Back to Journals » Clinical Ophthalmology » Volume 17
Prevalence and Associated Factors of Ocular Manifestations of Acquired Immune Deficiency Syndrome Among Adults at University of Gondar Hospital, North West Ethiopia, 2021
Authors Aragaw BB , Alemu HW , Assaye AK , Belete YA , Alemayehu HB
Received 18 February 2023
Accepted for publication 2 May 2023
Published 9 May 2023 Volume 2023:17 Pages 1323—1333
DOI https://doi.org/10.2147/OPTH.S406837
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr John B Miller
Birhanu Belete Aragaw,1 Haile Woretaw Alemu,2 Aragaw Kegne Assaye,2 Yared Ayelign Belete,1 Henok Biruk Alemayehu1
1Department of Ophthalmology and Optometry, School of Medicine, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia; 2Department of Optometry, School of Medicine, College of Medicine and Health Sciences University of Gondar, Gondar, Ethiopia
Correspondence: Birhanu Belete Aragaw, Tel +251923701934, Email [email protected]
Introduction: Acquired immune deficiency syndrome is a disease with common clinical ocular manifestations. Ocular manifestations lead to blindness, which has a common social and economic impact.
Purpose: This study aimed to assess the prevalence and associated factors of ocular manifestations of acquired immune deficiency syndrome among adults at the University of Gondar Hospital, North West Ethiopia, 2021.
Patients and Methods: A cross-sectional study was conducted on 401 patients from June to August 2021. Samples were selected based on a systematic random sampling technique. Data collection was done using structured questionnaires. Data extraction format was used to collect the clinical characteristics of patients including ocular manifestations. Data entry was done by EpiData version 4.6.0.6 and exported to the Statistical Package for the Social Sciences version 26 for data analysis. Associated factors were analyzed by binary logistic regression. P-value < 0.05 with a 95% confidence level was used to declare a significant association.
Results: A total of 401 patients were involved with a response rate of 91.5%. The overall prevalence of ocular manifestations of acquired immune deficiency syndrome was 28.9%. The common ocular manifestations were seborrheic blepharitis at 16.4% and squamoid conjunctival growth at 4.5%. Age > 35 years (AOR=2.52, 95% CI: 1.19, 5.35), Clusters of differentiation 4 count < 200 cells/μL (AOR=4.76, 95% CI:2.50, 9.09), World Health Organization stage II (AOR=2.60, 95% CI: 1.23, 5.50), history of eye disease (AOR=3.05, 95% CI: 1.38, 6.72), and duration of Human Immunodeficiency Virus > 5 years (AOR=2.79, 95% CI: 1.29, 6.05) were statistically associated with the ocular manifestation of acquired immune deficiency syndrome.
Conclusion and recommendations: In this study, the prevalence of ocular manifestation of acquired immune deficiency syndrome was high. Age, CD4 count, duration of HIV, eye disease history, and WHO clinical staging were the significant factors. Early eye checkups and regular ocular examinations of HIV patients would be helpful.
Keywords: ocular manifestation, HIV/AIDS, Gondar, Ethiopia
Introduction
Acquired immune deficiency syndrome (AIDS) is the most common cause of death in many parts of the United States, Europe, and sub-Saharan Africa.1 Globally, 38.4 million people were living with Human Immune Virus (HIV) and from those 28.7 million were accessing antiretroviral therapy (ART) in 2021.2 In eastern and southern Africa, 20.6 million people live with the virus.2 In sub-Saharan Africa, more than 16 million people have been negatively affected by the spread of infectious diseases.3 Ethiopia has the lowest prevalence rate of HIV/AIDS in East Africa. There are more than one million people who have the virus and are surviving with it.4
Ocular manifestations of HIV infection have been common worldwide. Globally, 70–80% of the people with HIV have been treated for an eye condition related to their HIV infection at some point during their illness.5 In the pre-Highly Active Antiretroviral Therapy (HAART) period, 50% to 75% of the HIV-infected individuals had HIV-related ocular problems.6 The total possibility that an HIV-positive person will have at least one abnormal ocular lesion (eye abnormality) over their lifetimes ranges from 52% to 57%.7
HIV-infected individuals presented with various ocular conditions that are directly attributed to HIV/AIDS and its effect on the human immune response.8,9 The disease can have an adnexal, anterior segment, posterior segment, orbital, and neuro-ophthalmic manifestations.10 Cytomegalovirus retinitis (CMV), Kaposi sarcoma, and squamous cell carcinoma remain the most common ocular disorder among HIV-infected population.8,11 The pattern of ocular conditions in HIV infection is related to the history of eye problems, WHO stage of HIV/AIDS, CD4 count, age, and duration of HIV/AIDS.8,10,12
People living with HIV/AIDS in developing countries who lose their vision typically have a short life expectancy.6 In developing countries, 5–25% of all the HIV patients become blind due to ocular complications of HIV/AIDS.13 HIV-related blindness has a significant impact, leading to a loss of economic independence, social standing, and family decision-making process, and productivity loss leads to a deterioration of quality of life.14,15
At present, antiretroviral therapy (ART) becomes more available in developing countries like Ethiopia; however, life expectancy and the prevalence of blindness related to HIV/AIDS are expected to go up.
