Back to Journals » Clinical Interventions in Aging » Volume 13
Prevalence and treatment of hip and knee osteoarthritis in people aged 60 years or older in Germany: an analysis based on health insurance claims data
Authors Postler A, Luque Ramos A , Goronzy J , Günther K-P, Lange T , Schmitt J, Zink A, Hoffmann F
Received 20 May 2018
Accepted for publication 20 September 2018
Published 14 November 2018 Volume 2018:13 Pages 2339—2349
DOI https://doi.org/10.2147/CIA.S174741
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Anne Postler,1 Andres Luque Ramos,2 Jens Goronzy,1 Klaus-Peter Günther,1 Toni Lange,3 Jochen Schmitt,3 Angela Zink,4 Falk Hoffmann2
1University Center of Orthopaedics and Traumatology, University Medicine Carl Gustav Carus Dresden, Technische Universität Dresden, Dresden, Germany; 2Department of Health Services Research, Carl von Ossietzky University, Oldenburg, Germany; 3Center for Evidence Based Healthcare, Medical Faculty, Technische Universität Dresden, Dresden, Germany; 4Epidemiology Unit, German Rheumatism Research Centre, Berlin, Germany
Objective: Osteoarthritis (OA) is highly prevalent throughout the world, especially in the elderly population, and is strongly associated with patients’ frailty. However, little is known about the prevalence and treatment of OA in elderly patients in routine clinical care in Germany.
Materials and methods: As a part of Linking Patient-Reported Outcomes with CLAIms Data for Health Services Research in Rheumatology (PROCLAIR), a cross-sectional study using claims data from a large Germany statutory health insurance (BARMER) was conducted. We included people aged 60 years or older and assessed the prevalence of OA of the hip or knee, defined as having outpatient diagnoses (ICD: M16 or M17) in at least two quarters of 2014. The use of conservative treatment, including analgesics and physical therapy, and total joint replacement was studied. Analyses were stratified by age, sex, comorbidities, and level of care dependency defined by social law.
Results: A total of 595,754 patients (mean age: 74.9 years; 69.8% female) were diagnosed with OA (21.8%), with the highest prevalence in those between 80 and 89 years (31.0%) and in females compared to males (23.9% vs 18.3%). Prevalence decreased with increasing level of care dependency from 30.5% in patients with a low level (0/1) to 18.7% in the highest level of care dependency. A total of 63.4% of the patients with OA received analgesics, with higher use with increasing age. Physical therapy was prescribed to 43.1% of the patients, but use decreased with age. In all, 5.3% of the patients received total joint replacement in 2014.
Conclusion: The lower frequency of coded OA with increasing level of care dependency may reflect underdiagnosis, and patients with many other medical problems seem to be at risk for inadequate recognition and treatment of their OA.
Keywords: osteoarthritis, total joint replacement, health services research, aged, analgesics, frail elderly
Introduction
The proportion of older people is constantly increasing in most industrialized countries. For instance, while 21% of the German population were 65 years or older in 2013, it is expected that at least every third person will be older than 65 years by 2060 and there will be twice as many people aged 70 or older as there are births in Germany.1–3
Osteoarthritis (OA) is the most prevalent chronic joint disease in the world, and half of the world’s population aged 65 or older suffers from some form of OA. It is one of the most common sources of pain and disability in the elderly,4–6 and international reports on the prevalence of OA diagnoses show an increasing number of patients with this disease.7–10 There are recommendations for the nonsurgical treatment of hip and knee OA in comprehensive patient care.11–15 Failed conservative therapy, pain, loss of function, and radiological changes are considered in the decision to perform total hip replacement (THR) or total knee replacement (TKR) surgeries,12,13,16–20 which are effective and cost-effective procedures for people with severe unresponsiveness to OA conservative therapy,21,22 also recommended in German guidelines.23,24
Clinical OA is strongly associated with frailty and pre-frailty in older adults, for whom preventive and therapeutic measures can be taken, especially if early detection of patients’ frailty and the promotion of physical exercise have been initiated.25 Higher risks in the elderly undergoing surgery are well known. These patients have higher mortality rates and increased length of hospital stay.26
However, little is known about elderly patients with OA in Germany and their specific treatment. A previous claims data-based study reported significant regional differences in hip and knee OA, as well as THR and TKR rates in Germany, but the findings were not analyzed with regard to different age groups.27 Further international studies reported about age-specific prevalence estimates for OA28–30 and described patterns of care received, comorbidities, and treatment but did not include physical therapy.31
The purpose of this study was to examine the prevalence of OA in older patients in Germany and to assess how they are currently treated, depending on age, sex, type of OA, comorbidities, and level of care dependency.
