Back to Journals » Risk Management and Healthcare Policy » Volume 15
Prevalence and Associated Factors of Cigarette Smoking Among Medical Students in Wroclaw, Poland
Authors Pazdro-Zastawny K, Dorobisz K , Bobak-Sarnowska E, Zatoński T
Received 21 September 2021
Accepted for publication 25 December 2021
Published 18 March 2022 Volume 2022:15 Pages 509—519
DOI https://doi.org/10.2147/RMHP.S337529
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Katarzyna Pazdro-Zastawny, Karolina Dorobisz, Ewelina Bobak-Sarnowska, Tomasz Zatoński
Department of Otolaryngology, Head and Neck Surgery, Wroclaw Medical University, Wroclaw, Poland
Correspondence: Karolina Dorobisz, Email [email protected]
Objective: The study aimed to evaluate the nicotine addiction syndrome among students of the medical university of Wroclaw.
Materials and Methods: The anonymous self-administered online questionnaire regarding tobacco and e-cigarettes smoking was sent to 5616 students. A total of 407 students from Wrocław Medical University who fulfilled the questionnaire were enrolled.
Results: One-fourth of the surveyed medical students smoke or have smoked cigarettes in the past. About 75% of students report that there is no information about the harmfulness of smoking and its consequences in the course of teaching in medical studies. The majority of students, 74.5% of women and 62.8% of men, agree that nicotine dependence syndrome should become part of the curriculum of medical universities.
Conclusion: The proportion of smokers among medical students is very high, and their knowledge of smoking is insufficient. It seems necessary to implement urgent education for medical students about the consequences of smoking and the treatment of nicotine dependence syndrome. The knowledge of future doctors about the harmfulness of smoking in the future will allow reducing the number of patients suffering from smoking-related diseases and may help reduce the number of smokers among students. It seems necessary to intensify the antismoking campaigns in Poland and worldwide.
Keywords: tobacco smoking, medical students, addiction syndrome
Introduction
Tobacco smoking has been a persistent and serious global social problem for years. Poland is the second-largest producer of tobacco products in the European Union. 26% of adult Poles smoke cigarettes - one in five regularly, and one in twenty - occasionally. The percentage of smokers is currently the lowest in the history of CBOS research. Thus, there is a downward trend in the number of heavy smokers – since 2011, there are 10% fewer smokers in Polish society. Research shows that men are more frequent smokers than women (24% vs 18%).1
According to WHO every year, more than 8 million people die from tobacco use, approximately 50% of its users. More than 7 million of those deaths are from direct tobacco use, while approximately 1.2 million result from exposure of non-smokers to second - hand smoke.2 It has been established that tobacco smoking constitutes the most common risk factor for the development and premature death from cardiovascular diseases, lung disorders, cancers, diabetes, and hypertension.3
Evaluating smoking behaviors is essential to establish tobacco control strategies to decrease avoidable morbidity and premature mortality, and to reduce health disparities. American Cancer Society states that
clinicians support all attempts to quit the use of combustible tobacco and work with smokers to eventually stop using any tobacco product, including e-cigarettes.4
Smoking contributes to health inequalities. Multiple pathways include targeted marketing and ready access for lower educated communities at greater risk, ties to cultural norms around smoking, and the challenges of communicating risks of smoking. Disproportions continue with regard to access to prevention programs and cessation services.5
The prevalence of smoking in the health profession around the world varies. In the United States it is close to 7%,6 in Europe it is 3.8% in Wales7 and reaches 22.1% in Germany.8 Among Asian countries smoking prevalence ranges from 2.1% (in Thailand) to 66.9% (China).9,10
There is limited information on smoking behaviors among medical university students in Poland. Compared to the United States, where only 3–5% of medical students smoke cigarettes every day, the percentage of smoking students in Poland is higher.11 Survey conducted in Wroclaw Medical University among the students of the Medical Faculty in 2012 revealed that 21% of students smoked cigarettes.12 Different study showed that the prevalence of smoking among 1st year medical students from Gdańsk, Poland is similar to the prevalence noted in other European Medical Universities – which rates from 21% in France to 26% in Turkey.11 The high smoking rates among the general population of western countries are contrary to rather low smoking rates among medical students in many western countries.13,14
Medical studies increase negative smoking- related attitudes. However, they are not a sufficient source of knowledge of and attitudes towards tobacco control and education/training on tobacco-related issues. Zarobkiewicz et al15 revealed high-frequency tobacco products use, including alternative tobacco products, among medical university students. There is a high need to introduce intensive preventive measures to limit and reduce the popularity of tobacco products along with alternative tobacco products. Janik-Koncewicz et al revealed that the level of knowledge about the diagnosis and treatment of tobacco dependence among the Wrocław medical students is low, and requires improvement through educational activities at both facultative and compulsory study level with special attention focused on pharmaceutical treatment of the nicotine dependence syndrome.12