Even though different studies have been done on the prevalence of ocular manifestations of HIV/AIDS in developing countries like Ethiopia, there is not much information about the factors associated with ocular manifestations in the study area. Therefore, the purpose of this study was to further determine the prevalence of ocular manifestation of HIV/AIDS and the associated factors among adult HIV patients.
Methods and Materials
Study Design, Setting, and Study Period
A hospital-based cross-sectional study was conducted among adult HIV patients attending at University of Gondar Comprehensive Specialized Hospital ART clinic from June to August 2021. Gondar Town is located 750 kilometers from the capital city of Ethiopia Addis Ababa. University of Gondar Comprehensive Specialized hospital is a tertiary health care center and teaching hospital. The hospital started offering (ART) service in 2005. At the beginning, more than 7500 adults were enrolled in care and counseling programs. Currently, the hospital is providing ART service for more than 5000 HIV patients.
Sample Size Calculation
The sample size for the first objective was 398 based on single population proportion formula using evidence from a study conducted in Ethiopia Gondar hospital,16 with the assumptions’=21.4% (p = 0.214) CI=95% and margin of error=4%.
For the second objective, the power approach, stat Calc (EPIinfo7) was used. Based on the reviewed literature, CD4 count and HAART use were the factors repeatedly associated with the ocular manifestation of HIV/AIDS. The sample size was determined based on the study conducted in Jimma, Ethiopia17 (Table 1).
 |
Table 1 Sample Size Calculation for the Second Objective |
By taking the largest of all, the final sample size was 438.
Sampling Technique
A systematic random sampling technique was used with an interval of 5 to select the study participants at ART clinic of University of Gondar Comprehensive Specialized hospital. Using a lottery method, a single number was taken from 1 to 5 to determine the first subject and continue with every fifth interval. There were 50 cases per day who visited the ART clinic. The interval was calculated by dividing the expected number of patients who attend to the center within 2 months by the total sample size (N=2000; n=438; K=(2000/438)=4.5=5).
Source and Study Population
All adult HIV patients who are receiving regular service at the University of Gondar Hospital ART clinic and patients attending during the data collection period.
Inclusion and Exclusion Criteria
All adult HIV patients attending at University of Gondar Hospital ART clinic were enrolled in the study, and patients who had additional medical problems of diabetes, hypertension, and ocular trauma were excluded from the study.
Operational Definition
CD4 count – CD4 count of the patients within the last 6 months during the data collection time.
Ocular manifestation of HIV/AIDS – If the patients had at least one of the following ocular findings: Herpes zoster ophthalmicus, CMV retinitis, HIV retinopathy, molluscum contagiosum, seborrheic blepharitis, ocular squamous neoplasia, and neuropthalmic disorder.10,13,18,19
Adnexal manifestations – Herpes zoster ophthalmicus, molluscum contagiosum and Kaposi’s sarcoma.19
Anterior segment manifestations – Ocular surface squamous neoplasia, seborrheic blepharitis.19
Posterior segment manifestations – Retinal microvasculopathy, CMV retinitis, or HIV retinopathy.19
Neuro-ophthalmic manifestations – Papilledema, optic neuritis, optic atrophy and cranial nerve palsy.19
Data Collection Procedure and Tools
A structured questionnaire was used to collect sociodemographic data. Selected patients were examined for possible HIV-related ocular problems. Visual acuity was taken by using the Snellen E- chart. External eye examination was done by torch and magnifying loop. The posterior segment was examined after dilation of the eye by using a direct ophthalmoscope. Data extraction format was used to record CD4 counts, viral load, WHO staging, HIV confirmation date from the medical record, and also the ocular findings.
