Back to Journals » Clinical and Experimental Gastroenterology » Volume 16
Prevalence of Oral Helicobacter pylori Infection in an Indigenous Community in Southwest Mexico
Authors Urrutia-Baca VH, Gonzalez Brosig KI, Salazar-Garza AA, Gomez-Flores R, Tamez-Guerra P, De La Garza-Ramos MA
Received 6 June 2023
Accepted for publication 12 September 2023
Published 21 September 2023 Volume 2023:16 Pages 173—180
DOI https://doi.org/10.2147/CEG.S424559
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Andreas M. Kaiser
Victor Hugo Urrutia-Baca,1,* Karen Ivonne Gonzalez Brosig,2 Alina Abigail Salazar-Garza,3,* Ricardo Gomez-Flores,4 Patricia Tamez-Guerra,4 Myriam Angelica De La Garza-Ramos3,*
1Institute for Obesity Research, Tecnologico de Monterrey, Monterrey, Nuevo León, México; 2School of Health Sciences, Universidad del Valle de Mexico, Monterrey, Nuevo León, México; 3School of Dentistry, Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo León, México; 4School of Biological Sciences, Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo León, México
*These authors contributed equally to this work
Correspondence: Myriam Angelica De La Garza-Ramos, School of Dentistry, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, Mexico, Tel +52 811 3404 370 ext. 1781, Email [email protected]
Purpose: Epidemiological studies have been conducted to improve the health and economic quality of life of indigenous communities in Mexico. These studies have found that infections cause frequent health problems. Helicobacter pylori are responsible for conditions ranging from gastritis to stomach cancer. This study determined the prevalence of H. pylori in families from Siltepec, Chiapas, Mexico.
Patient and Methods: Ninety-nine dental plaque samples from 36 families were studied. Real-time PCR was performed to detect H. pylori using previously reported primers. The Mann–Whitney U-test was used for the statistical analysis. According to the family role of H. pylori-positive individuals, the VacA s1/m1 genotype and CagA gene correlated.
Results: The mother had the highest expression of VacA s1/m1-/cagA- with 19% (8/42), followed by the first child with 14.3% (6/42). The major roles for the vacA s1/m1+/cagA- were the mother and first child with 9.5% (4/42), followed by the remaining children with 4.8% (2/42). The vacA s1/m1-/cagA+ genotype was 7.1% (3/42) for the mother and 4.8% (2/42) for the father. Finally, the vacA s1/m1+/cagA+ genotype only appeared in the mother, son I, and son III with 2.4% (1/42).
Conclusion: The vacA s1/m1/cagA genotypes predominated in the mother, suggesting potential transmission between the mother and child during the first years of life.
Plain Language Summary: Helicobacter pylori is a bacterium that causes duodenal and gastric ulcers and is a risk factor for gastric cancer. It has been found in the dental plaque of children and adults. This study was conducted to identify if the mother can transmit the infection to her children.
