Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
Prescriber utilization of dalfampridine extended release tablets in multiple sclerosis: a retrospective pharmacy and medical claims analysis
Authors Jara M, Sidovar M, Henney HR
Received 15 October 2014
Accepted for publication 21 November 2014
Published 16 December 2014 Volume 2015:11 Pages 1—7
DOI https://doi.org/10.2147/TCRM.S75837
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Michele Jara,1 Matthew F Sidovar,2 Herbert R Henney III2
1Drug Safety and Risk Management, 2Clinical Development and Medical Affairs, Acorda Therapeutics, Inc, Ardsley, NY, USA
Purpose: This study aimed to characterize the prescribing of dalfampridine extended release (D-ER) 10 mg tablet treatment in people with multiple sclerosis (MS).
Methods: A retrospective cohort study was performed using Medco pharmacy and medical claims. Medical claims were used to identify MS patients with more than one prescription for D-ER with 1 year of prior continuous enrollment (n=704). These patients were matched 2:1 on age, sex, and health insurance source with a comparison group of MS patients who were treatment naïve for D-ER (n=1,403). Categorical data were analyzed by Χ2 test; ordinal data by Wilcoxon rank sum test; and continuous data by Student’s t-test.
Results: Most patients were women aged 45–64 years. In the year preceding D-ER initiation, the prevalence of seizure and renal impairment was numerically lower in the D-ER cohort relative to those who were D-ER naïve (seizure: 3.1% versus 4.7%, respectively; renal impairment: 4.3% versus 5.1%, respectively); however, prescriptions for antiepileptic drugs in the two cohorts were comparable. In the year preceding treatment initiation, 62% of the D-ER cohort was prescribed MS-specific disease-modifying therapies relative to 45% who were D-ER naïve.
Conclusion: Seizure and renal impairment rates among D-ER-naïve patients were consistent with published literature, yet rates among those prescribed D-ER during the year preceding treatment initiation were slightly lower than rates among D-ER-naïve patients. Given that D-ER is contraindicated in patients with history of seizure or moderate or severe renal impairment, lower rates may indicate that risk-minimization strategies contributed to the lower prevalence.
Keywords: disease-modifying therapy, database, seizures, renal impairment, pharmacoepidemiology
Introduction
Multiple sclerosis (MS), the most common disabling neurologic disease in young adults, is estimated to affect more than 2.3 million people worldwide.1 It is characterized by degeneration and loss of the myelin sheath, which results in a loss or impairment of conduction in affected axons.2 The peak onset of MS is between the ages of 20 years and 50 years, and it is diagnosed in women approximately two to three times as often as in men.1,3
Dalfampridine extended release (D-ER) 10 mg tablet treatment twice daily (D-ER; known as prolonged-release fampridine in Europe and as fampridine modified- or sustained-release elsewhere) has been shown to improve walking in people with MS.4 However, D-ER is contraindicated in patients with moderate or severe renal impairment or history of seizure4 and since the incidence of seizure is dose related,5 patients should not exceed the maximum recommended daily dose. To better inform both prescribers and patients, a Risk Evaluation and Mitigation Strategy (REMS) was implemented since approval and was in effect at the time of this study. This program consisted of a medication guide and communication strategy to clearly communicate the potential risks associated with use of the product, particularly in regard to the increased risk of seizure and use in patients with renal impairment.
To better understand the prescribing practice of D-ER in patients with MS, we conducted a retrospective database study using prescription and medical claims. Of particular interest was assessment of the history of seizure and renal impairment among MS patients prescribed D-ER compared with those who were D-ER naïve to assess the performance of the REMS program for dalfampridine in place at the time of this study.4
Methods
This retrospective cohort study was conducted using prescription data from the pharmacy benefit management (PBM) and medical claims data, both from the Medco database from January 1, 2009 to September 15, 2012. With over 60 million covered lives, Medco is the largest PBM company in the US, and in addition, it has medical claims for approximately 10 million covered lives that are linked to a subset of the PBM data. All data in the current analysis were compliant with the Health Insurance Portability and Accountability Act.
