Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 14
Prevalence and Characterization of bifid mandibular Canal Using Cone Beam Computed Tomography: A Retrospective Cross-Sectional Study in Saudi Arabia
Authors Soman C , Wahass T , Alahmari H , Alamri N , Albiebi A , Alhabashy M , Talha A , Alqhtani N
Received 13 August 2022
Accepted for publication 20 September 2022
Published 30 September 2022 Volume 2022:14 Pages 297—306
DOI https://doi.org/10.2147/CCIDE.S386098
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Cristalle Soman,1 Tariq Wahass,2 Hatem Alahmari,2 Nader Alamri,2 Assaf Albiebi,2 Mohammed Alhabashy,2 Abdulrahman Talha,2 Nasser Alqhtani3
1Department of Oral and Maxillofacial Surgery and Diagnostic Science, College of Dentistry, Riyadh Elm University, Riyadh, Saudi Arabia; 2College of Dentistry, Riyadh Elm University, Riyadh, Saudi Arabia; 3Department of Oral and Maxillofacial Surgery and Diagnostic Science, College of Dentistry, Prince Sattam Bin Abdulaziz University, Alkharj, Saudi Arabia
Correspondence: Tariq Wahass, College of Dentistry, Riyadh Elm University, 4078, Alshabareqah St, Ishbiliyah District, Riyadh, Saudi Arabia, Tel +966 0112402529, Email [email protected]
Aim: The purpose of this study is to determine the prevalence and morphological characteristics of the bifid mandibular canal in a Saudi Arabian subpopulation, to aid in preventing surgical complications near the mandibular canal.
Patients and Methods: Using CBCT images obtained from the Radiology unit database in a University Hospital Clinics. A total of 488 CBCT images were investigated (244 Female – 178 Male). In the present study, the Naitoh classification was used to categorize the bifid mandibular canal into the following types: 1) Retromolar canal; 2) Dental canal; 3) Forward canal (with or without confluence); and 4) Buccolingual canal. Additional variation (Trifid canal) was included. All CBCTs were assessed in coronal, sagittal, axial, as well as panoramic views using specialized software.
Results: The prevalence of BMC was 28.7% (95% CI, 24.5 to 33.2), Gender (p = 0.404) and age (p = 0.654) had no statistical significances, laterality of BMC, patients with unilateral BMC were significantly older than those with bilateral BMC (mean ± SD ages of 40.5 ± 13.5 and 32.9 ± 13.8, respectively, p = 0.009). About two-thirds (67.5%) of the investigated BMC cases were found unilateral. The most common reported type of BMC was retromolar canal.
Conclusion: The incidence of bifid mandibular canal using CBCT is considered relatively high in Saudi Arabian subpopulation, with the most common type was the retro-molar canal.
Keywords: mandibular canal, bifid mandibular canal, cone-beam computed tomography, anatomical variation, surgical complications, dental implant
Introduction
The mandibular canal houses both the inferior alveolar artery and inferior alveolar nerve. The canal starts at the mandibular foramen and terminates at the mental foramen.1 Some variations relating to the location and configuration of the mandibular canal pose importance in clinical procedures that involve surgeries in the area.2
A mandibular canal variation known as the bifid mandibular canal (BMC) is characterized by a canal that splits into two branches, each of which may have its own neurovascular supply.3 It has been suggested that the alteration from the normal development occurs during the prenatal growth phase in which a lack of fusion between the three canals to form a single mandibular canal takes place, resulting in bifurcation or trifurcation of the canal.4 The prevalence of BMC varies from one population to another, furthermore, varies from which diagnostic imaging has been used.5,6 Traditionally, Orthopantomogram (OPG) was used to reveal such alteration, but it has been found that OPG underestimates the prevalence of BMC significantly when compared to a more recent technology such as cone-beam computed tomography (CBCT).7 When CBCT is compared to conventional CT scans, CBCT is considered the superior option in visualizing BMC with its high-resolution, high-accuracy, three-dimensional imaging with low radiation doses.8
When using OPG, the prevalence of BMC has been reported as 0.08% by Grover and Lorton,9 0.35% by Sanchis et al,10 0.9% by Nortje et al,3 and 0.95% by Langlais et al.11 Alternatively, studies that used CBCT in detecting BMC reported a prevalence of 15.6–64.8%.2,12–15
High variability in detecting BMC was noted in different populations. In a study done by Kang et al,7 the incidence of BMC in a Korean population was 10.2%. In a Turkish population, Orhan et al13 reported an incidence of 46.5%. And de Oliveira-Santos15 conducted a study in Belgium that demonstrated 19% incidence of BMC.