Tobacco product use education should be added to medical school curricula. A worrying percentage of medical students use tobacco products, including alternative tobacco products, and the inadequate knowledge, education, and cessation counseling skills to ensure precise guidance to patients. As future caregivers, medical students will play an important role in health promotion and disease prevention.16 There is a need for the construction of a medical school curriculum on cigarettes and alternative tobacco products as there is little information about medical student’s knowledge or are taught about them and extensive variations in attitudes about e-cigarettes together with an unsatisfactory education of tobacco products use.17 It particularly concerns students due to the fact that habits and health behaviors are formed during studies. Medical students are a future doctors who will influence the health attitudes of patients and play a crucial role in tobacco control decision-making at various levels from community to nation by offering a cessation counseling option.18,19 It was also revealed that although students support tobacco cessation training, the majority believe that they are not adequately trained and are not comfortable providing tobacco cessation education to patients. A formal evaluation of the curriculum is necessary so a profound tobacco prevention and cessation program can be created and introduced.20 Students highlight and the level of knowledge about the diagnosis and treatment of tobacco dependence is low, and requires improvement through educational activities at both facultative and compulsory study level with special attention paid to pharmaceutical treatment of the tobacco dependence syndrome.12
Aim of the Study
The study aimed to assess the current prevalence and patterns of tobacco and e-cigarette smoking evaluate attempt whether studies deliver training in tobacco prevention and treatment skills control in medical students in Wrocław, Poland.
Method
This research included data from a survey study conducted at Wrocław Medical University in Poland. Wrocław Medical University has 5616 students and consists of four faculties: medicine, dentistry, health sciences, pharmacy, both for Polish (PL) and English-speaking students (English Division, ED).
The anonymous self-administered online questionnaire regarding tobacco and e-cigarettes smoking was sent to 5616 students. A total of 407 students from Wrocław Medical University who fulfilled the questionnaire were enrolled. Data were collected in December 2020, during the winter semester of the academic year. In the online route, the project was advertised in an e-mail sent to the e-mail address assigned by the University. The students were informed about the study’s purpose and received detailed explanations and definitions of certain terms. The response rate was 7.24%. A questionnaire on smoking behavior and smoking-related knowledge was distributed online after sending it and completed by students. The questionnaire consisted of ten questions: five regarding demographic information (gender, age, year of study, smoking status, and exposure to passive smoking). The other five questions were used to assess knowledge about the harmful effects of tobacco smoking, smoking-related diseases, and medicines used in tobacco dependence treatment. The questionnaire was created by employees of Wrocław Medical University and was not validated. All study participants completed a questionnaire regarding demographic information (age, gender), smoking habits. Smoking was defined as smoking at least one cigarette per day or smoking at least 100 cigarettes in a lifetime.
Material
The study was conducted on 344 polish students, including 250 women and 94 men, and a group of 63 ED students, including 36 women and 27 men. The characteristics of the studied students are presented in Table 1.
 |
Table 1 Survey Participant Characteristics |
Results
10.3% of the surveyed students are active smokers of traditional cigarettes and 8.6% of e-cigarettes at the Medical University of Wroclaw. 17.7% of students smoked traditional cigarettes in the past, and 8.4% e-cigarettes (Table 2). 59.1% of non-smoking students have smoked a cigarette in their lifetime. Most of the students (59.7%) started smoking in high school, and 14.9% during their medical studies. 77.1% of students noticed that while studying at the Medical University, there was no information about the harmfulness of smoking. According to the survey data, 74.4% of students at social gatherings are exposed to secondhand smoke, and 32.4% at the University.
 |  |  |
Table 2 Survey Participant Results in Different Gender Groups |
Comparison of Results According to Gender
Women more often than men believe that the treatment of nicotine dependence syndrome should become part of the curriculum of Medical Universities (74.5% vs 62.8%; p = 0.024). Men smoke traditional cigarettes more often than women (16.5% vs 7.7%; p <0.001). The situation is similar with e-cigarettes (12.4% vs 7.0%; p <0.001). Women who do not smoke at the moment have smoked an e-cigarette less frequently than men (15.3% vs 30.2%; p <0.001). They also use other forms of nicotine administration less frequently (9.4% vs 19.8%; p = 0.009). Men are more likely than women to be exposed to secondhand smoke in the workplace (18.1% vs 9.1%); p = 0.015). These data are presented in Tables 3 and 4.