Data Quality Control
Data were collected by three optometrists. To maintain the quality of the data, the recruited data collectors were trained about the aim of the study and how to retrieve data. Questioners were prepared from reviewed pieces of literature Jimma (Ethiopia),17 Jakarta (Indonesia),20 Ghana,21 South Korea,22 and Taiwan.23 Structured questionnaires were first prepared in English, then translated to Amharic and back-translated to English by an independent translator. A pretest test was done on 21 patients at Debre Tabor hospital to check the consistency and completeness of the data item. The data collection process was monitored by the investigator throw-out the data collection period. Completed questionnaires were checked regularly for completeness of the information. In addition, double-entry of data was done in about 5% of the data collected.
Data Processing and Analysis
Data were entered into EpiData version 4.6.0.6 and exported to IBM Statistical Package for the Social Sciences (SPSS) version 26 software for data analysis. Both descriptive and analytical statistical procedures were performed. Descriptive statistics were used for the presentation of sociodemographic data and prevalence of ocular manifestations. Tables and figures were used for the presentation of data. Binary logistic regression was used to identify associated factors for ocular manifestations of HIV/AIDS. Bivariable and multivariable binary logistic regression models were used. Variables with a p-value less than 0.25 at bivariable logistic regression were entered into a multivariable logistic regression to identify significant variables for the ocular manifestation of HIV/AIDS. A p-value of less than 0.05 with a 95% confidence interval was used to declare a significant association between variables. Model fitness was checked by using Hosmer and Lemeshow’s goodness of fit (p=0.45).
Ethical Considerations
Ethical clearance was obtained from the University of Gondar College of Medicine and Health Sciences Ethical Review Board (ERB 688/06/2021). A permission letter was also obtained from the clinical director of Gondar Hospital and the ART clinic focal person. The risks and benefits of the study were clarified for the patients. Written informed consent was also taken from study patients. Personal identifiers were not included to maintain confidentiality. This study also complies with the Declaration of Helsinki principles on medical research involving human subjects. The health, rights and confidentiality of the study subjects during the data collection were the first consideration and everything done during the data collection on study participants were on patient’s interest. Patients with ocular manifestations of HIV/AIDS were advised and linked to the eye clinic for further diagnosis and management.
Results
Sociodemographic Characteristics of Study Participants
A total of 401 study participants were involved in the study with a response rate of 91.55%. The majority 79.1% (317) of participants were in the age group >35 years, with a median age of 45 and interquartile range (IQR, 37–50 years). More than half of 65.1% (261) were female participants. About 93.8% (376) were urban residents and 29.4% (118) of patients had a secondary school education level. About 35.9% (144) were housewives and 42.9% (172) of participants were married (Table 2).
 |
Table 2 Sociodemographic Characteristics of Study Participants Among Adult HIV Patients in Gondar University Comprehensive Specialized Hospital ART Clinic, 2021 |
Clinical Profile of Study Participants
Of the total 401 participants, the majority (98.5%) of them had received HAART. About 83.8% of the patients had CD4+ count ≥200 cells/µL with interquartile range (IQR, 264–585.50 cells/µL). No single participant was in WHO clinical stage IV, while 11.5% (46) of the participants were in WHO clinical stage II. Most (99%) of the patients had a viral load lower than 10,000. The majority 70.8% (284) of them had no history of eye disease and only 86 (21.4%) of patients had an eye checkup history. The prevalence of visual impairment was 13.96% (Table 3).
 |
Table 3 Clinical Profiles of Adult HIV Patients Attending at University of Gondar Comprehensive Specialized Hospital ART Clinic, 2021 |
Prevalence and Pattern of HIV/AIDS-Related Ocular Manifestations
Of 401 adult HIV patients, 28.9% of them had HIV/AIDS-related ocular manifestations with 95% CI (24.9, 33.4) (Figure 1).