Materials and methods
Database and study population
This study is part of the “Linking Patient Reported Outcomes with CLAIms Data for Health Service Research in rheumatology” (PROCLAIR) project, investigating the health care situation in patients with inflammatory rheumatic disorders (rheumatoid arthritis, ankylosing spondylitis) or OA of the hip or knee.
A cross-sectional study using de-identified claims data from a health insurance fund (BARMER) for the year 2014 was performed. The BARMER is one of the largest statutory health insurance funds covering ~11% of the German population all over the country. The distribution of socioeconomic status indicators and the prevalence of joint disorders in the BARMER are comparable to the whole German population.32 In Germany, a total of 70.7 million people (~87% of the population) was covered by one of the 131 statutory health insurance funds in 2014. These funds do not differ with regard to their benefits, and members have free choice of providers. Additional information on the German health care and long-term care system also in comparison to that of other countries can be found in Busse and Blümel.33
We included people aged 60 years or older who were insured on at least one day in each of the four quarters of the year 2014 in the BARMER. This criterion ensures that a large majority of people included were continuously insured, even though people who died during the last quarter were also included.
We identified patients with outpatient diagnoses of OA of the hip or knee, according to the ICD-10 (M16 or M17) in at least two quarters of 2014. In Germany, physicians working in outpatient care have to document all diagnoses once per quarter, making no exact date of diagnosis available. Besides analyses on the prevalence of hip/knee OA, all patients were also assigned to one of the three groups: OA of the hip only (only ICD-10 codes of M16), OA of the knee only (only ICD-10 codes of M17), or OA of both hip and knee (ICD-10 codes of M16 and M17).
Comorbidities
We used two measures of comorbidity: 1) levels of care dependency and 2) the Elixhauser index. Levels of care dependency were obtained from the German Long-Term Care Insurance (Gesetzliche Pflegeversicherung). Services are provided to those who require support for the activities of daily living, irrespective of whether they are community dwelling or living in a nursing home. In Germany, in 2014, there were three levels of care dependency. People in care level 1 (considerable need of care) required care at least once a day, and those in care level 2 (severe need of care) required basic care at least three times a day at different times and assistance in caring for their households a number of times a week. People in care level 3 (in extreme need for care) required assistance for basic care 24 hours a day, 7 days a week, and household help a number of times per week. People whose competence in coping with everyday life is considerably impaired (mostly people with dementia) can apply for benefits, even if they do not fulfill the eligibility criteria of care level 1 and are considered to be of care level 0. The highest level of care dependency for each patient in 2014 was incorporated in our analyses.
Furthermore, we used the Elixhauser index, which was developed for studies using large administrative databases34 and includes 31 severe diseases, but neither OA of the hip (M16) nor OA of the knee (M17). Although the Elixhauser index was originally created using ICD-9 codes, an adaptation for ICD-10 data has been developed by Quan et al35 and was used in our study. Comorbidities from the Elixhauser index were prevalent if there was a corresponding ICD-10 code in outpatient care in at least one quarter of 2014.
Treatment
We assessed the following treatment options, which are all covered by the statutory insurance: conservative treatment, including filled prescriptions of 1) analgesics; 2) non-pharmacological, physical therapy; and 3) actually performed surgical treatment as joint replacement. We identified outpatient prescriptions for analgesics according to the WHO’s pain ladder for a stepwise approach to pain management. These include nonsteroidal anti-inflammatory drugs (NSAIDs), coxibs, and metamizol (WHO step 1) and weak (tramadol, tilidine/naloxone, and codeine combinations; WHO step 2) to strong opioids (such as morphine, oxycodone, hydromorphone, fentanyl, and buprenorphine; WHO step 3). These were classified based on a previously used reference list of anatomical therapeutic chemical (ATC) codes.36,37 Physical therapy was assessed for different prescribed treatment modalities, including physiotherapy, massage therapy, exercise therapy, and electrotherapy. We also recorded total joint replacement procedures for the hip and knee for patients with diagnosed OA, irrespective of indication for surgery.
