Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
Presepsin as a diagnostic marker for sepsis: evidence from a bivariate meta-analysis
Authors Tong X, Cao Y, Yu M, Han C
Received 17 March 2015
Accepted for publication 4 May 2015
Published 2 July 2015 Volume 2015:11 Pages 1027—1033
DOI https://doi.org/10.2147/TCRM.S84811
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Xiaomeng Tong, Yongtong Cao, Min Yu, Chengwu Han
Department of Laboratory Medicine, China-Japan Friendship Hospital, Beijing, People’s Republic of China
Background: The diagnosis of sepsis remains a clinical challenge. Many studies suggest that presepsin plays a role in diagnosing sepsis, but the results remain controversial. This study aimed to identify the overall diagnostic accuracy of presepsin for sepsis through meta-analysis.
Methods: A systematic literature search was performed in PubMed and EMBASE to identify studies evaluating the diagnostic accuracy of presepsin in sepsis patients. Data were retrieved and the pooled sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio (DOR) were calculated. A summary receiver operating characteristic curve and area under curve (AUC) were used to evaluate the overall diagnostic performance. The statistical analysis was performed using Stata 12.0 and Meta-DiSc 1.4 software.
Results: Eleven publications with 3,106 subjects were included in the meta-analysis. The pooled sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and DOR were 0.83 (95% confidence interval [CI] 0.77–0.88), 0.81 (95% CI 0.74–0.87), 4.43 (95% CI 3.05–6.43), 0.21 (95% CI 0.14–0.30), and 21.56 (95% CI 10.59–43.88), respectively. The area under the curve was 0.89 (95% CI 0.86–0.92). Estimated positive and negative post-probability values for a sepsis prevalence of 20% were 53% and 5%, respectively. No publication bias was identified.
Conclusion: Based on currently available evidence, presepsin may have a valuable role in the diagnosis of sepsis, and its results should be interpreted carefully in the context of clinical condition and traditional markers.
Keywords: sepsis, presepsin, diagnosis, meta-analysis
Introduction
Sepsis is defined as a potentially fatal systemic inflammatory response syndrome (SIRS) caused by severe infection.1,2 Sepsis affects millions of patients worldwide each year, and in the USA is the cause of almost 750,000 hospital visits, 570,000 emergency department admissions, 200,000 deaths, and 16.7 billion dollars in medical expenditure every year.2,3 Based on report of the promoting global research excellence in severe sepsis, in developing countries, the mortality rate for sepsis tends to be worse, at 56% in Brazil and 45% in other developing countries, as compared with 30% in developed countries.4 According to the latest published literature, during the first decade of the 21st century, the nationwide average mortality was nearly one per 100,000 persons in mainland China.5 Further, the occurrence of sepsis continues to increase.1
Current guidelines recommend that antibacterial therapy should be initiated as soon as possible to optimize clinical outcomes in patients with sepsis.6 However, due to the coexistence of non-infectious SIRS in many critical patients without specific symptoms, how to identify and differentiate sepsis from SIRS at an early stage remains a clinical challenge. Many biomarkers can be used in the diagnosis of sepsis, but none has sufficient specificity or sensitivity to be routinely employed in clinical practice. Procalcitonin and C-reactive protein have been widely used, but have a limited ability to distinguish sepsis from other inflammatory conditions or to predict outcome.7 Therefore, the search for a novel and reliable biomarker which is helpful for early diagnosis of sepsis is ongoing.
In 2005, presepsin, a new sCD14-subtype biomarker, was identified.8 Presepsin is a soluble N-terminal fragment of the cluster of differentiation (CD) marker protein CD14.8 Presepsin is released into the circulation during activation of monocytes upon recognition of lipopolysaccharide from infectious agents, so has a role in the diagnosis of sepsis.8,9 In recent years, a number of studies have investigated the potential of presepsin in the diagnosis of sepsis, and have reached conflicting conclusions about whether presepsin can provide adequate differentiating power.10 To reach a more reliable conclusion, we performed a meta-analysis of the literature reporting on the use of presepsin to diagnose sepsis.
Materials and methods
This meta-analysis was performed using the guidelines of the Preferred Reporting Items for Systematic Reviews, as well as the meta-analysis statement and methods recommended by the Cochrane Diagnostic Test Accuracy Working Group.11,12 Institutional review board approval was not required for this retrospective meta-analysis, and no ethics statement was needed.