Patients with an MS diagnosis (International Classification of Diseases, ninth revision [ICD-9] code =340.xx) in the medical claims data, more than one D-ER prescription in the PBM data (National Drug code =10144–427-60), and 12 months of continuous enrollment in Medco prior to the first D-ER prescription were identified. MS patients prescribed D-ER were matched 2:1 with respect to age, sex, and health insurance source with MS patients identified as D-ER naïve. The date of first D-ER prescription claim was considered the date of initiation of treatment and this served as the index date for the D-ER patient. The index date for patients in the D-ER-naïve cohort was set to the date of the matched case. All patients selected for inclusion in the D-ER-naïve group were required to have an MS diagnosis prior to the index date of the D-ER patient to whom matching was done. Demographic information, preindex medication use, and medical history were determined for the 12-month preindex period (ie, preceding treatment initiation).
Claims-based evidence for occurrences of seizure, renal disorder, and renal impairment was examined during the 1-year preindex period. ICD-9 codes used for seizure identification included 345.xx (epilepsy and recurrent seizures) and 780.3x (convulsions). Renal disorder was defined using Deyo’s revision of the Charlson Comorbidity Index (CCI).6 The definition of renal impairment contains less severe renal-related diagnostic codes than CCI-defined renal disease. ICD-9 codes used for identification of renal impairment included 586 (unspecified renal failure), 585.x (chronic kidney disease [CKD]), 403.x (hypertensive CKD), 593.x (other disorders of kidney and ureter), 078.6 (hemorrhagic nephrosonephritis), 753.0 (congenital renal agenesis and dysgenesis), 753.1x (congenital cystic kidney disease), 250.4x (diabetes with renal manifestations), and 582.x (chronic glomerulonephritis). Overall and sex-specific prevalence estimates of seizure and renal impairment were calculated.
The number and percentage of patients prescribed more than one MS-specific disease-modifying treatments (DMTs), including interferon beta-1a, interferon beta-1b, glatiramer acetate, natalizumab, and fingolimod, during the 1-year preindex period are summarized. In addition, prescriptions for selected concomitant medications, including those known to lower seizure threshold, such as bupropion and tramadol, were analyzed. Because some antiepilepsy medications are also used for indications other than seizure, concurrent antiepilepsy medications were assessed to identify those that may be prescribed for conditions other than for seizure using the Thomson Reuters’ RED BOOK.7
Statistical comparisons were performed using χ2 test for categorical variables, Wilcoxon rank sum test for ordinal variables, and t-test for continuous variables. All data management and statistical analyses were performed using Version 9.1.3 of SAS (SAS Institute, Cary, NC, USA).
Results
A total of 929 patients identified from the medical claims with a diagnosis of MS were prescribed D-ER. Of these, 704 had at least 1 year of continuous enrollment prior to their initial D-ER prescription and were matched with the comparison group consisting of 1,403 D-ER-naïve MS patients; a match could not be identified for five of the patients in the D-ER-prescribed cohort.
Demographic characteristics of the cohorts are presented in Table 1. The mean age of patients prescribed D-ER was 55 years, with 71.6% of patients being between the ages of 45 years and 64 years; 71.6% of the patients were women. Neurologists were the primary prescribers, responsible for writing 79.1% of initial D-ER prescriptions.
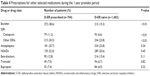
Prevalence of seizure and renal impairment
Prevalence estimates of seizure and renal impairment by age and sex are presented for the D-ER-prescribed and D-ER-naïve cohorts in Table 2. Among the 704 patients prescribed D-ER, 22 had a seizure-related diagnostic code prior to the initial D-ER prescription, resulting in an overall seizure prevalence estimate of 31 per 1,000 patients. The overall prevalence of seizure during the 1-year preindex period was higher among D-ER-naïve patients, at 47 per 1,000 patients; however, the difference between cohorts was not statistically significant.
