Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
Prevalence and Predictors of Postpartum Depression Among Male Partners Who Came to Postnatal Follow-up Clinic with Their Partner in Selected Public Health Centers of Wolaita Zone, Ethiopia, 2019
Received 20 July 2020
Accepted for publication 8 September 2020
Published 7 October 2020 Volume 2020:16 Pages 2307—2316
DOI https://doi.org/10.2147/NDT.S273045
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
This paper has been retracted.
Mesfin Markos,1 Aseb Arba2
1Wolaita Sodo University College of Medicine and Health Sciences, Department of Midwifery, Wolaita Sodo, Ethiopia; 2Wolaita Sodo University College of Medicine and Health Sciences, School of Nursing, Wolaita Sodo, Ethiopia
Correspondence: Aseb Arba
Wolaita Sodo University, College of Medicine and Health Sciences School of Nursing, PO BOX 200, Wolaita Sodo, Ethiopia
Email [email protected]
Background: Paternal postpartum depression is a serious public health problem which has a significant effect on mortality and morbidity level. Its effect is not limited to the partner, but it also affects the family, the marital relationship and development of the child. Therefore, this study was planned to assess the prevalence and predictors of paternal postpartum depression among accompanying partners in selected public health centers of Wolaita Zone, Ethiopia.
Methodology: An institution-based cross-sectional study was conducted among 423 male partners. The study was conducted in 25 randomly selected health centers and samples proportionally allocated to each health center. Finally, the study participants were selected by systematic random sampling method. The collected data were entered into EpiData version 4.2.0 and exported to IBM SPSS for further analysis. The Edinburgh postnatal depression scale was considered at a cutoff point ≥ 10 to detect depression. Descriptive and binary logistic regression analyses were done. Adjusted odds ratio (AOR) and p-value results in multivariable logistic regression were used to declare strength and presence of association.
Results: Four hundred and ten partners participated in this study making a response rate of 97%. Seventy (17%) of the participants had paternal postpartum depression. Family income (AOR=3.0; 95%CI: 1.1– 8.2), substance use (AOR=4.5; 95%CI: 1.5– 13.3), family support (AOR=3.9; 95%CI: 1.3– 11.3), marital relation (AOR=4.1; 95%CI: 1.5– 11.0), unplanned pregnancy (AOR=3.5; 95%CI: 1.4– 8.7) and infant sleeping problems (AOR=10.0; 95%CI: 4.1– 24.0) were variables significantly associated with paternal postnatal depression.
Keywords: paternal postpartum depression, Edinburgh postnatal depression scale, parenthood
Introduction
Paternal postpartum depression (PPPD) also known as “paternal postnatal depression” is a seldom recognized mental illness in male partners that occurs with major depressive symptoms occurring within four weeks of childbirth and may extend to one year. These depressive symptoms they are experiencing are the symptoms of fatigue and changes in sleep or appetite, crying, and outward emotional symptoms.1–4
In addition, there are other common symptoms of PPPD. These include: irritability, unhealthy sexual relationships or infidelity, working more or less, low energy, exhaustion, lack of motivation or poor concentration, weight or appetite change, risk-taking behaviors including substance use, physical signs, anger and outbursts, escapist behavior, such as spending excessive time watching television, on the internet or at work, violent behavior and suicidal thoughts.5–10
The postpartum period is the transformation to paternity and it is a challenging and vulnerable period for most partners. Studies showed that partners suffer from depression after the birth of a child.3,11 Historically, postpartum depression was assumed to be a mental illness of women only. But about one quarter of new male partners could also experience overwhelming depression after the birth of their child.3,12,13 The transition to paternity may be complex and devastating, and may negatively influence the men’s health. The change and practice to paternity is considered one of the most acute changes experienced throughout a man’s life.8 The experience is influenced by the partner itself, relationship, and infant factors.14,15
Postpartum depression is a clinically significant problem for male partners, families and community which is currently underdiagnosed, and undertreated. There is wide variation in estimate of the prevalence of PPPD, ranging from 4–25% of partners within the postpartum period and its average prevalence was 10%.3,12 Despite postpartum depression among women having been studied by different researchers in different countries, the prevalence of depression among the male partners of newborn is a not well recognized, underscreened and underdiagnosed.14,16
