Back to Journals » Journal of Blood Medicine » Volume 8
Prevalence of anemia and its associated factors among pregnant women receiving antenatal care at Aymiba Health Center, northwest Ethiopia
Authors Asrie F
Received 17 February 2017
Accepted for publication 16 March 2017
Published 11 April 2017 Volume 2017:8 Pages 35—40
DOI https://doi.org/10.2147/JBM.S134932
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin Bluth
Fikir Asrie
Department of Hematology and Immunohematology, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Introduction: Anemia is a global public health problem in both developing and developed countries; ~1.62 billion people suffer from anemia, and pregnant women are the most susceptible to it. The main aim of the present study was to assess the prevalence of anemia and associated risk factors among pregnant women receiving antenatal care at Aymiba Health Center, northwest Ethiopia.
Methods and materials: An institution-based cross-sectional study was conducted at Aymiba Health Center from January to March 2015. Hemoglobin level and intestinal parasitic infections in pregnant women were assessed. Sociodemographic data were collected using a structured questionnaire. The data were entered and analyzed using the SPSS version 20. Odds ratio, p<0.05, and binary logistic regression were used to assess the association of pregnant women’s sociodemographic characteristics with their hemoglobin levels and the prevalence of anemia.
Results: The mean with ±2 standard deviation of hemoglobin value was 12±1.3 (95% confidence interval [CI] =11.9–12.5), and the prevalence of anemia from a total of 206 study subjects was 52 (25.2%). Of this anemic group, 50 (24%) were in the second and third trimesters. Anemia was significantly associated with rural residence and intestinal parasitic infections (adjusted odds ratio [AOR] =9.17, 95% CI =2.15–40, p<0.001) and (AOR =55.091, 95% CI =6.88–441.19, p<0.001), respectively.
Conclusion: In the present study, the prevalence of anemia was lower than in previous studies conducted in various countries, including Ethiopia. More studies are needed regarding the importance of regular maternal care and health education promotion programs, which have the potential to play a more significant role in health care.
Keywords: hemoglobin, pregnancy, antenatal care, Aymiba, Ethiopia
Introduction
Anemia is defined as a decreased blood cell hemoglobin concentration. It is one of the most common nutritional deficiency diseases observed globally and affects more than 1.62 billion (25%) people of the world’s population, of which 56 million are pregnant women.1,2 Anemia is a major public health problem affecting all ages of the world’s population , its highest prevalence being among children aged <5 years and pregnant women.2
Anemia during pregnancy is considered severe when hemoglobin concentration is <7 g/dL, moderate when it is between 7 and 9.9 g/dL, and mild when it is 10–11 g/dL.3 Anemia during pregnancy is a major cause of morbidity and mortality of pregnant women in developing countries and has both maternal and fetal consequences.4 It is estimated that anemia causes >115,000 maternal and 591,000 perinatal deaths globally per year.3
In developing countries, the cause of anemia during pregnancy is multifactorial and includes nutritional deficiencies of iron, folate, and vitamin B12 and also parasitic diseases, such as malaria and intestinal parasitic infections. The relative contribution of each of these factors to anemia during pregnancy varies greatly by geographical location, season, and dietary practice.
In sub-Saharan Africa, iron and folate deficiencies are the most common causes of anemia in pregnant women.5
Anemia has a variety of contributing factors, including nutritional, genetic, and infectious disease factors; however, iron deficiency causes 75% of anemia cases.6 Iron deficiency anemia affects the development of a country by decreasing the cognitive development of children and the productivity of adults.7
Seventeen percent of Ethiopian women in the reproductive age group are anemic, and 22% of these women are currently pregnant.8 Despite its known effect on the population, very few data are available in this area.
The main aim of the present study was to assess the prevalence of anemia among pregnant women and identify its associated factors among those receiving antenatal care at Aymiba Health Center, northwest Ethiopia.
