Back to Journals » Clinical Ophthalmology » Volume 16
Prevalence and Behavioral-Based Risk Factors (Eye Cosmetic and Tobacco Use) of Symptomatic Dry Eye Disease in Four Middle Eastern Countries: Lebanon, Syria, Jordan, and Palestine
Authors Ghach W, Bakkar MM, Aridi M, Beshtawi I, Doughaily R, Al-Fayoumi N
Received 11 August 2022
Accepted for publication 19 October 2022
Published 21 November 2022 Volume 2022:16 Pages 3851—3860
DOI https://doi.org/10.2147/OPTH.S385040
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wissam Ghach,1,2 May M Bakkar,3 Mona Aridi,4 Ithar Beshtawi,5 Rita Doughaily,2 Noha Al-Fayoumi6
1Faculty of Communication, Arts and Sciences, Canadian University Dubai (CUD), Dubai, United Arab Emirates; 2School of Health Sciences, Modern University for Business and Science (MUBS), Damour, Lebanon; 3Faculty of Applied Medical Sciences, Jordan University of Science and Technology, Irbid, Jordan; 4School of Computer and Applied Sciences, Modern University for Business and Science (MUBS), Damour, Lebanon; 5Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine; 6Ibn Al-Nafees Hospital, Damascus, Syria
Correspondence: Wissam Ghach, School of Health Sciences, Modern University for Business and Science (MUBS), Damour, Lebanon, Tel +9615601801, Fax +9615601667, Email [email protected] Mona Aridi, School of Computer and Applied Sciences, Modern Universityfor Business and Science (MUBS), Damour, Lebanon, Tel +9615601801, Fax +9615601667, Email [email protected]
Purpose: To estimate the prevalence of symptomatic dry eye disease (DED) in four Middle Eastern Countries and investigate the association between behavioral-based risk factors and severity of DED.
Patients and Methods: Population-based cross-sectional study of 1463 participants from 4 Mediterranean countries (Lebanon, Syria, Jordan, and Palestine). The Arabic version of the Ocular Surface Disease Index (ARB-OSDI) questionnaire was used to estimate the prevalence and severity of symptomatic DED using an online format survey. The survey also included demographic questions and possible behavioral risk factors (tobacco and cosmetic use). One-Way ANOVA and multivariate regression analyses were used to investigate the association between OSDI mean scores and behavioral-based risk factors.
Results: The prevalence of symptomatic DED (OSDI score ≥ 13) among the overall population (332 males and 1132 females) reached 70.2%. Tobacco and cosmetic users reported a higher significant prevalence and severity of symptomatic DED than non-users (p < 0.0001). Smoking habits (eg, smoking cigarettes or Ajami, smoking in closed areas, and daily smoking) were more likely to report symptomatic DED. Bad hygiene process during the use of any cosmetic product was behind the high prevalence and severity of symptomatic DED among the females of the study population.
Conclusion: Symptomatic DED is substantial in Middle Eastern countries. It is statistically associated with cosmetic and tobacco use.
Keywords: eye dryness, Ocular Surface Disease Index, smoking, cosmetic use, middle east
Introduction
The Tear Film and Ocular Surface Society-Dry Eye Workshop II (TFOS DEWS II) defines dry eye disease (DED) as a
Multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.1
Several eye epidemiological studies revealed that the prevalence of DED is increasing globally whereas Asian and Arab countries registered the highest estimation.2–4 Among the Middle Eastern countries, West Bank- Palestine (69%), the Eastern Province of Saudi Arabia (62.4%) and Jordan (59%) showed the highest estimation of symptomatic DED.5–7 These epidemiological studies were alarming enough to highlight the possible relation between DED prevalence and the geographical area where the climate conditions and behavioral habits (eg, Tobacco and cosmetic use) are approximately similar.
