Back to Journals » Clinical Interventions in Aging » Volume 13
Prevalence and associated factors of depressive symptoms among elderly inpatients of a Chinese tertiary hospital
Authors Zou C , Chen SP, Shen J, Zheng XM, Wang LX, Guan LJ, Liu Q, Yang YX
Received 6 April 2018
Accepted for publication 31 July 2018
Published 13 September 2018 Volume 2018:13 Pages 1755—1762
DOI https://doi.org/10.2147/CIA.S170346
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Zhi-Ying Wu
Video abstract presented by Chuan Zou.
Views: 191
Chuan Zou,* Shanping Chen,* Jing Shen, Xiaomei Zheng, Lingxiao Wang, Lijuan Guan, Qian Liu, Yongxue Yang
Department of Gerontology and Geriatrics, Chengdu Fifth People’s Hospital, Chengdu-Montpellier Geriatric Research Center, Chengdu, China
*These authors contributed equally to this work
Background: Depression in the elderly is a serious and often underdiagnosed psychiatric disorder that has been linked to adverse outcomes in the hospital setting. This study aims to evaluate the prevalence of depressive symptoms and associated factors among elderly hospital inpatients.
Methods: The cross-sectional study included 411 consecutively hospitalized patients aged 60 years and older. Participants were evaluated within 48 hours of admission using an interviewer-administered questionnaire including the Geriatric Depression Scale and comprehensive geriatric assessment to provide basic demographic and clinical information.
Results: Most of the participants were male (64.5%), with a mean (SD) age of 75.9 (8.1) years between 60 and 97 years. The prevalence of depressive symptoms was 32.8%. Univariate analysis showed significant associations between depressive symptoms and older age, female gender, lower body mass index, number of chronic diseases, impaired family function, impaired cognition, malnutrition, increased frailty, and decreased ability to perform activities of daily living. After logistic regression, variables that remained significantly associated with depression were cognitive decline (odds ratio =1.97, 95% CI: 1.09–3.55), poor family function (odds ratio =2.01, 95% CI: 1.10–3.66), and frailty (odds ratio =5.07, 95% CI: 1.95–13.20). Depressive symptoms were independently associated with prolonged hospital length.
Conclusion: Depressive symptoms were prevalent among hospitalized elderly and independently associated with cognitive decline, poor family function, and frailty. Therefore, it is essential to screen for depression and perform a comprehensive geriatric assessment in these patients to identify and manage depressive symptoms.
Keywords: depressive symptoms, aged, inpatients, prevalence, comprehensive geriatric assessment
Introduction
Mental disorders are among the most prevalent chronic diseases of the elderly worldwide, with depression being one of the most common psychiatric disorders in this population.1,2 Depression in the elderly is associated with severe adverse health outcomes including disability,3 mortality,4 and reduced quality of life.5 It also leads to higher care burdens for family members and caregivers.6
Previously reported estimates of the prevalence of depression among older populations depend on many factors including methodology, diagnostic criteria, and characteristics of the samples. A meta-analysis study revealed that the median prevalence rate of depressive disorders in the world for the elderly population was 10.3%, with interquartile range varying between 4.7% and 16.0%.7 A higher prevalence of depressive symptoms has been reported in studies involving hospitalized elderly, ranging from 10% to 56%, especially when geriatric inpatients have medical conditions such as stroke or heart failure.8–13 Despite this higher prevalence, depression is not often diagnosed or properly treated in medical settings.
The existing studies indicated that hospitalized elderly with poor functional capacity9 were more likely to be affected by depression, and patients with severe medical diseases14 had the highest prevalence rate. Other common risk factors for inpatient geriatric depression were low education level,9 number of comorbidities,8 female gender,8 unmarried status,8 lower income,8 sleep disturbance,14 undernutrition,15 and poor cognitive functioning.16
Comprehensive geriatric assessment (CGA), a systematic approach aiming to assess physical functioning, comorbidity, nutrition, cognition, frailty, and emotional status in elderly patients, has widely been conducted in geriatric departments after patients have been hospitalized. Extensive studies have provided strong evidence that a geriatric intervention guided by CGA increased patients’ likelihood of being alive and in their own homes at 3–12 months follow-up and decreased the likelihood of being admitted to a nursing home.17–19
The aim of the present study was to determine the prevalence of depressive symptom and associated factors among hospitalized elderly. In addition, we have evaluated the association between depressive symptom and other CGA domains.
