Hina I. Depression and anxiety in cancer patients attending outpatient department of a tertiary hospital in Pakistan. Pak J Med Sci. 2009;25(5):734–737. | ||
Agbir TM, Audu MD, Adebowale TO, Goar SG. Depression among medical outpatients with diabetes: a cross-sectional study at Jos University Teaching Hospital, Jos, Nigeria. Ann Afr Med. 2010;20(3): 5–10. | ||
Dawodu A, Wagner CL. Prevention of vitamin D deficiency in mothers and infants worldwide – a paradigm shift. Pediatr Int Child Health. 2012;32(1):3–13. | ||
WHO. The Global Burden of Disease: 2014 Update. Geneva, Switzerland: World Health Organization; 2014:21–28. | ||
Eshetu DA, Woldeyohannes SM, Kebede MA, et al. Prevalence of depression and associated factors among HIV AIDS patients attending ART clinic at Debrebirhan Referral Hospital, North Showa, Amhara Region, Ethiopia. J Clin Psychiatry. 2015;9(2):13–25. | ||
Mohammed M, Mengistie B, Dessie Y, Godana W. Prevalence of depression and associated factors among HIV patients seeking treatments in ART Clinics at Harar Town, Eastern Ethiopia. J AIDS Clin Res. 2015;6:474. doi:10.4172/2155-6113.1000474. | ||
Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81(8):609–615. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.