Focusing on tobacco use, direct contact with the irritative smoke may lead to defects in ocular surface defense and retinal nerve fiber layer.8,9 Exposure to smoke toxicants may also affect the tear film secretion and stability as well as reduce blood flow or increase the formation of clots within ocular capillaries, which could limit the delivery of vital nutrients for eye health.10 Even though smokers are highly exposed to smoke irritants, a contradictive relationship between DED and smoking was concluded in 25 countries including Lebanon, Jordan, and Palestine.5,6,11,12 Additionally, limited studies had investigated the relationship of DED prevalence with the types of smoked tobacco (eg, cigarette, waterpipe).11,13
Additionally, the exposure to irritating toxicants in behavioral habits is not limited to smoking. As known, females predominantly use eye cosmetics to enhance their attractiveness and to improve self-confidence by intensifying the beauty of their eyes.14 According to the epidemiological review, females record consistently higher DED percentages than males.1 Even though the literature reported that toxicants in eye cosmetics may lead to discomfort, inflammation, oxidative stress, and tear film change,15–17 limited studies investigated the association between eye cosmetics and the perception of ocular discomfort and the reduction in the tear film lipid layer thickness.18,19 Additionally, no study has investigated the association between the prevalence of DED and cosmetic use among Arabic females who are well-known for their excessive use of eye cosmetics (eg, Kohl).20
An association study between the prevalence of symptomatic DED and behavioral habits (eye cosmetics and tobacco use) in Lebanon, Syria, Jordan, and Palestine is necessary to foster awareness about symptomatic DED and its associated risk factors. In the current study, an Arabic version of the OSDI (ARB-OSDI) questionnaire was utilized to assess quantitatively the prevalence of symptomatic DED and investigate behavioral-based risk factors (Eye cosmetics and Tobacco Use) in the four neighboring Middle Eastern countries.
Materials and Methods
The population was recruited from Lebanon, Syria, Jordan, and Palestine between March 2021 and December 2021 using the convenience sampling. A total of 1463 participants (aged ≥ 18) were asked to participate in this non-clinical cross-sectional study using an online version of the questionnaire distributed throughout several online platforms. Participants with eye surgeries, active ocular diseases, and ocular or systemic medications that are known to interfere with tear film production or ocular surface integrity were excluded from the study.6,11
Study Tool
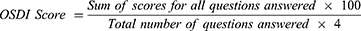
The ARB-OSDI utilized in the current study is a validated Arabic version of the OSDI questionnaire on dry eye symptoms induced by environmental factors over the preceding week.21 The OSDI questionnaire was originally developed by the Outcomes Research Group at Allergan Inc. (Irvine, California) and was designed to provide a rapid assessment of symptoms related to ocular irritation and dry eye disease.22 The 12-item OSDI questionnaire is three sections: 5 questions related to the ocular symptoms, 4 questions related to vision-related function, and 3 questions related to the environmental triggers. Each item was graded on a scale of 0 to 4 ranging from none of the time to all of the time. The OSDI score was then calculated according to the following formula:
In the current study, the OSDI status was classified with a cut-off value of OSDI score ≥ 13 between normal status and DED status (mild, moderate, and severe).23,24 The measurement scale of the OSDI status was divided into three intervals: the interval of normal cases [0, 12], the interval of mild-to-moderate cases [13, 32], and the interval of severe cases [33, 100].23,24
The risk factor of tobacco exposure was assessed through questions related to the types of tobacco used eg, regular cigarette, electronic cigarette, Mouassal waterpipe (an Arabic translation for “honeyed” which contains 30% tobacco and around 70% honey/sugarcane as well as glycerol and flavor) and Tumbak or Ajami (an Arabic translation for “non-honeyed” pure dark paste of tobacco),25 indoor-outdoor smoking areas, rate of smoking (daily, weekly, and monthly), quantification of cigarettes or waterpipes per week along with the smoking duration (in years).
The risk factor of cosmetic exposure was assessed through questions related to the type of eye makeup (mascara, eyeliner, eyeshadow, eyelashes, and anti-aging cream), rate of makeup use (daily, weekly, and monthly) along with application hours per day, and cleaning methods (water, soapy water, cleansing products) along with the rate of night cleansing (never, sometimes, always). The overall study tool is provided in the Supplementary Information.
