Back to Journals » Cancer Management and Research » Volume 13
Preoperative C-Reactive Protein/Albumin Ratio is a Prognostic Indicator for Survival in Surgically Treated Gastrointestinal Stromal Tumors: A Retrospective Cohort Study
Authors Cao X, Cui J, Li Z, Zhao G
Received 22 February 2021
Accepted for publication 10 May 2021
Published 24 May 2021 Volume 2021:13 Pages 4155—4167
DOI https://doi.org/10.2147/CMAR.S307873
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eileen O'Reilly
Xianglong Cao, Jian Cui, Zijian Li, Gang Zhao
Department of Gastrointestinal Surgery, Beijing Hospital, National Center of Gerontology; Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, People’s Republic of China
Correspondence: Gang Zhao Email [email protected]
Background: Systemic inflammation and malnutrition may promote tumor progression. C-reactive protein/albumin ratio (CAR) is linked to the poor long-term survival of several malignant tumors.
Purpose: To explore the predictive value of CAR in gastrointestinal stromal tumors (GISTs).
Methods: A retrospective study was conducted on 325 patients with primary GIST surgically treated with curative intent from 2009 to 2018. The cut-off point of CAR was set using X-tile software. Kaplan–Meier method and multivariate Cox regression model were used to study the prognostic value of CAR. The time-dependent receiver operating characteristic curve (tROC) was drawn, and the prognostic accuracy of CAR, Glasgow prognostic score (GPS), and National Institute of Health (NIH) risk classification was compared by the area under the curve (AUC).
Results: The best cut-off point of CAR was 0.55. Increased CAR was associated with the location of the lower digestive tract, larger tumor size, higher mitotic index, higher NIH risk classification, lower ALB, higher CRP, and higher GPS (all p< 0.05). Multivariable analysis revealed that CAR (hazard ratio [HR] 2.598, 95% confidence interval [CI] 1.385– 4.874; p=0.003) was an independent predictor of overall survival. Additionally, the AUC of CAR was lower than that of NIH risk classification at 2 years (0.601 vs. 0.775, p=0.002) and 5 years (0.629 vs 0.735, p=0.069). However, the AUC of NIH risk classification significantly increased (2-year OS 0.801, p=0.251; 5-year OS 0.777, p=0.011) when combined with CAR.
Conclusion: CAR is a new independent predictor of poor survival in patients with GIST. CAR combined with NIH risk classification can effectively improve the performance of prognosis prediction.
Keywords: gastrointestinal stromal tumor, C-reactive protein, C-reactive protein/albumin ratio, prognosis
Background
Gastrointestinal stromal tumors (GISTs) are the most frequent soft tissue sarcomas with an annual incidence in the United States of approximately 7 per million population.1 The incidence has risen slightly over the last decade.1 In China, due to the inaccuracy of provincial GIST registration data, the National Cancer Center’s annual report does not include the incidence of GIST. However, the incidence is estimated to be between 4.3 and 21.1 per million population.2 Surgery and targeted agent therapy have made progress, but the prognosis of GIST patients is still weak due to early recurrence or distant metastasis.3,4 Given GIST’s inconsistent biological behavior and variable response to treatment, it is critical to predict the risk of recurrence in GIST patients, and we need additional predictive and/or prognostic indicators to optimize management decisions, which include considering adjuvant therapy, optimizing treatment, evaluating the intensity of monitoring, and providing adequate patient counseling.
GIST prognostic systems have made great strides since the National Institute of Health (NIH) consensus criteria were introduced in 2002.5 Unlike many other malignant tumors that use the TNM system, GIST still retains a standardized and universally accepted prognostic system. Since gastrointestinal stromal tumors seldom spread via submucosal infiltration or lymphatic vessels, the commonly accepted UICC/AJCC TNM method for cancer has restricted use.6,7 The most widely used systems are the National Institute of Health (NIH),5 the Joensuu modified NIH,8 the Armed Forces Institute of Pathology (AFIP),9 and the Memorial Sloan Kettering Cancer Center (MSKCC) nomogram,10 Tumor size, location, and mitosis are the main variables used by these systems. However, which system is the most reliable is still a controversial issue.