Various complications may associate with BMC, including injury to the nerve or the blood vessel caused by third molar extraction, implant placement, or bilateral sagittal split osteotomy procedures, subsequently, paraesthesia or bleeding could be the result.16,17 Moreover, difficulty in obtaining successful anaesthesia may also be a consequence in the case of BMC.18,19
There are multiple classifications for BMC. Few of them were based on panoramic views.11,20 But a more commonly used classification, that is based on CBCT viewings, was put forth by Naitoh et al2 which classified BMC into four main types: 1) Retromolar canal; 2) Dental canal; 3) Forward canal (with or without confluence); 4) Bucco-lingual canal. Additionally, there is a special type showcasing trifurcation of the mandibular canal.6,17
This study aims to determine the prevalence and morphological characteristics of the bifid mandibular canal in a Saudi Arabian subpopulation in order to assist dental professionals take this anatomical variation under consideration when performing surgical procedures near the mandibular canal and to compare the findings with previous studies that used similar methodology to identify BMC in various populations.
Materials and Methods
This retrospective cross-sectional study investigated the prevalence of Bifid Mandibular Canal in Saudi Arabia. Classification was according to (Naitoh et al, 2009).2 This classification was used due to it being based on a CBCT study, and for being commonly used in other studies which would make comparing results feasible. We examined the number of BMCs, if present unilaterally or bilaterally, and if there is a statistically higher prevalence in one gender or age group.
(Naitoh, 2009)2 classification of BMCs (illustrated in Figure 1 and Figure 2):
- Type I (Retromolar canal type): The retromolar canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward, reaching the retromolar region.
- Type II (Dental canal type): The dental canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward, reaching the roots of the molars.
- Type III (Forward canal type): Forward canal without confluence: The forward canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward to the second molar region. Forward canal with confluence: The forward canal, which bifurcates from the mandibular canal in the mandibular ramus, courses anteriorly and then rejoin the main mandibular canal.
- Type IV (Buccolingual canal type): The buccal canal, which bifurcates from the mandibular canal in the mandibular ramus, courses bucco-inferiorly. Lingual canal: The lingual canal, which bifurcates from the mandibular canal in the mandibular ramus, courses lingually and then penetrates through the lingual cortical bone.
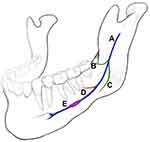 |
Figure 1 (A) The main mandibular canal. (B) The retromolar canal type. (C) The forward canal type, without confluence. (D) The dental canal type. (E) The forward canal type, with confluence. |
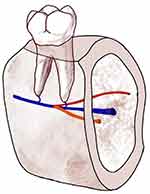 |
Figure 2 The main mandibular canal (Blue line); The buccolingual canal type (Red lines). |
Inclusion Criteria
- Above 15 years of age.
- CBCT data from Riyadh Elm University hospitals.
- Clear visualization of the mandibular canal.
Exclusion Criteria
- Under 15 years of age.
- Presence of a cyst or tumor in the mandible, rendering the canal unclear.
- History of systemic diseases affecting the bone.
- History of surgical procedures in the mandible.