Methods
Study participants
This was a cross-sectional study approved by the Ethics in Research Committee of the Chengdu Fifth People’s Hospital. From January 2015 to August 2017, we enrolled a consecutive series of patients aged 60 years and older who were admitted to the geriatric wards of Chengdu Fifth People’s Hospital, which was also the Chengdu-Montpellier Geriatric Center. Study participants were excluded if they were diagnosed with severe cognitive dysfunction, hearing impairment, severe cardiopulmonary diseases, reduced level of consciousness, crucial organ failure, or other unstable medical illnesses. Baseline demographic characteristics and depressive symptoms were recorded and assessed by the main researchers during face-to-face interview using a general questionnaire. Laboratory results, hospital length of stay, and hospital fees were recorded from electronic medical records. CGA was conducted within 48 hours of admission by a team consisting of geriatricians and a geriatric nurse. Written informed consent was obtained from all participants (or their legal proxies).
Assessment of depressive symptom
The study used 15-Geriatric Depression Scale (GDS) to assess depressive symptom among elderly people in the preceding week. Each of the 15 items was coded as 0 (no) or 1 (yes). The GDS-15 has been used in numerous studies on geriatric depression with a sensitivity of 79% and specificity of 77% in the general hospital.20,21 In this study, participants with a total GDS-15 score of 6 or above were classified as depressed.22
Assessment of CGA
Comorbidities: the prevalence of 18 common medical conditions was determined using a checklist that followed the question: “Do you suffer, or were you ever told by a doctor that you suffer, from the following problems in the past one year?” Chronic diseases included cardiovascular disease and hypertension, diabetes mellitus, obstructive pulmonary disease, malignancy, Parkinson’s disease, arthritis or osteoarthritis, chronic kidney disease, etc. Comorbidity, defined as more than three chronic diseases, was calculated for analysis.
Physical function: activities of daily living (ADLs) were measured using the modified Barthel Index, which consists of 10 items (grooming, bathing, eating, dressing, toilet use, fecal and urinary continence, ability to go up and down stairs, and walking in a hallway). This index ranges from 0 to 100, with a score of 100 indicating full independence, a score of 60–99 indicating partial dependence, and a score of <60 full dependence.23
Nutrition: nutrition was assessed with the Mini Nutritional Assessment Short Form (MNA-SF), with scores ranging from 0 to 14; scores of <8 indicated malnutrition, between 8 and 11 indicated risk of malnutrition, more than 11 indicated normal nutritional status.24
Family function: family functioning was assessed using the Family APGAR Index, which evaluates Adaptability, Partnership, Growth, Affection, and Resolve, and scores each component from zero to two. The Chinese version of Family APGAR index has been widely used in China, with satisfactory validity and reliability.25 The total score range varies from 0 to 10. Higher scores indicate higher levels of satisfaction with family functioning. According to the cut-off scores, a score of 0–7 indicates moderate family dysfunction and 8–10 indicates supportive family functioning.26
Frailty: the 5-item FRAIL scale was used for screening for frailty. There are five components: fatigue, resistance, ambulation, illnesses, and loss of weight. Frailty scores range from 0 to 5 and represent frail (3–5), pre-frail (1–2), and robust (0) health status.27
Cognitive function: cognitive function was measured using the Chinese version of the MMSE. Cognitive impairment was considered possible if the MMSE score was <18 for illiterate, <21 for elderly with primary education, and <25 above junior middle school.28
Assessment of covariates
Demographic characteristics: questions about age, gender, and smoking and drinking habits were answered by the participants.
Physical examination: body mass index was calculated as weight in kilograms divided by height in meters squared at admission; systolic blood pressure and diastolic blood pressure were defined by the mean of two out of three measures using standard protocol in admission.
Laboratory tests: blood routine, C-reactive protein, fasting glucose, serum albumin, low-density lipoprotein, and data on kidney and hepatic function were collected via the electronic medical record.
Assessment of outcomes
Prolonged hospital length: defined as more than third quartile of hospital length of our participants.
Higher hospital expense: defined as more than third quartile of hospital expense of our participants.