Search strategy and literature selection
PubMed and EMBASE were used as the main search engines to identify suitable studies up to December 2014. The following key search terms were used: “sepsis OR severe sepsis OR septic shock” AND “sCD14-subtypes OR presepsin” AND “sensitivity OR specificity OR accuracy”. References of included articles were also searched manually to identify relevant publications. Included studies had to meet all of the following criteria: the study evaluated the diagnostic accuracy of presepsin for sepsis in humans; it had clear diagnostic criteria for sepsis; it could supply or calculate data for both sensitivity and specificity; and publication in English. Abstracts, letters, and reviews were excluded because of the limited information they provided; studies that did not report or could not calculate sensitivity or specificity and those with overlapping or repeating data were also excluded.
Data extraction and quality assessment
All included studies were assessed by two independent reviewers in order to reduce the risk of errors. In the event of disagreement, a third author assessed the articles and made the final decision. A data extraction form was created and the data retrieved from the articles included first author, publication year, the country of origin, samples, presepsin assay methods, cutoff value, and true positive, false positive, true negative, and false negative numbers for each study. For studies containing several groups or different backgrounds, each one was treated as a single study. The quality of the selected studies was assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) list, an evidence-based approach for quality assessment in systematic reviews of diagnostic accuracy studies, which includes 14 items assessing risk of bias, sources of variation (applicability), and reporting quality; each item is rated “yes”, “no”, or “unclear”. The maximum value for each study is 14.13
Meta-analysis
This study was performed according to the standard bivariate meta-analysis method.14 First, we calculated pooled estimates of sensitivity and specificity, with corresponding 95% confidence intervals (CIs). Based on the pooled estimates of sensitivity and specificity, we calculated positive likelihood ratios (PLRs), negative likelihood ratios (NLRs), and diagnostic odds ratios (DORs), which we used as overall indices of diagnostic accuracy. We also constructed a summary receiver operating characteristic (SROC) curve and calculated the area under the curve (AUC) to summarize the overall diagnostic performance of presepsin.
Heterogeneity was assessed using the I2 inconsistency test. I2 >50% indicated substantial heterogeneity, which was then analyzed by meta-regression to identify potential covariates. Post-test probability was calculated using an overall prevalence of 20% with Fagan nomograms. A Deeks’ funnel plot was used to detect publication bias.15 All analyses were performed using the Midas module in Stata 12.0 (Stata Corporation, College Station, TX, USA) and Meta-DiSc 1.4 for Windows (XI, Cochrane Colloquium, Barcelona, Spain). All statistical tests were two-sided, with P-values less than 0.05 taken as the threshold for statistical significance.
Results
Characteristics of included studies
A total of eleven publications including 12 studies published in 2011–2015 were included in this meta-analysis.16–26 The main reasons for excluding a study were: the study could not retrieve sensitivity and specificity data and reconstruct a 2×2 table or they were not diagnostic studies. The study selection process is shown in Figure 1.
  | Figure 1 Flow of study identification, inclusion, and exclusion. |
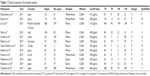
The 12 studies included 1,725 sepsis patients and 1,381 control subjects. Eight studies were performed in Asia16–18,23–26 and four were done in Europe.19–22 Six studies used plasma as the assay sample,18–23 four used whole blood,16,17,24,26 and two used serum.25 All the samples were analyzed by chemiluminescent enzyme immunoassay, and the cutoff values ranged from 317 to 864 pg/mL. For sepsis patients, all the studies supplied detailed diagnostic criteria, which are widely accepted for studies regarding sepsis. With the exception of one retrospective study,25 all the studies were prospective. Except for one study with a QUADAS score <10,16 all studies had a QUADAS score ≥10, indicating that our results were reliable. Table 1 summarizes the clinical characteristics and QUADAS scores for all the included studies.
Diagnostic accuracy
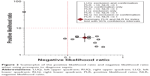
The following pooled parameters were calculated over all 12 studies examining presepsin for diagnosis of sepsis: sensitivity, 0.83 (95% CI 0.77–0.88); specificity, 0.81 (95% CI 0.74–0.87); PLR, 4.43 (95% CI 3.05–6.43); NLR, 0.21 (95% CI 0.14–0.30) (Figure 2); and DOR, 21.56 (95% CI 10.59–43.88). All five performance indices showed high I2 values, ie, sensitivity 85.46%, specificity 82.65%, PLR 75.54%, NLR 84.38%, and DOR 100.00% (all P<0.05), suggesting substantial heterogeneity among the included studies.
