Back to Journals » Cancer Management and Research » Volume 11
Preoperative fasting hyperglycemia is an independent prognostic factor for postoperative survival after gallbladder carcinoma radical surgery
Authors Zheng P, Wang X, Hong Z, Shen F, Zhang Q
Received 26 October 2018
Accepted for publication 22 December 2018
Published 12 February 2019 Volume 2019:11 Pages 1425—1432
DOI https://doi.org/10.2147/CMAR.S192273
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Peng Zheng,1,* Xiaoqian Wang,2,* Zhong Hong,1 Feixia Shen,2 Qiyu Zhang3
1Department of Hepatobiliary Surgery, The Second Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, China; 2Department of Endocrinology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, China; 3Department of Hepatobiliary Surgery, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, China
*These authors contributed equally to this work
Background: Preoperative high blood glucose levels are closely associated with poor performance and high mortality in cancer patients. This study was designed to investigate the relationship between preoperative fasting hyperglycemia and the prognosis of patients with gallbladder cancer (GBC) after undergoing GBC radical surgery.
Patients and methods: A retrospective analysis of 83 eligible patients who underwent GBC radical surgery between 2007 and 2016 was performed. Factors affecting overall survival (OS) and recurrence-free survival (RFS) were analyzed by univariate and multivariate analyses.
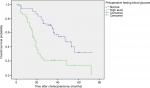
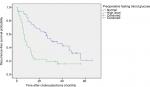
Results: Of the 83 patients, 35 (42.2%) had preoperative fasting hyperglycemia. The median OS of the enrolled patients was 12 months. The median OS in patients with fasting hyperglycemia before surgery was 18 months, which was shorter than for patients with normal fasting blood glucose levels before surgery (47 months, P<0.001). Preoperative fasting hyperglycemia was associated with shorter survival times in univariate analyses (HR, 3.215; 95% CI, 1.846–5.601; P<0.001). Multivariate analysis showed that patients with preoperative fasting hyperglycemia had a lower OS (HR, 2.832; 95% CI, 1.480–5.418; P=0.002) and RFS (HR, 2.051; 95% CI, 1.127–3.733; P=0.019) than patients with normal preoperative fasting blood glucose levels.
Conclusion: Preoperative fasting hyperglycemia is an independent indicator of poor prognosis in GBC patients after GBC radical surgery.
Keywords: fasting hyperglycemia, gallbladder carcinoma, GBC radical surgery, prognosis
Introduction
Gallbladder cancer (GBC) is the most common malignant tumor of the biliary tract, and it accounts for 80%–95% of biliary cancer cases.1 GBC is the fifth most common malignancy of the gastrointestinal tract, and it accounts for ~1% of all cancers in China.2 The prognosis of GBC is still poor because of atypical symptoms, late diagnosis, single treatment choices, and lack of effective diagnostic markers.3 Currently, the prognosis of GBC depends mainly on the pathologic detection of cancer tissue and distinguishing the stage, classification, and pathologic type of cancer to judge the prognosis of the patients. Epidemiologic studies have reported that the 3- and 5-year survival rates for patients with this disease are 30% and 5%.4 Therefore, given the poor prognosis for GBC in general, efforts to identify other factors that influence recurrence and patient survival are needed for this disease.