Extensive studies have shown that inflammation and malnutrition may promote the occurrence, progression, and metastasis of malignant tumors.11–13 Several studies have identified that inflammatory markers based on white blood cells and acute-phase proteins are related to poor prognosis in various tumors.14–17 In recent years, the role of C-reactive protein (CRP) and albumin in the interaction network between systemic inflammatory response and cancer has attracted increased attention.18–20 Markers based on CRP and albumin, such as the Glasgow prognostic score (GPS) and its variants, are correlated with cancer patients’ long-term survival, including GIST.21–23 The CAR, a combination of serum CRP and albumin(ALB), has been used to assess cancer patients’ immunonutritional status and has recently been identified to be linked to the poor long-term survival of various malignant tumors.24–26 Accordingly, CAR may have a potential impact on predicting the long-term survival of GIST. CAR may be a promising prognostic marker based on inflammation in patients with radical resection of GIST. It may provide more prognostic information than the existing NIH risk classification system, help us identify high-risk patients more accurately, and may help to improve treatment decision-making and prognosis. However, to date, the predictive value of CAR on the survival of patients with GIST after curative resection remains poorly understood.
The current research’s primary aim was to investigate the prognostic value of preoperative CAR in patients with GIST who underwent radical resection. Besides, we evaluated the correlation between CAR and CRP, ALB, GPS, compared their predictive ability, and finally investigated whether CAR combined with NIH risk stratification system can improve its prognostic value.
Methods
Ethics Statement
All participants obtained the written informed consent that their data was kept in the hospital data bank and used for research approved by the Ethics Committee of the Beijing Hospital, the National Geriatrics Center. The data collection follows the Helsinki Declaration’s principles, following existing national legislation, and in line with the principle of protection of personal data.
Patients
From January 2009 to January 2018, a total of 325 patients with primary GIST who underwent open or laparoscopic surgery in the Department of Gastrointestinal Surgery of Beijing Hospital directly under the National Health Commission of China were considered included in this study.
The inclusion criteria were: (1) Pathologically diagnosed as GIST, with no distant metastasis; (2) underwent R0 resection;27 (3) ASA physical status before surgery were classified as I–III; (4) patients with detailed clinicopathological and preoperative serum laboratory data.
The exclusion criteria were as follows: (1) complicated with other primary malignant tumors; (2) infectious and non-cancerous inflammatory diseases; (3) Tumor rupture occurred during operation.
Data Collection and Definition
The pathological diagnosis and risk assessment of GIST is based on the latest version of the China guidelines.27 Patient characteristics assessed included age, gender, American Society of Anesthesiologists classification of physical status (ASA-PS) classification, tumor size, tumor location, mitotic index, and NIH risk classification. The preoperative physiological status of the patients was evaluated by the ASA-PS classification.28 The results of serum CRP and albumin were obtained within one week before the operation. The CAR was calculated as follows: CAR= serum CRP (g/L)/albumin (g/L); The GPS was categorized as: score 2 represented the decrease of albumin (<35g/l) and the increase of CRP (>10mg/l); score 1 represented normal albumin (≥35g/l) and the increase of CRP (>10mg/l); and score 0 represented normal albumin (≥35g/l) and normal CRP (≤10mg/l).29
Follow‐up
Routine follow-up included medical history (symptoms and physical examination), laboratory blood tests, abdominal and pelvic enhanced computed tomography (CT), or magnetic resonance imaging (MRI) scans. Intermediate- or high-risk patients had CT, or MRI scans every three months for three consecutive years, then every six months until the fifth year, and then once a year after that.27 Low-risk patients had CT, or MRI scans every six months for five years. For patients who could not be followed up in the outpatient clinic, we conducted a telephone follow-up. The overall survival (OS) time was defined as the surgery date with the most recent follow-up or death. The last follow-up was in December 2020.
Statistical Analysis
Using X tile software 3.6.1, we conducted an X tile plot analysis to determine the optimal CAR cutoff value for predicting five-year OS. The quantitative data was presented using the mean ± standard deviation. The Student’s t-test was used to evaluate the differences of continuous variables, while the Chi-square test was used to compare categorical variables. To evaluate the correlation between CAR and CRP, ALB, and GPS, Pearson r and Kendall tau correlation coefficients were calculated and their significance was determined. Survival analysis was performed by the Kaplan–Meier method with the Log rank test. We used the Cox proportional hazards model with a stepwise forward variable selection method to conduct univariate and multivariate survival analysis. We presented the hazard ratios (HR) derived from Cox analysis as relative risks and their associated 95% confidence intervals (CIs). The additive model was conducted to evaluate the interaction among subgroups to investigate whether other factors would affect the effect of CAR on OS. The prediction accuracy of different biomarkers was evaluated by time-dependent receiver operating characteristics (t-ROC) analysis. Statistical analysis was carried out with the SPSS version 26.0 (IBM Corporation, Armonk, NY, USA), the GraphPad Prism version 8.3.0 (GraphPad Software, Inc., San Diego, CA, USA), and the R software package version 4.0.2 (The R Foundation for Statistical Computing, Vienna, Austria; https://www.r-project.org/). Statistical significance was set at p < 0.05.
