Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Preoperatively elevated serum inflammatory markers increase the risk of periprosthetic joint infection following total knee arthroplasty in patients with osteoarthritis
Authors Xu C , Guo H, Qu PF , Fu J, Kuo FC , Chen JY
Received 31 May 2018
Accepted for publication 23 July 2018
Published 17 September 2018 Volume 2018:14 Pages 1719—1724
DOI https://doi.org/10.2147/TCRM.S175854
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Chi Xu,1 Heng Guo,1 Pengfei Qu,1 Jun Fu,1 Feng-Chih Kuo,2 Ji-Ying Chen1
1Department of Orthopedics, General Hospital of People’s Liberation Army, Beijing, China; 2Department of Orthopedic Surgery, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan
Background: The purpose of this study was to evaluate the prevalence of preoperatively elevated serum inflammatory markers and to determine its association with periprosthetic joint infection (PJI) in patients with osteoarthritis (OA) undergoing total knee arthroplasty (TKA).
Methods: From January 2010 to May 2014, we retrospectively reviewed 3,376 consecutive patients who were scheduled for unilateral TKA due to OA. Patients with inflammatory arthritis, posttraumatic arthritis, previous knee surgery, simultaneous surgery or arthroplasty, and comorbidity with autoimmune disease, hepatitis, renal disease, respiratory tract infections, urinary tract infection, and malignancy were excluded. One hundred and forty patients with preoperatively elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) were enrolled. The control group was matched by age, sex, body mass index, and year of index surgery in 1:1 ratio. All patients were followed for a minimum of 1 year or until the occurrence of PJI. PJI was defined based on the criteria in the International Consensus Meeting. A multivariate Cox proportional hazards model was utilized to calculate the HR and 95% CI.
Results: The prevalence of preoperatively elevated inflammatory markers was 4.1%. The rate of PJI was significantly higher in the both elevated ESR and CRP groups (12.5%, 4/32) compared with both normal group (1.4%, 2/140) and either high group (0.9%, 1/108) (P<0.001). Patients with preoperative elevated ESR and CRP had a significant risk of PJI compared to those with normal serum inflammatory markers (HR: 15.8, 95% CI: 2.57–96.7, P=0.003) after adjusting confounding factors. The cumulative rate for PJI was 6.3% (95% CI: 0%–14.27%) at 1 year and 16.5% (95% CI: 0%–30.66%) at 5 years for both high ESR and CRP groups, which was significantly higher than other 2 groups (P=0.0002).
Conclusion: Although the prevalence of preoperatively elevated ESR and CRP is low, routine examination of ESR and CRP preoperatively might be necessary to prevent subsequent PJI in patients with OA following TKA.
Keywords: erythrocyte sedimentation rate, C-reactive protein, periprosthetic joint infection, total knee arthroplasty, osteoarthritis
Background
Total knee arthroplasty (TKA) has been proven to be the most effective treatment for patients with end-stage joint disease.1 Although periprosthetic joint infection (PJI) is not a common complication of TKA, it is absolutely one of the most catastrophic. The incidence of PJI has been reported as 0.4%–2% after primary TKA.2 In order to prevent PJI, it is necessary for orthopedists to identify surgical contraindications. Studies have shown that several demographic factors and comorbidities are risk factors for PJI after TKA.3–5
Erythrocyte sedimentation rate (ESR) is a nonspecific hematological test used as an indirect parameter of increased acute-phase reactants,6,7 and C-reactive protein (CRP) is an acute-phase protein that is synthesized by the liver within 6 hours of the onset of inflammation.8,9 Both are simple, inexpensive, and readily available tests in clinical practice in the diagnosis of PJI and treatment efficacy of PJI by monitoring the trends. ESR/CRP combinations are cost-effective and accurate screening tools to rule out PJI in the postoperative periods.10,11 Normal trends of postoperative ESR/CRP following TKA have been well studied.12 However, the literature about preoperative abnormal ESR or CRP prior to TKA is limited.13,14 Except for physiological factors, some diseases commonly cause obvious changes in preoperative ESR and CRP levels, including trauma, urinary tract infection, hepatitis, malignancy, and inflammatory disease.15–17 Furthermore, several studies have revealed that ESR and CRP are slightly increased in knee osteoarthritis (OA) compared to knee non-OA patients.18,19 However, most orthopedic surgeons do not obtain preoperative ESR and CRP as a baseline to help evaluate potential postoperative surgical site infection. It remains unclear whether these patients with higher preoperative elevated serum inflammatory markers are more vulnerable to PJI after TKA.