The relationship between diabetes and cancers has always been studied. A pooled analysis of a prospective cohort based on Asian populations shows that diabetes is closely associated with increased risk of multiple digestive tract tumors including esophageal cancer, gastric cancer, colon cancer, rectal cancer, liver cancer, cholangiocarcinoma, and pancreatic cancer.5 Another population-based case–control study in Shanghai, China, shows that diabetes is a risk factor for gallbladder cancer independent of body mass index (BMI), and its effect is mediated in part by biliary stones and serum high-density lipoprotein levels.6 The possible biologic links between diabetes and cancer are reported to be hyperinsulinemia, inflammation, and hyperglycemia.7
Positron emission tomography imaging using 18F-fluorodeoxyglucose has shown that tumor cells have higher blood glucose absorption than normal cells,8 and the plasma glucose levels in cancer patients may be an important prognostic indicator.9 Park et al found that stomach and lung cancer patients with a fasting serum glucose level above 126 mg/dL had higher mortality rates.10 Others have shown that the median survival period is significantly shorter for gastric adenocarcinoma patients who are GLUT-1-positive than for those who are GLUT-1-negative.11 The biologic cause of these clinical outcomes may be that glycolysis, as a biochemical feature of cancer, is primarily mediated by GLUT-1. GLUT-1 is a transmembrane transport protein that facilitates glucose transport into cells, and its expression is increased in epithelium-derived tumors, such as head and neck cancers and gastric and colorectal carcinomas.12,13 Regardless of whether GLUT-1 immunoreactivity was detected in GBC cases, patients with strong GLUT-1 expression had significantly shorter survival times after surgery than patients with negative or weak expression.14
Therefore, considering these results, we collected preoperative fasting blood glucose levels in patients who underwent gallbladder cancer surgery and their follow-up survival times. We hypothesized that preoperative fasting blood glucose levels are related to the prognosis of GBC and that higher preoperative blood glucose levels may have greater effects. Analyzing the prognosis of patients with GBC can improve the survival rate of patients by targeted improvements to postoperative patient care.
Patients and methods
This study was a retrospective study conducted in accordance with the Helsinki Declaration and approved by the Ethics Committee of the Second Affiliated Hospital of Wenzhou Medical University. All data were anonymized; therefore, patient consent was waived by the Ethics Committee of the Second Affiliated Hospital of Wenzhou Medical University. A total of 105 people were included in the study, and those without preoperative fasting blood glucose data, with evidence of other infectious diseases or who were lost to follow-up were excluded. Clinical data within 30 days before surgery for 83 of the patients were included. All clinical information and laboratory parameters were collected from the patients’ hospital medical records. All patients underwent radical operation for GBC during 2007–2016 at the Second Affiliated Hospital, Wenzhou Medical University. All final diagnoses were confirmed by pathologic examination. It is recommended that postoperative GBC patients receive corresponding adjuvant treatment according to their GBC stage and performance status. Abdominal computed tomography and blood indexes should be reviewed every 3 months for the first year after operation. Once each year, the patients were contacted by phone, and their recent physical condition was obtained. The date of follow-up was from the date of surgery to the date of death or last contact, or the end of September 2018. Overall survival (OS) was defined as the date from the surgery to the date of death or the last follow-up. Recurrence-free survival (RFS) was calculated from the date of surgery until the first relapse or death for any reason, or to the date of last follow-up.
Clinical information
The following medical data were retrospectively collected from the patients in the hospital: gender, age, BMI, hemoglobin, serum albumin, neutrophil-to-lymphocyte ratio (NLR), serum CA 19-9, serum carcinoembryonic antigen (CEA), pathologic data (tumor differentiation, tumor size, tumor lymph node metastasis), and TNM staging (The United States Joint Committee on Cancer [7th edition], staging of gallbladder cancer). Serum CA 19-9 and CEA levels were detected by electrochemiluminescence immunoassays (Cobas; Roche Diagnostics, Germany) performed at the Clinical Laboratory Department, Second Affiliated Hospital of Wenzhou Medical University, China. The normal reference values according to a previous study are as follows: CEA ≤5 µg/L, CA 19-9 ≤37 U/mL, NLR <2.6.15 The definition of radical resection is that the primary tumor is removed together with the metastatic lymph nodes and the affected tissue. (For the T1a GBC, we performed a simple cholecystectomy using a laparotomy or laparoscopic surgery. For the T1b GBC, we used an extended cholecystectomy. For patients with GBC in stage T2 or above, we usually perform an extended cholecystectomy. In the extended cholecystectomy, the gallbladder bed wedge resection or IVb/V liver resection can be performed according to the intraoperative condition. The scope of lymph node dissection should include the cystic duct lymph node, the common bile duct lymph node, the lymph nodes around the hepatoduodenal ligament [the hepatic artery and portal vein lymph nodes], and the posterior superior pancreaticoduodenal lymph node.) The tumor pathology shows that there is no tumor tissue at the margin.