Different scholars estimate the prevalence of PPPD extending from 1.2–25.5% in a community based study. It was higher among male partners whose partner had paternal postnatal depression; that ranges from one quarter to half of partners who were affected with depression.3,11 In Ethiopia, a study on the prevalence of PPPD was not conducted, but the prevalence of maternal postpartum depression ranged from 23.3–34%.17–19
PPPD carries increased suicide risk or loss of self-esteem and is associated with different variables as shown in conceptual framework Figure 1 in Supplementary data. In addition, it causes negative impact on the family, poor parenting behaviors, the marriage relationship, reduced parent–infant interaction, has implications for healthy child growth and development.20–25 Several factors have been identified that may precipitate PPPD including paternal factors; employment status, relationship factors; poor marital relationships; and infant-related problems.24,26–28 Although its prevalence is not adequately studied, recent investigations showed that the problem has advanced considerably over the past three decades. The estimates of the prevalence of PPPD within the first year vary widely ranging from 4–27%.2,29,30
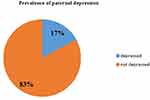 |
Figure 1 Prevalence of paternal postpartum depression among partners who came to postnatal follow-up clinic with their partner in Wolaita Zone public health centers, Ethiopia, (n= 410). |
The prevalence of maternal postpartum depression among Ethiopian postpartum women is high compared to global reported figure ranges from 4.5–20%.17–19,31 However, paternal depression among partners of a newborn is a new concept in Ethiopia. Despite the problem having been studied by different researchers in other countries, to our knowledge, there is no study conducted in Ethiopia on the problem under study, therefore we planned to assess the prevalence of paternal postpartum depression and its associated factors among partners who come to the postnatal follow-up clinic at Wolaita Zone health centers.
Significance of the Study
This study will be important for different stakeholders in addressing the issues related to paternal morbidity and mortality during the postpartum period. The result will point out prevention measures that are important for decreasing the occurrence of depression among partners of the newborns. The result will also provide information for strategic planning of comprehensive postnatal care and follow-up, support and care of partners with newborns. It is also expected that, the findings will be important for further psychiatric evaluation and hence, advanced mental health care and support will be integrated with the routine postnatal care and follow-up management guidelines. The study results may also show solutions for the paternal postpartum-related depression at the community level. And it also will be a baseline source for additional further research regarding PPPD.
Objectives
- To determine the prevalence of PPPD among partners who came to the postnatal follow-up clinic with their partner in selected Wolaita Zone health facilities, Ethiopia, 2019.
- To identify the factors associated with PPPD among partners who came to the postnatal follow-up clinic with their partner in selected Wolaita Zone health facilities, Ethiopia, 2019.
Methods and Materials
Study Area and Study Period
The study was conducted in public health centers of Wolaita Zone, which is one of administrative zones in SNNPR of Ethiopia. The zone has a total population size of 15 million as estimated in 2018 and it is divided in to 17 woredas (districts). There are seven hospitals and 73 health centers under Wolaita Zone health department. This study was conducted in selected public health centers of Wolaita Zone, which had postnatal follow-up units from April 1 to May 2, 2019.
Study Design
Institutional based cross-sectional study design was employed.
Population
All male partners who came to postnatal clinics with their partner to selected public health centers of Wolaita Zone during the study period were considered the study population.
Study Subjects
The study subjects were male partners who present at time of data collection in selected public health centers of Wolaita Zone and included in the study.
Inclusion and Exclusion Criteria
All male partner who come to postnatal follow-up clinic during the third visit with his partner and had an infant ≥4 weeks. Male partners who were not able to respond to questions were excluded.