Statistical methods
First, we calculated the prevalence of hip/knee OA and three subtypes (OA of hip only, OA of knee only, and OA of hip and knee together). These analyses were further stratified by age (60–69, 70–79, 80–89, 90–99, and 100+ years), sex (male and female), levels of care dependency (four categories), the most frequent comorbidities of the Elixhauser index, and the numbers of comorbidities (0–1, 2–4, 5–7, and 8+).
In order to determine specific treatment modalities, we calculated the proportion of patients with at least one prescription for an analgesic or physical therapy and the proportion of patients who had undergone surgical treatment. Prevalences were also estimated with 95% CIs. Predictors for those who received joint replacement were examined by a multivariable logistic regression, adjusting for age, sex, and number of comorbidities using the same categories as described earlier. ORs with 95% CIs were also estimated.
We performed all statistical analyses with SAS for Windows version 9.2 and 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics statement
An ethics approval for the PROCLAIR study was obtained from the ethics committee of the Charité University Medicine, Berlin, in 2015 (EA1/051/15).
Results
Baseline characteristics
In 2014, of 7.2 million insured adults and of 2.7 million insured people of >60 years of age, a total of 595,754 patients were diagnosed with hip/knee OA in at least two quarterly periods. The mean age of those with hip/knee OA was 74.9 years, and 69.8% were female. In 87.7% of all patients with OA, no level of care dependency was found. A total of 49.0% of all OA patients had two to four comorbidities on the Elixhauser index and 25.8% had five to seven. The most frequent comorbidities were arterial hypertension (78.7% of all patients), diabetes mellitus (29.0% of all patients), depression (27.9% of all patients), and cardiac arrhythmias (26.5% of all patients).
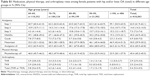
Prevalence of hip/knee OA
The total prevalence of hip/knee OA was 21.8% (n=595,754). As shown in Table 1, females were more often affected than males (23.9% vs 18.3%) The highest prevalence of OA was found in people aged 80–89 years (31.0%) and in those aged 90–99 years (28.9%). After an age of 99 years, the OA prevalence decreased. The prevalence of OA decreased with increasing level of care dependency from 30.5% in patients with a low level (0/1) to 18.7% in patients with the highest level of care dependency. A higher number of comorbidities was associated with a higher prevalence of OA, and this was also found in all subgroups of OA. For instance, patients with eight or more comorbidities had a threefold increased prevalence of OA compared to those with 0–1 comorbidities (37.0% and 12.3%). When having a look at the different comorbidities included in the Elixhauser index, with the exception of obesity (34.5%), the prevalence of OA ranged between 25.3% and 30.7% in patients with the most common comorbidities (data not shown).
  | Table 1 Prevalence of hip and/or knee OA stratified by age, sex, level of care, and comorbidities |
Overall, OA of the hip was documented in 6.2% of patients, 12.1% had OA of the knee, and 3.5% had OA of both hip and knee (Table 1). Differences between age groups, sex, levels of care, and the number of comorbidities were also found in all subgroups of OA. The only difference was found when considering comorbidities of the Elixhauser index separately. The prevalence of knee OA was increased in obese patients (20.5%) when compared to that of other comorbidities (14.0%–16.4%). However, the prevalence of hip OA did not differ in patients with obesity (7.3%) compared to that of other comorbidities (7.0%–8.5%).
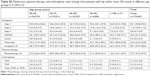
Use of medications
Because there were no differences in patterns of treatment between subgroups of OA, we present treatment patterns only in all patients with hip/knee OA.
Overall, 63.4% (95% CI: 63.3%–63.5%) of these patients had received prescriptions for analgesics and 44.1% for NSAIDs (Table 2). The prescription of step 1 drugs, on the WHO’s pain ladder, was largely the same in all age groups. The application of NSAIDs, however, decreased with age (48.1% aged 60–69 years received NSAIDs compared to 20.1% aged 100 years or older), while metamizol was increasingly prescribed with age (21.0% and 47.4% in people aged 60–69 and 100+ years, respectively). Prescriptions of strong opioids (WHO step 3) also increased in later decades of life, and the most frequent application of opioids was recorded in the groups of 90 years or older.