Plasma glucose
Fasting plasma glucose (fasting for >8 hours) was determined from 5 to 6 am on any day before surgery as part of the preoperative laboratory tests. Normal fasting blood glucose levels range from 70 to 99 mg/dL (American Diabetes Association). Levels starting at 100 mg/dL indicate high blood glucose levels on an empty stomach, so fasting hyperglycemia is defined according to this threshold value. Accordingly, the patients were assigned to the fasting hyperglycemia group and the normal fasting blood glucose group. Among the fasting hyperglycemia group, only two patients were diagnosed with diabetes before enrolment and took insulin daily to control blood glucose.
Statistical method
For categorical variables, significant differences were assessed using the chi-squared test or Fisher’s exact test. For continuous data, the mean difference was compared using the Mann–Whitney test or independent-sample t-test. Univariate and multivariate Cox proportional hazard models were used to test the association between variables and OS. OS was calculated as the time from the date of surgery to the date of death from any cause or the last follow-up. Survival curves were analyzed by the Kaplan–Meier method and compared using the log-rank test. A P-value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 22 (SPSS, Lnc., Chicago, IL, USA).
Results
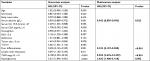
Table 1 shows the clinical and pathologic features of 83 patients. Of the 83 patients, 35 had preoperative fasting hyperglycemia (42.2%), most were female (60, 72.2%) and the average age was 66.1 years (SD =10.4). Gender (P=0.02), low hemoglobin (P=0.006), high NLR (P<0.001), and high CEA (P=0.002) were significantly different between the hyperglycemic patients and the normal blood glucose patients, which may affect patient preoperative glucose levels. Regarding tumor characteristics, advanced infiltration depth T (P=0.001), large tumor size (P=0.002), advanced TNM stage (P=0.002), and lymph node metastasis (P<0.001) had great influences in high fasting blood glucose levels. Other patient-related factors, such as age, serum albumin, BMI, serum CA 19-9 levels, the presence of stones, and tumor differentiation, were not associated with preoperative high blood glucose levels.
Of the 83 patients, 53 died, 4 were lost to follow-up, and 26 survived. For the OS (P<0.001) (Figure 1) and RFS (P<0.001) (Figure 2), the prognosis was significantly worse in patients with high fasting blood glucose levels than in patients with normal fasting blood glucose levels. Patients in the normal blood glucose level group had a median OS time of 47 months (95% CI, 31.69–62.30), and those in the preoperative fasting hyperglycemia group had a median OS of 18 months (95% CI, 15.183–20.817). The recurrence rate during follow-up in this study was 71.1% (59 patients), and the median disease-free survival in our series was 17 months. The median RFS was significantly shorter in the hyperglycemic group than in the normal blood glucose group (8 months and 31 months, respectively; P<0.001).
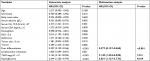
Table 2 shows the OS-related variables after GBC radical surgery according to univariate and multivariate Cox proportional hazard models. In the univariate analysis, preoperative fasting hyperglycemia, invasive depth III + IV, TNM III + IV, lymph node metastasis, poor differentiation, serum albumin levels, NLR ≥2.6, and CA 19-9 >37 U/mL were correlated with poor OS. Multivariate analysis identified that serum albumin (HR, 0.942; 95% CI, 0.895–0.992; P=0.022) and poor differentiation (HR, 0.233; 95% CI, 0.107–0.508; P<0.001) positively affected OS. However, TNM stage III + IV (HR, 8.024; 95% CI, 2.635–24.439; P<0.001) and hyperglycemia (HR, 2.832; 95% CI, 1.480–5.418; P=0.002) negatively impacted OS. Table 3 shows a univariate and multivariate Cox proportional hazard regression model for RFS. According to the univariate analysis, significant prognostic factors for RFS were preoperative fasting hyperglycemia, invasive depth III + IV, TNM III + IV, lymph node metastasis, poor differentiation, decreased serum albumin levels, NLR <2.6, and CA 19-9 >37 U/mL. Multivariate analysis identified two adverse prognostic factors, high blood glucose levels (HR, 2.051; 95% CI, 1.127–3.733; P=0.019) and TNM III + IV (HR, 3.140; 95% CI, 1.444–6.828; P=0.004), which affect RFS. Poor differentiation positively affected RFS (HR, 0.277; 95% CI, 0.137–0.560; P<0.001).