Statistical analyses
All statistical analyses for the present study were carried out with the SPSS for Windows software package, version 22.0 (SPSS Inc., Chicago, IL, USA). The normal variables were reported as mean ± standard deviation (SD), while the nonnormal variables were described by median ± interquartile range. Categorical variables were reported as frequency and proportions. We first performed univariate analysis to investigate the association between all individual variables and depressive symptom at admission by Student’s t-tests/analysis of variance when distributions were normal and Mann–Whitney U/Kruskal–Wallis tests otherwise. Only those univariate variables that showed a significant relationship with the outcome were subsequently tested in the final logistic regression model (enter). Another multiple logistic regression was also performed to explore the association between depressive symptoms and prolonged hospital length and higher hospital expense. First, we used the unadjusted model, then used two mutually adjusted models: 1) model 1: (age and gender); 2) model 2: model 1+ CGS (comorbidity + ADL + MMSE+ APGAR + frailty + MNA-SF). Two-sided P-values were considered to be statistically significant at ≤0.05.
Results
The study included 411 hospitalized patients with a mean (SD) age of 75.9 (8.1) years between 60 and 97 years, predominantly males (64.5%). The most frequent reasons for admission (Table 1) to the hospital were respiratory illnesses (36.3%), metabolic disorders (18.7%), cardiovascular conditions (17.8%), gastrointestinal conditions (8.0%), and infectious diseases (5.1%). The median length of hospital stay was 9 days (interquartile range: 3–72). Only one patient died during the hospitalization.
  | Table 1 Admission of elderly patients (N=411) |
Depressive symptoms were present in 32.8% of the study participants. Univariate analysis revealed that significant associations were seen between depressive symptoms and older age, female gender, lower body mass index, more chronic diseases, impaired family function, cognitive impairment, malnutrition, increased frailty, and need for support while performing ADL (Table 2). The depressed group also showed longer hospitalization.
The meaningful findings of the univariate analysis were also evaluated with logistic regression analysis (Table 3). According to the logistic regression analysis, depressive symptoms were significantly presented in the elderly with poor cognitive function (odds ratio [OR] =1.97, 95% CI: 1.09–3.55) compared to the ones with normal cognition. Depressive symptoms were also found in elderly patients with dysfunctional family support (OR =2.01, 95% CI: 1.10–3.66). Frail subjects were more likely to have depressive symptoms than the ones who were not (OR =5.07, 95% CI: 1.95–13.20).
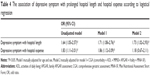
Another logistic regression was conducted to identify whether depressive symptom were associated with the outcome (prolonged hospitalization and high hospital expense). In the unadjusted analysis, depressive symptoms were associated with longer hospitalization (OR =1.64, 95% CI: 1.05–2.57) and higher hospital expense (OR =1.83, 95% CI: 1.11–3.01). The results were similar in model 1 with confounding factors of age and gender. When adding the variables of CGA in model 2, depressive symptoms were only independently associated with longer hospitalizations (OR =1.73, 95% CI: 1.02–2.93) (Table 4).
Discussion
While the majority of research was done to understand the differences in demographic characteristics (gender, age, marital status, education, income) and depression in community-settings elderly,29–31 our study evaluated depressive symptoms among elderly inpatients in a Chinese public university hospital and found independent associations for depressive symptoms and some CGA domains such as poor family function, cognitive impairment, and frailty. We also found that depressive symptoms were associated with longer hospitalization in elderly inpatients.
This study revealed that 32.8% of hospitalized older adults experience depressive symptoms. This finding is similar to previous cross-sectional study showing depression rates of 38.6% among elderly inpatients in China,32 but higher than the 18.1% rate described in another Chinese study involving hospitalized elderly people conducted in 13 general hospitals.14 This could be due to the use of different measurements for depression and the differences in study populations (eg, types and severity of the original diseases that caused the hospitalization).
In contrast with community-based studies,29–31 we found no significant differences in the prevalence of depression among different genders, or ages of elderly inpatients, which are congruent with those of several studies conducted in China14,33 and Brazil.9 This could be explained based on the fact that the stress of getting sick and being hospitalized can be considered an adverse condition for hospitalized elderly independent of gender and age, which increased the risk of depression.34 Therefore, health status, routinely evaluated by CGA, might be a more important factor associated with depression among elderly people.