Data Analysis
The data were analyzed using the Statistical Package for the Social Sciences, version 21 (SPSS, International Business Machine Corp. IBM, Chicago, IL, USA). The prevalence of symptomatic DED in the participants was determined by the percentage of the population with OSDI score ≥ 13 (mild, moderate, and severe OSDI status). The significant differences between variables were evaluated using the multivariate regression analysis and the One-way ANOVA tests.
Ethical Considerations
The Institutional Review Board (IRB) at the Modern University for Business and Science (MUBS) has reviewed and approved the protocol of the study (MU - 20210323-22E). The study was conducted according to the principles contained in the Declaration of Helsinki. Informed consent was obtained from all the participants prior to their participation in the study. Confidentiality and absence of potential risk were controlled during data collection and analysis.
Results
In this study, a total of 1463 persons participated from four Middle Eastern countries. The highest participation rate was from Palestine (576 respondents: 39.4%) and Jordan (508 respondents: 34.7%) while the Syrian and Lebanese people showed the lowest rate(115 respondents: 7.9%; 264 respondents: 18%, respectively) (Table 1). The majority of the respondents were females from all the participating countries (1132 females; 77.4%). Except for Syria, almost half of the study population (814 respondents; 55.6%) belonged to the young age group (18–24 years old). Looking at the participants’ habits, the prevalence of smoking and makeup use habits was high in the study population (65.6% and 66.1%, respectively) with comparable results among the four study countries.
DED Comparison Among the Four Countries
According to Table 1, the prevalence of symptomatic DED in the studied countries was relatively high where 70.5% of the studied population showed symptoms of mild-to-severe DED (OSDI score was ≥ 13). Among the four countries, the highest prevalence of symptomatic DED (OSDI score ≥ 13) and DED severity (represented by mean OSDI scores) was distinguished in the Jordanian respondents (73.4%; mean score =31.5). The F-value is 7.64 (p-value < 0.0001), which indicates a statistically significant difference between the mean OSDI scores of the four countries as demonstrated by the One-Way ANOVA test. Additionally, the Tukey Post Hoc test showed that Jordan has an OSDI mean score higher than each of the other three countries (p-value < 0.001).
DED and Tobacco Use
In the current study, smoking factors such as rate, duration (in years), types, and areas of smoking were investigated as shown in Table 2. Of the study population, smokers demonstrated a 3 times higher prevalence of symptomatic DED (OSDI score ≥ 13) and 4.75 times higher DED severity (represented by mean OSDI scores) than the non-smokers. The highest prevalence of symptomatic DED (OSDI scores ≥ 13) was recorded among the smokers of Ajami tobacco compared to those who smoked other types. On the other hand, the highest DED severity (represented by mean OSDI scores) was recorded among mixed tobacco smokers.
 |
Table 2 OSDI Status, Mean Scores (Standard Deviation), One-Way ANOVA, and Distribution of Responses (Relative Percentages) with Respect to Smoking Types, Rates, and Areas |
Smoking rate (daily, weekly, monthly) did not show a perfect harmonic relation with the symptomatic DED (prevalence and severity). Except for respondents who smoked weekly, all the other groups were consistent with the expectation that the prevalence of symptomatic DED (OSDI scores ≥ 13) increases with the regular consumption of tobacco (Daily = 95.2% > Monthly = 78.2% > No smoking = 30.6%). Expectedly, the highest DED severity (represented by mean OSDI scores) was recorded among the daily smokers (OSDI mean score = 41).
Smoking areas (indoor or outdoor) revealed a better harmonic relation with the symptomatic DED (prevalence and severity). Expectedly, the highest prevalence of symptomatic DED (94.5% of the participants recorded OSDI scores ≥ 13) and DED severity (mean OSDI score = 43.3) was recorded among indoor smokers (where bad ventilation areas are expected) compared to outdoor smokers and non-smokers.
