Back to Journals » Journal of Blood Medicine » Volume 14
Prevalence of Inherited Thrombophilia in Women with Recurrent Pregnancy Loss During the First Trimester of Pregnancy
Authors Yousif TYE
Received 30 December 2022
Accepted for publication 31 March 2023
Published 5 April 2023 Volume 2023:14 Pages 253—259
DOI https://doi.org/10.2147/JBM.S401469
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Tagwa Yousif Elsayed Yousif1,2
1Department of Medical Laboratory Technology, Faculty of Applied Medical Sciences, Jazan University, Gizan, 45142, Saudi Arabia; 2Department of Medical Laboratory Sciences, College of Medical Laboratory Sciences, Alneelian university, Khartoum, Sudan
Correspondence: Tagwa Yousif Elsayed Yousif, Email [email protected]
Purpose: This study aims to investigate the prevalence of inherited thrombophilia in women with recurrent pregnancy loss during the first trimester of pregnancy. The study was assessed the potential role of inherited thrombophilia in recurrent miscarriages and evaluate the consequences of this condition on the reproductive outcomes of affected women.
Material and Methods: This study was an analytical descriptive carried out in Khartoum, Sudan. The research comprised 98 controls who had given birth twice or more without experiencing a miscarriage and 120 patients. Each patient had done more than two miscarriages especially when the pregnancy is at its beginning trimester. (APCR), and (PS) were investigated using the clotting approach. There was an assessment of biological activities of (ATIII), (PC), and (PS) for both groups using the chromogenic method.
Results: The average age of the patients was 34, which was higher than the average age of the controls (33.5). The patient group had a much higher rate of multiple miscarriages among the women.: 35 (29.17%), 45 (37.50%), and 40 (33.33%). The incidence of PC deficiencies was determined to be 1.02% (1/98), whereas neither ATIII nor PS deficiencies were seen in the control group (0/98). APCR was more prevalent in the control group (4.10% or 4/98).
Conclusion: Despite contradicting evidence to the contrary in the literature, our findings imply that most miscarriages occur when pregnancy is at the first trimester when a woman is pregnant and they are all caused by thrombophilia.
Keywords: activated protein C resistance, antithrombin III, protein C, protein S, repeated miscarriages, thrombophilia
Introduction
Pregnancy loss that occurs three times in a row before the twentieth week of the last menstrual period is defined as recurrent pregnancy loss (RPL).1,2 Various underlying causes may be responsible for RPL, including uterine abnormalities, hormonal imbalances, autoimmunity, certain medications, chemicals, X-rays, and environmental factors. Additionally, genetic defects have also been identified as potential contributors. One such genetic defect is an alteration in the SERPINC1 (Serpin Family C Member 1) gene, which leads to an antithrombin III deficiency.3,4 Antithrombin III is a protein found in the blood and is responsible for keeping the balance between clotting and bleeding.5
Previous studies have indicated that thrombophilia, either inherited or acquired, is linked to recurrent pregnancy loss (RPL).6 Additionally, the relative risk of certain thrombophilia-related problems is often increased due to subpar case-control research designs, although the absolute risk is still extremely low.7 Antiphospholipid antibody syndrome should be thoroughly screened and undergo therapy if acquired thrombophilia is the primary cause of RPL.8,9
Protein C and S are both glycoproteins produced by the liver and are essential for the body’s natural anticoagulant system. Vitamin K, like its cofactor protein S, is also essential for protein C to function properly.10–12 Activated protein C (APC) is produced when the coagulation factor thrombin is exposed to protein C. Protein C activity is within the normal range in a healthy, non-complicated pregnancy.13–15
Injection of heparin during pregnancy can prevent blood clots in women with antithrombin deficiency, although it is estimated that only 3% to 50% of pregnant women with this deficiency actually develop a clot.16,17 Despite the evidence being scant, anticoagulation is used to protect women with hereditary thrombophilia from having a negative pregnancy outcome.18 Additionally, the independent roles of protein S deficiency and miscarriage have rarely been studied.19
Despite the evidence linking thrombophilia to RPL, no systematic study has been performed to properly evaluate the role of genetic thrombophilia in RPL risk. Therefore, the aim of this study is to assess the role of genetic thrombophilia in recurrent pregnancy loss by conducting a comprehensive meta-analysis. By doing so, we hope to fill the existing gap in the knowledge and provide a clearer picture of the impact of genetic thrombophilia on pregnancy outcome.