Sample Size Determination and Sampling Procedure
The sample size was determined by using a single population formula. A 95%CI, 5% margin of error, and proportion of 50% were assumed because of the absence of the proportion of paternal postpartum depression in Ethiopia. The initial sample size was 384. After adding the nonresponse rate 10%, the final sample size was 423 shown in supplementary data.
The total number of public health centers in Wolaita Zone was 73. From these, three of them had no postnatal care follow-up figures to report in the previous month before the study. From the rest, 25 health centers were selected by lottery method. The sample size was allocated proportionally to each health center based on the previous months client follow-up records in the postnatal care unit shown in supplementary data. Then, study subjects from selected health centers were chosen by systematic random sampling method. The first partner was selected by lottery method and others selected were every second from the preceding participant.
Data Collection Tools
A structured questionnaire was adapted from previously published literature.4,13,32 The questionnaire had four parts; sociodemographic, personal, relationship, infant and environmental factors with depression, which was uploaded as supplementary data. It was prepared in English and translated into Amharic language by experts, then retranslated back into English by a different expert to ensure its consistency. The reliability of the questionnaire was checked and its Cronbach’s alpha reliability coefficient result was 0.81. It measures the feeling of partners during the previous seven days of the postnatal period. The Edinburgh postnatal depression scale (EPDS) was used to assess the depressive symptoms.33
Data Collection Procedure
A face-to-face interview was conducted using a structured and pretested questionnaire. The designed questionnaire contains close-ended and some open-ended questions. Exit interview was conducted in a private place after they received the service they required and after getting consent of participation. A total of 25 midwives were selected for data collection and four experts with an MSc in maternity and reproductive health were used for supervision.
Variables
Dependent Variable
- Paternal postpartum depression
Independent Variables
- Sociodemographic and personal factors: age, religion, educational status, employment status, number of newborns, family income, substance use, history of depression, experience of being father to baby.
- Relationship factors: family set up, relationship with parents, support from friend, marital status, marital relation, family support, number of wife, and relative mental illness.
- Infant and environmental factors: Residence of wife after delivery, housing status, planned/unplanned pregnancy, antenatal follow-up status, mode of delivery, presence/absence of male partner at delivery of a baby, GA of the pregnancy, congenital birth problems, place of delivery, infant sleeping problem, and history of loss of child.
Operational Definitions
- Depression: when the cumulative score of Edinburgh postnatal depression scale (EPDS) was 10 or above. The scale has 10 items and each item of the scale was scored from 0 to 3, yielding a total range of 0–30. The score of questions number 1, 2, and 4 were the first choice and scored as 0, the second choice scored as 1, the third choice scored as 2 and the last choice scored as 3 and the score of question number 3, 5, 6, 7, 8, 9, and 10 were scored the first as 3, second as 2, third as 1 and the last 0.
- Substance use: when the male partners used any one or more of the substances (alcohol, chat, and or cigarette).
Data Quality Assurance
Data were collected by trained health-care providers who have previous experience of data collection and participation in research. Training was given to data collectors. Training addressed the detailed explanation of every question with clear understanding. Then the research tool was pretested in Bilate Charicho and Anka Duguna health centers among 22 male partners, and necessary arrangements and corrections were made to standardize the questionnaire. The quality of the data collection process was supervised by the principal investigator.
Data Analysis
Data were coded and entered to EpiData version 4.2.0 and exported to IBM SPSS version 20 software package for analysis. Descriptive statistics were done to get frequencies, percentages and cross-tabulations. Then, binary logistic regression statistical model was employed for bivariate and multivariable analysis. The outcome variable is based on EPDS score; a cutoff point ≥10 was categorized as presence of depression. Finally, the presence of association of covariates with depression was declared when p-values <0.05 and AORs at 95%CI in multivariable analysis.