The One-Way ANOVA test showed a considerable statistical significance among DED severity (represented by OSDI mean scores) and all the studied factors of tobacco use (p < 0.001) as represented in Table 2. Additionally, Spearman correlation tests showed a strong negative correlation between the DED severity, smoking rate (rho = −0.670, P-value < 0.0001) and smoking areas (rho = −0.673, P-value < 0.0001).
To investigate the relationship between smoking and the OSDI score, a multiple regression analysis was carried out to test whether there is a linear relationship between the dependent variable, the OSDI score (Y), and the independent variables, the number of smoking years (X1), the number of cigarettes smoked (X2), and the number of water pipes smoked (X3) on weekly basis (Table 3). According to the multiple regression test, 43.7% of the DED variance was linked to independent variables (X1), (X2), and (X3) which confirms the association hypothesis of DED prevalence with smoking, specifically the duration, and frequency of smoking (cigarette or waterpipe). Also, the coefficient of the regression model (OSDI Score (Y) = 13.33 + 1.138X1+ 0.143X2 + 1.665X3) indicated that smoking water pipe has more contribution to the OSDI score (X3 by a factor of 1.665) than smoking cigarettes (X2 by a factor of 0.143) during the long-term smoking (X1 by a factor of 1.138). On the other hand, the standardized coefficients indicated that cigarette smoking has a considerable impact on DED where its standardized coefficient (0.381) recorded the highest value among the other two independent variables. The impact of waterpipe smoking came in the second place with a standardized coefficient value of (0.324), whereas, the effect of smoking years on DED came in the third place with a standardized coefficient of (0.242). As a result, both regression and correlation tests confirmed that the higher the rate of smoking tobacco, the higher the prevalence of symptomatic DED (OSDI scores ≥ 13).
 |
Table 3 Multivariate Regression Results Analysis for OSDI Scores on the Basis of the Number of Smoking Years, Smoked Cigarettes, and Waterpipes per Week |
DED and Eye Cosmetics Use
Eye cosmetics usage is a common tradition and whilst some products are utilized in proximity to the ocular surface, the current study also aimed to investigate the use of eye cosmetics among 1132 females (males were excluded in this section) and identify any association between symptomatic DED (prevalence and severity) and cosmetic usage (eg the factors of rate; duration in hours); type; cleaning techniques and rates). The results are summarized in Table 4.
Regardless of the groups of cosmetics, cosmetics users demonstrated a higher prevalence of symptomatic DED (OSDI score ≥ 13), in which these percentages ranged between 77.5-and 85.1% than the non-cosmetics users (69.3% of the participants recorded OSDI scores ≥13). Expectedly, all the users of cosmetics recorded higher DED severity (represented by mean OSDI scores) than non-users. The highest prevalence of symptomatic DED (OSDI scores ≥ 13) and DED severity (represented by mean OSDI scores) was recorded among the users of eyeliner internally (84.4%; mean score = 38.4) and mascara (85.1%; mean score = 38.1) compared to those who utilized other types of eye cosmetics.
As opposed to the factors of cosmetic usage rate (daily, weekly, monthly) and duration of cosmetic wear (D < 6 hours, 6 < D < 12 hours, D > 12 hours), the cosmetics cleaning protocol (material and rate) revealed a better harmonic relation with the symptomatic DED (prevalence and severity) as represented in Table 4. Expectedly, the lowest prevalence of symptomatic DED (OSDI scores ≥ 13) and OSDI severity (represented by mean OSDI scores) was recorded among the makeup users who remove regularly their eye makeup before sleep (74.9%; mean score = 30.3) and who use cleansing creams for makeup removal (72.6%; mean score = 28.8) compared to those who did not remove their eye makeup regularly or who cleaned their eye makeup with either water or soapy water.
Finally, the One-Way ANOVA test showed a considerable statistical significance among DED severity (represented by OSDI mean scores) and all the studied factors of cosmetic use (p < 0.001) as represented in Table 4.