Material and Methods
This study was an analytical descriptive carried out in Khartoum, Sudan, the Scientific Research Ethics Committee of Alneelian University approved this research, which was done based on declaration of Helsinki. All participants in the study gave their informed consent.120 women who had experienced two or more miscarriages in the first trimester of their pregnancies made up the study group (patient group), as contrasted to 98 women in the control group who had delivered two or more infants without experiencing a miscarriage. Abortions in the first trimester of pregnancy are common, and the investigation could not rule out the possibility that these abortions were caused by chromosomal abnormalities, infections, anatomical abnormalities, or endocrine dysfunction. Women who were pregnant at the time of the study were barred from taking part in either study.
The plasma was separated by mixing 9 parts blood with 1 part sodium citrate (3.2%) and spinning the mixture at 2000 revolutions per minute (rpm) for 15 minutes. After collecting the plasma, it was kept at 35 degrees Celsius until testing could be performed. For the purpose of a hemostasis test. Chromogenic measurements of ATIII and PC were taken with the help of an automated coagulometer and the TEChrom AT (anti-Xa) and TEChrom PC kits from TECO GmbH. (Coatron 6). PS and APCR were evaluated utilizing the Coatron 6 and Amelung KC4 semi-automatic coagulometers, amongst other methods.
The odds ratio (OR) and 95% confidence interval were determined for each inhibitor separately. The Chi-square test in IBM SPSS V.22 was then used to assess APCR. We used a significance level of P 0.05 for all t-test comparisons.
Findings
One hundred and twenty women who had experienced two or more miscarriages during the first trimester of pregnancy (the patient group) and ninety-eight women (the control group) who had experienced two or more normal deliveries (without a miscarriage) were tested for the natural coagulation inhibitors ATIII, PC, PS, and APCR.
The frequency of errors in ATIII, PC, and PS are provided together with APCR. APCR, ATIII, PC, and PS deficits were seen in the patient group at rates of 5.00% (6/120), 4.17% (5/120), 5.00% (6/120), and 7.50% (9/120), respectively. While there were no ATIII or PS deficits in the control group, there were 1% (1.02%) (1/98) PC inadequacies. APCR was more prevalent in the control group (4.10% or 4/98). The ORs are 4.08 (0.49 34.4), 1.84 (0.585.79), and 4.25 (1.57–11.47), respectively, for PC, APCR, and total problems (Table 1).
 |
Table 1 The Prevalence of Antithrombin III, Protein C and Protein S Deficiencies and the Prevalence of APCR in the Women with RLP and in the Controls |
The data demonstrated no statistically significant difference in mean impairment scores between patients and controls on the ATIII, PC, PS, or APCR. The prevalence of ATIII, PC, and PS deficits, as well as APCR and Totals, did not differ significantly between the groups (Table 1).
In both controls and RLP-positive women, there were impairments in the prevalence of protein C, protein S, antithrombin III, and APCR. The distribution and average value of the frequency with which each group has ATIII, PC, and PS impairments. Discovered that ATIII, PC, and PS impairments in both populations result from heterozygote abnormalities. Patients had APCR-SR values between 1.45 and 2.10, while controls had values between 1.46 and 2.20, demonstrating the same trend (Table 2). With the methods were used, the normal range for ATIII, PC, and PS is 70–135%; however, the normal range for APCR-SR is greater than 2.2 (>2.2).
 |
Table 2 The Distribution and Mean Values of ATIII, PC, PS, and APCR Deficiency Frequencies, as Well as Their Frequencies Within Each Group, Were Calculated |
The median age of patients was 34 (range: 21–45), while it was 33 in the comparison group. The patients were 34.3 years old on average (SD 5.72). (SD 5.80) (Table 3).
 |
Table 3 Summary of the Age of the Two Groups |
In the patient group, 35 (29.17%) women had a history of 3 miscarriages, 45 (37.50%) had a history of 4 miscarriages and 40 (33.33%) had a history of more than 4 miscarriages (Table 4).