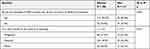 |
Table 3 Number (Percentage) of Responses to the Survey Questions on the NDS as a Part of the Curriculum Teaching Methods in Different Gender Groups |
 |
Table 4 Number (Percentage) of Responses to the Questionnaire on Nicotine Dependence Syndrome in Different Gender Groups |
Comparison of Results According to Nationality
The answers to the questions about the tobacco addiction syndrome in the groups of students completing the questionnaire in Polish and English and the results of statistical tests are presented in Tables 5 and 6.
 |
Table 5 Number (Percentage) of Answers to the Survey Questions on Tobacco Addiction Syndrome in Groups with Different Language Versions of the Survey |
 |
Table 6 Number (Percentage) of Responses to the Survey Questions on Nicotine Addiction Syndrome in Groups with Different Language Versions of the Survey |
Students who filled out the questionnaire in Polish less frequently than those who filled in it in English stated that in the course of education, there was information about the harmfulness of smoking (17.4% vs 52.4%; p <0.001) and that the treatment of tobacco addiction syndrome was the topic of some classes in the course of the previous teaching (17.4% vs 34.9%; p = 0.003). Polish-speaking students who are now non-smokers, in the past, smoked more often (64.4% vs 35.4%; p <0.001) and started smoking earlier (before university) than English-speaking students (84.7% vs 67.4%; p = 0.036). It is the same with e-cigarettes. Polish-speaking students who are now non-smokers in the past have smoked more often (42.4% vs 17.2%; p <0.001) and started smoking e-cigarettes earlier (before studies) than English-speaking students (81.0% vs 34.2%; p <0.001). Polish-speaking students are now less likely to use other forms of nicotine administration, such as IQOS (8.1% vs 11.1%; p <0.001). They also use other forms of nicotine administration less frequently (9.3% vs 30.2%; p <0.001). English-speaking students are more often exposed to passive smoking at the University (44.4% vs 30.2%; p = 0.039), in the workplace (23.8% vs 9.6%); p = 0.003) and in a dormitory (12.7% vs 4.9%; p = 0.038).
Discussion
The study aimed to evaluate the nicotine addiction syndrome among students of the Medical University of Wroclaw. Their smoking habits were analyzed, as well as the knowledge they received during their studies about the harmfulness of tobacco smoking. Our experience has found many important results worth discussing.
One-fourth of the surveyed medical students smoke or have smoked cigarettes in the past, which seems to be in line with the overall population. Many studies show an upward trend in smoking among medical students, which seems to be very disturbing.21–24 In assessing the results in terms of nationality, smoking in Poland begins at an earlier age, but this does not affect the percentage of smoking among students. A similar percentage of smokers is shown in works.25 According to the study from Berlin,24 the number of smoking men and women studying medical science is comparable, which is not in line with our results, where men significantly dominate. On the other hand, Monteiro et al26 show that the number of smoking men is decreasing, and women are increasing, but there are still more men smoking than women worldwide. The results of a study conducted in 2019 in Poland that estimated the prevalence of tobacco and e-cigarette use indicate a steady decrease in the frequency of smoking in Poland.27
Unfortunately, 75% of students report that there is no information about the harmfulness of smoking and its consequences in the course of teaching in medical studies. The majority of students, 74.5% of women and 62.8% of men, agree that nicotine dependence syndrome should become part of the curriculum of Medical Universities. Due to such a high percentage of smoking students, it seems necessary to introduce teaching about the addiction syndrome, as well as possible therapies for smoking cessation. This knowledge should be implemented from the earliest stages of medical studies, and the topic continued throughout the study.28 According to other studies, students do not associate smoking with mortality and chronic diseases like lung cancer or chronic obstructive pulmonary disease.24,29 Kusma et al24 also noted the need for changes in education on tobacco addiction at Medical Universities. Tessier et al30 presented in their works that the knowledge of students about the consequences of smoking is comparable to that of students of other fields.