Discussion
In agreement with the literature on DED prevalence among the Arab population, the average estimation of DED prevalence is relatively high (70.2%) with high ranging percentages (65.2–73.4%) among the studied countries.4,26 The high prevalence in the Arab countries could be associated with the high prevalence of rheumatoid arthritis, diabetes mellitus, and the heavy use of age-related systemic and topical medications in elderly people.4 Additionally, the population of the Middle Eastern countries is identified with poor education concerning DED, irregular follow-up, high proportions of contact lens use along with some environmental factors (eg, heavy use of air conditions, hot weather, excessive use of electronic devices, fine particulate pollution, and corrosive air salts due to proximity of countries to the sea).26 As being Middle Eastern countries (also Arab) with similar climate features, Lebanon, Syria, Jordan, and Palestine were chosen for this study to minimize the interference of environmental risk factors in the study findings.27
Evolution of DED Among the Studied Countries
The comparison of the current finding with the previous DED studies showed an increase in the prevalence of symptomatic DED in Lebanon (from 36.4% to 62.5%), Jordan (from 59% to 73.4%), and Palestine (from 69% to 72.7%).5,6,11 On the other hand, this study showed the first estimation of DED prevalence in Syria (65.2%). This increase in DED estimation could be explained by the shifting of people’s behavior towards heavy use of digital devices for remote learning/working and/or the continuous wearing of masks during the spread of the COVID-19 pandemic.28,29 To neutralize the variation of COVID interference among the four countries and to enlarge the sample population in the next section of the discussion, the respondents from the four countries were merged into one study population from the Middle East.
Symptomatic DED and Smoking
Lebanon, Syria, Jordan, and Palestine recorded high rates of smoking (53.9%, 34.8%, 38.1%, and 39.7%, respectively) in the MENA region.30,31 For that, several types of tobacco such as Mouassal waterpipe, Ajami waterpipe, regular cigarette, and e-cigarette were investigated in the current association study with DED. According to the literature about tobacco, water pipes may have higher amounts of irritants (ie, Nicotine, Heavy metals, Carbon monoxide (CO), Polycyclic aromatic hydrocarbons (PAHs)) and generate more aerosols (puff smoke) than cigarettes.32–34 However, the moisturized puffs in the waterpipe could be less irritating particularly upon dilution with water.35 The latter would explain why cigarette smokers had more DED severity (higher OSDI mean score) than waterpipe smokers. On the other hand, the low DED severity among e-cigarette smokers confirmed the hypothesis that e-cigarettes contain fewer toxicants than other types of tobacco.36 Among waterpipes, the low DED severity among Mouassal tobacco users could be explained by the features of tobacco in producing 30–40% less CO when mixed with molasses.37
The current study focused on the ocular exposure to the irritative aerosols of tobacco based on the assumption that the ocular surface may be exposed to over 1014 short‐lived radicals through the gas-tar phases of the puff smoke. The radicals in the puff smoke may increase the risk of lipid peroxidation of the outer layer of the pre-corneal tear film and eventually dry eye symptoms.38 The complexity (over 7000 chemicals), formulations (tobacco brands) and the variability of waterpipe use (size of waterpipe, level of water, amount of tobacco in the waterpipe head, and the type of coal) are limiting factors for finding justification.10,13,37,39 Regardless of the types of tobacco, indoor and frequent smoking could lead to a high risk of DED where smokers will be exposed to cumulative levels of aerosol irritants in the absence of an effective ventilation system.40 When people smoke every day, they are continuously exposed to the irritants of tobacco which in turn could increase the risk of diagnosis with DED.