Discussion
GBC is a rare disease that is the most common invasive tumor in the biliary system.1,16 However, GBC progresses quickly and has few early symptoms.17 Therefore, early detection and early surgical treatment16 are advocated, but the prognosis for GBC remains poor. It is, thus, necessary to find new biomarkers that could be used for GBC prognosis. We found that preoperative fasting hyperglycemia is a poor predictor of OS and RFS in GBC patients after GBC radical surgery.
In our study, women with preoperative fasting hyperglycemia had a higher prevalence than those with normal blood glucose levels. However, according to univariate and multivariate analyses, gender is not an important predictor of OS difference. There was no correlation between preoperative fasting hyperglycemia levels and age, BMI, serum albumin levels, serum CA 19-9 levels, gallstones, or histopathologic differentiation. Although previous studies have shown that high preoperative fasting blood glucose levels are associated with lower serum albumin levels,18 we did not find a significant correlation between these parameters in our study. Some studies have also shown that the preoperative BMI level is associated with hyperglycemia in non-small-cell lung cancer patients.19 However, our study and Cai et al’s study confirmed that preoperative fasting hyperglycemia was not associated with BMI.18 However, our sample size is small, and the association between high preoperative fasting blood glucose levels and BMI should be further clarified with a larger sample size.
Gallstones are the main cause of GBC,20,21 but we did not find an association between gallbladder stones and overall OS or RFS in GBC patients undergoing GBC radical surgery. Preoperative fasting hyperglycemia was a poor predictor of overall OS and RFS in GBC patients who underwent GBC radical surgery. Compared to patients with normal fasting blood glucose levels before surgery, patients with preoperative fasting hyperglycemia had poorer GBC differentiation (P=0.005), higher possibilities to present lymph node metastasis (P<0.001), more advanced TNM staging (P=0.002), lower hemoglobin levels (P=0.006), higher NLR (≥2.6; P<0.001), higher serum CEA levels (P=0.002), greater tissue infiltration (P=0.001), and larger tumor size (P=0.002). However, in the study by Cai et al,18 hemoglobin levels were not associated with preoperative fasting hyperglycemia. The difference between our experiments may be related to the lymphoma itself, and a larger sample size is needed for verification. We found no correlation between the NLR and the long-term prognosis of gallbladder cancer, which is also different from Pang et al’s study.15
Glucose is a nutrient required for tumor growth, and the infinite growth characteristics of tumors have attracted great interest in the relationship between tumors and glucose.22 Studies have found that diabetes can increase the risk and mortality of several cancers, such as pancreatic cancer, liver cancer, and rectal cancer.23 Patients with type 2 diabetes often present with insulin resistance. Many studies have found that insulin-like growth factor and insulin resistance increase the prognosis and risk of some cancers.24 At the same time, diabetic patients have increased cardiovascular risk, delayed wound healing, increased risk of wound infection, arrhythmia, and delayed gastric emptying caused by neurologic complications, which affect the prognosis.25 Moreover, although hyperglycemia is a characteristic of metabolic disorders in diabetic patients,26 there are few studies on hyperglycemia and cancer. Recent studies have found that a high-sugar diet is associated with increased cancer cell proliferation,27 and hyperglycemia can synergize with cancer cell proliferation, migration, invasion, and recurrence.28 For example, in JAR cells, a choriocarcinoma cell line, the expression of glucose transporters is altered under hyperglycemic conditions. Increased glucose uptake and glycolysis rates29,30 have been shown in endometrial and breast tumors, and GLUT1 and GLUT3 expressions are higher in tumors with low differentiation.31 In addition, decreasing blood glucose levels during the remission period in gynecologic tumor patients are currently considered to be related to decreased GLUT1 expression.32 Hyperglycemia is also associated with cell proliferation, and studies have found that hyperglycemia regulates cyclin-dependent kinase 2, E2F, cycln A, and the cell cycle.27,33 In addition, hyperglycemia is important for cancer cells to synthesize DNA, RNA, and protein.34 The blood glucose concentration influences endometrial cancer cell proliferation and is positively correlated with endometrial cancer cell production,35 which is also associated with unrestricted cell growth due to the dysregulation of apoptosis.33 Recently, some studies have found that hyperglycemia and GBC are related.33 GLUT1 expression was also found in GBC and was associated with its prognosis.14 In addition, we found that miR-139-5p was significantly downregulated in GBC tissue and predicted poor prognosis. miR-139-5p overexpression directly inhibits PKM2 expression and regulates glycolysis.36
It is undeniable that our research has some shortcomings. For example, our study is a retrospective study, and the number of patients is not very large. All of the patients included in the study were Asian, and both diabetes and nondiabetes patients were included. Thus, we could not avoid the effects of the diabetes status. However, the patients included in the study were newly diagnosed patients with preoperative data, and we excluded pretreated patients. The blood glucose levels were also calculated using samples collected at 5–6 am after 8 hours of fasting, which reduced the variation caused by eating and the circadian rhythm effect on glucose metabolism.