Figure 3 gives the SROC curve for the included studies, and shows a plot of the rate of true positives as a function of the rate of false positives for the individual studies. The AUC was 0.89 (95% CI 0.86–0.92), indicating a good discriminatory ability of presepsin measurement for sepsis. Fagan’s nomogram for likelihood ratios indicates that using presepsin to diagnose sepsis increased the post-probability to 53% when the results were positive and reduced the post-probability to 5% when the results were negative (Figure 4).
  | Figure 3 Summary receiver operating characteristic curve for presepsin measurements to diagnose sepsis. |
  | Figure 4 Fagan’s nomogram for likelihood ratios and pre-test and post-test probabilities when using presepsin measurements to diagnose sepsis. |
Meta-regression and publication bias
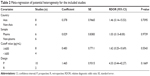
We identified significant heterogeneity among the included studies, so a meta-regression analysis was performed to explore the possible sources for this heterogeneity. We used four covariates in the meta-regression: country of origin (Asia versus non-Asia); test samples (plasma versus serum or whole blood); cutoff value (≥600 versus <600 pg/mL); and study design (prospective versus retrospective). The outcomes of the regression are shown in Table 2. In the present study, none of the above covariates were found to be significant sources of heterogeneity (all P>0.05).
We used the Deeks’ funnel plot asymmetry test to assess for the likelihood of publication bias. The slope coefficient for presepsin was associated with a P-value of 0.49, suggesting symmetry in the data and a low likelihood of publication bias (Figure 5).
  | Figure 5 Deeks’ funnel plot assessing the likelihood of publication bias. |
Discussion
Making an early and accurate diagnosis is critical for improving the prognosis in patients with sepsis. Current methods or biomarkers used for the diagnosis of sepsis remain unsatisfactory,7 and more reliable diagnostic markers are needed. A growing number of studies suggest that presepsin may play a role in identifying sepsis, and our present study summarizes the overall diagnostic performance of presepsin for sepsis based on the current available literature.
Our results reveal that the sensitivity and specificity of presepsin were 0.83 and 0.81, respectively, with a relatively high rate of missed diagnosis (17%) and misdiagnosis (19%). Likelihood ratios are indices that take into account the interaction between sensitivity and specificity in their calculation, and a PLR of 10 and NLR of 0.1 are considered to be convincing evidence to rule in or rule out a diagnosis, respectively.27 In this study, the overall PLR was 4.43, suggesting that the likelihood of a positive presepsin assay result was about fourfold higher in sepsis patients than in patients without sepsis. The pooled NLR was 0.21, suggesting the subjects remains may be sepsis patients even the results of presepsin was negative. The DOR combines the strengths of sensitivity and specificity and has the advantage of accuracy as a single indicator, with higher values indicating higher accuracy. In this meta-analysis, the mean DOR was 21.56, indicating a relatively high level of overall accuracy. The SROC curve was also used to summarize the overall diagnostic performance of the included studies, and the AUC was 0.89, indicating good diagnostic performance.
Although presepsin has an important role in diagnosing sepsis, we suggest that measurement of presepsin be combined with other traditional markers, such as procalcitonin, C-reactive protein, and white blood cells. From a recent published meta-analysis, the sensitivity and specificity of procalcitonin in diagnosing sepsis were 0.77 and 0.79, respectively;28 however, procalcitonin is still a valuable diagnostic marker for sepsis in clinical practice.29 Further, sepsis patients may benefit from procalcitonin-guided therapy with a shorter duration of antibiotic treatment when compared with standard care.30 In this study, we also noticed a relatively high rate of missed diagnosis and misdiagnosis using presepsin, so this indicator may not be reliable enough on its own but should instead be used in conjunction with more conventional tests, such as procalcitonin, rather than replace procalcitonin. Thus, it would be better to set up a diagnostic model or a decision tree when using these markers.31,32 With improvements in presepsin assay methods, presepsin may become a point-of-care tool for bedside diagnosis of sepsis in the future.