A larger percentage of females than males had claims for analgesics (65.6% and 58.1%), except for the latest decade where we found no differences. Females received prescriptions for strong opioids more often, whereas prescriptions for NSAIDs were quite comparable between female and male patients.
Physical therapy
Physical therapy was prescribed less frequently than analgesics for 43.1% (male: 37.7%, female: 45.4%) of all OA patients (Table 2). With increasing age, this proportion decreased from 45.4% in patients aged 70–79 years to 23.2% in those aged at least 100 years; in particular, this trend was more pronounced in female patients (refer Supplementary materials and Tables 1 and 2).
Total joint replacement
In total, 5.3% of all patients had actually undergone a total hip or knee replacement procedure within the year 2014. THR was performed in 6.4% of patients with OA of the hip only, and TKR was performed in 3.5% of patients with OA of the knee only (data not shown). In all groups, the implantation was performed most frequently at age 60–69 years, as well as at age 70–79 years, (5.6% and 6.0%) with decreasing numbers of patients in the older age groups in both female and male patients (Tables 2, S1, and S2). Overall surgery was more often performed in females.
Compared to patients aged 100 years or older, OA patients of 70–79 years had the highest likelihood of receiving THR or TKR (OR 6.00; 95% CI: 2.69–13.42). Further factors that increased the likelihood of surgery were a low number of comorbidities (maximum of 1 compared to more than 8; OR 1.39; 95% CI: 1.32–1.46) and being female (OR 1.12; 95% CI: 1.10–1.15) (Table 3).
  | Table 3 Results of a multivariable logistic regression on factors associated with total joint replacement (hip or knee) |
Discussion
In this cross-sectional study using data of a large German health insurance, we found an increasing prevalence of hip/knee OA with age up to 89 years and a higher prevalence in females. Prevalence decreased with increasing level of care dependency. Analgesics were more often prescribed than physical therapy, and different age trends were found.
Several large population-based surveys showed an increasing OA prevalence with age.38–41 In contrast to other studies, in our study, the prevalence of OA decreased after the age of 89 years. We assume that this is due to the fact that claims data reflect health care utilization, which may decrease with a higher age and restricted mobility. The association of OA with sex has been inconsistent.38 While knee OA is more prevalent in women in most studies,39,41,42 hip OA may be equally distributed or even more prevalent in men.39,40 However, different estimates may also be attributed to the inclusion criteria of studies and may depend on clinical or radiographic definition. In two recent studies, the clinical prevalence of OA was higher in women, while radiographic OA was more prevalent in men.39,42
In our study, the prevalence of OA increased with the number of comorbidities. Most elderly patients suffered from several comorbidities in addition to OA, and at least two further comorbidities were coded in 83.7% of cases. Obesity was found in about one-fifth of the cohort, and the prevalence of OA was highest among these patients. Obesity is known as a modifiable risk factor for OA43 and for functional limitation as well.44 Patients with knee OA show a significantly higher prevalence of obesity when compared with patients who suffer from hip OA. Although a dose–response relationship between BMI and risk of hip OA exists,45 obesity seems to be a more important risk factor for the development of knee OA.43,46 Diabetes, which is another important risk factor for the development of OA,47 was the second most recorded comorbidity, but the prevalence of OA was only slightly elevated in these patients.
We observed an inverse relation between the level of care dependency and OA prevalence. This is not explained by different patterns according to age, sex, or Elixhauser comorbidities (data not shown). An explanation could be that in cases of multiple painful disorders and extensive care needs, overlapping musculoskeletal symptoms are underdiagnosed, as they no longer have priority.48 Although pain and disruption of activities appear to stimulate the patient to seek medical consultation, negative attitudes regarding OA (from either the patient or general practitioner) appear to be a disincentive to consultation.49 Turkiewicz et al42 found that one in three patients with OA symptoms do not consult a physician. It is known that older patients often do not disclose their pain or consider pain as being a part of aging50 or that pain is caused in the context of mobility, which decreases the awareness of OA in bedridden patients. Additionally, misconceptions, poor communication, and cognitive barriers may result in underrecognition of pain in chronic diseases in elderly patients.51
Multiple guidelines for OA generally agree that adequate treatment requires a combination of non-pharmacological and pharmacological modalities.12,13,16,52 Therapeutic recommendations, however, often do not consider specific requirements in different age groups. Regarding this context, it is of special interest that 63.4% of the included patients received analgesics and women and patients with a higher number of comorbidities had a greater likelihood of being prescribed analgesic drugs. Age is also of interest as opioids are more frequently prescribed with increasing age, which may be attributed to a higher degree of comorbidities. In general, patients with more comorbidities use more medications and more often receive prescriptions for analgesics.44 The finding that the usage of drug prescription increased with age has to be critically discussed because of adverse reactions, especially in elderly patients.53,54
It is well known that regular moderate-level exercise does not exacerbate OA pain or accelerate the pathological process of OA but rather reduces pain and morbidity.55 Nevertheless, prescription of physiotherapy was recorded in less than half of all patients, and we do not know the reasons for that. It may be due to insufficient awareness of OA in older, multimorbid patients, leading to undertreatment. In addition, a contributing factor may lie in the health care system itself where nondrug therapies, in particular physical therapy, could be prescribed initially at low levels.