Methods and materials
Study design, area, and period
A cross-sectional study was conducted at Aymiba Health Center from January to March 2015. The study was conducted at Aymiba town, northwest Ethiopia, in Dembia District, North Gondar administrative zone, in the Amhara region. Aymiba is 17 km from Gondar town and 716 km north of Addis Ababa. The estimated total population of the district is about 263,000.
Study population
The study participants were pregnant women who visited Aymiba Health Center for antenatal care. Those who were pregnant and fulfilled the inclusion criteria were enrolled in the study. Each participant was recruited only once on their first visit during the study period.
Sample size and sampling procedures
A total of 206 pregnant women were enrolled in this study. Sample size was estimated using the general formula for single population proportion, with the following assumptions: anemia prevalence (P) of 16%,9 95% confidence level, and 5% marginal error.
This gave us a sample size of 206. All pregnant women who voluntarily agreed to participate in the study were included. Pregnant women receiving therapy for anemia or who were unable to respond to the questionnaire due to illness or unwilling to participate in the study were excluded.
Data collection
After obtaining informed written consent, history of sociodemographic, nutritional, obstetric and gynecological data, and clinical conditions were collected, followed by a physical exam. A hemoglobinometer (HemoCue HB 201+ analyzer, SETEMA Limited PLC, Ängelholm, Sweden) was used to determine the hemoglobin concentration from a capillary blood sample collected from the fingertip of each pregnant woman aseptically using a sterile single use disposable lancet. This was done by trained and experienced laboratory technicians. The necessary safeguards were applied during blood collection. A drop of blood was allowed to enter the optical window of the microcuvette through capillary action after discarding the first drop of blood. The microcuvette was then placed into the cuvette holder for photometric determination of the hemoglobin level.10
Stool specimens were collected in a clean and labeled container from the study participants. A portion of the stool was processed with a direct microscopic technique to detect intestinal parasites immediately. Two trained medical laboratory technologists examined the samples microscopically, first with a 10× and then with a 40× objective, for helminth eggs, larvae, and cysts of protozoan parasites.
Data processing
The data were entered, cleaned, and analyzed with the SPSS statistical software version 20 (IBM Corp., Armonk, NY, USA). Summary statistics such as frequencies and percentages were computed. Logistic regression was used to identify the factors associated with anemia. A 95% confidence interval (CI) and a p-value of <0.05 were considered statistically significant.
Ethical consideration
Ethical approval was obtained from the University of Gondar, School of Biomedical and Laboratory Sciences Ethical Clearance Committee, and a permission letter was obtained from the Aymiba Health Center administrator before going ahead with the study. The voluntary nature of participation and the right to withdraw at any time were emphasized, and written informed consent was obtained from every participant. Confidentiality was maintained throughout the collection and processing of the specimens, and each study participant was informed about the objective of the study. In addition to this, abnormal test results of the study subjects were shared with their physicians for further investigation and management.
Results
Sociodemographic characteristics
A total of 206 pregnant women participated in the study. More than 90% of the study participants were of Amhara ethnicity, and >60% were orthodox Christians by religion. The mean age of the study participants was 28.34±6.1 years, and 13.6% of the study participants were >35 years. Most of the study participants were educated up to the level of primary school (59.7%), about 92% of the participants were married, and about 38.8% were housewives by occupation (Table 1).
  | Table 1 Sociodemographic features of the study participants from January to March 2015 |
Obstetric and medical history
Among the study participants, 96 (46.6%) had had more than two deliveries previously. About 136 (66.0%) of the study participants had a birth interval of >18 months between the pregnancies, and 167 (81.9%) had a prior history of contraceptive use before becoming pregnant (Table 2). There was a past medical history of intestinal parasitosis in 20 (36.36%) of the study participants (Table 3). A total of 69 (33.5%) participants were in the third trimester, and 130 (63.5%) and 7 (3.4%) were in the second and first trimesters, respectively (Table 4).