Ethical Consideration
The study was approved by the Research and Ethical approval Committee of School of Nursing, Lideta College of Health Sciences and Business where the authors worked as part-time instructors. An official letter from the School of Nursing was written to Wolaita Zone Health Department and to Health centers. The study was conducted in accordance with the Declaration of Helsinki. Informed voluntary consent was taken before starting the interview. Privacy and confidentiality was maintained during the interview. The subjects were informed that any information they provided was confidential shown in supplementary data. Any personal identification of the study participants was not recorded during data collection.
Results
Socioeconomic and Paternal Personal Factors
It was planned to interview 423 partners in this study. Out of them, 410 successfully participated in the study making the response rate of 97%. The mean age of the participants was 32.02±5.36 years and two thirds of respondents were in between 25 and 34 years, the age of baby at the time of interview of fathers was 44.49±3.04 days after delivery. Out of 410, 153 (37.3%) were fathers of the first child, while 257 (62.7%) were experienced partners. The majority of 385 (93.9%) partners had one newborn, and the rest had twin and triple newborns, and 210 (51.2%) of partners were orthodox by religion. One hundred and eighty (43.9%) of partners completed higher education, 370 (90.2%) of partners were government employees. Among the employed, 331 (89.5%) were permanent employees and 39 (9.5%) of them were temporary employees. Among these, 312 (76%) received paternal leave. The average family income of the respondents were 5064±2669.41 Ethiopian birr, ranging from 1000–26,000 and 257 (62.7%) of the respondents were not comfortable with their family income, 42 (10.2%) of the participant were using at least one of the substances shown in Table 1.
 |
Table 1 Socioeconomic and Paternal Factors of Participant Who Came to Postnatal Follow-Up Clinic with Their Partner in Wolaita Zone Public Health Centers, Ethiopia (n=410) |
Relationship-related Characteristics of the Participants
All of the respondents were married and almost all of them 408 (99.5%) were living together with their partner. Almost all of the respondents 407 (99.3%) had one wife. Nearly all of partners reported that they lived with nuclear family. Three hundred and fifty-five (86.6%) of the respondents had a good marital relationship. About three quarters of the respondents had a good relationship (70.2%), with their parents had support from friends (72.9%) and had family support (73.4%) as shown in Table 2.
 |
Table 2 Relationship Related Characteristics of Partners Who Came to Postnatal Follow-up Clinic with Their Partner in Wolaita Zone Public Health Centers, Ethiopia (n=410) |
Infant and Environment-related Characteristics of the Participants
Concerning their housing, 270 (65.9) of the respondents were living in rental houses, and only 25 (6.1%) respondents wives went to her mother or family house for delivery. More than two thirds of pregnancies were planned 316 (77.1%). More than two-thirds, 340 (82.9%) and 342 (93.4%) of partners were present at the time of antenatal checkup and delivery of infant, respectively. Among all respondents, 336 (82%) reported that the delivery of their child were vaginal delivery. Most of the babies 301 (73.4%) were delivered at term and more than two-thirds, 334 (81.5%) of infants were delivered at governmental health institution. Seven (1.7%) respondents had congenital problems. Eighty-two (20%) infants had sleeping problems shown in Table 3.
 |
Table 3 Infant and Environmental Related Characteristics of Partners Who Came to Postnatal Follow-up Clinic with Their Partner in Wolaita Zone Public Health Centers, Ethiopia (n= 410) |
Prevalence of Paternal Postpartum Depression
From all participants, 70 (17%) of respondents scored above cutoff point for PPPD (≥10), and 340 (83%) participants were scored below the cutoff point for paternal postpartum depression. Hence the prevalence of PPPD was 17% with (13.36, 20.64) at 95%CI as shown in Figure 1.