Total joint replacement was performed in 5.3% of all patients with OA in 2014. While the prevalence of knee OA was higher than the prevalence of hip OA in our cohort (12.1% vs 6.2%), the frequency of knee replacement was lower. As the large majority of THR is performed because of OA (80.1%) and only a small portion (12.5%) because of fractures,56 this can be interpreted as different therapeutic approaches. Knee OA may be easier to treat by noninterventional procedures, and in an earlier investigation from the Ulm OA study, we have seen that time to surgery is longer in knee patients when compared to that in hip patients.56 Another reason may be that patients after THR are more satisfied compared to patients after TKR.57 These factors can influence the decision of primary care physicians regarding referral to surgery.
We observed a significant association between total joint replacement and patient age, as well as number of comorbidities. The older the patients and the more comorbidities they have, the less frequently total joint replacement was performed. This is probably due to the well-known increase in complication rates, longer length of stay, and higher readmission rates in patients with higher numbers of comorbidities58,59 and may be another disincentive for referring physicians, as well as surgeons, to perform operative treatment in older patients. However, in a study from the Swedish Arthroplasty Register, it is known that comorbidities do not influence quality of 1 year postoperatively60 and tell rather lite about mortality.61 About the same patients, it is known that their life expectancy was slightly higher than in general population, possibly due to preoperative patient selection.62
On the other hand, elderly patients themselves often have concerns regarding recommended surgical procedures. In 2008, Hudak et al63 asked 886 patients of 60 years of age or older and found that 84% of them had concerns about the surgery, including concerns about the anticipated quality of life as a result of surgery, the care facility after surgery, the timing of the surgery, and the patient’s capacity to meet the demands of the surgery, including those related to the recovery period.
Strengths and limitations
Field studies in elderly people often face specific challenges, eg, a high number of institutionalized or cognitive impaired people who tend not to participate. This problem of selective nonresponse does not arise when claims data are used, which include all insured people, independent of their current health state. The large database enabled us to compare the prevalences of ICD-10-coded knee and hip OA or both according to sex, age, level of care dependency, and region of residents. We were also able to assess a large set of treatment options.
However, we do not have further health-related and clinical information (eg, functional or cognitive status or data on pain level). It remains unclear whether all patients with clinically relevant OA could be detected, in particular in the elderly. Diagnoses in claims data rely on the coding by the treating physician, which do not always match accepted diagnostic criteria. There are no studies on the validity of OA diagnoses from Germany, and findings from other countries might not be transferable. According to the definition of Shrestha et al,64 our algorithms requiring outpatient diagnoses of OA in at least two quarters in 1 year would be classified as restrictive. However, as the number of outpatient visits is comparably large in Germany,33 we believe that our algorithm leads to a suitable balance between specificity and sensitivity. Furthermore, the prevalence might be underestimated because people solely having diagnoses of polyarthritis (ICD-10: M15) were not included in our algorithm, However, our main goal was to compare groups with hip, knee, and hip/knee OA, and in patients having only diagnoses of polyarthritis, it is unclear which joints are affected. However, we did not exclude people with polyarthritis, and indeed, 12% of our patients with hip/knee OA also had diagnoses of polyarthritis. In addition, we cannot distinguish whether medication and physical therapy are prescribed solely for the OA or also for other conditions. In German claims data, there is no direct link between diagnoses and specific treatments in outpatient care. In particular in older patients with many comorbidities, OA may not be the major reason why patients consulted a physician, and therefore, the true burden of OA may be underestimated. Furthermore, since the cross-sectional data cover 1 year only, patients who did not have treatment for their OA may have received treatment the previous years. This is plausible given the fact that OA often has an intermittent course of disease with changing treatment needs. We included only people who died during the last quarter and did not consider those who died in the first three quarters and possibly had less treatment. In addition, we wanted to investigate approximately the same insurance period.