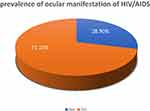 |
Figure 1 The proportion of ocular manifestation of HIV/AIDS among adult patients attending in University of Gondar Comprehensive Specialized Hospital ART clinic 2021. |
The most common ocular manifestations of HIV/AIDS were seborrheic blepharitis (16.4%) followed by squamoid conjunctival growth (4.5%) (Figure 2).
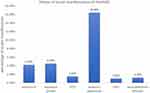 |
Figure 2 Pattern of HIV/AIDS-related ocular manifestations among adult patients attending at University of Gondar Comprehensive Specialized Hospital ART clinic, 2021. |
Factors Associated with HIV/AIDS-Related Ocular Manifestations
In bivariable logistic regression, certain variables such as sex, age, WHO clinical stage of HIV, CD4 count, duration of HIV, history of eye disease, and eye checkup history were associated with the ocular manifestation of HIV/AIDS with a p-value <0.25.
In multivariable logistic regression analysis, age, CD4 count, WHO clinical stage of HIV/AIDS, eye disease history, and duration of HIV were statistically significant variables with p-value <0.05. Patients in the age group >35 years had 2.5 times higher odds of having ocular manifestation compared to patients ≤35 years of age (95% CI: 1.19, 5.35). Patients who had a CD4 count of fewer than 200 cells/µL had 4.7 times increased odds of having ocular manifestations compared with those having CD4 count ≥200 cells/µL (95% CI: 2.50, 9.09). HIV patients with a duration of higher than 5 years had 2.8 times more odds of having ocular manifestations than patients with a duration of ≤5 years (95% CI: 1.29, 6.05). Patients who were on WHO stage II had 2.6 times more odds of having ocular manifestation compared with WHO stage I (95% CI: 1.23, 5.50). Patients who had a history of eye disease had 3 times increased odds of having ocular manifestation compared with their counterparts (95% CI: 1.38, 6.72) (Table 4).
Discussion
This study assessed the prevalence and associated factors of ocular manifestations of HIV/AIDS among adult HIV patients. The prevalence of ocular manifestation of HIV/AIDS was 28.9% (95% CI: 24.9, 34.4). This finding was consistent with the studies done in Jimma (Ethiopia) 25.3%,17 Bahirdar (Ethiopia) 25.7%,12 China 33.8%,24 and Nepal 26.49%.25
However, the result of this study was lower than the studies done in Gondar (Ethiopia), 60%,26 Kenya 60.2%,27 Ghana 48%,21 South Korea 48%,22 Nigeria 37.1%,28 and Indonesia 63.3%.20 This variation might be due to the difference in sampling technique and sample size. The study done in Gondar was on pre-HAART patients and also on patients who were in the advanced stage of the disease. So, this might overestimate the result of the study done in Gondar. The higher prevalence of ocular manifestation in Ghana might be due to the WHO clinical staging of the disease since 77% of the study patients were in WHO clinical stages III and IV. Also, in the study conducted in Kenya, 33.8% of the study participants were seeking eye ocular examination during the data collection time. This may overestimate the ocular manifestations of HIV/AIDS. About 30% of the study samples in the South-Korean study were patients referred to the eye clinic for medical treatment and the mean CD4 count was 266.7cells/µL. In the study done in Indonesia and Kenya, patients with other systemic diseases such as diabetes and hypertension were not excluded from the study. These differences might increase the prevalence ocular manifestations of HIV/AIDS.
On the other hand, the prevalence of ocular manifestations in our study was higher than the studies done at Hawassa (Ethiopia) 14.2%29 Burundi, 21%30 Taiwan 4.6%,23 and India 8%.31 This discrepancy might be due to, different operational definitions and study designs. In Taiwan, a retrospective cohort study with a chart review of HIV patients for possible ocular problem records was conducted. This might underestimate the prevalence of ocular manifestation of HIV/AIDS. In the study conducted in Burundi and India, the sample size was 154 and 121 patients, respectively. So, this small sample size may underestimate the result of the study. Compared with the study done in India, the variation might be due to socioeconomic and sociodemographic differences.