Factors Associated with Paternal Postpartum Depression
Bivariable analysis was done for each independent variables with the dependent variable using binary logistic regression. The variables with p<0.25 in bivariable analysis were exported to multivariable analysis. These variables were employment status, comfortable to family income, substance use, history of depression, relationship with parents, friend support, family support, marital relationship, planned pregnancy, attend antenatal checkup with partner, accompany partner at the time of delivery of child, infant sleeping problems, and child loss before the birth of this child. From these variables, six variables were significantly associated with PPPD.
The partners who were not comfortable on the family income were three times more likely to develop depression than those who were comfortable with family income (AOR=3.0; 95%CI: 1.1–8.0). Those partners who currently use substances were five times more likely to develop depression than those not using substances (AOR=5.0; 95%CI: 1.7–14.5). In addition, partners who had no family support were nearly four times more likely to be depressed than those who had family support (AOR=3.8; 95%CI: 1.3–11.1).
Those partners who did not have a good marital relationship with their partner were 4.4 times more likely to be depressed than those with good marital relationship (AOR=4.4; 95%CI: 1.6–11.7). Those partners who had unplanned pregnancy (delivery) were 3.5 times more likely to be depressed than those partners with planned pregnancy (AOR=3.5; 95%CI: 1.4–8.8). Those partners whose infant had sleeping problems were nearly 11 times more likely to develop PPPD compared to their counterparts (AOR=10.9; 95%CI: 4.6–25.8) as displayed in Table 4.
Discussion
The current study planned to determine the prevalence and predictors of paternal postnatal depression among partners who came to postnatal follow-up clinics with their partner in public health centers of Wolaita Zone, Ethiopia. In this study, 70 (17%) (95%CI: 13.36–20.64) partners had depression; this showed that a significant proportion of partners were suffering from PPPD. This figure goes in line with studies conducted in Saudi Arabia,32 Japan,34 and Northwest China35 where the prevalence of PPPD was 16.6%, 16.7%, and 13.6%, respectively. This might be due to variation in study population, study time variation of the study between previous study and this study.
However, this proportion was lower when compared with a similar study conducted in Ireland where the level of paternal postnatal depression was 28%.4 This might be due to the population difference, sample size and study period difference. And the current proportion of paternal depression was somewhat higher when compared to other studies in Japan in 2017 which was 8.8,36 in Australia, 9.7,37 in Brazil, 11.9,13 and in US, 10.3.12
This discrepancy in prevalence of PPPD might be due to the difference in study method, population, assessment tool, and study period. For example, the study conducted in Japan was studied by longitudinal method, and in Australia the Kessler-6 scale was used,37 in Brazil BDI was used,13 and in the US they used the Center for Epidemiologic Studies Depression Scale (CESD).12 The current result was also higher when compared with another study conducted in Japan in 2018, in which 11.2% of partners were depressed.38 This difference might be due to cutoff point difference, sample size difference, sociodemographic difference.
In the current study, paternal postnatal depression was significantly associated with partners who were not comfortable to their family income)AOR=3.0; 95%CI: 1.1–8.0). This finding was consistent with the study done in Ireland,4 and in the University of Lublin.39 It might be because of the fact that parenthood increases the need of fulfilling the essential materials for the family including the newborn's basic needs. Facing difficulty due to economic conditions might further affect the mood of partners during the postpartum period.
In the current study, PPPD was significantly higher among partners who were using substances than that of nonusers (AOR=5.0; 95%CI: 1.7–14.5). This result was in line with the studies conducted in Brazil and Japan.13,40 This might be due to taking substances during this period that might change the mood of partners or it might cause them economic crisis due to increased demand of family as well as expense of substance.
Furthermore, partners who had no family support were nearly four times more likely to be affected by paternal postpartum depression than that of partners who had family support (AOR=3.8; 95%CI: 1.3–11.1). This result goes in line with the study conducted in Ireland.4 This might be due to the fact that feelings of loneliness may change the mood of the partners. However, family support was not associated with depression in the study conducted in Saudi Arabia.32 This might be due to difference in study setting, study period, and population.