The sample selection was randomized, and the size was 422 CBCTs (244 Female and 178 Male). CBCT images were obtained from the Radiology unit database from University Hospital Clinics from a private university in Riyadh. The acquired CBCTs were taken during the years 2018–2020. CBCT data was captured using Sirona Galileos (Germany) at 85 kV, 5 −7 mA, and 14s. Analysis was done using the digital imaging analysis software, Galileos viewer (Sidexis XG), version 1.6 using panoramic windows for initial screening and multiplanar reformatted windows with 5cm slice thickness using axial, coronal and sagittal views for detailed analysis. All the investigators who are primarily dentists were calibrated using 5 CBCT scans each to enable them to use the software for initial data screening and segregation of data was performed according to inclusion and exclusion criteria. CBCTs were evaluated by the investigators for initial data screening, Segregation and scrutinization for presence of bifid canals, following which the details of the bifid canal were analyzed by an Oral and maxillofacial Radiologist with more than 8 years of expertise in the use of CBCT. The screening and segregation of scans were done every week for 20 cases. Following which, the data analysis was carried out for 5 scans every week with the duration of data analysis. The data collection was completed in 7 months.
Ethical Approval
The study collected retrospective imaging data files of the patient. The study followed declaration of Helsinki, 2013 with Information confidentiality declaration submitted for ethical approval for the use of deidentified data for all the age groups in the inclusion criteria, including patients from 15–17 years. This study was registered and approved by the Institutional Review Board (IRB) at Riyadh Elm University with the approval number: FIRP/2021/103/600/577.
Statistical Analysis
Numerical variables were presented as mean ± standard deviation, whereas categorical variables were expressed as frequencies and percentages. The prevalence of bifid mandibular canal (BMC) was assessed using the one-sample proportions test with continuity correction, and the outcomes were presented as the prevalence and 95% confidence interval. Correlation analysis was carried out using Wilcoxon rank sum test for numerical variables and Pearson’s Chi-squared test or Fisher’s exact test for categorical variables (whenever appropriate). Statistical significance was considered at p < 0.05.
Result
Characteristics of Patients
Initially, data was collected for a total of 481 patients. However, the records of 59 patients were excluded (the reasons for exclusion are listed in Table 1). Accordingly, we analyzed the data of 422 patients. Among 422 patients, 123 patients were found to have bifid canal, unilaterally and bilaterally. The mean ± age of patients was 38.5 ± 15.0 years. Females represented 57.8% of the sample (Table 2).
 |
Table 1 The Reasons for Exclusion Among the Patients Who Were Not Included |
 |
Table 2 Characteristics of the Sample Under Study |
Characteristics of BMC and the Associated Factors
The prevalence of BMC was 28.7% (95% CI, 24.5 to 33.2). Among those patients, unilateral BMC was prevalent among 67.5% and bilateral BMC among 32.5%. BMC was located on the right side in 67.5% and on the left side in 61.0% of patients (Table 3). BMC was not associated with patients’ age (p = 0.654) or gender (p = 0.404, Table 4).
 |
Table 3 Characteristics of BMC for the Sample Under Study |
 |
Table 4 Factors Associated with BMC |
The Association Between Demographic Characteristics and the Side and Laterality of BMC
Patients’ age was not associated with having BMC on the right side (p = 0.080) or the left side (p = 0.379). Likewise, patients’ gender did not imply significant differences for BMC on the right side (p = 0.592) or the left side (p = 0.902, Table 5). Considering the laterality of BMC, results showed that patients with unilateral BMC were significantly older than those with bilateral BMC (mean ± SD ages of 40.5 ± 13.5 and 32.9 ± 13.8, respectively, p = 0.009). Nevertheless, BMC laterality did not differ based on patients’ gender (p = 0.471, Table 6).
 |
Table 5 The Association Between Demographic Characteristics and the Side of BMC |
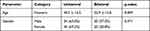 |
Table 6 Factors Associated with the Laterality of BMC |
Distribution of Various Types of BMC Among the Patients
The most commonly reported types of BMC on the left side included type I - retromolar canal (28.5%), type II - dental canal (16.3%) and Type III - forward canal with confluence (8.1%, Figure 3). On the right side, the most common types were type I - Retromolar canal (25.2), type II - Dental canal (13.0%) and type III - Forward canal without confluence (11.4%, Figure 4). More details about the distribution of BMC types are provided in Table 7.