The study aimed to investigate the prevalence of preoperatively elevated serum inflammatory markers and to evaluate whether they are associated with PJI in patients with OA following primary TKA.
Materials and methods
From January 2010 to May 2014, 3,796 consecutive patients (4,216 TKAs) were scheduled during the study period. Patients with comorbidities that caused elevated ESR and CRP were not included, including inflammatory arthritis, posttraumatic arthritis, autoimmune disease, hepatitis, renal disease, respiratory tract infections, urinary tract infection, and malignancy. Patients with previous surgery on the index knee, previous arthroplasty history, or bilateral knee OA were also excluded, resulting in 3,376 patients (3,376 unilateral TKAs). Among them, 140 patients with elevated preoperative serum markers were identified: 108 patients with elevated ESR or CRP and 32 patients with both elevations. For each case, we randomly assigned 1 control patient with normal preoperative ESR and CRP by age (±5 years), sex, body mass index (BMI; ±1 kg/m2), and year of index surgery (within 1 year). All patients were followed up for at least 1 year or until infection. This study was approved by the ethics committee of General Hospital of People’s Liberation Army, and written informed consent was obtained from the subjects.
Venous blood samples were obtained preoperatively at the day of admission. We used the Westergren method20 and nephelometric immune assay21 to determine ESR and CRP, respectively. Elevated ESR was defined as >30 mm/h,22 and elevated CRP was defined as >10 mg/L.23 If both ESR and CRP were elevated, an Infectious Diseases physician was consulted for evaluation of potential infection in the patients. Routine urinary analysis, anteroposterior chest radiography, and blood cultures were examined for those patients. None of these patients had any sign of infection at knee joints. The clinical records of these patients were manually reviewed in detail to extract relevant information that included patients’ demographic data, diabetes, smoking status, prior joint infection, and anesthesia type. Current smoking was defined as patients who had smoked within 1 year.
Operation
All patients received primary TKA in our hospital using a standard surgical technique. Preoperative antibiotic was administrated with 1 g of first-generation cephalosporin within 1 hour before skin incision. If patients have allergy to cephalosporin or penicillin or a high risk for methicillin-resistant Staphylococcus aureus colonization, 1 g of vancomycin was administered within 1 hour before skin incision. Redosing of preoperative antibiotics was considered in patients with body weight over 80 kg. The straight central skin incision and medial parapatellar arthrotomy were used with a tourniquet set up at 250 mmHg. Femoral, tibial, and patellar components were fixed with a handmade antibiotic-loaded bone cement. The deep fascia was repaired with #2 Quill (Depuy, Raynham, MA, USA) absorbable sutures and subcutaneous tissue was closed with simple interrupted # 2-0 Vicryl (VCP751D, Depuy) stitches with the knee at 30° of flexion. The skin was subsequently closed with a staple. Postoperative antibiotics were prescribed for <24 hours (given every 8 hours for 3 times). A wound drain was routinely used and removed on the first 24 hours after surgery.
Definition of PJI
PJI was defined by the International Consensus Meeting in 2013.24 A definite PJI is present when:
- There is a sinus tract communicating with the prosthesis, or
- A phenotypically identical pathogen is isolated by culture from 2 or more separate tissue or fluid samples obtained from the affected prosthetic joint, or
- When 3 of the following 5 criteria exist: 1) elevated serum ESR and serum CRP; 2) elevated synovial white blood cell count, or ++ change on leukocyte esterase test strip; 3) elevated synovial polymorphonuclear percentage; 4) positive histological analysis of periprosthetic tissue; and 5) a single positive culture.