Keywords: Helicobacter pylori, infection, gastrointestinal diseases, infection transmission, nutrition
Introduction
Helicobacter pylori is a gram-negative, microaerophilic, curved bacillus with multiple sheathed polar flagella that infects the human gastrointestinal mucosa.1 This bacterium is the most common cause of chronic gastritis and gastric and duodenal ulcers.2
The International Agency for Research on Cancer (IARC), a World Health Organization agency specializing in cancer, classified H. pylori as a group 1 carcinogen for humans due to its close relationship with the development and progression of gastric adenocarcinoma, among others.3 This pathogen is one of the most prevalent worldwide, mainly in developing countries, with a prevalence of colonization of 70% in adults and 50% in children influenced by socioeconomic status and quality of life.4
H. pylori has many virulence factors that allow establishment, colonization, and damage to the gastric epithelium. Strains with alleles s1/m1 secrete an active toxin associated with developing peptic ulcers and gastric cancer; this region was also recently described as a determining factor in the cytotoxicity and development of gastric disorders.5 Some strains of H. pylori produce the CagA cytotoxin, It is reported that individuals infected with cagA-positive and certain cagA alleles (eg, cagA1a) have a higher risk of developing peptic ulcer and gastric cancer.6
H. pylori is commonly spread from person to person through saliva and by consuming food or water contaminated with fecal matter. It is usually acquired during childhood, and infection increases with age. Most children in developing countries are infected by age ten.4,7 In the search to understand transmission in children, studies suggest that the mother-child relationship is a crucial factor for H. pylori transmission in the early stages of life.8 In one study, children with H. pylori-positive mothers had a relative risk of contracting the infection 5.3 times higher than children whose mothers were negative.9 Konno et al10 reported that there is a predominance of transmission of H. pylori infection from mother to child. The mother spends more time in contact with the child than the father. Parenting and childcare practices, including breastfeeding, bottle-feeding, or using a pacifier, are often handled by the mother.11 On the other hand, some reports suggest that H. pylori infection can be acquired from siblings, mainly from older siblings to younger siblings.12,13 However, few studies on the relationship of H. pylori strains between families and members use molecular genotyping techniques.10,14 Therefore, this intrafamilial transmission of H. pylori could contribute to the exchange and persistence of pathogenic strains associated with developing associated diseases. H. pylori has been detected in children and their families in the subgingival dental plaque, which acts as a reservoir for the bacteria.15,16
The frequency of H. pylori in Mexican children has decreased in recent years, while in 1998, the frequency of infection was found to be 50%; in 2012 and 2018, it was 38%.17,18 However, the diagnosis of H. pylori infection in children is difficult to make since symptoms such as abdominal pain, nausea, vomiting, and occasionally diarrhea are nonspecific.19 There are no previous studies focused on the analysis of infection within the family and genotyping of H. pylori until the present study.
This study aims to verify the transmission of H. pylori between mothers and children in Siltepec, Chiapas, Mexico.
Patients and Methods
Study Design
This descriptive cross-sectional study was conducted during a medical brigade in Siltepec, Chiapas, Mexico, a rural indigenous community with 38,143 inhabitants in the Sierra Madre of southwestern Mexico (15° 33’ N and 92° 20’ W). The region is considered a producer of migrants, with high levels of poverty and marginalization.
The Ethics Committee of the School of Dentistry of the Universidad Autonoma de Nuevo Leon reviewed and approved the study with registration number SPSI-01613/00147. All experiments were performed in accordance with the Research Regulations of the Universidad Autonoma de Nuevo Leon and the ethical principles of the Declaration of Helsinki.
Ninety-nine individuals corresponding to 36 families, signed informed consent and participated in the study. Informed consent of the parents and/or legal guardians and the child´s consent was obtained from individuals under 18. The inclusion criterion was families with at least one mother and one child. The exclusion criteria were antimicrobial and/or antiviral use at the time or three months before the study, systemic disease, symptoms of dyspepsia, a history of gastrointestinal disease, pregnant women, and a positive diagnosis of H. pylori infection before the study.
Oral Cavity Sampling
A certified dental surgeon collected a sample of the dental plaque from each participant from the supragingival and subgingival regions. Subsequently, the sample was placed in a 1.5 mL tube containing soy trypticase supplemented with 10% glycerol. These samples were stored at –20°C and transported to the CIDICS-UANL laboratory with appropriate biosafety measures for processing.
Oral H. Pylori Detection
The commercial GeneJET genomic DNA purification Kit (Cat #K0721, Thermo Scientific, Waltham, MA, USA) was used for genomic DNA extraction according to the manufacturer’s recommendations. Real-time PCR was performed for H. pylori detection using the primers previously reported by Mendoza-Cantu et al17 qPCR reactions were performed in 96-well plates containing 12.5 μL of 2X maxima qPCR master mix (Thermo Scientific), 0.3 μM primers mix forward/reverse, 0.2 μM probe, and 100 ng of the sample. DNA 100 ng from H. pylori strains ATCC 700824 or ATCC43504 and nuclease-free water 25 μL was added as a positive and negative control, respectively. The qPCR assay was carried out in a LightCycler 480 II thermal cycler (Roche, Mannheim, Germany). The thermal cycler was programmed with a single-color hydrolysis probe format (6-FAM, filter combination 465 nm excitation, and 510 nm emission) as follows: one denaturalization cycle (95°C, 10 min), thirty-five amplification cycles (95°C, 10s, 4°C/s ramp rate; 55°C, 15s, 2°C/s ramp rate; 72°C, 15s, 4°C/s quantification analysis ramp rate), one melting cycle (95°C, 5s, 4°C/s ramp rate; 65°C, 1 min, 2.2°C/s ramp rate, 97°C with a 5°C continuous acquisition), and one cooling cycle (40°C, 10s, 1.5°C/s ramp rate).