In addition, partners who did not have a good marital relationship with their partner were more likely to develop PPPD (AOR=4.4; 95%CI: 1.6–11.7). But, this factor was not associated with the study conducted in Saudi Arabia.32 This change might be due to population, sample size, methodology difference. In the current study, partners who had unplanned pregnancy were significantly associated with PPPD (AOR=3.5; 95%CI: 1.4–8.8). This result is in line with the study conducted in 2010 in Japan.41 This might be the similarity in the assessment tool. This result differs from the study conducted in Ireland, in which there was no significant association between planning of pregnancy and PPPD.4 This might be due to the population difference.
Furthermore, the association found in the current study was having an infant with sleeping problems. Partners who had an infant with sleeping problems were more likely to be depressed than that of partners who had an infant without sleeping problems (AOR=10.9; 95%CI: 4.6–25.8). This result was consistent with the study conducted in Ireland.4 This finding might show that the partners were worried about the healthiness of the child and this further might cause them to develop depression.
Recommendations
Depending on the findings, the following recommendations were forwarded to the Wolaita Zone Health Department, health professionals, different NGOs and researchers working on health and other sectors.
- In collaboration with the Ministry of Health, it is recommended to develop guideline for postnatal follow-up that include mental and reproductive health screening for both partners (father and mother).
- We recommend Wolaita Zone Health department to offer basic facilities needed for childcare with affordable cost during postnatal follow-up.
- We recommend health professionals to provide health education on the effects of substance use by using different mass media and making it inaccessible easily by low cost.
- We recommend provision of pre-marriage, preconception and perinatal counseling service in collaboration with other sectors.
- NGOs and governmental organizations working on sexual and reproductive health (SRH) should provide further attention on utilization of family planning methods to minimize unplanned pregnancy.
- Provide better training for health-care providers on how to counsel regarding paternal postpartum depression prevention and related issues.
- We recommend health professionals to provide mental health screening for partners, especially during preconception care, antenatal care, perinatal and postnatal period.
- The researchers are recommended to conduct further research by using different design (mixed study) and setting to identify further risk factors to paternal postpartum depression.
Strength and Limitation of Study
This study focused on paternal postpartum depression which was not conducted before in the study area. However, there could be introduction of social desirability bias. To minimize this bias, data collectors explained about purpose of study and confidentiality of their response. By its cross-sectional nature, it is difficult to establish causal relationship between the covariates and the outcome variable. In addition, authors faced difficulty for comparison due to limitation of literature on related topics.
Conclusion
PPPDn was high among partners who came to postnatal clinics of the Health Centers of Wolaita Zone. Economic problems, substance use, relationship factors, family support, marital relationship, unplanned pregnancy and infant sleeping problems were a significant predictors of PPPD in the study area.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; EPDS, Edinburg postnatal depression scale; GA, gestational age; PPND, paternal postnatal depression; PPPD, paternal postpartum depression; SNNPR, Southern, Nation Nationalities and People’s Region; SPSS, statistical package for social sciences.
Data Sharing Statement
All interested persons or institutions could get final logistic regression SPSS file by sending email to [email protected].
Acknowledgment
We appreciate the managers of health center, study participant and data collectors for their cooperation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work. Authors received no funding for this study.
References
1. National Institute of Mental Health. Major depression among adults. 2015. Available from: https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-amongadults. shtml.
2. Cameron EE, Sedov ID, Tomfohr-Madsen LM. Prevalence of paternal depression in pregnancy and the postpartum: an updated meta-analysis. J Affect Disord. 2016;206:189–203. doi:10.1016/j.jad.2016.07.044
3. Goodman JH. Postpartum depression beyond the early postpartum period. J Obstet Gynecol Neonatal Nurs. 2004b;33:410–420. doi:10.1177/0884217504266915
4. Philpott LF, Corcoran P. Paternal postnatal depression in Ireland: prevalence and associated factors. Midwifery. 2018;56:121–127. doi:10.1016/j.midw.2017.10.009
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Press, Inc; 2004.