When stratified by sex, the prevalence of seizure during the 1-year preindex period was numerically lower in women than in men prescribed D-ER (28 per 1,000 female patients versus 40 per 1,000 male patients), but higher in D-ER-naïve women (51 per 1,000 patients) compared with D-ER-naïve men (38 per 1,000 patients); neither of these differences was statistically significant.
The overall prevalence of renal impairment during the 1-year preindex period was numerically higher among D-ER-naïve patients (51 per 1,000 patients) compared with that among those prescribed D-ER (43 per 1,000 patients); however, this difference was not statistically significant. Comparison by sex showed that during the 1-year preindex period, the prevalence of renal impairment was lower in women than in men and that it was similar in women regardless of D-ER status. During the same preindex period, the prevalence of renal impairment in men was lower among patients prescribed D-ER (50 per 1,000 patients) compared with D-ER-naïve patients (73 per 1,000 patients).
Renal disorders during the 1-year preindex period was uncommon and significantly lower in patients prescribed D-ER compared with D-ER-naïve patients (1% versus 2.5%; P=0.02) (data not shown).
History of prescribed medications
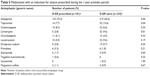
Prescriptions for MS-specific DMTs (initial or refill) during the 1-year preindex period are presented in Table 3. In general, the utilization of more than one DMT in the 1-year preindex period was significantly higher among patients prescribed D-ER than among D-ER-naïve patients (61.4% versus 41.2%). In particular, prescriptions for glatiramer acetate were nearly double for those who were prescribed D-ER (30.5%) than in the comparator group (16.1%).
|
Table 3 Prescriptions for MS-specific disease-modifying therapies during the 1-year preindex period |
Prescriptions for other medications during the 1-year preindex period for patients prescribed D-ER were generally higher than or approximately equal to those for D-ER-naïve patients. Specifically, prescriptions for baclofen were significantly higher for those prescribed D-ER compared with D-ER-naïve patients (38.6% versus 15.3%, respectively; P=0.01). Similarly, prescriptions for selective serotonin reuptake inhibitors antidepressants were significantly higher for patients prescribed D-ER compared with prescriptions for D-ER-naïve patients.
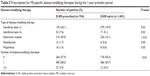
Overall, prescriptions for antiepileptics (Table 4) during the 1-year preindex period was 25.7% in those prescribed D-ER compared with 23.8% in D-ER-naïve patients (P=0.34). Among patients who were prescribed antiepileptics, a higher proportion was prescribed gabapentin in the D-ER cohort compared with the D-ER-naïve cohort (73.5% versus 65.6%; P=0.04; Table 5). Prescriptions for tramadol and bupropion, products having strong causal correlations with drug-associated seizure,8 were similar among MS patients regardless of D-ER prescription history, at approximately 6%–7%. Prescriptions for other medications with an indication for seizure were substantially lower across study cohorts regardless of D-ER status.
Discussion
A retrospective database study was conducted comparing MS patients prescribed D-ER with D-ER-naïve MS patients in an effort to better understand the descriptive epidemiology of these patients, assess the history of seizure and renal impairment prior to D-ER initiation, and examine the prescribing of MS-specific DMTs prior to D-ER initiation.
A primary emphasis of this study was to examine the prevalence of seizure and renal impairment in the year preceding D-ER initiation. Limitations on the use of medical billing claims data should be considered when interpreting these data because of the potential use of “rule out coding” by providers, which could improve reimbursement for diagnostic workups. This may overestimate the frequency of actual diagnosis by coding conditions as if they were established. In the year preceding D-ER initiation, the prevalence of seizure was numerically lower among patients prescribed D-ER (31 per 1,000 patients or 3.1%) than among D-ER-naïve patients (47 per 1,000 patients or 4.7%). The average seizure prevalence among MS patients is 3.1% (range: 2.3%–4.0%), calculated from six population-based studies; this is approximately threefold greater than the rate of seizure found in the general population.9 Although the differences in seizure rate between the D-ER cohort and the D-ER-naïve group were nonsignificant, the lower prevalence among D-ER users may suggest that the product label and REMS communication strategy in place at the time of this study were partially effective in controlling prescribing behavior to maximize product safety; nevertheless, some practitioners continue to prescribe D-ER to patients with a history of seizure.