Regarding the associated factors, age >35 years, WHO clinical stage II, CD4 count < 200 cells/µL, duration of HIV >5 years, and history of eye disease were statistically significant factors for ocular manifestations of HIV/AIDS.
In this study, patients in the age group older than 35 years had 2.5 times increased odds of having ocular manifestation compared with those younger than 35 years. A similar result was reported in Jimma, Ethiopia,17 and Ghana.21 The possible reason for this finding might be due to the effect of age on the patient’s immune system. As the age of the patient increases the immune status of the body will deteriorate, which leads to low CD4 cells count in the blood.
According to this study, subjects who had a CD4 count <200 cells/µL had 4.7 times increased odds of having ocular manifestations compared with patients who had a CD4 count ≤200cells/µL. This result was coherent with the studies conducted in Jimma,17 Bahirdar,12 Gondar,26 Ghana,21 and Indonesia.20 CD4+ T cells count of less than 200 cells/µL is a well-established fact for higher ocular manifestations of HIV/AIDS. As the CD4 count cells deteriorate the patient’s immune system also deteriorates, which increases the risk of immunocompromised disease including ocular manifestations.32,33
In the present study, patients who had an eye disease history had three 3 times more odds of having ocular manifestations. This finding was coherent with the study done in Bahirdar, Ethiopia.12 The possible reason for this might be due to patients with the ocular disease have an increased risk of ocular coinfection. Also, some findings might be misdiagnosed as the ocular manifestation of HIV/AIDS.
According to this study, patients who were in WHO clinical stage II had 2.6 times more odds of having ocular manifestations of HIV/AIDS compared with patients who are in WHO stage I of the disease. This result was consistent with the studies done in Ghana21 and Indonesia.20 The WHO clinical stage of HIV infection is based on the immune status of the patient. The immune status of patients who are in WHO clinical stages II, III, and IV are low. The risk of eye disease is increased with the advanced immune suppression stage of HIV infection.33
In addition, patients with a longer duration of HIV/AIDS had 2.8 times more odds of having ocular manifestations. This finding was in line with the study done in Jakarta, Indonesia.20 Nowadays, antiretroviral therapy contributes to the increasing life span of HIV-positive persons and they live longer. As the duration increases, the immune status of the patient decreases due to the long-term effect of the virus on white blood cells.
However, factors like sex, HAART, and eye checkup history were not associated with ocular manifestations of HIV/AIDS in this study, which were previously reported to have an association with the ocular manifestation of HIV/AIDS in other studies done before.12,17,21
In this study, the commonest ocular manifestations of HIV/AIDS were adnexal of which seborrheic blepharitis is the commonest at 16.4% followed by squamoid conjunctival growth at 4.5% and molluscum contagiosum at 4.2%. This finding was similar to the result reported in Hawassa29 Bahirdar,12 Jimma,17 and the systematic review in England.10 However, this result is different from the study conducted in Gondar,26 Taiwan,23 and South Korea,22 where the commonest ocular manifestation was HIV retinopathy, CMV retinitis, and neuropthalmic disorders. This variation might be due to the studies in Gondar, Taiwan, and, South Korea being done on patients in an advanced stage of the disease (stage III and IV) where HIV retinopathy, CMV retinitis, and neuropthalmic disorders are common.
Limitation of the Study
In this study, the study design used was a cross-sectional study design, so it does not show the cause-and-effect relationship among variables. Also, as a result of time and resource constraints, pathology was not done to differentiate squamoid conjunctival growth from pterygium.
Recommendations
For the University of Gondar Comprehensive Specialized hospital
- It is better if the hospital gives regular follow-ups and manages HIV patients with low CD4 counts during follow-ups.
- It is also better if the hospital creates an integrated patient examination and link system in the ART clinic and eye clinic.
For the Ministry of Health
- It is better if the Ministry of Health also takes the responsibility to establish and expand integrated ocular screening, examination, and referral programs for HIV patients.
For future researchers
- I also encourage other researchers to focus on associated factors of ocular manifestations of HIV/AIDS with a comparative method.