An absolute quantification analysis was performed using the LightCycler 480 II version 1.5 software (Roche Molecular Systems, Inc., Pleasanton, CA, USA) and Rest 2009 version 1.22 software (QIAGEN GmbH, Hilden, Germany).
Statistical Analysis
The association between oral H. pylori infection and each nominal variable was determined using the Chi-square and Fisher’s exact tests. One-way ANOVA, Tukey’s post hoc, and Student’s t-test were used to compare means. The Kruskal–Wallis and the U-Mann–Whitney tests were used for numerical variables. A p-value <0.05 was statistically significant. Data were analyzed with SPSS IBM v22.0 statistical software.
Results
Ninety-nine subjects were evaluated. The majority were women, 61.6% (61/99), with a mean age of 21 ± 16. Of the total sample, 42 (42.5%) were positive for H. pylori. Twenty-eight women (28.3%) and 14 men (14.1%) were H. pylori positive. The mean age of the infected individuals was 23.8 ± 15.81. Negative patients had a lower mean age (19.2 ± 15.47).
The subjects were classified according to their family role related to H. pylori infection; 51 children (51.5%), 31 mothers (31.3%), and 14 fathers (14.1%). The children had the highest prevalence of oral infection with H. pylori (18.2%; 12.2% first son, 3% second son, and 3% third son), followed by the mothers with 16.2% and the fathers with 6.1% (Table 1).
 |
Table 1 The Prevalence of H. Pylori Infection Related to the Family Role |
According to the mother-child intrafamily relationship, eight families (22.2%) had a mother with at least one child with H. pylori infection; in four (11.1%), a father and at least one child, and in 3 (8.3%) families, both parents and at least one child, had an infection (Table 2).
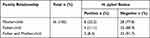 |
Table 2 Distribution of the Families Based on H. Pylori Infection and the Relationship Between Parents and Children |
In infected patients, the prevalence of the vacA s1/m1 and CagA genes was 40.5% (17/42) and 21.4% (9/42), respectively. Most of the subjects (19/42; 45.2%) had the vacA s1/m1-/cagA- genotype; however, 14 (33.4%) had the vacA s1/m1+/cagA- genotype. The vacA s1/m1-/cagA+ genotype was only present in 6 (14.3%), and 3 individuals (7.1%) had the vacA s1/m1+/cagA+ genotype.
The relationship with gender and age of the subjects was identified according to the number of genotypes. Females had the highest number of vacA s1/m1-/cagA- genotypes (13/42; 31%). The vacA s1/m1+/ cagA- was present in 10 (23.8%). This genotype was also observed in males but in fewer subjects. Three (7.1%) individuals in both genders had the vacA s1/m1-/cagA+ genotype. Finally, two (4.8%) females and one male (2.4%) had the vacA s1/m1+ /cagA+ genotype (Table 3).
 |
Table 3 Distribution of H. Pylori Genotypes |
The genotypes varied according to the age of the patients, 19.52 ± 17.3 for the genotype vacA s1/m1+/cagA-; 15.8 ± 19.5 for vacAs1/m1+/cagA+, 26.63 ± 14.83 for vacAs1/m1-/cagA-, and 28.83 ± 13.43 for vacA s1/m1-/cagA+.
The family role of the H. pylori-positive individuals was evaluated. The genotypes of the VacA s1/m1 and CagA genes correlated. For the vacA s1/m1-/cagA- genotype, the mother was the role with the highest expression with 19% (8/42), followed by the first son with 14.3% (6/42). The majority roles were that of the mother and the first child, with 9.5% (4/42), followed by the rest of the children with 4.8% (2/42) for the vacA s1/m1+/cagA- genotype. The vacA s1/m1-/cagA+ genotype was 7.1% (3/42) for the mother, which is the majority role, followed by the father with 4.8% (2/42). Finally, the vacA s1/m1+ cagA+ genotype appeared in only one individual each (2.4%) for the mother, first son, and third son.