Less is known about the epidemiology of renal impairment in people with MS. Although MS is associated with neurogenic bladder, renal dysfunction is not known to be a sequela of MS.10 In our study, the prevalence of renal impairment was numerically lower among MS patients prescribed D-ER (43 per 1,000 patients or 4.3%) than among D-ER-naïve MS patients (51 per 1,000 patients or 5.1%). Renal disorders were also lower among patients prescribed D-ER compared with D-ER-naïve patients (1% versus 2.5%, respectively). These results are difficult to put into context given the limited literature available in MS patients. In the general US population, an analysis of data from the National Health and Nutrition Examination Survey in the period 2001–2010 found that 10.2% of the US population aged 20 years or older had CKD (renal impairment) Stages 1–4.11 In MS patients, only one study on mild impairment was identified in the published literature, which reported that 36% (9/25) of the patients had mild impairment.10 Although the small number of patients included increases the variability of the estimate, these data indicate that the prevalence of mild renal impairment is higher in MS patients than in the general population.
D-ER therapy is contraindicated in patients with moderate or severe kidney disease. Therefore, the number of patients with renal impairment who are treated with D-ER is expected to be lower than that of the general MS population. The lower prevalence of renal impairment in patients using D-ER observed in this study suggests that product labeling and the REMS program in place at the time of this study may have contributed to the lower prevalence.
Prescriptions for MS-specific DMTs during the 1-year preindex period were higher for patients prescribed D-ER compared with that for D-ER-naïve patients, approximately 62% versus 45%, respectively; in particular, prescriptions for glatiramer acetate were nearly twice as high in D-ER users (Table 3). The clinical literature suggests that 50%–60% of MS patients use these therapies.12,13 DMT use in our study cohorts is similar to estimates in the clinical literature, but on opposite ends of the distribution. It is unclear why D-ER users were significantly more likely to be using DMTs than D-ER-naïve patients in this age-, sex-, and health insurance-source-matched analysis.
Antiepilepsy drugs were prescribed to approximately one-quarter of MS patients in the 1-year preindex period regardless of D-ER status. Among MS patients, neuropathic pain is likely to account for high use of antiepilepsy medications, which are recommended as treatment for a variety of neuropathic pain conditions.14 In particular, more than half of antiepilepsy prescriptions during the 1-year preindex period was attributable to gabapentin, a drug that is considered first-line treatment for chronic painful dysesthesia,15 which is the most common type of pain in MS patients.16 Additionally, other antiepilepsy drugs prescribed to our study population included carbamazepine, which is recommended for the treatment of trigeminal neuralgia in MS patients,15 and topiramate, which is also used to prevent migraine headaches.17
MS-related walking impairment has been associated with increased age and longer duration of disease,18 where the time duration from disease onset to Expanded Disability Status Score 6 (cane needed for walking) ranges from 16 years19 to 28 years.20 This in part may explain the high mean age of patients in this study.
Several limitations of this study should be noted, including that the medical claims component of the Medco database is available for only a subset of patients. Additionally, because claims data are primarily used for administrative purposes so that health care providers may obtain reimbursement for services, data errors regarding prescribing or diagnostic miscoding are possible. Claims data also limit the ability to examine the severity of MS disease progression as well as the extent of renal impairment. Another limitation of such database studies is the inability to link prescribing of medications with a particular condition, and this is relevant for interpretation of the results regarding use of antiepilepsy and other concomitant medications. Furthermore, analyses of pharmacy data assumes that patients who fill a prescription take the prescribed medication. Despite these limitations, the geographic distribution and the range of insurance sources represented in this study suggest generalizability of the results to other insured populations.
In conclusion, in this study population, D-ER is commonly prescribed to older MS patients who may have advanced disease. Although the prescribing of antiepileptics prior to D-ER initiation was substantial, these medications are commonly used for the treatment of MS-related pain. Seizure and renal impairment rates among D-ER-naïve patients were consistent with those in published literature, yet the rates among D-ER users during the 12-month period preceding D-ER initiation were slightly lower than the rates among D-ER-naïve patients, which could suggest that the risk minimization messages were somewhat effective.