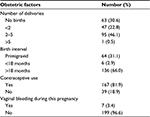  | Table 2 Obstetric factors of the study participants |
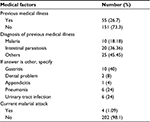  | Table 3 Medical factors of the study participants |
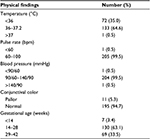  | Table 4 Physical findings of the study participants |
Dietary habits of study participants
The dietary habits and nutritional analysis showed that 174 (84.5%) of the study participants ate additional food during pregnancy (Table 5).
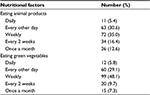  | Table 5 Nutritional habit of study participants |
Laboratory findings
A total of 52 (25.2%) participants had hemoglobin concentration levels of <11 g/dL, 16 (7.9%) had intestinal parasitic infections, and 5 (2.4%) were positive for HIV (Table 6).
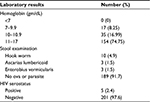  | Table 6 Laboratory results of study participants Abbreviation: HIV, human immunodeficiency virus. |
Association of sociodemographic factors and clinical conditions with anemia
Logistic regression analysis was carried out to assess the possible relationship between anemia and sociodemographic characteristics and clinical conditions. The results showed that it was significantly associated with rural residence (adjusted odds ratio [AOR] =9.17, 95% CI =2.15–40, p<0.001) and with intestinal parasitic infections (AOR =55.091, 95% CI =6.88–441.19, p<0.001) (Table 7).
  | Table 7 Logistic regression results of clinical findings of women receiving ANC Abbreviations: ANC, antenatal care; CI, confidence interval; HIV, human immunodeficiency virus. |
Discussion
Anemia in pregnancy is a common problem in most developing countries and a major cause of morbidity and mortality. It has a significant impact on the health of the fetus and of the mother. The present study was carried out to determine the prevalence and associated factors of anemia among women receiving ANC at Aymiba Health Center. The overall prevalence of anemia in this study was 25.2%, which was almost comparable to the results of studies conducted in Republic of Korea (30.2%),14 South Africa (19.7%),15 rural areas of Southern Ethiopia (29%),16 and Azezo (21.6%).18
The prevalence is considerably lower than that previously reported from India (84.9%),6 Nigeria (40.4%),11 Jimma town, southwest Ethiopia (41.9%),12 Peru (70.1%),17 and China (58.6%).19 The present study findings of anemia were also lower than that stated in Ethiopian demographic and health survey reports of 2005, namely, 30.6%.8 The findings of the present study were not in agreement with the World Health Organization 2005 report, which stated that the highest proportion of individuals affected by anemia were in Africa in both pregnant and nonpregnant women of childbearing age.20
The possible reason for the lower prevalence of anemia in the current study might be differences in the study area (geographical variation) and administration of iron supplements in health facilities, which is helpful in reducing anemia during pregnancy.
However, the present study showed a higher prevalence of anemia than a similar study that was done at Gondar University Hospital, which reported it to be 16.65%.9 The possible reason for the higher prevalence of anemia in the current study might be differences in monthly income.
In this study, the majority of anemic cases, 67.3% (35/52), were of the mild type (hemoglobin 10–10.9 g/dL), followed by cases of moderate anemia (7–9.9 g/dL) and 0% severe anemia (32.7%) (hemoglobin <7 g/dL). A similar report for Ethiopia stated 49% (41/83) of the cases were of mild anemia, 46% moderate anemia, and 5% severe anemia. A similar report for Pakistan stated that the majority of the cases were of mild anemia (75.0%) and a few of moderate anemia (14.8%) and severe anemia (0.7%).21 Similarly, a report from India in 2010 also showed that the majority (50.9%) had moderate anemia, with mild type of anemia accounting for 30.17% and severe anemia for 18.9%, respectively.22
In this study, no association between anemia and the number of children was observed.