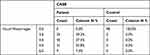 |
Table 4 Frequencies of the History of Miscarriages in Both Groups |
Correlations
For exploring of the relationships between different variables. The hypothesis of association will be significant if P < 0.05. Ran tests of association for various variables and the results were as follows. P = 0.000 which is highly significant. It is evident that the association between age and number of miscarriages for the patient group is significant. This suggests that the frequency of miscarriages among patients is significantly influenced by their age (Table 5).
 |
Table 5 Relationship Between Age and Number of Miscarriages for the Patients |
The results show there is no evidence that age of the patients affect the levels of ATIII, PC, PS or APCR to a significant level. It is not clear from the data above that the control group’s older age significantly influences the levels of ATIII, PC, PS, or APCR (Table 6).
 |
Table 6 Relationship Between Age and ATIII, PC, PS and APCR in Patients’ and Control Groups |
The foregoing data do not clearly show that ATIII, PC, PS, or APCR have a substantial impact on miscarriage rates. The connections between the various protein level pairings in the patients, however, are noteworthy (Table 7).
 |
Table 7 A Correlation Between the Number of Miscarriages, ATIII, PC, PS, and APCR in the Patient Group’s |
Employing the Chi-square test, can determine if there is a statistically significant connection between the patient and control groups with regards to their protein status. The table below displays the outcomes. According to the data above, ATIII and PS are considerably related with the group of women, however PC and APCR are not significantly connected with the women’s group (Table 8).
 |
Table 8 Relationship Between the Protein Level and the Group (Patient or Control) (Normal or Deficient) |
These findings show that the means for PC and APCR for the two groups of women are considerably different, although the results for ATIII and PS (for which we have already established that they are not independent in the previous sections) are inconsequential (Table 9).
 |
Table 9 T-Test for ATIII, PC, PS and APCR Protein Levels That are Group-Independent Samples |
Discussion
This study aimed to determine if and how activation protein C resistance (APCR), protein C and protein S deficiency, and antithrombin III (ATIII) levels were associated with repeated losses in the first trimester of pregnancy. One hundred twenty individuals with recurrent pregnancy loss (RPL) and ninety-eight healthy controls underwent tests for ATIII, PC, and PS deficiencies, as well as the existence of APCR. According to the current study, deficiencies in APCR, AT, PC, and PS may be found in both healthy individuals and those who have experienced thromboembolic events. Although it is yet unknown whether or not genetic thrombophilia plays a role in recurrent miscarriages, more patients than controls had ATIII, PC, or PS deficits, and more patients with APCR (2.99 for the minimum, 4.50 for the maximum, and 2.99 for the mean, compared to 2.23, 3.90, and 2.77 for the patient group).
However, ethical considerations should be taken into account when conducting studies of this nature.20 Women should be made aware of the potential risks associated with testing for genetic thrombophilias, such as false positives or inaccurate results. In addition, it is important that women are not pushed into testing if they do not feel comfortable doing so. Furthermore, informed consent must be obtained from all participants and any results should be kept confidential.
Overall, it is clear that there’s a need for better study designs to determine if a lack of ATIII, PC, or PS, or the presence of any other factor, was responsible for the patients’ recurrent miscarriages. Because of this, Walker et al propose that women who have them undergo frequent prenatal testing.12,21,22 However, hereditary thrombophilia testing is unnecessary for women experiencing repeated miscarriages or problems with late pregnancy outside of clinical research, as revealed by Patnaik et al11,12,23 Therefore, if a woman is at a higher risk of developing venous thromboembolism during pregnancy, she should be advised to use graduated compression stockings as early as possible in her pregnancy. Vascular uteroplacental insufficiency has been linked to an increased risk of venous thromboembolism, as well as acquired or hereditary thrombophilia.13,23
Conclusion
Research found that there were associations between different pairs of protein levels in patient groups, suggesting that thrombophilia may have a role in first-trimester losses.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Kupferminc MJ. Thrombophilia and pregnancy. Reprod. Biol Endocrinol. 2003;1(1):111. doi:10.1186/1477-7827-1-111
2. Brill-Edwards P, Ginsberg JS, Gent M. Safety of withholding antepartum heparin in women with a previous episode of venous thromboembolism. N Engl J Med. 2000;343(20):1439–1444. doi:10.1056/nejm200011163432002
3. Martinelli I. Thromboembolism in women. Semin Thromb Hemost. 2006;32(7):709–715. doi:10.1055/s-2006-951455
4. Robertson L, Wu O, Langhorne P, et al. Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: risk and Economic Assessment of Thrombophilia Screening (TREATS) study. Br J Haematol. 2005;132(11):171–196. doi:10.3310/hta10110
5. Simcox LE, Ormesher L, Tower C, Greer IA. Thrombophilia and Pregnancy Complications. Int J Mol Sci. 2015;16(12):28418–28428. doi:10.3390/ijms161226104
6. Tait RC, Walker ID, Perry DJ, et al. Prevalence of antithrombin deficiency in the healthy population. Br J Haematol. 1994;87(1):106–112. doi:10.1111/j.1365-2141.1994.tb04878.x
7. Gerhardt A, Scharf RE, Beckman MW. Prothrombin and factor V mutations in women with thrombosis during pregnancy and the puerperium. N Engl J Med. 2000;342(6):374–380. doi:10.1056/NEJM200002103420602
8. Robertson L, Wu O, Langhorne P, et al. Thrombophilia in pregnancy: a systematic review. Br J Haematol. 2006;132(2):171–196. doi:10.1111/j.1365-2141.2005.05847.x
9. Liu X, Chen Y, Ye C, et al. Hereditary thrombophilia and recurrent pregnancy loss: a systematic review and meta-analysis. Int J Mol Sci. 2021;36(5):1213–1229. doi:10.1093/humrep/deab010
10. Kluijtmans LA, van den Heuvel LP, Boers H, et al. Molecular genetic analysis in mild hyperhomocysteinemia: a common mutation in the methylenetetrahydrofolate reductase gene is a genetic risk factor for cardiovascular disease. Am J Hum Genet. 1996;58(1):35–41. PMID: 8554066.