The clinical interpretation of presepsin results should take into account the clinical context of the patient. For example, the AUC was 0.784 in a non-acute kidney injury group and 0.698 an acute kidney injury group when presepsin was used to diagnose sepsis.25 In our meta-analysis, we also included patients with abdominal sepsis or burn sepsis, and the diagnostic performance of presepsin in these two kinds of sepsis were also different.20,22 Presepsin concentrations increase with age and kidney dysfunction, so interpretation of presepsin concentrations might be different in the elderly or in patients with impaired renal function.25 Adapted thresholds are needed for specific populations in clinical practice.33 We suggest that the results of a presepsin assay must be interpreted carefully in the context of medical history, physical examination, and microbiological assessment of patients.
Measurement of presepsin concentrations is not only useful for diagnosis of sepsis and evaluating its severity, but also for predicting the prognosis of patients with sepsis. Masson et al reported that early presepsin was higher in patients with severe sepsis or septic shock who died than in those who survived, and suggested that presepsin measurements may be of clinical importance for early risk stratification and provide useful prognostic information in these patients.34 Further, Endo et al reported that continuous measurement of presepsin has a role in monitoring the clinical response to therapeutic interventions in patients with sepsis.35 The results of these two results suggest that monitoring of presepsin is more clinically meaningful except for sepsis diagnosis.
Our study also has several limitations that should be discussed. First, we included only eleven publications because of our strict inclusion criteria, so our study may have lacked enough statistical power to draw a definite conclusion, and more clinical diagnostic studies are needed to be able to reach a final conclusion. Second, we identified significant heterogeneity among the included studies; although we performed a meta-regression to determine possible covariates, we did not find meaningful covariates. Thus, the heterogeneity could not be explained by meta-regression analysis. Further studies should pay attention to this problem. Finally, we only included studies published in English, which may have resulted in language bias, and the inclusion of other language publications or studies with null results may have yielded different results.
Conclusion
Taken together, our results suggest that presepsin plays a valuable role in the diagnosis of sepsis. Clinical interpretation of presepsin results should consider other traditional markers and the clinical context of the individual patient. Further studies should be performed to validate our findings.
Disclosure
The authors report no conflicts of interest in this work.
References
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–851. | ||
Cetinkaya A, Erden A, Avci D, et al. Is hypertriglyceridemia a prognostic factor in sepsis? Ther Clin Risk Manag. 2014;10:147–150. | ||
Levy MM, Artigas A, Phillips GS, et al. Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis. 2012;12:919–924. | ||
Westphal GA, Koenig Á, Caldeira Filho M, et al. Reduced mortality after the implementation of a protocol for the early detection of severe sepsis. J Crit Care. 2011;26:76–81. | ||
Chen XC, Yang YF, Wang R, Gou HF, Chen XZ. Epidemiology and microbiology of sepsis in mainland China in the first decade of the 21st century. Int J Infect Dis. 2015;31:9–14. | ||
Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228. | ||
Henriquez-Camacho C, Losa J. Biomarkers for sepsis. Biomed Res Int. 2014;2014:547818. | ||
Yaegashi Y, Shirakawa K, Sato N, et al. Evaluation of a newly identified soluble CD14 subtype as a marker for sepsis. J Infect Chemother. 2005;11:234–238. | ||
Mussap M, Noto A, Fravega M, Fanos V. Soluble CD14 subtype presepsin (sCD14-ST) and lipopolysaccharide binding protein (LBP) in neonatal sepsis: new clinical and analytical perspectives for two old biomarkers. J Matern Fetal Neonatal Med. 2011;24 Suppl 2:12–14. | ||
Zou Q, Wen W, Zhang XC. Presepsin as a novel sepsis biomarker. World J Emerg Med. 2014;5:16–19. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. | ||