The genotypes found in each family member were identified according to the number of families, considering the presence of the genotypes in at least 1 family member (Table 4). Coinfection with two different genotype combinations was found in 6/36 families (16.6%). Coinfection with the vacA s1/m1+/ cagA- and vacA s1/m1-/ cagA- genotypes was observed in 4/36 families (11.1%). Coinfection with the vacA s1/m1-/cagA- and the vacA s1/m1-/cagA+ genotypes was observed in 2/36 families (5.5%). In 1/36 families (2.7%), three genotypes were observed, vacA s1/m1+/cagA+, vacA s1/m1-/cagA-, and vacA s1/m1- /cagA+.
 |
Table 4 Distribution of Helicobacter Pylori Genotypes in Families with at Least One Infected Member |
Discussion
Dental plaque samples were obtained from families in the Siltepec, Chiapas community to verify the presence of H. pylori in dental plaque. We found that in at least 15 out of 36 families, a member was infected with H. pylori; in 8 out of 36 families, the mother and at least one child were infected. In 3 out of 36 families, both parents and the child were infected, and in 4 out of 36 families, the father and child were infected.
The presence of H. pylori in dental plaque has been confirmed in several studies. This finding has been related to gastrointestinal reinfection.15,17 Tsami et al16 conducted a study in which dental plaque samples were taken from 35 children with gastrointestinal symptoms and 45 family members (mother or father). Gastric biopsies were also collected from all the children. They concluded that 15/35 were positive for H. pylori and 6/15 infected children, and 20 non-infected children were also positive in dental plaque samples. H. pylori was found in the dental plaque of 7 mothers and 4 fathers of the corresponding positive children.
Umeda et al20 studied the prevalence of H pylori using nested PCR. They studied supragingival plaque, tongue, and whole saliva samples and found that the bacterium persisted in the oral cavity even after eradication from the stomach and duodenum. H. pylori was identified in dental plaque in 41.2% of subjects with periodontal pockets ≥4 mm and 9.1% with probing depths <4 mm. These findings indicate that periodontal pockets might be favorable for H. pylori.
Reinfection with H. pylori is frequent in developing countries. It is classified as recrudescence when recolonization occurs with the same strain within 12 months after eradication and reinfection when infection occurs due to colonization with a new strain more than 12 months after eradication.21 Current quadruple therapy with a proton pump inhibitor, bismuth, tetracycline, and levofloxacin for 5 to 7 days has been highly effective.22 It is known that vertical and horizontal transmission of infection can occur. Vertical transmission is an infection that spreads from ascendant to descendent within the same family. Horizontal transmission involves contact with individuals outside the family or environmental contamination. The fact that the stomach is the only reservoir and that H. pylori can persist in the oral cavity is evidence of the possibility of intrafamily transmission of the disease.7
Another contact transmission that influences mother-to-child transmission is the presence of H. pylori in the mother’s vagina; H. pylori may colonize in an acidic vaginal environment.23 Several articles indicated vertical transmission of H. pylori exists in the vagina during birth. The prevalence of H. pylori in pregnant women is about 20%.24
The family infection rate in this study was 41.67% (15/36 families). These data have important practical implications that make it feasible to apply and incorporate the strategies for treating and preventing H. pylori infection among family members.
In 2021, experts from China conducted a national consensus to review current evidence and develop strategies for population-wide and family-wide control and management of H. pylori infection.25 According to statement nine, they propose controlling and managing H. pylori infection in the family as an important strategy to prevent intra-family transmission and infection. Without a doubt, adapting and implementing these strategies could mitigate the disease burden in Mexico. Nguyen et al,26 developed a community-based cross-sectional study in 533 participants from 135 households with multiple generations living in the same household to investigate the relationship between H. pylori infection in children and other household members. They found a significant association between H. pylori infection in children and mothers. These results are consistent with those found in the present study.