This finding is supported by the findings of previous reports in Eastern Sudan, Nigeria, and Zaire23–25 and is contrary to a report from Tanzania.26
The incidence of anemia during pregnancy is expected to be higher as the number of pregnancies increases because of the repeated drain on the iron reserves. In fact, multiparity, especially when the pregnancies have occurred in a rapid sequence, is traditionally regarded as a cause of anemia in pregnancy. However, the present study showed no consistent relationship between increasing number of children and the incidence of anemia. Possibly, the experience gained from the first pregnancy followed by increased awareness and good dietary practices, as well as increased interaction with other pregnant women at the antenatal clinic, might counterbalance its effect. This study also did not observe any relationship between prevalence of anemia and increasing gestational age, suggesting that all pregnant women were susceptible to anemia throughout the gestational period. In order to avoid anemia during pregnancy, receiving early antenatal care would serve as an important preventive measure. The same result was observed in a study conducted in India and Gondar.9,18,27
In the present study, intestinal parasitic infections were found to be significantly associated with anemia in pregnant women (AOR =55.091, 95% CI =6.88–441.19, p<0.001), as were the findings of previous reports.9,18,26
This study showed a significant association between anemia and rural residence (AOR =9.17, 95% CI =2.15–40, p<0.001), which is consistent with previous reports.9,18,27
The present study showed no significant association between anemia and maternal age, housewives, monthly income, level of education; iron supplement but significant association was reported in previous studies); previous reports and the present study may be due to differences in monthly income and educational level.9,12,18,19,27
Conclusion
The overall prevalence of anemia was low in our study, and this might be a result of the ongoing strategy concerning primary health care in Ethiopia, which seems well planned and implemented. Intestinal parasitic infections, rural residence, and HIV infection were observed to be factors associated with maternal anemia. Governmental and nongovernmental health institutions should provide health education to pregnant women on prevention of infectious diseases such as intestinal parasitic infections. Health education, nutrition assessment, and iron supplementation are encouraged during antenatal care servicing, and the effectiveness of such interventions should be evaluated.
Limitation
The study did not classify anemia on the basis of red blood cell morphology, ie, as microcytic, macrocytic, normocytic, and Ferritin levels.
Acknowledgments
The author expresses his thanks the University of Gondar for funding this project. He also extends his special thanks and appreciation to the participants, who voluntarily participated in this study, as well as the Aymiba Health Center workers for their unstinted support, guidance, and material for the study.
Disclosure
The author reports no conflicts of interest in this work.
References
WHO/CDC. Worldwide Prevalence of Anemia 1993–2005: WHO Global Database on Anemia. Geneva, Switzerland: WHO Press; 2008. | ||
Balarajan Y, Ramakrishnan U, Ozaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet. 2011;378(9809):2123–2135. | ||
Salhan S, Tripathi V, Singh R, Gaikwad HS. Evaluation of hematological parameters in partial exchange and packed cell transfusion in treatment of severe anemia in pregnancy. Anemia. 2012;2012:608658. | ||
Akhtar M, Hassan I. Severe anemia during late pregnancy. Case Report Obstet Gynecol. 2012;2012:3. | ||