 |
Table 7 Distribution of Various Types of BMC Among the Patients |
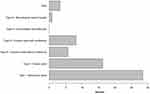 |
Figure 3 Percentages of different types of BMC in the left side of the investigated cases. |
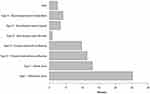 |
Figure 4 Percentages of different types of BMC in the right side of the investigated cases. |
Discussion
The mandibular canal is an anatomical structure that contains the inferior alveolar neurovascular bundle, which both the original and its normal variations are important to the vascularization and the dental structures supply and their surrounding tissue, thus, facilitating appropriate treatment and limiting the complications, the clinician should be aware in these kinds of variations.6 Considering the possible clinical complications of this variable which have been reported in the literature, including the challenge of providing sufficient anesthesia, some studies recommend the use of Gow-Gates or Akinosi-Vazirani technique.19,21 Furthermore, the possibility of bifid neurovascular bundle injury during implant site preparation and insertion, a third molar extraction, and orthognathic surgery (BSSO). In addition, some of the complications could happen during endodontic treatment (extrusion of sealer or over-instrumentation). This kind of injury could directly affect the mandibular canal or indirectly the bifid mandibular canal.6 The present study aims to assess the prevalence and characterization of the bifid mandibular canal in the Saudi Arabia subpopulation using Cone-beam computed tomography.
The investigation of bifid mandibular in the literature varies from study to study. Cone-beam computed tomography and CT scans were employed in some studies, while others used cadavers and orthopantomograms (OPG). When compared to more contemporary technologies, such as CBCT, Orthopantomogram (OPG), which was utilized in the past to evaluate the bifid mandibular canal, has certain limitations due to the two-dimensional perspective and the superimposition of other structures. The visualization of the mandibular canal using panoramic radiography has been cited in the literature in which it was not visible to some degree in 32%, 36%, and 64% of the cases studied by Naitoh et al,22 Klinge et al,23 and Lindh et al24 respectively. This brings attention to the limitation of this modality to detect bifid mandibular canal. The detection of BMC using panoramic radiography was less than one percent in multiple studies9–11,20,25 while found in a range between 1.98–11% in other studies.26–28 CBCT-based studies have shown a considerably higher prevalence of bifid mandibular canal 15.6–64.8% which is in agreement with the present study.7 The findings of the present study and the studies which used CBCT for the detection of bifid canal was noted to be have a higher prevalence of detection in comparison to those studies using panoramic radiography. This can clearly demonstrate the higher accuracy in the detection of anatomic details using CBCT in comparison to panoramic radiography. The detailed information thus obtained can be of much value especially during implant/surgical procedures in this area of mandible with decrease in hemorrhage and better treatment outcome.
In the present study, the prevalence of BMC was 28.7% (95% CI, 24.5 to 33.2). This suggests that there is no statistically significant difference in the prevalence of BMC between males and females which complies with different studies in the literature.2,29–31 On the other hand, this finding is incompatible with a study obtained by Muinelo-Lorenzo et al that showed that BMC was found to be statistically significant positive among male participants.32 The prevalence of BMC in a study carried out by Villaça-Carvalho et al was compatible with this current study’s findings in which BMC was detected in 80 out of 300 participants (26.67%).33 In this study, the most common type of BMC is the type I - retromolar canal (28.5%), which is in line with many other studies including Zhou et al,34 Zhang et al,30 Kang et al.7 However, many studies revealed the most common type is the forward canal including, Qaid et al,35 Orhan et al,13 Okumuş et al,21 Naitoh et al,2 Yang et al.36 In the present study, the incidence of the trifid canal (2.4%), is in agreement with a previous study.21 However, some studies reported no incidence of trifid canals.35,37
There are some limitations extended to this study. It was noted that some of the CBCTs that were examined had lower resolution than the others, which may cause inaccurate interpretation in the examination process especially due to ring artifacts. Furthermore, the diagnostic ability between the examiners could be a limitation during initial data screening and segregation, which might have contributed to be a confounding factor.