Conclusion
Not all elderly German patients seem to receive conservative treatment for their OA according to available guidelines, although the prevalence of OA in elderly patients is high and is associated with a high burden of comorbid conditions.
It is crucial to recognize the reasons for pain in patients with OA and to apply an appropriate therapy, especially in the presence of several comorbidities and increasing levels of care dependency. Pain medication as well as physical therapy and surgical strategies should be adapted to the type of musculoskeletal impairment, as well as the general health status of the patient.
Acknowledgments
We thank the BARMER health insurance for the opportunity to use the data for these analyses. The study was sponsored by the Federal Ministry of Education and Research, Germany (01EC1405). The funding sources had no role in study design, data collection, analysis, interpretation, writing, or submission of the manuscript.
Author contributions
AP, ALR, JG, K-PG, TL, JS, AZ, and FH have been involved in planning and the execution and AP, ALR, and FH in the analysis of this study. AP and FH have written the draft, and all authors have corrected the manuscript. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
K-PG has received research grants from Zimmer, Link, and Aesculap but outside the submitted work. JS has received institutional funding of investigator-initiated research from Novartis, ALK, Sanofi, Pfizer, Wyeth, and MSD. The other authors have no commercial association that might pose a conflict of interest in connection with the submitted article.
References
Bundesamt S. Bevölkerung Deutschlands bis 2060. 13. koordinierte Bevölkerungsvorausberechnung. 2015. | ||
Sädbud L. Demografischer Wandel in Deutschland. Auswirkungen auf Krankenhausbehandlungen und Pflegebedürftige im Bund und in den Ländern [Countries SÄdBud. Demographic change in Germany. Effects on hospital treatment and people in need of care in the federal and state governments. Of 2010]. 2010. German. | ||
Sädbud L. Die Generation 65+. Statement des Präsidenten des Statistischen Bundesamtes Roderich Egeler [The generation 65+. Statement of the President of the Statistical Federal Office Roderich Egeler]. 2015. German. | ||
Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006;20(1):3–25. | ||
Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41(5):778–799. | ||
Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. | ||
Allen KD, Golightly YM. State of the evidence. Curr Opin Rheumatol. 2015;27(3):276–283. | ||
Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115–2126. | ||
Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355–369. | ||
Pilz V, Hanstein T, Skripitz R. Projections of primary hip arthroplasty in Germany until 2040. Acta Orthop. 2018;89(3):308–313. | ||
Chang J, McGrory BJ, Rana A, et al. Current orthopaedic surgeon practices for nonarthroplasty treatment of osteoarthritis of adult hip and knee. J Surg Orthop Adv. 2015;24(4):213–220. | ||
National Institute for Health and Care Excellence. Osteoarthritis: care and management Clinical guideline; 2014. In: 2014 National Institute for Health and Care Excellence (UK), London. | ||
Mcalindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–388. | ||
Fernandes L, Hagen KB, Bijlsma JW, et al; European League Against Rheumatism (EULAR). EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125–1135. | ||
National Clinical Guideline Centre (UK). National Institute for Health and Clinical Excellence: Guidance. Osteoarthritis: Care and Management in Adults. London: National Institute for Health and Care Excellence (UK); 2014 Feb. | ||
Gademan MG, Hofstede SN, Vliet Vlieland TP, Nelissen RG, Marang-van de Mheen PJ. Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview. BMC Musculoskelet Disord. 2016;17(1):463. | ||
Gossec L, Hawker G, Davis AM, et al. OMERACT/OARSI initiative to define states of severity and indication for joint replacement in hip and knee osteoarthritis. J Rheumatol. 2007;34(6):1432–1435. | ||