11. Patnaik MM, Haddad T, Morton CT. Pregnancy and thrombophilia. Semin Respir Crit Care Med. 2007;28(5):753–765. doi:10.1586/14779072.5.4.753
12. Walker ID. Thrombophilia in pregnancy. J Clin Pathol. 2000;53(8):573–580. PMID: 11002758. doi:10.1136/jcp.53.8.573
13. Bates SM. Management of pregnant women with thrombophilia or a history of venous thromboembolism. Hematology Am Soc Hematol Educ Program. 2007;1(1):143–150. doi:10.1182/asheducation-2007.1.143
14. McNamee K, Dawood F, Farquharson RG. Thrombophilia and early pregnancy loss. Best Pract Res Clin Obstet Gynaecol. 2012;26(1):91–102. doi:10.1016/j.bpobgyn.2011.10.002
15. Arachchillage DJ, Mackillop L, Chandratheva A, Motawani J, MacCallum P, Laffan M. Thrombophilia testing: a British society for haematology guideline. Br J Haematol. 2022;198(3):443–458. doi:10.1111/bjh.18239
16. Mekaj Y, Lulaj S, Daci F, et al. Prevalence and role of antithrombin III, protein C and protein S deficiencies and activated protein C resistance in Kosovo women with recurrent pregnancy loss during the first trimester of pregnancy. J Hum Reprod Sci. 2015;8(4):224–229. PMID: 26752858. doi:10.4103/0974-1208.170407
17. Preston FE, Rosendaal FR, Walker ID, et al. Increased fetal loss in women with heritable thrombophilia. Lancet. 1996;348(9032):913–916. doi:10.1016/s0140-6736(96)04125-6
18. Alecsandru D, Klimczak AM, Velasco AG, Pirtea P, Franasiak JM. Immunologic causes and thrombophilia in recurrent pregnancy loss. Fertil Steril. 2021;115(3):561–566. doi:10.1016/j.fertnstert.2021.01.011
19. Dizon-Townson D, Miller C, Sibai B, et al. The relationship of the factor V Leiden mutation and pregnancy outcomes for mother and fetus. Obstet Gynecol. 2005;106(3):517–524. doi:10.1097/01.AOG.0000173986.32528.ca
20. Hatasaka HH. Recurrent miscarriage: epidemiologic factors, definitions, and incidence. Clin Obstet Gynecol. 1994;37(3):625–634. doi:10.1097/00003081-199409000-00016
21. Scharrer I, Hach-Wunderle V, Aygoren E, et al. Frequency and clinical manifestations of congenital ptasminogen and fibrinogen deficiency compared to AT III-, PC-, and PS- deficiency in patients suffering from thromboses. Fibrin Proteolysis. 1988;2(2):16–17.
22. Barbour LA, Oja JL, Schultz LK. A prospective trial that demonstrates that dalteparin requirements increase in pregnancy to maintain therapeutic levels of anticoagulation. Am J Obstet Gynecol. 2004;191(3):1024–1029. doi:10.1016/j.ajog.2004.05.050
23. GriYn JH, GriYn JH, GriYn JH, et al. Anticoagulant protein C pathway defective in a majority of thrombophilic patients. Blood. 1993;82(7):1989–1993. doi:10.1182/blood.V82.7.1989.1989
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