Zhou et al27 conducted a study in 10,735 families (31,098 people) from 29 provinces of mainland China to examine familial H. pylori infection, related factors, and the transmission pattern. They reported an individual H. pylori infection rate of 40.66% (43.45% for adults and 20.55% for children and adolescents) and familial infection rates between 50.27% and 85.06% among 29 provinces (average 71.21%). In this study, we observed a slightly lower family infection rate, and the infection rate of adults (father plus mother; 22.3%) was higher compared to children (first, second plus third child; 18.1%), consistent with what was reported by Zhou et al.27
Despite the interesting results obtained in this study, it is limited by the number of families and individuals who participated. Conducting a massive study on this approach in different states and cities of Mexico is advisable.
Our results show that the mother is likely the primary source of infection for her children. This infection may be by oral-oral transmission, but it is important to consider that hygienic conditions are poor in underdeveloped countries. Ingestion of contaminated food or water cannot be ruled out.
Conclusion
There is a significant relationship between intrafamily infection and H. pylori in the dental bacterial plaque, which may act as a reservoir for the spread of infection.
Data Sharing Statement
The data supporting the study findings are available from the corresponding author, Myriam Angelica De La Garza-Ramos, upon reasonable request.
Acknowledgments
We thank Sergio Lozano-Rodriguez, M.D., MWC®, for his help in translating and editing the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bayona Rojas MA. Microbiological conditions for culturing Helicobacter Pylori. Rev Colomb Gastroenterol. 2013;28(2):94–99.
2. Kusters JG, van Vliet AHM, Kuipers EJ. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev. 2006;19(3):449–490. doi:10.1128/cmr.00054-05
3. Mobley HLT, Mendz GL, Hazell SL. Helicobacter Pylori: Physiology and Genetics. ASM Press; 2001.
4. Kienesberger S, Perez-Perez GI, Olivares AZ, et al. When isHelicobacter pyloriacquired in populations in developing countries? A birth-cohort study in Bangladeshi children. Gut Microbes. 2018;9(3):252–263. doi:10.1080/19490976.2017.1421887
5. Bachir M, Allem R, Tifrit A, et al. Primary antibiotic resistance and its relationship with cagA and vacA genes in Helicobacter pylori isolates from Algerian patients. Braz J Microbiol. 2018;49(3):544–551. doi:10.1016/j.bjm.2017.11.003
6. Momtaz H. Study of Helicobacter pylori genotype status in saliva, dental plaques, stool and gastric biopsy samples. World J Gastroenterol. 2012;18(17):2105. doi:10.3748/wjg.v18.i17.2105
7. Kayali S, Manfredi M, Gaiani F, et al. Helicobacter pylori, transmission routes and recurrence of infection: state of the art. Acta Biomed. 2018;89(8–S):72–76. doi:10.23750/abm.v89i8-S.7947
8. Mamishi S, Eshaghi H, Mahmoudi S, et al. Intrafamilial transmission ofHelicobacter pylori: genotyping of faecal samples. Br J Biomed Sci. 2016;73(1):38–43. doi:10.1080/09674845.2016.1150666
9. Malaty HM, Kumagai T, Tanaka E, et al. Evidence from a nine-year birth cohort study in japan of transmission pathways of Helicobacter pyloriInfection. J Clin Microbiol. 2000;38(5):1971–1973. doi:10.1128/jcm.38.5.1971-1973.2000
10. Konno M, S-i Y, Suga T, Takahashi M, Sato K, Fujii N. Predominance of mother-to-child transmission of helicobacter pylori infection detected by random amplified polymorphic DNA fingerprinting analysis in Japanese families. Pediatr Infect Dis J. 2008;27(11):999–1003. doi:10.1097/INF.0b013e31817d756e