Symptomatic DED and Cosmetic Use
Contrary to smoking, all types of cosmetic types recorded a comparable relationship with DED prevalence whereas Eyeliner (internally) and mascara users recorded the highest DED prevalence and severity. Here, their proximity and migration across the eyelid margin may increase the risk of their accidental exposure and thereby could explain the finding with either tear-film instability and/or corneal epithelium inflammation.17 During frequent use of eye makeup, the lipophilic constituents of the formulations may also diffuse through the surface lipid layer and accumulate at the lipid-aqueous interface to reduce the stability of the overlying tear film layer.41 Besides, the water-based formulations (eg, eyeliner and mascara products) provide a high risk of ocular irritation caused by Demodex mites which survive in cosmetic products or applicators and have a high affinity toward oil-rich environments (tear lipid film).16
As known, eye hygiene is necessary to reduce the risk of chemical overexposure and microbial contamination during the continuous use of cosmetics. Due to the lipophilicity of the formulations, water (lipophobic) alone will not effectively remove the eye makeup.16 This would explain why worse DED prevalence and severity were recorded among respondents who used water alone or with soap as alternatives to surfactant-containing cleaners. Regardless of the possible association of these cleansing products with tear film instability, makeup removal products (slightly basic PH value ≈ 7.3–7.4) provide a better cleansing effect (eg, waterproof products) with less risk of eye irritation than regular soaps (more basic PH values > 9)).17,42
Strength and Limitations
The current study has investigated the first association data of symptomatic DED with tobacco and cosmetic use among four Middle Eastern countries (Lebanon, Syria, Jordan, and Palestine). The outcome of this study could provide their Ministries of Public Health and the medical research institutions with evidence regarding behavioral-based risk factors of DED to be a guiding platform for further investigations into DED. In addition, public health specialists, ophthalmologists, and optometrists could utilize these data to implement SDG3-based programs to spread awareness of DED and its associated factors among these populations. However, some limitations in the design of this study should be noted. The study findings relied only on an online self-responding questionnaire where some responding bias or social desirability could affect these findings. Also, the findings depended solely on the subjective analysis which could be consistent or not with the clinical signs.43 Thus, additional studies are recommended to assess clinically the occurrence of DED signs among these populations and investigate its association with tobacco and cosmetic use.
Conclusion
Almost three-quarters of the studied population had been diagnosed with symptomatic DED assessed with the validated ARB-OSDI survey. Jordan and Palestine had recorded the highest prevalence of symptomatic DED compared to Lebanon and Syria. This paper has clearly shown that cosmetic usage and tobacco smoking are significantly associated with the prevalence and severity of symptomatic DED (P < 0.05). In tobacco use; cigarettes, Ajami, indoor and daily smokers were more likely to report the symptomatic DED. Regardless of cosmetic types and frequency, users were more likely to report the symptomatic DED when eye hygiene was not effectively considered. The study provides a valuable platform for prospective studies on the evolution of DED in Middle Eastern countries.
Abbreviations
DED, dry eye disease; OSDI, Ocular Surface Disease Index; MENA, the Middle East and North Africa.
Acknowledgments
This work was supported by the Modern University for Business and Science (MUBS).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.008
2. Tsubota K, Yokoi N, Watanabe H, et al. A new perspective on dry eye classification: proposal by the Asia dry eye society. Eye Contact Lens. 2020;46(January):S2–S13. doi:10.1097/ICL.0000000000000643
3. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334–365. doi:10.1016/j.jtos.2017.05.003
4. Aljarousha MA, Badarudin NE, Che Azemin MZ, Aljeesh Y, Abuimara A. A systematic review on prevalence, risk factors, clinical diagnosis and medical management of dry eye disease in the Arab population. Afr Vis Eye Health. 2021;80(1):591.
5. Shanti Y, Shehada R, Bakkar MM, Qaddumi J. Prevalence and associated risk factors of dry eye disease in 16 northern west bank towns in Palestine: a cross-sectional study. BMC Ophthalmol. 2020;20(1):1–8. doi:10.1186/s12886-019-1277-9
6. Bakkar MM, Shihadeh WA, Haddad MF, Khader YS. Epidemiology of symptoms of dry eye disease (DED) in Jordan: a cross-sectional non-clinical population-based study. Cont Lens Anterior Eye. 2016;39(2015):1–6. doi:10.1016/j.clae.2016.01.003
7. Alharbi A, Alanazi N, Alhamad J, et al. Prevalence of symptomatic dry eye and its risk factors among coastal population in eastern province of Saudi Arabia. J Clin Exp Ophthalmol. 2018;9:34.