Acknowledgments
This research was supported by Acorda Therapeutics, Inc. Editorial assistance was provided by The Curry Rockefeller Group, LLC, Tarrytown, NY, which was supported by Acorda Therapeutics, Inc, Ardsley, NY.
Disclosure
MJ and MS are employees and stockholders of Acorda Therapeutics, Inc; HH was an employee and stockholder of Acorda Therapeutics, Inc, at the time of this study. The authors report no other conflicts of interest in this work.
References
National Multiple Sclerosis Society.org. [Who gets MS? (Epidemiology)]. New York; 2014. Available from: http://www.nationalmssociety.org/What-is-MS/Who-Gets-MS. Accessed October 13, 2014. | ||
Waxman SG. Conduction in myelinated, unmyelinated, and demyelinated fibers. Arch Neurol. 1977;34(10):585–589. | ||
Frohman EM. Multiple sclerosis. Med Clin North Am. 2003;87(4):867–897, viii–ix. | ||
Ampyra® (dalfampridine) extended release tablets [prescribing information]. Ardsley, NY: Acorda Therapeutics, Inc; 2013. | ||
Haut S, Bienen EJ, Miller A. Clinical overview of the seizure risk of dalfampridine. Expert Opin Drug Saf. 2012;11(4):651–657. | ||
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. | ||
Red Book. Montvale, NJ: Thomson Healthcare; 2009. | ||
Zagaria MAE. Common causes of drug-induced seizures. US Pharm. 2010;35(1):20–23. | ||
Kelley BJ, Rodriguez M. Seizures in patients with multiple sclerosis: epidemiology, pathophysiology and management. CNS Drugs. 2009;23(10):805–815. | ||
Calabresi PA, Austin H, Racke MK, et al. Impaired renal function in progressive multiple sclerosis. Neurology. 2002;59(11):1799–1801. | ||
Kuznik A, Mardekian J, Tarasenko L. Evaluation of cardiovascular disease burden and therapeutic goal attainment in US adults with chronic kidney disease: an analysis of national health and nutritional examination survey data, 2001–2010. BMC Nephrol. 2013;14:132. | ||
Prescott JD, Factor S, Pill M, Levi GW. Descriptive analysis of the direct medical costs of multiple sclerosis in 2004 using administrative claims in a large nationwide database. J Manag Care Pharm. 2007;13(1):44–52. | ||
Minden S, Hoaglin D, Jureidini S, et al. Disease-modifying agents in the Sonya Slifka Longitudinal Multiple Sclerosis Study. Mult Scler. 2008;14(5):640–655. | ||
Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3 suppl):S3–S14. | ||
Pollmann W, Feneberg W. Current management of pain associated with multiple sclerosis. CNS Drugs. 2008;22(4):291–324. | ||
O’Connor AB, Schwid SR, Hermann DN, Markman JD, Dworkin RH. Pain associated with multiple sclerosis: review proposed classification. Pain. 2007;137(1):96–111. | ||
McDonagh M, Peterson K, Lee N, Thakurta S. Drug class review: antiepileptic drugs for indications other than epilepsy. Update 2. Portland, OR: Oregon Health & Science University; 2008. Available from: http://www.ncbi.nlm.nih.gov/books/NBK10371/pdf/TOC.pdf. Accessed October 13, 2014. | ||
Trojano M, Liguori M, Bosco Zimatore G, et al. Age-related disability in multiple sclerosis. Ann Neurol. 2002;51(4):475–480. | ||
Runmarker B, Andersen O. Prognostic factors in a multiple sclerosis incidence cohort with twenty-five years of follow-up. Brain. 1993;116(pt 1):117–134. | ||
Tremlett H, Paty D, Devonshire V. Disability progression in multiple sclerosis is slower than previously reported. Neurology. 2006;66(2):172–177. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.