Conclusion
The incidence of bifid mandibular canal by using CBCT is considered relatively high in Saudi population, with the most common type is the retro-molar canal. The study emphasis the need for detailed anatomical review of the imaging data prior to any implant/oral surgical procedures in this area to avoid complications. Future studies should be aimed to evaluate the course of the bifid canals in the area in association to the length of bifurcations of the canal.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki 2013, and approved by the Institutional Review Board of Riyadh Elm University (IRB approval number ”FUGRP/2021/222/385/383).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study and from the guardians of patients below 18 years for the use of deidentified imaging data.
Acknowledgments
We are grateful to all the concerned team who aided in the conduct of our research. We would like to thank the research center at Riyadh Elm University for the support.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study is supported by Research and Innovation Center at Riyadh Elm University for promotion of scientific research.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
References
1. Lea F. Anatomy of the human body. Clemente CDCranial nerves. 1985;4:1165–1169.
2. Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2009;24(1):155–159.
3. Nortjé CJ, Farman AG. The radiographic appearance of the inferior dental canal: an additional variation. Br J Oral Surg. 1977;15(2):171–172. doi:10.1016/0007-117x(77)90050-6
4. Chávez-Lomeli ME, Mansilla Lory J, Pompa JA, Kjaer I. The human mandibular canal arises from three separate canals innervating different tooth groups. J Dent Res. 1996;75(8):1540–1544. doi:10.1177/00220345960750080401
5. von Arx T, Bornstein MM. The bifid mandibular canal in three-dimensional radiography: morphologic and quantitative characteristics. Swiss Dent J. 2021;131(1):10–28.
6. Valenzuela-Fuenzalida JJ, Cariseo C, Gold M, Díaz D, Orellana M, Iwanaga J. Anatomical variations of the mandibular canal and their clinical implications in dental practice: a literature review. Surg Radiol Anat. 2021;43(8):1259–1272. doi:10.1007/s00276-021-02708-7
7. Kang JH, Lee KS, Oh MG, et al. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci Dent. 2014;44(1):53–60. doi:10.5624/isd.2014.44.1.53
8. Venkatesh E, Elluru SV. Cone beam computed tomography: basics and applications in dentistry. J Istanb Univ Fac Dent. 2017;51(3 Suppl 1):S102–s121. doi:10.17096/jiufd.00289
9. Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg. 1983;41(3):177–179. doi:10.1016/0278-2391(83)90076-9
10. Sanchis JM, Peñarrocha M, Soler F. Bifid mandibular canal. J Oral Maxillofac Surg. 2003;61(4):422–424. doi:10.1053/joms.2003.50004
11. Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc. 1985;110(6):923–926. doi:10.14219/jada.archive.1985.0033
12. Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(1):e25–31. doi:10.1016/j.tripleo.2009.08.027
13. Orhan K, Aksoy S, Bilecenoglu B, Sakul BU, Paksoy CS. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: a retrospective study. Surg Radiol Anat. 2011;33(6):501–507. doi:10.1007/s00276-010-0761-y
14. Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T. Bifid mandibular canals: cone beam computed tomography evaluation. Dentomaxillofac Radiol. 2010;39(4):235–239. doi:10.1259/dmfr/66254780
15. de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16(2):387–393. doi:10.1007/s00784-011-0544-9
16. Claeys V, Wackens G. Bifid mandibular canal: literature review and case report. Dentomaxillofac Radiol. 2005;34(1):55–58. doi:10.1259/dmfr/23146121
17. Mizbah K, Gerlach N, Maal TJ, Bergé SJ, Meijer GJ. The clinical relevance of bifid and trifid mandibular canals. Oral Maxillofac Surg. 2012;16(1):147–151. doi:10.1007/s10006-011-0278-5
18. DeSantis JL, Liebow C. Four common mandibular nerve anomalies that lead to local anesthesia failures. J Am Dent Assoc. 1996;127(7):1081–1086. doi:10.14219/jada.archive.1996.0333
19. Lew K, Townsen G. Failure to obtain adequate anaesthesia associated with a bifid mandibular canal: a case report. Aust Dent J. 2006;51(1):86–90. doi:10.1111/j.1834-7819.2006.tb00406.x
20. Nortjé CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 1977;15(1):55–63. doi:10.1016/0007-117x(77)90008-7
21. Okumuş Ö, Dumlu A. Prevalence of bifid mandibular canal according to gender, type and side. J Dent Sci. 2019;14(2):126–133. doi:10.1016/j.jds.2019.03.009
22. Naitoh M, Katsumata A, Kubota Y, Hayashi M, Ariji E. Relationship between cancellous bone density and mandibular canal depiction. Implant Dent. 2009;18(2):112–118. doi:10.1097/ID.0b013e318198da7e
23. Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants. 1989;4(4):327–332.