Virgili G, Conti AA, Murro V, Gensini GF, Gusinu R. Systematic reviews of diagnostic test accuracy and the Cochrane collaboration. Intern Emerg Med. 2009;4:255–258. | ||
Whiting PF, Weswood ME, Rutjes AW, Reitsma JB, Bossuyt PN, Kleijnen J. Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol. 2006;6:9. | ||
Shen Y, Zhu H, Wan C, et al. Can cholesterol be used to distinguish pleural exudates from transudates? Evidence from a bivariate meta-analysis. BMC Pulm Med. 2014;14:61. | ||
Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–893. | ||
Shozushima T, Takahashi G, Matsumoto N, Kojika M, Okamura Y, Endo S. Usefulness of presepsin (sCD14-ST) measurements as a marker for the diagnosis and severity of sepsis that satisfied diagnostic criteria of systemic inflammatory response syndrome. J Infect Chemother. 2011;17:764–769. | ||
Endo S, Suzuki Y, Takahashi G, et al. Usefulness of presepsin in the diagnosis of sepsis in a multicenter prospective study. J Infect Chemother. 2012;18:891–897. | ||
Liu B, Chen YX, Yin Q, Zhao YZ, Li CS. Diagnostic value and prognostic evaluation of presepsin for sepsis in an emergency department. Crit Care. 2013;17:R244. | ||
Ulla M, Pizzolato E, Lucchiari M, et al. Diagnostic and prognostic value of presepsin in the management of sepsis in the emergency department: a multicenter prospective study. Crit Care. 2013;17:R168. | ||
Vodnik T, Kaljevic G, Tadic T, Majkic-Singh N. Presepsin (sCD14-ST) in preoperative diagnosis of abdominal sepsis. Clin Chem Lab Med. 2013;51:2053–2062. | ||
Behnes M, Bertsch T, Lepiorz D, et al. Diagnostic and prognostic utility of soluble CD 14 subtype (presepsin) for severe sepsis and septic shock during the first week of intensive care treatment. Crit Care. 2014;18:507. | ||
Cakir Madenci Ö, Yakupoğlu S, Benzonana N, et al. Evaluation of soluble CD14 subtype (presepsin) in burn sepsis. Burns. 2014;40:664–669. | ||
Ishikura H, Nishida T, Murai A, et al. New diagnostic strategy for sepsis-induced disseminated intravascular coagulation: a prospective single-center observational study. Crit Care. 2014;18:R19. | ||
Kweon OJ, Choi JH, Park SK, Park AJ. Usefulness of presepsin (sCD14 subtype) measurements as a new marker for the diagnosis and prediction of disease severity of sepsis in the Korean population. J Crit Care. 2014;29:965–970. | ||
Nakamura Y, Ishikura H, Nishida T, et al. Usefulness of presepsin in the diagnosis of sepsis in patients with or without acute kidney injury. BMC Anesthesiol. 2014;14:88. | ||
Takahashi G, Shibata S, Ishikura H, et al. Presepsin in the prognosis of infectious diseases and diagnosis of infectious disseminated intravascular coagulation: a prospective, multicentre, observational study. Eur J Anaesthesiol. 2015;32:199–206. | ||
Akobeng AK. Understanding diagnostic tests 2: likelihood ratios, pre- and post-test probabilities and their use in clinical practice. Acta Paediatr. 2007;96:487–491. | ||
Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:426–435. | ||
Reinhart K, Meisner M. Biomarkers in the critically ill patient: procalcitonin. Crit Care Clin. 2011;27:253–263. | ||
Prkno A, Wacker C, Brunkhorst FM, Schlattmann P. Procalcitonin-guided therapy in intensive care unit patients with severe sepsis and septic shock – a systematic review and meta-analysis. Crit Care. 2013;17:R291. | ||
Li HX, Liu ZM, Zhao SJ, Zhang D, Wang SJ, Wang YS. Measuring both procalcitonin and C-reactive protein for a diagnosis of sepsis in critically ill patients. J Int Med Res. 2014;42:1050–1059. | ||
Gibot S, Béné MC, Noel R, et al. Combination biomarkers to diagnose sepsis in the critically ill patient. Am J Respir Crit Care Med. 2012;186:65–71. | ||
Chenevier-Gobeaux C, Trabattoni E, Roelens M, Borderie D, Claessens YE. Presepsin (sCD14-ST) in emergency department: the need for adapted threshold values? Clin Chim Acta. 2014;427:34–36. | ||
Masson S, Caironi P, Spanuth E, et al. Presepsin (soluble CD14 subtype) and procalcitonin levels for mortality prediction in sepsis: data from the Albumin Italian Outcome Sepsis Trial. Crit Care. 2014;18:R6. | ||
Endo S, Suzuki Y, Takahashi G, et al. Presepsin as a powerful monitoring tool for the prognosis and treatment of sepsis: a multicenter prospective study. J Infect Chemother. 2014;20:30–34. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.