Statistical analysis
Categorical variables were presented as frequencies and percentages, and continuous variables as means and SD. The clinical characteristics between groups were compared with the use of the ANOVA test for continuous variables and the chi-squared test for categorical variables. The effects of preoperatively elevated serum inflammatory markers on the development of PJI were evaluated with the use of Kaplan–Meier curves. Differences in the cumulative PJI rate were assessed using the log-rank test. HRs and 95% CIs for risk of PJI were estimated with the use of Cox proportional hazards models. Adjusted HRs for the development of PJI was expressed in a multiple Cox regression model after adjusting for age, sex, BMI, diabetes, smoking, prior joint injection, and anesthesia type. A P-value of <0.05 was considered significant. All the statistical analyses were performed with the statistical software packages R (http://www.R-project.org, The R Foundation, Vienna, Austria) and Empower Stats (http://www.empowerstats.com, X&Y Solution, Inc, Boston, MA, USA).
Results
The demographic data (age, gender, and BMI) did not differ significantly in 3 groups (Table 1). Diabetes, smoking status, and prior joint infection prior to TKA were similar between 2 groups. The mean ESR and CRP levels were significantly higher in the both high and either high group compared with normal ESR and CRP groups (P<0.001). Patients with both high preoperative ESR and CRP were prone to have regional anesthesia (P=0.021). The mean follow-up after TKA was 43.7±11.7 months (range 24–64 months).
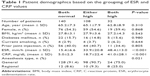  | Table 1 Patient demographics based on the grouping of ESR and CRP values |
The prevalence of preoperatively elevated inflammatory markers was 4.1%. The overall rate of PJI was 2.14% (6 of 280). The PJI rate was 0.7% (1/140) in the both normal ESR and CRP groups, 0.9% (1/108) in the either high ESR or CRP group, and 12.5% (4/32) in both elevated ESR and CRP groups (Figure 1). Patients with preoperative either high ESR or CRP did not have an increased risk of PJI in univariate and multivariate analyses (Table 2). However, patients with preoperative elevated ESR and CRP had a significant risk of PJI compared to those with normal preoperative ESR and CRP (HR: 18.5, 95% CI: 1.86–184.1, P=0.013) after adjusting for age, sex, BMI, diabetes, smoking status, prior joint injection, and anesthesia type.
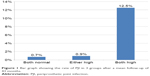  | Figure 1 Bar graph showing the rate of PJI in 3 groups after a mean follow-up of 43 months. |
When stratified by the groups, the cumulative rate for PJI was 0.7% (95% CI: 0%–2.10%) at 1 year and at 5 years for normal ESR and CRP groups, 0% (95% CI: 0%–0%) at 1 year and 1.22% (95% CI: 0%–3.57%) at 5 years for either high ESR and CRP group, and 6.3% (95% CI: 0%–14.27%) at 1 year and 16.5% (95% CI: 0%–30.66%) at 5 years for both high ESR and CRP groups (P=0.0002, Figure 2).