6. Melrose S. Paternal postpartum depression: how can nurses begin to help? Contemp Nurse. 2014;34(2):199–210. doi:10.5172/conu.2010.34.2.199
7. Veskrna L. Peripartum depression – does it occur in partners and does it matter? J Men's Health. 2010;7(4):420–430.
8. Wilson CW. Paternal postpartum distress: available at a discourse analytic study. 2008. Available from: https://hydra.hull.ac.uk/assets/hull:5742a/content.
9. McCoy SJB. Postpartum depression in men. 2012. Avaliable from: http://tinyurl.com/jbavrmb.
10. McKellar L, Pincombe J, Henderson A. ‘Coming ready or not!’ Preparing parents for parenthood. Br J Midwifery. 2009;17(3):160–167. doi:10.12968/bjom.2009.17.3.40078
11. Anna deMagistris MC, Carta M, Fanos V. Postpartum depression and the male partner. J Pediatr Neonat Individual Med. 2013;2:15–27.
12. Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and partners on parenting behavior. Pediatrics. 2006;118:659–668. doi:10.1542/peds.2005-2948
13. Pinheiro R, Magalhães P, Horta B, Pinheiro K, Da Silva R, Pinto R. Is paternal postpartum depression associated with maternal postpartum depression? Population‐based study in Brazil. Acta Psychiatr Scand. 2006;113(3):230–232. doi:10.1111/j.1600-0447.2005.00708.x
14. Brockington I. Postpartum psychiatric disorders. Lancet. 2004;363(9405):303–310. doi:10.1016/S0140-6736(03)15390-1
15. Wilkins C. A qualitative study exploring the support needs of first-time mothers on their journey towards intuitive parenting. Midwifery. 2006;22(2):169–180. doi:10.1016/j.midw.2005.07.001
16. Musser AK, Ahmed AH, Foli KJ, Coddington JA. Paternal postpartum depression: what health care providers should know. J Pediatr Health Care. 2013;27(6):479–485. doi:10.1016/j.pedhc.2012.10.001
17. Fantahun A, Cherie A, Deribe L. Prevalence and factors associated with postpartum depression among mothers attending public health centers of wolaita zone, Ethiopia, 2016. Clin Pract Epidemiology Ment Health. 2018;14:196–206. doi:10.2174/1745017901814010196
18. Kerie S, Menberu M, Niguse W. Prevalence and associated factors of postpartum depression in Southwest, Ethiopia, 2017: a cross-sectional study. BMC Res Notes. 2018;11:623. doi:10.1186/s13104-018-3730-x
19. Tefera TB, Erena AN, Kuti KA, Hussen MA. Perinatal depression and associated factor among reproductive aged group women at Goba and Robe Town of Bale Zone, Oromia Region, Ethiopia. Maternal Health, Neonatology, and Perinatology. 2015;1:12. doi:10.1186/s40748-015-0013-6
20. Quevedo L, da Silva RA, Coelho F, et al. Risk of suicide and mixed episode in men in the postpartum period. J Affect Disord. 2011;132:243–246. doi:10.1016/j.jad.2011.01.004
21. Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressives symptoms: exploring multiple relations with child and family functioning. J Child Psychol Psychiatry. 2005;46:479–489. doi:10.1111/j.1469-7610.2004.00368.x
22. Feldman R, Eidelman AI. Parent–infant synchrony and the social-emotional development of triplets. Dev Psychol. 2004;40:1133–1147. doi:10.1037/0012-1649.40.6.1133
23. Solantaus T, Salo S. Paternal postnatal depression: partners emerge from the wings. Lancet. 2005;365:2158–2159. doi:10.1016/S0140-6736(05)66754-2
24. Demontigny F, Girard ME, Lacharite C, Dubeau D, Devault A. Psychosocial factors associated with paternal postnatal depression. J Affect Disord. 2013;150:44–49. doi:10.1016/j.jad.2013.01.048