8. Satici A, Bitiren M, Ozardali I, Vural H, Kilic A, Guzey M. The effects of chronic smoking on the ocular surface and tear characteristics: a clinical, histological and biochemical study. Acta Ophthalmol Scand. 2003;81(6):583–587. doi:10.1111/j.1395-3907.2003.00158.x
9. Narnoli P, Dhasmana R, Khanduri R. Dry eye disease and retinal nerve fiber layer changes in chronic smokers. Indian J Ophthalmol. 2021;69(5):1178. doi:10.4103/ijo.IJO_976_20
10. Thomas J, Jacob GP, Abraham L, Noushad B, Jacob GP. The effect of smoking on the ocular surface and the precorneal tear film. Australas Med J. 2012;5(4):221–226. doi:10.4066/AMJ.2012.1035
11. Sherry A, Aridi M, Ghach W. Prevalence and risk factors of symptomatic dry eye disease in Lebanon. Cont Lens Anterior Eye. 2020;43(4):355–358. doi:10.1016/j.clae.2019.08.001
12. Tariq MA, Amin H, Ahmed B, Ali U, Mohiuddin A. Association of dry eye disease with smoking: a systematic review and meta-analysis. Indian J Ophthalmol. 2022;70(6):1892–1904. doi:10.4103/ijo.IJO_2193_21
13. Bakkar MM, Haddad MF, Khabour OF. The effects of tobacco waterpipe smoking on the ocular surface. Clin Exp Optom. 2022;105:1–7.
14. Mulhern R, Fieldman G, Hussey T, Lévêque J, Pineau P. Do cosmetics enhance female caucasian facial attractiveness? Int J Cosmet Sci. 2003;25(4):199–205. doi:10.1046/j.1467-2494.2003.00188.x
15. Yazdani M, Elgstøen KBP, Utheim TP. Eye make-up products and dry eye disease: a mini review. Curr Eye Res. 2022;47(1):1–11. doi:10.1080/02713683.2021.1966476
16. Ng A, Evans K, North RV, Jones L, Purslow C. Impact of eye cosmetics on the eye, adnexa, and ocular surface. Eye Contact Lens Sci Clin Pract. 2016;42(4):211–220.
17. Craig JP, Wang MTM, Craig JP. Investigating the effect of eye cosmetics on the tear film: current insights. Clin Optom. 2018;10:33.
18. Ng A, Evans K, North R, Purslow C. Eye cosmetic usage and associated ocular comfort. Ophthalmic Physiol Opt. 2012;32(6):501–507. doi:10.1111/j.1475-1313.2012.00944.x
19. Franck C. Fatty layer of the precorneal film in the ‘office eye syndrome. Acta Ophthalmol. 1991;69(6):737–743.
20. Hardy AD, Walton RI, Myers KA, Vaishnav R. Availability and chemical composition of traditional eye cosmetics (“kohls”) used in the United Arab Emirates of Dubai, Sharjah, Ajman, Umm Al-Quwain, Ras Al-Khaimah, and Fujairah. J Cosmet Sci. 2006;57(2):107–125.
21. Bakkar MM, El-Sharif AK, Al Qadire M. Validation of the Arabic version of the ocular surface disease index questionnaire. Int J Ophthalmol. 2021;14(10):1595. doi:10.18240/ijo.2021.10.18
22. Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615–621. doi:10.1001/archopht.118.5.615
23. Grubbs JR, Tollesson-Rinehar S, Huynh K, Davis RM. A review of quality of life measures in dry eye questionnaires. Cornea. 2014;33(2):215–218. doi:10.1097/ICO.0000000000000038
24. Prokopich CL, Bitton E, Caffery B, et al. Screening, diagnosis and management of dry eye disease: practical guidelines for Canadian optometrists. Can J Optom. 2015;76(suppl 1):4–26. doi:10.13140/RG.2.1.2788.4963
25. Qasim H, Alarabi AB, Alzoubi KH, Karim ZA, Alshbool FZ, Khasawneh FT. The effects of hookah/waterpipe smoking on general health and the cardiovascular system. Environ Health Prev Med. 2019;24(1):58. doi:10.1186/s12199-019-0811-y
26. Al-Maskari AZ, Alarfaj K, Shaheen MS, et al. Middle east preferred practice patterns for dry eye disease: a modified delphi consensus. Open Ophthalmol J. 2021;15:1.