Conclusion
The overall prevalence of ocular manifestations of HIV/AIDS among adult HIV patients was higher than some of the studies conducted in Ethiopia and Africa. The most common ocular manifestations of HIV/AIDS were seborrheic blepharitis and squamoid conjunctival growth. The prevalence was higher among patients, age >35 years, CD4+ count <200 cells/µL, WHO clinical stage II, patients with history of eye disease, and duration of HIV >5 years.
Though ocular manifestations of HIV/AIDS were high, HIV/AIDS patients especially those with lower CD4+ cell count, patients with duration of HIV >5 years and patients with older age should have eye checkup and follow-up by an ophthalmologist and optometrists, and there should be concerted care with a multidisciplinary approach. Further prospective studies should be carried out to investigate why some ocular findings are rare in our setting so that the real clinical picture and possible reasons will be known. The association between age and ocular manifestation warrants further investigation.
Acknowledgments
The authors would like to acknowledge the University of Gondar College of Medicine and Health Sciences for financial support to accomplish this work. The authors would like to thank the data collectors, ART clinic staffs and study participants for their valuable engagement during the data collection. The authors would also like to thank Mr Abiy Maru for his support and comments during the data analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Quinn TC. Global burden of the HIV pandemic. Lancet. 1996;348(9020):99–106. doi:10.1016/S0140-6736(96)01029-X
2. Global HIV and AIDS Statistics. Available from: www.unaids.org.
3. Chin J. Current and future dimension of the HIV/AIDS pandemic in women and children. Lancet. 1990;336:221–224. doi:10.1016/0140-6736(90)91743-T
4. Hladik W, Shabbir I, Jelaludin A, Woldu A, Tsehaynesh M, Tadesse W. HIV/AIDS in Ethiopia: where is the epidemic heading? Sex Transm Infect. 2006;82(suppl1):i32–i35. doi:10.1136/sti.2005.016592
5. Rosignoli L. Ocular manifestations of HIV infection; 2013. Available from: https://emedicine.medscape.com/article/1216172-overview. Accessed
6. Kestelyn PG, Cunningham ET. HIV/AIDS and blindness. Bull World Health Organ. 2001;79:208–213.
7. Biswas J. Acquired immunodeficiency syndrome and the eye. J Assoc Physicians India. 2001;49:551–557.
8. Peters RP, Kestelyn PG, Zierhut M, Kempen JH. The changing global epidemic of HIV and ocular disease. Ocul Immunol Inflamm. 2020;28(7):1007–1014. doi:10.1080/09273948.2020.1751214
9. Govender P, Hansraj R, Naidoo K, Visser L. Ocular manifestations of HIV/AIDS: a literature review*(Part 1). Afr Vis Eye Health. 2010;69(4):193–199. doi:10.4102/aveh.v69i4.141
10. Cunningham ET, Margolis TP. Ocular manifestations of HIV infection. N Engl J Med. 1998;339(4):236–244. doi:10.1056/NEJM199807233390406
11. Thorne J, Jabs D, Kempen J, Holbrook J, Nichols C, Meinert C. Studies of ocular complications of AIDS research group incidence of and risk factors for visual acuity loss among patients with AIDS and cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Ophthalmology. 2006;113(8):1432–1440. doi:10.1016/j.ophtha.2006.03.021
12. Sharew G, Azage M. Predictors of HIV/AIDS related ocular manifestations among HIV/AIDS patients in Felege Hiwot Referral Hospital, Northwest Ethiopia. J Ophthalmol. 2015;2015:1–7. doi:10.1155/2015/965627
13. Feroze KB, Wang J. Ocular manifestations of HIV; 2017.
14. Angra S, Murthy G, Gupta S, Angra V. Cataract related blindness in India & its social implications. Indian J Med Res. 1997;106:312–324.
15. Murthy G. The socioeconomic impact of human immunodeficiency virus/acquired immune deficiency syndrome in India and its relevance to eye care. Indian J Ophthalmol. 2008;56(5):395. doi:10.4103/0301-4738.42416
16. Amare B, Admassu F, Assefa Y, Moges B, Ali J, Kassu A. Pattern of ocular manifestation of HIV/AIDS among patients on HAART in ART clinic of Gondar University Hospital Northwest Ethiopia. J Clinic Exp Ophthalmol. 2011;2(192):2.