Conclusion
This study demonstrates that preoperative fasting hyperglycemia is a reliable and objective indicator of GBC mortality and recurrence after GBC radical surgery. Preoperative fasting blood glucose levels can supplement clinical considerations for decision making in preoperative GBC patients. Further investigation is needed to better understand the mechanisms by which blood glucose levels are associated with clinical outcomes. In the future, we need to prospectively and continuously check the fasting blood glucose levels in the months and years after surgery to detect the relationships between the average fasting blood glucose concentration and the survival time and/or RFS.
Acknowledgment
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Peng Zheng and Xiaoqian Wang are co-first authors. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Lazcano-Ponce EC, Miquel JF, Muñoz N, et al. Epidemiology and molecular pathology of gallbladder cancer. CA Cancer J Clin. 2001;51(6):349–364. | ||
Legan M. Cyclooxygenase-2, p53 and glucose transporter-1 as predictors of malignancy in the development of gallbladder carcinomas. Bosn J Basic Med Sci. 2010;10(3):192–196. | ||
Xu WY, Zhang HH, Yang XB, et al. Prognostic significance of combined preoperative fibrinogen and CA199 in gallbladder cancer patients. World J Gastroenterol. 2018;24(13):1451–1463. | ||
Hu MT, Wang JH, Yu Y, et al. Tumor suppressor LKB1 inhibits the progression of gallbladder carcinoma and predicts the prognosis of patients with this malignancy. Int J Oncol. 2018;53(3):1215–1226. | ||
Chen Y, Wu F, Saito E, et al. Association between type 2 diabetes and risk of cancer mortality: a pooled analysis of over 771,000 individuals in the Asia cohort Consortium. Diabetologia. 2017;60(6):1022–1032. | ||
Shebl FM, Andreotti G, Rashid A, et al. Diabetes in relation to biliary tract cancer and stones: a population-based study in Shanghai, China. Br J Cancer. 2010;103(1):115–119. | ||
Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33(7):1674–1685. | ||
Do SK, Jeong JY, Lee SY. Glucose transporter 1 gene variants predict the prognosis of patients with early-stage non-small cell lung cancer. Ann Surg Oncol. 2018;25(11):3396–3403. | ||
Lamkin DM, Spitz DR, Shahzad MM, et al. Glucose as a prognostic factor in ovarian carcinoma. Cancer. 2009;115(5):1021–1027. | ||
Park SM, Lim MK, Shin SA, Yun YH. Impact of prediagnosis smoking, alcohol, obesity, and insulin resistance on survival in male cancer patients: National Health Insurance Corporation Study. J Clin Oncol. 2006;24(31):5017–5024. | ||
Kawamura T, Kusakabe T, Sugino T, et al. Expression of glucose transporter-1 in human gastric carcinoma: association with tumor aggressiveness, metastasis, and patient survival. Cancer. 2001;92(3):634–641. | ||
Noguchi Y, Marat D, Saito A, et al. Expression of facilitative glucose transporters in gastric tumors. Hepatogastroenterology. 1999;46(28):2683–2689. | ||
Haber RS, Rathan A, Weiser KR, et al. GLUT1 glucose transporter expression in colorectal carcinoma: a marker for poor prognosis. Cancer. 1998;83(1):34–40. | ||
Legan M, Tevžič S, Tolar A, Luzar B, Marolt VF. Glucose transporter-1 (GLUT-1) immunoreactivity in benign, premalignant and malignant lesions of the gallbladder. Pathol Oncol Res. 2011;17(1):61–66. | ||