Gossec L, Paternotte S, Bingham CO 3rd, et al; OARSI-OMERACT Task Force Total Articular Replacement as Outcome Measure in OA. OARSI/OMERACT initiative to define states of severity and indication for joint replacement in hip and knee osteoarthritis. An OMERACT 10 Special Interest Group. J Rheumatol. 2011;38(8):1765–1769. | ||
Zhang W, Doherty M, Arden N, et al; EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). EULAR evidence based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2005;64(5):669–681. | ||
Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18(4):476–499. | ||
Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508–1519. | ||
Räsänen P, Paavolainen P, Sintonen H, et al. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop. 2007;78(1):108–115. | ||
Lützner J, Lange T, Schmitt J, et al. The S2k guideline: S2k-Leitlinie: Indikation Knieendoprothese Evidenz- und konsensbasierte Indikationsstellung in der Knie-Endoprothetik (EKIT-Knie) [Indications for knee endoprosthesis: Evidence and consent-based indications for total knee arthroplasty]. Orthopade. 2018;47(9):777–781. German. | ||
Schmitt J, Lange T, Günther KP, et al. Indication Criteria for Total Knee Arthroplasty in Patients with Osteoarthritis – A Multi-perspective Consensus Study. Z Orthop Unfall. 2017;155(5):539–548. | ||
Castell MV, van der Pas S, Otero A, et al. Osteoarthritis and frailty in elderly individuals across six European countries: results from the European Project on OSteoArthritis (EPOSA). BMC Musculoskelet Disord. 2015;16:359. | ||
Kuperman EF, Schweizer M, Joy P, Gu X, Fang MM. The effects of advanced age on primary total knee arthroplasty: a meta-analysis and systematic review. BMC Geriatr. 2016;16:41. | ||
Schäfer T, Pritzkuleit R, Jeszenszky C, et al. Trends and geographical variation of primary hip and knee joint replacement in Germany. Osteoarthritis Cartilage. 2013;21(2):279–288. | ||
Harrold LR, Yood RA, Andrade SE, et al. Evaluating the predictive value of osteoarthritis diagnoses in an administrative database. Arthritis Rheum. 2000;43(8):1881–1885. | ||
Jordan K, Clarke AM, Symmons DP, et al. Measuring disease prevalence: a comparison of musculoskeletal disease using four general practice consultation databases. Br J Gen Pract. 2007;57(534):7–14. | ||
Kopec JA, Rahman MM, Berthelot JM, et al. Descriptive epidemiology of osteoarthritis in British Columbia, Canada. J Rheumatol. 2007;34(2):386–393. | ||
Birtwhistle R, Morkem R, Peat G, et al. Prevalence and management of osteoarthritis in primary care: an epidemiologic cohort study from the Canadian Primary Care Sentinel Surveillance Network. CMAJ Open. 2015;3(3):E270–E275. | ||
Luque Ramos A, Hoffmann F. [Differences in chronic back pain and joint disorders among health insurance funds: Results of a cross-sectional study based on the data of the Socioeconomic Panel from 2013]. Z Rheumatol. 2017;76(3):238–244. | ||
Busse R, Blümel M. Germany: Health system review. Health Syst Transit. 2014;16(2):1–296, xxi. | ||
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. | ||
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. | ||
Hoffmann F, Schmiemann G. Pain medication in German nursing homes: a whole lot of metamizole. Pharmacoepidemiol Drug Saf. 2016;25(6):646–651. | ||
Schulze J, Freitag MH, Glaeske G, Schmiemann G, Hoffmann F. Schmerzmittelversorgung von Pflegeheimbewohnern mit und ohne Krebserkrankung Am häufigsten mit Metamizol [Pain medication in nursing home residents with and without cancer. Most frequently with metamizole]. Schmerz. 2015;29(3):276–284. German. | ||
Felson DT. Epidemiology of hip and knee osteoarthritis. Epidemiol Rev. 1988;10:1–28. | ||
Kim C, Linsenmeyer KD, Vlad SC, et al. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis Rheumatol. 2014;66(11):3013–3017. | ||
Lawrence RC, Felson DT, Helmick CG, et al; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. | ||
Laxafoss E, Jacobsen S, Gosvig KK, Sonne-Holm S. Case definitions of knee osteoarthritis in 4,151 unselected subjects: relevance for epidemiological studies: the Copenhagen Osteoarthritis Study. Skeletal Radiol. 2010;39(9):859–866. | ||