25. Kvalevaag AL, Ramchandani PG, Hove O, Assmus J, EberhardGran M, Biringer E. Paternal mental health and socioemotional and behavioral development in their children. Pediatrics. 2013;131:e463–e469. doi:10.1542/peds.2012-0804
26. Boyce P, Condon J, Barton J, Corkindale C. First-time partners study: psychological distress in expectant partners during pregnancy. Aust N Z J Psychiatry. 2007;41:718–725. doi:10.1080/00048670701517959
27. Bronte-Tinkew J, Moore KA, Matthews G, Carrano J. Symptoms of major depression in a sample of partners of infants sociodemographic correlates and links to partner involvement. J Fam Issues. 2007;28:61–99. doi:10.1177/0192513X06293609
28. Dave S, Nazareth I, Sherr L, Senior R. The association of paternal mood and infant temperament a pilot study. Br J Dev Psychol. 2005;23:609–621. doi:10.1348/026151004X22962
29. Wilson CW. Paternal postpartum distress: a discourse analytic study. 2008. Available from: https://hydra.hull.ac.uk/catalog/hull:5742.
30. Wee KY, Skouteris H, Pier C, Richardson B, Milgrom J. Correlates of ante- and postnatal depression in partners: a systematic review. J Affect Disord. 2011;130:358–377. doi:10.1016/j.jad.2010.06.019
31. O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9:379–407. doi:10.1146/annurev-clinpsy-050212-185612
32. Shaheen NA, AlAtiq Y, Thomas A, et al. Paternal postnatal depression among partners of newborn in Saudi Arabia. Am J Men's Health. 2019;13:1557988319831219. doi:10.1177/1557988319831219
33. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–786. doi:10.1192/bjp.150.6.782
34. Suto M, Isogai E, Mizutani F, Kakee N, Misago C, Takehara K. Prevalence and factors associated with postpartum depression in partners: a regional, longitudinal study in Japan. Res Nurs Health. 2016;39(4):253–262. doi:10.1002/nur.21728
35. Zhang YP, Zhang LL, Wei HH, et al. Postpartum depression and the psychosocial predictors in first-time partners from northwestern China. Midwifery. 2016;35:47–52.
36. Takehara K, Suto M, Kakee N, Tachibana Y, Mori R. Prenatal and early postnatal depression and child maltreatment among Japanese partners. Child Abuse Negl. 2017;70:231–239. doi:10.1016/j.chiabu.2017.06.011
37. Giallo R, D’Esposito F, Cooklin A, et al. Psychosocial risk factors associated with partners’ mental health in the postnatal period: results from a population-based study. Soc Psychiatry Psychiatr Epidemiol. 2013;48:563–573. doi:10.1007/s00127-012-0568-8
38. Nishigori H, Obara T, Nishigori T, et al. The prevalence and risk factors for postpartum depression symptoms of partners at one and 6 months postpartum: an adjunct study of the Japan Environment and Children’s Study. J Matern Fetal Neonatal Med. 2020;33:2797–2804.
39. Tuszyńska-Bogucka W, Nawra K. Paternal postnatal depression a review. Arch Psychiatry Psychother. 2014;2:61–69. doi:10.12740/APP/26286
40. Luoma I, Puura K, Mantymaa M, Latva R, Salmelin R, Tamminen T. Partners’ postnatal depressive and anxiety symptoms: an exploration of links with paternal, maternal, infant and family factors. Nord J Psychiatry. 2013;67:407–413. doi:10.3109/08039488.2012.752034
41. Nishimura A, Ohashi K. Risk factors of paternal depression in the early postnatal period in Japan. Nurs Health Sci. 2010;12(2):170–176. doi:10.1111/j.1442-2018.2010.00513.x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