Baker SJ, DeMaeyer EM. Nutritional anemia: its understanding and control with special reference to the work of the world health organization. Am J Clin Nutr. 1979;32(2):368–417. | ||
Toteja GS, Singh P, Dhillon BS, et al. Prevalence of anemia among pregnant women and adolescent girls in 16 districts of India. Food Nutr Bull. 2006;27(4):311–315. | ||
Vivek RG, Halappanavar AB, Vivek PR, Halki SB, Maled VS, Deshpande PS. Prevalence of anemia and its epidemiological. Deter Pregnant Women. 2012;5(3):216–223. | ||
Central Statistics Agency. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia: Central Statistics Agency; 2011. | ||
Mulgeta M, Zelalem A, Meseret A, Bamlaku E. Prevalence and predictors of maternal anemia during pregnancy in Gondar, north west Ethiopia. Hindawi Publish Corp. 2013;2014:2–3. | ||
Cheesbrough M. District Laboratory Practice in Tropical Countries Part 2. 2nd ed. New York, NY: Cambridge University Press; 2006. | ||
Dim CC, Onah HE. The prevalence of anemia among pregnant women looking in Enngu south eastern Nigeria. MedGenMed. 2007;9(3):11. | ||
Desalegn S. Prevalence of anemia in pregnant women in Jimma town, southwestern Ethiopia. Ethiop Med J. 1993;31(4):251–258. | ||
Obse N, Mossie A, Gobena T. Magnitude of anemia and associated risk factors among pregnant women attending antenatal care in Shalla Woreda, West Arsi Zone, Oromia Region, Ethiopia. Ethiop J Health Sci. 2013;23(2):165–173. | ||
Van Bogart LJ. Anemia and pregnancy outcomes in a South African rural population. J Obstet Gynecol. 2006;26 (7):617–619. | ||
Mart´i-Carvajal A, Peña-Martí G, Comunian G, Muñoz S. Prevalence of anemia during pregnancy: results of Valencia (Venezuela) anemia during pregnancy study. Arch Latinoam Nutr. 2002;52(1):5– 11. | ||
Jamal HA, Rebecca PS. Iron deficiency anemia is not a rare problem among women of reproductive ages in Ethiopia. BMC Blood Disord. 2009;9:7. | ||
Becerra C, Gonzales GF, Villena A, de la Cruz D, Flori A. Prevalence of anemia in pregnant women, Pucallpa Regional Hospital, Peru. Rev Panam Salud Publica. 1998;3(5):285–292. | ||
Alem M, Enawgaw B, Gelaw A, Kena T, Seid M, Olkeba Y. Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Azezo Health Center Gondar town, Northwest Ethiopia. J Interdiscipl Histopathol. 2013;1(3):137–144. | ||
Ma AG, Schouten E, Wang Y, et al. Anemia prevalence among pregnant women and birth weight in five areas in China. Med Princ Pract. 2009;18:368–372. | ||
Jin L, Yeung LF, Cogswell ME, et al. Prevalence of anaemia among pregnant women in South-East China, 1993–2005. Public Health Nutr. 2010;13(10):1511–1518. | ||
Baig-Ansari N, Badruddin SH, Karmaliani R, et al. Anemia prevalence and risk factors in pregnant women in an urban area of Pakistan. Food Nutr Bull. 2008;29:132–139. | ||
Vijaynath, Jitendra, Ramesh P, Abhishek P. Prevalence of anemia in pregnancy. Indian J Appl Basic Med Sci. 2010;12:23–35. | ||
Adam I, Khamis AH, Elbashir MI. Prevalence and risk factors for anemia in pregnant women of Eastern Sudan. Trans R Soc Trop Med Hyg. 2005;99:739–743. | ||
Iloabachie GC, Meniru GI. The increasing incidence of anemia in pregnancy in Nigeria. Orient J Med. 1990;2:194–197. | ||
Jackson DJ, Klee EB, Green SD, Mokili JL, Elton RA, Cutting WA. Severe anemia in pregnancy: a problem of primigravidae in rural Zaire. Trans R Soc Trop Med Hyg. 1991;85:829. | ||
Hinderaker SG, Olsen BE, Bergsjo P, Lie RT, Gasheka P, Kvåle G. Anemia in pregnancy in the highlands of Tanzania. Acta Obstet Gynecol. 2001;80:18–26. | ||
Levy A, Fraser D, Katz M, Mazor M, Sheiner E. Maternal anemia during pregnancy is an independent risk factor for low birth weight and preterm delivery. Eur J Obstet Gynecol Reprod Biol. 2005;122:182–186. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