27. Climate Center. Middle east - climate fact sheet; 2021. Available from: https://www.climatecentre.org/wp-content/uploads/RCCC-ICRC-Country-profiles-Region_Middle_East.pdf.
28. Yousef S. Visual display and dry eye related symptoms among medical students during corona virus waves. Med J Cairo Univ. 2021;89(12):2909–2913. doi:10.21608/mjcu.2021.225227
29. Marinova E, Dabov D, Zdravkov Y. Ophthalmic complaints in face-mask wearing: prevalence, treatment, and prevention with a potential protective effect against SARS-CoV-2. Biotechnol Biotechnol Equip. 2020;34(1):1323–1336. doi:10.1080/13102818.2020.1838323
30. Abdulrahim S, Jawad M. Socioeconomic differences in smoking in Jordan, Lebanon, Syria, and Palestine: a cross-sectional analysis of national surveys. PLoS One. 2018;13(1):1–11. doi:10.1371/journal.pone.0189829
31. Khattab A, Javaid A, Iraqi G, et al. Smoking habits in the middle east and North Africa: results of the BREATHE study. Respir Med. 2012;106:S16–S24. doi:10.1016/S0954-6111(12)70011-2
32. Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005;116(1):e113–e119. doi:10.1542/peds.2004-2173
33. Yadav S, Rawal G. Waterpipe tobacco smoking: a mini-review. J Transl Intern Med. 2018;6(4):173–175. doi:10.1515/jtim-2016-0013
34. Daher N, Saleh R, Jaroudi E, et al. Comparison of carcinogen, carbon monoxide, and ultrafine particle emissions from narghile waterpipe and cigarette smoking: sidestream smoke measurements and assessment of second-hand smoke emission factors. Atmos Environ. 2009;44(1):8–14. doi:10.1016/j.atmosenv.2009.10.004
35. Chaouachi K. Hookah (Shisha, Narghile) smoking and environmental tobacco smoke (ETS). A critical review of the relevant literature and the public health consequences. Int J Environ Res Public Health. 2009;6(2):798–843. doi:10.3390/ijerph6020798
36. Callahan-Lyon P. Electronic cigarettes: human health effects. Tob Control. 2014;23((SUPPL):2. doi:10.1136/tobaccocontrol-2013-051470
37. Shihadeh A, Eissenberg T. Tobacco Smoking Using a Waterpipe: Product, Prevalence, Chemistry/ Toxicology. Pharmacological Effects, and Health Hazards; 2005.
38. Frei B, Forte TM, Ames BN, Cross CE. Gas phase oxidants of cigarette smoke induce lipid peroxidation and changes in lipoprotein properties in human blood plasma. Protective effects of ascorbic acid. Biochem J. 1991;277(1):133–138. doi:10.1042/bj2770133
39. FDA. Cigarettes; 2022. Available from: https://www.fda.gov/tobacco-products/products-ingredients-components/cigarettes.
40. Alsaqr A, Masmali A, Fagehi R, et al. Ocular dryness assessment in Saudi employees working indoors and outdoors. Clin Optom. 2018;10:51–56. doi:10.2147/OPTO.S163303
41. Malik A, Claoué C. Transport and interaction of cosmetic product material within the ocular surface: beauty and the beastly symptoms of toxic tears. Cont Lens Anterior Eye. 2012;35(6):247–259. doi:10.1016/j.clae.2012.07.005
42. Maudgal PC. Ocular burn caused by soft brown soap. Bull Soc Belge Ophtalmol. 1996;263:81–84.
43. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539–574. doi:10.1016/j.jtos.2017.05.001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.