Pang Q, Zhang LQ, Wang RT, et al. Platelet to lymphocyte ratio as a novel prognostic tool for gallbladder carcinoma. World J Gastroenterol. 2015;21(21):6675–6683. | ||
Kanthan R, Senger JL, Ahmed S, Kanthan SC. Gallbladder cancer in the 21st century. J Oncol. 2015;2015(10):1–26. | ||
Zhu AX, Hong TS, Hezel AF, Kooby DA. Current management of gallbladder carcinoma. Oncologist. 2010;15(2):168–181. | ||
Cai Q, Luo X, Liang Y, et al. Fasting blood glucose is a novel prognostic indicator for extranodal natural killer/T-cell lymphoma, nasal type. Br J Cancer. 2013;108(2):380–386. | ||
Luo J, Chen YJ, Chang LJ. Fasting blood glucose level and prognosis in non-small cell lung cancer (NSCLC) patients. Lung Cancer. 2012;76(2):242–247. | ||
Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome. Clin Epidemiol. 2014;6:99–109. | ||
Shen HX, Song HW, Xu XJ, et al. Clinical epidemiological survey of gallbladder carcinoma in northwestern China, 2009-2013: 2379 cases in 17 centers. Chronic Dis Transl Med. 2017;3(1):60–66. | ||
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. | ||
Suh S, Kim KW. Diabetes and cancer: is diabetes causally related to cancer? Diabetes Metab J. 2011;35(3):193–198. | ||
Giovannucci E, Insulin GE. Insulin, insulin-like growth factors and colon cancer: a review of the evidence. J Nutr. 2001;131(11 Suppl):3109S–3120. | ||
Cook KD, Borzok J, Sumrein F, Opler DJ. Evaluation and perioperative management of the diabetic patient. Clin Podiatr Med Surg. 2019;36(1):83–102. | ||
Heindel JJ, Blumberg B, Cave M, et al. Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol. 2017;68:3–33. | ||
Masur K, Vetter C, Hinz A, et al. Diabetogenic glucose and insulin concentrations modulate transcriptome and protein levels involved in tumour cell migration, adhesion and proliferation. Br J Cancer. 2011;104(2):345–352. | ||
Duan W, Shen X, Lei J, et al. Hyperglycemia, a neglected factor during cancer progression. Biomed Res Int. 2014;2014(4176):1–10. | ||
Young CD, Anderson SM. Sugar and fat – that’s where it’s at: metabolic changes in tumors. Breast Cancer Res. 2008;10(1):202. | ||
Rudlowski C, Moser M, Becker AJ, et al. GLUT1 mRNA and protein expression in ovarian borderline tumors and cancer. Oncology. 2004;66(5):404–410. | ||
Krzeslak A, Wojcik-Krowiranda K, Forma E, et al. Expression of GLUT1 and GLUT3 glucose transporters in endometrial and breast cancers. Pathol Oncol Res. 2012;18(3):721–728. | ||
Krone CA, Ely JT. Controlling hyperglycemia as an adjunct to cancer therapy. Integr Cancer Ther. 2005;4(1):25–31. | ||
Ryu TY, Park J, Scherer PE. Hyperglycemia as a risk factor for cancer progression. Diabetes Metab J. 2014;38(5):330–336. | ||
Piątkiewicz P, Czech A. Glucose metabolism disorders and the risk of cancer. Arch Immunol Ther Exp (Warsz). 2011;59(3):215–230. | ||
Han J, Zhang L, Guo H, et al. Glucose promotes cell proliferation, glucose uptake and invasion in endometrial cancer cells via AMPK/mTOR/S6 and MAPK signaling. Gynecol Oncol. 2015;138(3):668–675. | ||
Chen J, Yu Y, Chen X, et al. miR-139-5p is associated with poor prognosis and regulates glycolysis by repressing PKM2 in gallbladder carcinoma. Cell Prolif. 2018;51(6):e12510. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.