17. Bekele S, Gelaw Y, Tessema F. Ocular manifestation of HIV/AIDS and correlation with CD4+ cells count among adult HIV/AIDS patients in Jimma town, Ethiopia: a cross sectional study. BMC Ophthalmol. 2013;13(1):1–6. doi:10.1186/1471-2415-13-20
18. Alan Kozarsky M. HIV and your eyes. WebMED; 2020.
19. Kusagur S, Gururaj K. Clinical study of ocular manifestations in HIV/AIDS and its correlation with CD4+ T cells. Int J Biol Med Res. 2013;4(3):3284–3289.
20. Lestari YD, Sitompul R, Edwar L, Djoerban Z. Ocular diseases among HIV/AIDS patients in Jakarta, Indonesia. Southeast Asian J Trop Med Public Health. 2013;44(1):62–71.
21. Martin-Odoom A, Bonney EY, Opoku DK. Ocular complications in HIV positive patients on antiretroviral therapy in Ghana. BMC Ophthalmol. 2016;16(1):1–6. doi:10.1186/s12886-016-0310-5
22. Kim SJ, Park SJ, Yu HG, Kim NJ, Jang H-C, Oh M-D. Ocular manifestations of acquired immunodeficiency syndrome in Korea. J Korean Med Sci. 2012;27(5):542. doi:10.3346/jkms.2012.27.5.542
23. Tsen C-L, Chen Y-S, Wu K-S, et al. Ocular manifestations of human immunodeficiency virus infection at a tertiary referral center in Taiwan. Ocul Immunol Inflamm. 2019;27(7):1071–1076. doi:10.1080/09273948.2018.1499939
24. Lai TY, Wong RL, Luk FO, Chow VW, Chan CK, Lam DS. Ophthalmic manifestations and risk factors for mortality of HIV patients in the post‐highly active anti‐retroviral therapy era. Clin Exp Ophthalmol. 2011;39(2):99–104. doi:10.1111/j.1442-9071.2010.02400.x
25. Lamichhane G, Shah D, Sharma S, Chaudhary M. Ocular manifestations in HIV/AIDS cases in Nepal. Nepal J Ophthalmol. 2010;2(1):45–50. doi:10.3126/nepjoph.v2i1.3704
26. Assefa Y, Yohannes A, Melesi A. Ocular manifestations of HIV/AIDS patients in Gondar University Hospital, Northwest Ethiopia. Ethiop J Health Dev. 2006;20:3.
27. Luambo OA, Shadrack A. Ocular disease burden among HIV infected adults in an Urban Kenyan Hospital. IOSR Journal of Nursing and Health Science. 2021;10(1):25–31.
28. Arowolo MO, Awoyesuku EA, Pedro-Egbe CN. Ocular diseases in HIV-positive patients in a tertiary hospital in Nigeria. world. 2019;13(14):15.
29. Amsalu A, Desta K, Nigussie D, Delelegne D. Ocular manifestation and their associated factors among HIV/AIDS patients receiving highly active antiretroviral therapy in Southern Ethiopia. Int J Ophthalmol. 2017;10(5):776. doi:10.18240/ijo.2017.05.20
30. Cochereau I, Mlika-Cabanne N, Godinaud P, et al. AIDS related eye disease in Burundi, Africa. Br J Ophthalmol. 1999;83(3):339–342. doi:10.1136/bjo.83.3.339
31. Shah SU, Kerkar SP, Pazare AR. Evaluation of ocular manifestations and blindness in HIV/AIDS patients on HAART in a tertiary care hospital in western India. Br J Ophthalmol. 2009;93(1):88–90. doi:10.1136/bjo.2008.149237
32. Vrabec TR. Posterior segment manifestations of HIV/AIDS. Surv Ophthalmol. 2004;49(2):131–157. doi:10.1016/j.survophthal.2003.12.008
33. Moraes HV. Ocular manifestations of HIV/AIDS. Curr Opin Ophthalmol. 2002;13(6):397–403. doi:10.1097/00055735-200212000-00010
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