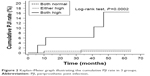  | Figure 2 Kaplan–Meier graph illustrating the cumulative PJI rate in 3 groups. |
Discussion
This comparative study revealed that preoperative elevated ESR and CRP may increase the rate of PJI in patients with OA following TKA. Patients with preoperative elevated ESR and CRP had a higher rate of PJI compared to those with preoperative normal ESR and CRP or with either high ESR or CRP at our institution. The study enrolled only OA patients and excluded possible preoperative factors that would increase the rate of PJI. Additionally, the types of anesthesia among the study were different between groups. However, the effect estimates did not change significantly after adjusting all confounders including anesthesia types. Studies have also shown that the use of different anesthesia types (general vs neuraxial anesthesia) is not associated with an increased rate of surgical site infection in patients undergoing total joint arthroplasty.25
In this study, we used preoperative ESR or CRP level to predict PJI rate in patients with OA undergoing primary TKA. We found patients with preoperative elevated ESR and CRP had an increased cumulated rate of PJI at 1 and 5 years. The early onset infection may be due to a more significant change of intraarticular immunological environment that is prone to pathogenic bacteria. One previous study used preoperative ESR and CRP to predict the postoperative complications in primary TKA.13 The author concluded that preoperative CRP and ESR analyses before elective TKA could not predict postoperative 90-day complications, including myocardial infarction, arrhythmia, pulmonary embolism, wound infection, acute renal failure, and reoperation. The reason for an increased risk of the late-onset infection in patients with high serum ESR and CRP levels prior to TKA is unknown. The rationale may be that such patients are poor-condition hosts who are more vulnerable to a hematogenous infection.
It has been shown that ESR and CRP levels can be influenced by, for instance, sex, age, and BMI.26–28 They also tend to be significantly raised in patients with infections, malignancies, or inflammatory diseases. In our study, these demographic factors were compared between groups, and the above diseases were excluded. Recent reports reveal that ESR and CRP are slightly elevated in OA. Hanada et al19 reported that CRP level was useful for assessing knee OA in early stages, but not in severe stages. ESR and CRP may increase in the presence of clinical symptoms such as tenderness, swelling, and patellar ballottement.29 We considered whether the elevated inflammatory markers affect the postoperative rate of infection. To the best of our knowledge, there is no study on this topic, except for 1 abstract in 2013 AAOS/AAHKS.30 In this abstract, the author found elevated ESR in 38.5% and CRP in 26.9% of 94 patients.
There are many studies on the cause of the elevated ESR and CRP in OA. Some researchers suggested that inflammatory mediators produced by intraarticular tissues caused the elevation of ESR and CRP levels.31,32 Saxne et al33 indicated the inflammation might possibly change the sensitivity of the cartilage to low-grade trauma in the early stage of OA. Through case history inquiries, we found that several patients had received intraarticular therapies in the case group. Some papers have reported injections prior to TKA were associated with increased risks of PJI.34 Cancienne et al35 used a national database to explore if there was an association between preoperative intraarticular knee injection at various time intervals prior to ipsilateral TKA and infection. Therefore, intraarticular injections may cause direct inoculation or hematogenous seeding of bacteria into knee joints, or activation of quiescent infection by the injected steroid, which lead to intraarticular inflammatory responses and elevated ESR and CRP levels.36,37
Several limitations of the current study should be considered. First, the design was retrospective and certain biases of retrospective study could not be avoided. Second, only 4 patients developed a PJI in both high groups during the follow-up, which might be an insufficient sample size for identification of association between both high serum ESR and CRP levels and the development of PJI. However, the effect estimates were consistent in both univariate and multivariate analyses despite the wide 95% CI. Further study should focus on investigating these relationships using a larger cohort. Third, the results were from a single institution. Last but not the least, patients with high serum ESR and CRP levels might have certain surgical contraindications. However, we informed the risk of infection to the patients and adapted every prophylactic method, including standard prophylactic antibiotics. Furthermore, we used antibiotic-loaded bone cement to prevent infection after TKA.