Lack of proper knowledge of students regarding nicotine dependence syndrome may result in the lack of a competent approach to patients in the future. The knowledge of students and future doctors will not promote smoking cessation. A non-smoker up to the age of 90 is six times more likely to survive than a smoker.31 Reid et al31 also mention that 70% of smokers visit GP every year, most of them receive no advice or help to quit smoking.
Limitations of the Study
Anonymous and voluntary survey, so it can be assumed that the answers were reliable. The study is cross-sectional and gives a picture of the situation in only one Medical University, but its results are in line with the work of other medical schools. In subsequent works, it is necessary to consider extending the questionnaire with the knowledge of students transferred during medical studies about the harmfulness of smoking and methods of its treatment.
Conclusions
The proportion of smokers among medical students is very high, and their knowledge of smoking is insufficient.
It seems necessary to implement urgent education for medical students about the consequences of smoking and the treatment of nicotine dependence syndrome.
The knowledge of future doctors about the harmfulness of smoking in the future will allow reducing the number of patients suffering from smoking-related diseases and may help reduce the number of smokers among students.
It seems necessary to intensify the antismoking campaigns in Poland and worldwide.
Ethics Statements
The study protocol was approved by the ethic committee of Wroclaw Medical University and followed the Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Center for Social Opinion Research. Research report. Smoking. No. 104/2019. Available from: https://cbos.pl/SPISKOM.POL/2019/K_104_19.PDF.
2. World Health Organization. WHO global report on trends in prevalence of tobacco use 2000–2025. 3rd ed; Geneva: 2019. Available from: https://www.who.int/news/item/19-12-2019-who-launches-new-report-on-global-tobacco-use-trends.
3. West R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol Health. 2017;32:1018–1036. doi:10.1080/08870446.2017.1325890
4. American Cancer Society. American Cancer Society position statement on electronic cigarettes; February, 2018. Available from: https://www.cancer.org/healthy/stay-away-from-tobacco/e-cigarette-position-statement.html.
5. Samet JM. The environment and health inequalities: problems and solutions. J Health Inequal. 2019;5(1):21–27. doi:10.5114/jhi.2019.87818
6. Hayes RB, Geller AC, Crawford SL, et al. Medical school curriculum characteristics associated with intentions and frequency of tobacco dependence treatment among 3rd year U.S. medical students. Prev Med. 2015;72:56–63. doi:10.1016/j.ypmed.2014.12.035
7. Lewis KE, Shin D, Davies G. Smoking habits and attitudes toward tobacco bans among United Kingdom hospital staff and students. Int J Tuberc Lung Dis. 2011;15(8):1122–1126. doi:10.5588/ijtld.10.0783
8. La Torre G, Kirch W, Bes-Rastrollo M, et al. Tobacco use among medical students in Europe: results of a multicentre study using the Global Health Professions Student Survey. Public Health. 2012;126(2):159–164. doi:10.1016/j.puhe.2011.10.009
9. Warren CW, Sinha DN, Lee J, Lea V, Jones NR. Tobacco use, exposure to secondhand smoke, and cessation counseling among medical students: cross-country data from the Global Health Professions Student Survey (GHPSS), 2005–2008. BMC Public Health. 2011;11:72. doi:10.1186/1471-2458-11-72
10. Chen X, Tang X, Stanton B, Li H, Chen W. Cigarette smoking among medical students in China and modifiable risk factors for smoking prevention. Health Educ. 2012;112(4):333–349. doi:10.1108/09654281211237162
11. Siemińska A, Jassem JM, Uherek M, Wilanowski T, Nowak R, Jassem E. Postawy wobec palenia tytoniu wśród studentów pierwszego roku medycyny. Pneumonol Alergol Pol. 2006;74:383–388.
12. Janik-Koncewicz K, Zatoński T, Połtyn-Zaradna K, et al. An attempt to assess knowledge about tobacco dependence among students at the Medical University in Wroclaw. Ann Agric Environ Med. 2012;19(3):345–349.