24. Lindh C, Petersson A, Klinge B. Visualisation of the mandibular canal by different radiographic techniques. Clin Oral Implants Res. 1992;3(2):90–97. doi:10.1034/j.1600-0501.1992.030207.x
25. Zografos J, Kolokoudias M, Papadakis E. [The types of the mandibular canal] Oi typoi tou porou tou kato phatniakou neurou. Melete 700 panoramikon aktinographion. Hell Period Stomat Gnathopathoprosopike Cheir. 1990;5(1):17–20.
26. Fuentes R, Arias A, Farfán C, et al. Morphological variations of the mandibular canal in digital panoramic radiographs: a retrospective study in a Chilean population. Folia Morphol. 2019;78(1):163–170. doi:10.5603/FM.a2018.0058
27. Kuczynski A, Kucharski W, Franco A, Westphalen FH, De lima AA, Fernandes A. Prevalence of bifid mandibular canals in panoramic radiographs: a maxillofacial surgical scope. Surg Radiol Anat. 2014;36(9):847–850. doi:10.1007/s00276-014-1298-2
28. Miličević A, Salarić I, Đanić P, et al. Anatomical variations of the bifid mandibular canal on panoramic radiographs in citizens from Zagreb, Croatia. Acta Stomatol Croat. 2021;55(3):248–255. doi:10.15644/asc55/3/2
29. Rashsuren O, Choi JW, Han WJ, Kim EK. Assessment of bifid and trifid mandibular canals using cone-beam computed tomography. Imaging Sci Dent. 2014;44(3):229–236. doi:10.5624/isd.2014.44.3.229
30. Zhang YQ, Zhao YN, Liu DG, Meng Y, Ma XC. Bifid variations of the mandibular canal: cone beam computed tomography evaluation of 1000 Northern Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;126(5):e271–e278. doi:10.1016/j.oooo.2018.06.008
31. Dedeoglu N, Duman S. Prevalence of bifid mandibular canals in Turkish Eastern Anatolia population: a retrospective study. J Clin Diagn Res. 2020;14:13–17. doi:10.7860/JCDR/2020/42721.13508
32. Muinelo-Lorenzo J, Suárez-Quintanilla JA, Fernández-Alonso A, Marsillas-Rascado S, Suárez-Cunqueiro MM. Descriptive study of the bifid mandibular canals and retromolar foramina: cone beam CT vs panoramic radiography. Dentomaxillofac Radiol. 2014;43(5):20140090. doi:10.1259/dmfr.20140090
33. Villaça-Carvalho MF, Manhães LR
34. Zhou X, Gao X, Zhang J. Bifid mandibular canals: CBCT assessment and macroscopic observation. Surg Radiol Anat. 2020;42(9):1073–1079. doi:10.1007/s00276-020-02489-5
35. Qaid N, Aldilami A, AL-Jawfi K, Shamala A. Prevalence and morphological assessment of bifid mandibular canal using cone beam computed tomography among a group of yemeni adults. Original Article. J Indian Acad Oral Med Radiol. 2021;33(3):242–247. doi:10.4103/jiaomr.jiaomr_218_20
36. Yang X, Lyu C, Zou D. Bifid mandibular canals incidence and anatomical variations in the population of shanghai area by cone beam computed tomography. J Comput Assist Tomogr. 2017;41(4):535–540. doi:10.1097/rct.0000000000000561
37. Nithya J, Aswath N. Assessing the prevalence and morphological characteristics of bifid mandibular canal using cone-beam computed tomography - a retrospective cross-sectional study. J Clin Imaging Sci. 2020;10:30. doi:10.25259/jcis_67_2019
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