Conclusion
This study demonstrated preoperative elevated serum ESR and CRP level was a significant independent risk factor for PJI. We suggest that obtaining serum ESR and CRP data is necessary prior to primary TKA, and surgeons should be aware of this risk stratifying patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Seol JH, Seon JK, Song EK. Comparison of postoperative complications and clinical outcomes between simultaneous and staged bilateral total knee arthroplasty. J Orthop Sci. 2016;21(6):766–769. | ||
Garvin KL, Konigsberg BS. Infection following total knee arthroplasty: prevention and management. J Bone Joint Surg Am. 2011;93(12):1167–1175. | ||
Namba RS, Inacio MC, Paxton EW. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Joint Surg Am. 2013;95(9):775–782. | ||
Wu C, Qu X, Liu F, Li H, Mao Y, Zhu Z. Risk factors for periprosthetic joint infection after total hip arthroplasty and total knee arthroplasty in Chinese patients. PLoS One. 2014;9(4):e95300. | ||
Malinzak RA, Ritter MA, Berend ME, Meding JB, Olberding EM, Davis KE. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty. 2009;24(6 Suppl):84–88. | ||
Feldman M, Aziz B, Kang GN, Opondo MA, Belz RK, Sellers C. C-reactive protein and erythrocyte sedimentation rate discordance: frequency and causes in adults. Transl Res. 2013;161(1):37–43. | ||
Kainth MK, Gigliotti F. Simultaneous testing of erythrocyte sedimentation rate and C-reactive protein: increased expenditure without demonstrable benefit. J Pediatr. 2014;165(3):625–627. | ||
Rasmussen LA, Nielsen HJ, Sørensen S, et al. Ranitidine reduces postoperative interleukin-6 induced C-reactive protein synthesis. J Am Coll Surg. 1995;181(2):138–144. | ||
Magro F, Sousa P, Ministro P. C-reactive protein in Crohn’s disease: how informative is it? Expert Rev Gastroenterol Hepatol. 2014;8(4):393–408. | ||
Austin MS, Ghanem E, Joshi A, Lindsay A, Parvizi J. A simple, cost-effective screening protocol to rule out periprosthetic infection. J Arthroplasty. 2008;23(1):65–68. | ||
Parvizi J, della Valle CJ. AAOS Clinical Practice Guideline: diagnosis and treatment of periprosthetic joint infections of the hip and knee. J Am Acad Orthop Surg. 2010;18(12):771–772. | ||
Park KK, Kim TK, Chang CB, Yoon SW, Park KU. Normative temporal values of CRP and ESR in unilateral and staged bilateral TKA. Clin Orthop Relat Res. 2008;466(1):179–188. | ||
Godoy G, Sumarriva G, Ochsner JL, et al. Preoperative acute inflammatory markers as predictors for postoperative complications in primary total knee arthroplasty. Ochsner J. 2016;16(4):481–485. | ||
Ackland GL, Scollay JM, Parks RW, de Beaux I, Mythen MG. Pre-operative high sensitivity C-reactive protein and postoperative outcome in patients undergoing elective orthopaedic surgery. Anaesthesia. 2007;62(9):888–894. | ||
Piper KE, Fernandez-Sampedro M, Steckelberg KE, et al. C-reactive protein, erythrocyte sedimentation rate and orthopedic implant infection. PLoS One. 2010;5(2):e9358. | ||
Wolfe F. The many myths of erythrocyte sedimentation rate and C-reactive protein. J Rheumatol. 2009;36(8):1568–1569. | ||
Elgeidi A, Elganainy AE, Abou Elkhier N, Rakha S. Interleukin-6 and other inflammatory markers in diagnosis of periprosthetic joint infection. Int Orthop. 2014;38(12):2591–2595. | ||
Takahashi M, Naito K, Abe M, Sawada T, Nagano A. Relationship between radiographic grading of osteoarthritis and the biochemical markers for arthritis in knee osteoarthritis. Arthritis Res Ther. 2004;6(3):R208–R212. | ||
Hanada M, Takahashi M, Furuhashi H, Koyama H, Matsuyama Y. Elevated erythrocyte sedimentation rate and high-sensitivity C-reactive protein in osteoarthritis of the knee: relationship with clinical findings and radiographic severity. Ann Clin Biochem. 2016;53(Pt 5):548–553. | ||