13. Ashton CH, Kamali F. Personality, lifestyles, alcohol and drug consumption in a sample of British medical students. Med Educ. 1995;29(3):187–192. doi:10.1111/j.1365-2923.1995.tb02828.x
14. Patkar AA, Hill K, Batra V, Vergare MJ, Leone FT. A comparison of smoking habits among medical and nursing students. Chest. 2003;124(4):1415–1420. doi:10.1378/chest.124.4.1415
15. Zarobkiewicz MK, Wawryk-Gawda E, Woźniakowski MM, Sławiński MA, Jodłowska-Jędrych B. Tobacco smokers and electronic cigarettes users among Polish universities students. Rocz Panstw Zakl Hig. 2016;67(1):75–80.
16. Zhou S, Van Devanter N, Fenstermaker M, Cawkwell P, Sherman S, Weitzman M. A study of the use, knowledge, and beliefs about cigarettes and alternative tobacco products among students at one U.S. medical school. Acad Med. 2015;90(12):1713–1719. doi:10.1097/ACM.0000000000000873
17. Hinderaker K, Power DV, Allen S, Parker E, Okuyemi K. What do medical students know about e-cigarettes? A cross-sectional survey from one U.S. medical school. BMC Med Educ. 2018;18(1):32. doi:10.1186/s12909-018-1134-1
18. Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013;2013(5):CD000165. doi:10.1002/14651858.CD000165.pub4
19. Salgado MV, Mejía RM, Kaplan CP, Pérez-Stable EJ. Smoking-related attitudes and knowledge among medical students and recent graduates in Argentina: a cross-sectional study. J Gen Intern Med. 2017;32(5):549–555. doi:10.1007/s11606-016-3890-0
20. Cannick GF, Horowitz AM, Reed SG, Drury TF, Day TA. Opinions of South Carolina dental students toward tobacco use interventions. J Public Health Dent. 2006;66(1):44–48. doi:10.1111/j.1752-7325.2006.tb02550.x
21. Hamadeh RR. Smoking habits of medical students in Bahrain. J Smoking Related Dis. 1994;5:189–195.
22. Ramakrishna GS, Sankara Sarma P, Thankappan KR. Tobacco use among medical students in Orissa. Natl Med J India. 2005;18:285–289.
23. Ahmadi J, Khalili H, Jooybar R, Namazi N, Aghaei PM. Cigarette smoking among Iranian medical students, resident physicians and attending physicians. Eur J Med Res. 2001;6:406–408.
24. Kusma B, Quarcoo D, Vitzthum K, et al. Berlin’s medical students’ smoking habits, knowledge about smoking and attitudes toward smoking cessation counseling. J Occup Med Toxicol. 2010;5:9. doi:10.1186/1745-6673-5-9
25. Chkhaidze I, Maglakelidze N, Maglakelidze T, Khaltaev N. Prevalence of and factors influencing smoking among medical and non-medical students in Tbilisi, Georgia. J Bras Pneumol. 2013;39(5):579–584. doi:10.1590/S1806-37132013000500008
26. Monteiro CA, Cavalcante TM, Moura EC, Claro RM, Szwarcwald CL. Population-based evidence of a strong decline in the prevalence of smokers in Brazil (1989–2003). Bull World Health Organ. 2007;85(7):527–534. doi:10.2471/BLT.06.039073
27. Pinkas J, Kaleta D, Zgliczyński WS, et al. The prevalence of tobacco and E-cigarette use in Poland: a 2019 Nationwide Cross-Sectional Survey. Int J Environ Res Public Health. 2019;16(23):4820. doi:10.3390/ijerph16234820
28. Smith DR, Leggat PA. An international review of tobacco smoking among medical students. J Postgrad Med. 2007;53:55–62. doi:10.4103/0022-3859.30333
29. Raupach T, Shahab L, Baetzing S, et al. Medical students lack basic knowledge about smoking: findings from two European medical schools. Nicotine Tob Res. 2009;11:92–98. doi:10.1093/ntr/ntn007
30. Tessier JF, Freour P, Belougne D, Crofton J. Smoking habits and attitudes of medical students towards smoking and antismoking campaigns in nine Asian countries. The Tobacco and Health Committee of the International Union against Tuberculosis and Lung Diseases. Int J Epidemiol. 1992;21:298–304. doi:10.1093/ije/21.2.298
31. Reid RD, Pipe AL, Riley DL, Sorensen M. Sex differences in attitudes and experiences concerning smoking and cessation: results from an international survey. Patient Educ Couns. 2009;76:99–105. doi:10.1016/j.pec.2008.11.001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