In our study, significantly more depressive symptoms were found among those with higher frailty scale. Makizako et al35 also revealed older people with frailty were prone to have incidence of depression 15-months later. Previous studies indicate that factors similar to components of physical frailty, such as mobility, balance problems, weakness, poor endurance, etc, may lead to disability and functional dependence, thus increasing the risk for developing depressive symptoms in elderly adults.36,37 The possible biological mechanisms accounting for frailty, such as cerebrovascular disease, oxidative stress, chronic inflammation, hypothalamic–pituitary–adrenal axis dysregulation, and mitochondrial dysfunction, are also identified in individuals with late-life depression.38,39 A meta-analysis conducted by Soysal et al40 has proven the reciprocal interaction between depression and frailty in older adults. Therefore, it might be essential to evaluate and manage frailty in order to improve depressive symptoms.
A significant association was also seen between depressive symptoms and impaired cognition in our study. A meta-analysis conducted by Ismail showed that depression is common in people with mild cognitive impairment (MCI), with an overall pooled prevalence of 32%.41 Depression may come from the impairment in attention and working memory, changes in sleep patterns, and social isolation accompanied by cognitive impairment.42 Moreover, the brain structure changes in MCI share some common features of late-life depression.43,44 Numerous studies have demonstrated the relationship between inpatient elderly depression and objective family support such as living alone, or being widowed or divorced.8,9,30 In our study, we found poor subjective family support assessed by Family APGAR Index was independently associated with depression. With the increasing age, elderly patients’ social roles and self-concept has been changed, and the emotional support of functional family has become more important for them.45 When elderly patients are sick and hospitalized, a dysfunctional family dynamic may contribute to the occurrence of depression. Our findings are aligned with previous research suggesting that depression has strong negative relationship with family function in elderly.46,47
In our present study, longer hospitalization was observed in depressive elderly than their nondepressed counterparts, which is consistent with the previous studies.9,48 This might be explained in that the depressed group was more frail, had more comorbidity conditions, had worse nutritional status, and was disabled. However after controlling for these confounding factors, depressive symptoms still influenced the hospitalization process. The mechanisms linking depression to longer hospitalization are not clear, but are likely to include multiple pathways such as slow resolution of inflammatory responses, impaired behavioral adaptation, and greater susceptibility to infection.49 Further work is needed to investigate these biological and behavioral pathways in elderly patients.
One limitation of our study is the adoption of the GDS scale, rather than structured interviews for diagnosing depression, to measure depressive symptom, which is considered more appropriate for identification and less sensitive to somatic symptoms that might cause overestimation of depression. Another methodological limitation is inherent in the cross-sectional study design, which generates information concerning prevalence and associated factors, but not concerning etiological factors or the direction of causality. Finally, the study was performed at a single tertiary care hospital, and thus the result might be prudently generalized to other settings and needs to be verified in larger population and across multiple hospital centers.
Conclusion
Depressive symptom was prevalent among the hospitalized elderly, especially among patients with frailty, poor cognition, and less family support. Our results should encourage geriatricians to adopt a brief instrument such as GDS-15 and CGA to early screen depressive symptoms. Future studies are needed to identify the appropriate measures to intervene elderly inpatient with depressive symptom and their impact on patients’ function and health outcomes.