Curvers J, Kooren J, Laan M, et al. Evaluation of the Ves-Matic Cube 200 erythrocyte sedimentation method: comparison with Westergren-based methods. Am J Clin Pathol. 2010;134(4):653–660. | ||
Bilgic F, Akinci Sozer O, Ozcan O, Gurpinar AB, Yilmaz H, Ay Y. Evaluation of inflammation during fixed orthodontic treatment. Arch Oral Biol. 2016;71:54–58. | ||
Caswell M, Pike LA, Bull BS, Stuart J. Effect of patient age on tests of the acute-phase response. Arch Pathol Lab Med. 1993;117(9):906–910. | ||
Parvizi J, Tan TL, Goswami K, et al. The 2018 Definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty. 2018;33(5):1309–1314. | ||
Parvizi J, Gehrke T; International Consensus Group on Periprosthetic Joint Infection. Definition of periprosthetic joint infection. J Arthroplasty. 2014;29(7):1331. | ||
Kopp SL, Berbari EF, Osmon DR, et al. The impact of anesthetic management on surgical site infections in patients undergoing total knee or total hip arthroplasty. Anesth Analg. 2015;121(5):1215–1221. | ||
Siemons L, Ten Klooster PM, Vonkeman HE, van Riel PL, Glas CA, van de Laar MA. How age and sex affect the erythrocyte sedimentation rate and C-reactive protein in early rheumatoid arthritis. BMC Musculoskelet Disord. 2014;15:368. | ||
Nestel AR. ESR adaptation for age – a forgotten pearl. BMJ. 2012;344:e1403–e1409. | ||
Oeser A, Chung CP, Asanuma Y, Avalos I, Stein CM. Obesity is an independent contributor to functional capacity and inflammation in systemic lupus erythematosus. Arthritis Rheum. 2005;52(11):3651–3659. | ||
Punzi L, Ramonda R, Oliviero F, et al. Value of C reactive protein in the assessment of erosive osteoarthritis of the hand. Ann Rheum Dis. 2005;64(6):955–957. | ||
American Association of Hip and Knee Surgeons and American Academy of Orthopaedic Surgeons. Preoperatively Elevated ESR and CRP in Total Knee Arthroplasty. 2013. Available from: https://www.medschool.lsuhsc.edu/orthopaedics/docs/Preoperatively%20%20Elevated%20ESR%20and%20CRP%20in%20Total%20Knee%20Arthroplasty%20AAHKS%20AAOS%202013.pdf. Accessed May 23, 2018. | ||
He Y, Siebuhr AS, Brandt-Hansen NU, et al. Type X collagen levels are elevated in serum from human osteoarthritis patients and associated with biomarkers of cartilage degradation and inflammation. BMC Musculoskelet Disord. 2014;15:309. | ||
Konttinen YT, Sillat T, Barreto G, Ainola M, Nordström DC. Osteoarthritis as an autoinflammatory disease caused by chondrocyte-mediated inflammatory responses. Arthritis Rheum. 2012;64(3):613–616. | ||
Saxne T, Lindell M, Månsson B, Petersson IF, Heinegård D. Inflammation is a feature of the disease process in early knee joint osteoarthritis. Rheumatology. 2003;42(7):903–904. | ||
Desai A, Ramankutty S, Board T, Raut V. Does intraarticular steroid infiltration increase the rate of infection in subsequent total knee replacements? Knee. 2009;16(4):262–264. | ||
Cancienne JM, Werner BC, Luetkemeyer LM, Browne JA. Does timing of previous intra-articular steroid injection affect the post-operative rate of infection in total knee arthroplasty? J Arthroplasty. 2015;30(11):1879–1882. | ||
Shemesh S, Heller S, Salai M, Velkes S. Septic arthritis of the knee following intraarticular injections in elderly patients: report of six patients. Isr Med Assoc J. 2011;13(12):757–760. | ||
Xu C, Peng H, Li R, et al. Risk factors and clinical characteristics of deep knee infection in patients with intra-articular injections: a matched retrospective cohort analysis. Semin Arthritis Rheum. 2018;47(6):911–916. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