Turkiewicz A, Gerhardsson de Verdier M, Engström G, et al. Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology (Oxford). 2015;54(5):827–835. | ||
Stürmer T, Günther KP, Brenner H. Obesity, overweight and patterns of osteoarthritis: the Ulm Osteoarthritis Study. J Clin Epidemiol. 2000;53(3):307–313. | ||
Bindawas SM. Relationship between frequent knee pain, obesity, and gait speed in older adults: data from the Osteoarthritis Initiative. Clin Interv Aging. 2016;11:237–244. | ||
Jiang L, Rong J, Wang Y, et al. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2011;78(2):150–155. | ||
Reyes C, Leyland KM, Peat G, Cooper C, Arden NK, Prieto-Alhambra D. Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: a population-based cohort study. Arthritis Rheumatol. 2016;68(8):1869–1875. | ||
King KB, Rosenthal AK. The adverse effects of diabetes on osteoarthritis: update on clinical evidence and molecular mechanisms. Osteoarthritis Cartilage. 2015;23(6):841–850. | ||
Hoffmann F, van den Bussche H, Wiese B, Glaeske G, Kaduszkiewicz H. Diagnoses indicating pain and analgesic drug prescription in patients with dementia: a comparison to age- and sex-matched controls. BMC Geriatr. 2014;14:20. | ||
Paskins Z, Sanders T, Hassell AB. What influences patients with osteoarthritis to consult their GP about their symptoms? A narrative review. BMC Fam Pract. 2013;14:195. | ||
Schreier MM, Stering U, Pitzer S, Iglseder B, Osterbrink J. Pain and pain-assessment in nursing homes: Results of the OSiA study. Schmerz. 2015;29(2):203–210. | ||
Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med. 2001;17(3):457–478, vi. | ||
Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4):465–474. | ||
Hoffmann F, Meinecke P, Freitag MH, Glaeske G, Schulze J, Schmiemann G. Who gets dipyrone (metamizole) in Germany? Prescribing by age, sex and region. J Clin Pharm Ther. 2015;40(3):285–288. | ||
Garbe E, Jobski K. Utilisation of transdermal fentanyl in Germany from 2004 to 2006. Pharmacoepidemiol Drug Saf. 2012;21(8):904–905. | ||
American Geriatrics Society Panel on E, Osteoarthritis. Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J Am Geriatr Soc. 2001;49(6):808–823. | ||
Günther KP, Stürmer T, Sauerland S, et al. Prevalence of generalised osteoarthritis in patients with advanced hip and knee osteoarthritis: the Ulm Osteoarthritis Study. Ann Rheum Dis. 1998;57(12):717–723. | ||
Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K. Comparing patient outcomes after THA and TKA: is there a difference? Clin Orthop Relat Res. 2010;468(2):542–546. | ||
Tay KS, Cher EWL, Zhang K, Tan SB, Howe TS, Koh JSB. Comorbidities Have a Greater Impact Than Age Alone in the Outcomes of Octogenarian Total Knee Arthroplasty. J Arthroplasty. 2017;32(11):3373–3378. | ||
Schwartz FH, Lange J. Factors that affect outcome following total joint arthroplasty: a review of the recent literature. Curr Rev Musculoskelet Med. 2017;10(3):346–355. | ||
Greene ME, Rolfson O, Gordon M, Garellick G, Nemes S. Standard comorbidity measures do not predict patient-reported outcomes 1 year after total hip arthroplasty. Clin Orthop Relat Res. 2015;473(11):3370–3379. | ||
Bülow E, Rolfson O, Cnudde P, Rogmark C, Garellick G, Nemes S. Comorbidity does not predict long-term mortality after total hip arthroplasty. Acta Orthop. 2017;88(5):472–477. | ||
Cnudde P, Rolfson O, Timperley AJ, et al. Do patients live longer after THA and is the relative survival diagnosis-specific? Clin Orthop Relat Res. 2018;476(6):1166–1175. | ||
Hudak PL, Armstrong K, Braddock C 3rd, Frankel RM, Levinson W. Older patients’ unexpressed concerns about orthopaedic surgery. J Bone Joint Surg Am. 2008;90(7):1427–1435. | ||
Shrestha S, Dave AJ, Losina E, Katz JN. Diagnostic accuracy of administrative data algorithms in the diagnosis of osteoarthritis: a systematic review. BMC Med Inform Decis Mak. 2016;16:82. |
Supplementary materials
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.