Acknowledgments
This work was supported by the Health and Family Planning Commission of Sichuan Province (No 150021). The authors thank the nurses, clinicians, administrators, and management staff of the geriatric wards of Chengdu Fifth People’s Hospital and Chengdu-Montpellier Geriatric Center, for their participation and support for this research. We thank Sammon DO Brian for his linguistic assistance during the preparation of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. World Health Statistics 2010. Geneva: World Health Organization; 2010. | ||
Mccall WV, Kintziger KW. Late life depression: a global problem with few resources. Psychiatr Clin North Am. 2013;36(4):475–481. | ||
Beekman AT, Penninx BW, Deeg DJ, de Beurs E, Geerling SW, van Tilburg W. The impact of depression on the well-being, disability and use of services in older adults: a longitudinal perspective. Acta Psychiatr Scand. 2002;105(1):20–27. | ||
Abas M, Hotopf M, Prince M. Depression and mortality in a high-risk population. 11-Year follow-up of the Medical Research Council Elderly Hypertension Trial. Br J Psychiatry. 2002;181:123–128. | ||
Olver JS, Hopwood MJ. Depression and physical illness. Med J Aust. 2013;1(4):9–12. | ||
Baldwin RC, Anderson D, Black S, et al. Guideline for the management of late-life depression in primary care. Int J Geriatr Psychiatry. 2003;18(9):829–838. | ||
Barua A, Ghosh MK, Kar N, Basilio MA. Prevalence of depressive disorders in the elderly. Ann Saudi Med. 2011;31(6):620–624. | ||
Alamri SH, Bari AI, Ali AT. Depression and associated factors in hospitalized elderly: a cross-sectional study in a Saudi teaching hospital. Ann Saudi Med. 2017;37(2):122–129. | ||
Mendes-Chiloff CL, Ramos-Cerqueira AT, Lima MC, Torres AR. Depressive symptoms among elderly inpatients of a Brazilian university hospital: prevalence and associated factors. Int Psychogeriatr. 2008;20(5):1028–1040. | ||
Conde Martel A, Hemmersbach-Miller M, Anía Lafuente BJ, Sujanani Afonso N, Serrano-Fuentes M. Prevalence of depressive symptoms in hospitalized elderly medical patients. Rev Esp Geriatr Gerontol. 2013;48(5):224–227. | ||
Pepersack T, de Breucker S, Mekongo YP, Rogiers A, Beyer I. Correlates of unrecognized depression among hospitalized geriatric patients. J Psychiatr Pract. 2006;12(3):160–167. | ||
de Man-van Ginkel JM, Hafsteinsdóttir T, Lindeman E, Burger H, Grobbee D, Schuurmans M. An efficient way to detect poststroke depression by subsequent administration of a 9-item and a 2-item Patient Health Questionnaire. Stroke. 2012;43(3):854–856. | ||
Guallar-Castillón P, Magariños-Losada MM, Montoto-Otero C, et al. Prevalence of depression and associated medical and psychosocial factors in elderly hospitalized patients with heart failure in Spain. Rev Esp Cardiol. 2006;59(8):770–778. | ||
Li N, Chen G, Zeng P, et al. Prevalence of depression and its associated factors among Chinese elderly people: A comparison study between community-based population and hospitalized population. Psychiatry Res. 2016;243:87–91. | ||
German L, Feldblum I, Bilenko N, Castel H, Harman-Boehm I, Shahar DR. Depressive symptoms and risk for malnutrition among hospitalized elderly people. J Nutr Health Aging. 2008;12(5):313–318. | ||
Koenig HG, Gittelman D, Branski S, Brown S, Stone P, Ostrow B. Depressive symptoms in elderly medical-surgical patients hospitalized in community settings. Am J Geriatr Psychiatry. 1998;6(1):14–23. | ||
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553. | ||
Edwards BJ, Zhang X, Sun M, et al. Neurocognitive deficits in older patients with cancer. J Geriatr Oncol. 2018;9(5):482–487. | ||
Ellis G, Gardner M, Tsiachristas A, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:CD006211. | ||
Blank K, Gruman C, Robison JT. Case-finding for depression in elderly people: balancing ease of administration with validity in varied treatment settings. J Gerontol A Biol Sci Med Sci. 2004;59(4):378–384. | ||
Cullum S, Tucker S, Todd C, Brayne C. Screening for depression in older medical inpatients. Int J Geriatr Psychiatry. 2006;21(5):469–476. | ||
Dennis M, Kadri A, Coffey J. Depression in older people in the general hospital: a systematic review of screening instruments. Age Ageing. 2012;41(2):148–154. | ||
Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709. | ||