11. Rosu O-M, Gimiga N, Stefanescu G, et al. The effectiveness of different eradication schemes for pediatric Helicobacter pylori infection—a single-center comparative study from Romania. Children. 2022;9(9):1391. doi:10.3390/children9091391
12. Mentis A-F. Merging Helicobacter pylori eradication and family history-based genetic counseling in patients with gastric cancer: towards an overarching approach in clinical practice. Ann Gastroenterol. 2021. doi:10.20524/aog.2021.0589
13. Cervantes DT, Fischbach LA, Goodman KJ, Phillips CV, Chen S, Broussard CS. Exposure to Helicobacter pylori–positive siblings and persistence of Helicobacter pylori Infection in early childhood. J Pediatr Gastroenterol Nutr. 2010;50(5):481–485. doi:10.1097/MPG.0b013e3181bab2ee
14. Roma-Giannikou E, Karameris A, Balatsos B, et al. Intrafamilial spread of helicobacter pylori: a genetic analysis. Helicobacter. 2003;8(1):15–20. doi:10.1046/j.1523-5378.2003.00126.x
15. Valdez-Gonzalez JA, Mares-Moreno PC, Kowolik MJ, Vargas-Villlarreal J, Gonzalez-Salazar F, De la Garza-Ramos MA. Detection of Helicobacter pylori in dental plaque of Mexican children by real-time PCR. Health. 2014;06(04):231–235. doi:10.4236/health.2014.64034
16. Tsami A, Petropoulou P, Kafritsa Y, Mentis YA, Roma-Giannikou E. The presence of Helicobacter pylori in dental plaque of children and their parents: is it related to their periodontal status and oral hygiene? Eur J Paediatr Dent. 2011;12(4):225–230.
17. Mendoza-Cantú A, Urrutia-Baca VH, Urbina-Ríos CS, De la Garza-Ramos MA, García-Martínez ME, Torre-Martínez HHH. Prevalence ofHelicobacter pylori vacAGenotypes andcagAGene in Dental Plaque of Asymptomatic Mexican Children. Biomed Res Int. 2017;2017:1–10. doi:10.1155/2017/4923640
18. Duque X, Vilchis J, Mera R, et al. Natural History of Helicobacter pylori Infection in Mexican Schoolchildren. J Pediatr Gastroenterol Nutr. 2012;55(2):209–216. doi:10.1097/MPG.0b013e318248877f
19. Bosques-Padilla FJ, Remes-Troche JM, González-Huezo MS, et al. IV consenso mexicano sobre Helicobacter pylori. Rev Gastroenterol Mex. 2018;83(3):325–341. doi:10.1016/j.rgmx.2018.05.003
20. Umeda M, Kobayashi H, Takeuchi Y, et al. High Prevalence ofHelicobacter pyloriDetected by PCR in the Oral Cavities of Periodontitis Patients. J Periodontol. 2003;74(1):129–134. doi:10.1902/jop.2003.74.1.129
21. Niv Y. H pylori recurrence after successful eradication. World J Gastroenterol. 2008;14(10):1477. doi:10.3748/wjg.14.1477
22. Matsumoto H, Shiotani A, Graham DY. Current and future treatment of Helicobacter pylori infections. Helicobacter pylori Human Dis. 2019;2019:211–225.
23. Xm W. Is there an association between oral helicobacter pylori and hypertension, coronary artery disease? J Hypertens Manag. 2016;2(1). doi:10.23937/2474-3690/1510008
24. Yee JKC. Are the view of Helicobacter pylori colonized in the oral cavity an illusion? Exp Mol Med. 2017;49(11):e397–e397. doi:10.1038/emm.2017.225
25. Ding S-Z, Du Y-Q, Lu H, et al. Chinese consensus report on family-based Helicobacter pyloriinfection control and management (2021 edition). Gut. 2022;71(2):238–253. doi:10.1136/gutjnl-2021-325630
26. Nguyen VB, Nguyen GK, Phung DC, et al. Intra-familial transmission of Helicobacter pylori infection in children of households with multiple generations in Vietnam. Eur J Epidemiol. 2006;21(6):459–463. doi:10.1007/s10654-006-9016-y
27. Zhou X-Z, Lyu N-H, Zhu H-Y, et al. Large-scale, national, family-based epidemiological study onHelicobacter pyloriinfection in China: the time to change practice for related disease prevention. Gut. 2023;72(5):855–869. doi:10.1136/gutjnl-2022-328965
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