Chu CS, Liang CK, Chou MY, et al. Short-Form Mini Nutritional Assessment as a useful method of predicting the development of postoperative delirium in elderly patients undergoing orthopedic surgery. Gen Hosp Psychiatry. 2016;38:15–20. | ||
Chau TT, Hsiao TM, Huang CT, Liu HW. A preliminary study of family Apgar index in the Chinese. Gaoxiong Yi Xue Ke Xue Za Zhi. 1991;7(1):27–31. | ||
Smilkstein G, Ashworth C, Montano D. Validity and reliability of the family APGAR as a test of family function. J Fam Pract. 1982;15(2):303–311. | ||
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. | ||
Katzman R, Zhang MY, Ouang-Ya-Qu, et al. A Chinese version of the Mini-Mental State Examination; impact of illiteracy in a Shanghai dementia survey. J Clin Epidemiol. 1988;41(10):971–978. | ||
St John PD, Blandford AA, Strain LA. Depressive symptoms among older adults in urban and rural areas. Int J Geriatr Psychiatry. 2006;21(12):1175–1180. | ||
Yaka E, Keskinoglu P, Ucku R, Yener GG, Tunca Z. Prevalence and risk factors of depression among community dwelling elderly. Arch Gerontol Geriatr. 2014;59(1):150–154. | ||
Mechakra-Tahiri S, Zunzunegui MV, Préville M, Dubé M. Social relationships and depression among people 65 years and over living in rural and urban areas of Quebec. Int J Geriatr Psychiatry. 2009;24(11):1226–1236. | ||
Liu X, Jiang Y, Wang L. Investigations of depression status of senile inpatients in general hospital. J Clin Psychosom Dis. 2006;12(4):256–257. | ||
Zhang J, Ye M, Huang H, Li L, Yang A. Depression of chronic medical inpatients in China. Arch Psychiatr Nurs. 2008;22(1):39–49. | ||
Beekman AT, Deeg DJ, van Tilburg T, Smit JH, Hooijer C, van Tilburg W. Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord. 1995;36(1–2):65–75. | ||
Makizako H, Shimada H, Doi T, et al. Physical frailty predicts incident depressive symptoms in elderly people: prospective findings from the Obu Study of Health Promotion for the Elderly. J Am Med Dir Assoc. 2015;16(3):194–199. | ||
Weyerer S, Eifflaender-Gorfer S, Wiese B, et al. Incidence and predictors of depression in non-demented primary care attenders aged 75 years and older: results from a 3-year follow-up study. Age Ageing. 2013;42(2):173–180. | ||
Strawbridge WJ, Deleger S, Roberts RE, Kaplan GA. Physical activity reduces the risk of subsequent depression for older adults. Am J Epidemiol. 2002;156(4):328–334. | ||
Brown PJ, Roose SP, Fieo R, et al. Frailty and depression in older adults: a high-risk clinical population. Am J Geriatr Psychiatry. 2014;22(11):1083–1095. | ||
Vaughan L, Corbin AL, Goveas JS. Depression and frailty in later life: a systematic review. Clin Interv Aging. 2015;10:1947–1958. | ||
Soysal P, Veronese N, Thompson T, et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Res Rev. 2017;36:78–87. | ||
Ismail Z, Elbayoumi H, Fischer CE, et al. Prevalence of Depression in Patients With Mild Cognitive Impairment: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2017;74(1):58–67. | ||
Steffens DC, Potter GG. Geriatric depression and cognitive impairment. Psychol Med. 2008;38(2):163–175. | ||
Lebedeva AK, Westman E, Borza T, et al. MRI-Based Classification Models in Prediction of Mild Cognitive Impairment and Dementia in Late-Life Depression. Front Aging Neurosci. 2017;9:13. | ||
Wasserman LI, Ivanov MV, Ananjeva NI, et al. Cognitive impairments in depression: neuropsychological and MRI-studies. Zh Nevrol Psikhiatr Im SS Korsakova. 2015;115(1 Pt 2):13–19. | ||
Silverstein M, Litwak E. A task-specific typology of intergenerational family structure in later life. Gerontologist. 1993;33(2):258–264. | ||
Lu C, Yuan L, Lin W, Zhou Y, Pan S. Depression and resilience mediates the effect of family function on quality of life of the elderly. Arch Gerontol Geriatr. 2017;71:34–42. | ||
García Lozano L, Mérida Quiñones F, Mestre Reoyo I, et al. Depression in the elderly and the role of family dynamics. Aten Primaria. 2000;25(4):226–229. | ||
Poole L, Leigh E, Kidd T, Ronaldson A, Jahangiri M, Steptoe A. The combined association of depression and socioeconomic status with length of post-operative hospital stay following coronary artery bypass graft surgery: data from a prospective cohort study. J Psychosom Res. 2014;76(1):34–40. | ||
Kiecolt-Glaser JK, Glaser R. Depression and immune function: central pathways to morbidity and mortality. J Psychosom Res. 2002;53(4):873–876. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.