Results
Clinicopathological Characteristics
The detailed clinicopathological characteristics are summarized in Table 1. Of the enrolled 325 patients, 165 (50.7%) were males, and 160 (49.3%) were females. The average age of the patients was 60.28±11.97 (range, 24–85) years. Most of the patients, 79 (24.3%) and 184 (56.6%) cases, were ASA-PS grade I and II, and the other 62 (19.1%) cases were ASA-PS grade III. The stomach was the most common primary site (206 cases, 63.4%), followed by the intestine (64 cases, 19.7%), colorectum (23 cases, 7.1%), and extra-gastrointestinal tract (32 cases, 9.8%).
 |
Table 1 Relationship Between Clinical Characteristics and C-Reactive Protein/Albumin Ratio |
Based on tumor size, 73 (22.5%), 129 (39.7%), 75 (23.1%), 48 (14.7%) patients were divided into ≤2cm, 2.1–5cm, 5.1–10cm, >10cm groups, respectively. The median maximum tumor diameter was 4.0cm. According to Mitotic index, 196 (60.3%), 53 (16.3%), 76 (23.4%) patients were categorized into ≤5, 6–10, >10 per 50HPF groups, respectively. On the basis of the criteria of the NIH risk classification, 58 (17.8%), 93 (28.6%), 58 (17.8%), and 116 (35.7%) patients were grouped into very low-, low-, intermediate-, and high-risk groups, respectively.
The Best Cut-off Value of CAR, CRP, and ALB for Predicting OS
Using a X-tile analysis for predicting five-year OS we found 0.55 was the best cut-off value for CAR. Consequently, patients were separated into CAR-low (<0.55, n = 292) and CAR-high (≥0.55, n = 33) groups. We also determined that the best cut-off points of CRP and ALB were 18.20 and 35, respectively.
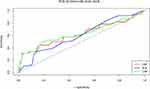
Time-dependent ROC analysis showed the areas under the curve (AUC) for 5-year OS were 0.633 for CAR (p=0.002), 0.628 for CRP (p=0.003), and 0.603 for ALB (p=0.027), respectively (Figure 1).
Correlation Between the CAR and Clinicopathological Factors
Contrasted with patients in the CAR-low category, those in the CAR-high category were more commonly to be found in the lower digestive tract (χ2=13.703, p = 0.003) and was prone to larger tumor size (χ2=25.270, p<0.001), higher mitotic index (χ2=10.344, p = 0.006) and higher NIH risk classification (χ2=15.298, p = 0.002). The CAR-high category also had significantly decreased ALB (χ2=32.823, p<0.001), increased CRP (χ2=249.581, p<0.001), and higher GPS (χ2=117.758, p<0.001). Table 1 compared the details between the two categories.
Furthermore, CAR was closely related to CRP (r=0.988; P <0.001), and GPS (Kendall’s tau-b=0.542, P<0.001). Besides, CAR and ALB had a significant negative correlation, but the correlation was weak (r=−0.275; P<0.001).
OS in the CAR-Low and CAR-High Categories
The median follow-up period was 64 months, of which 14 patients (42.4%) died in the CAR-high category and 40 patients (13.7%) in the CAR-low category. GIST relapsed in 73 cases (22.5%), including 15 cases (45.5%) in the CAR-high category. Overall, the one-year, three-year, and five-year OS rates were 93.8%, 83.9%, and 78.9%, respectively. In the Kaplan–Meier analysis, the CAR-high category (97.0%, 72.7%, and 57.0%, respectively) had a significantly shorter one-year, three-year, and five-year OS than the CAR-low category in the total cohort (99.0%, 93.8%, and 88.0%, respectively; p<0.001) (Figure 2A). Distinguished by the corresponding cut-off value (18.20 for CRP, 35.0 for ALB, and 1 for GPS), the five-year OS rate in the CRP-high category, the ALB-low category, and the GPS 2 category (62.5%, 69.3%, and 50.4%, respectively) was significantly lower than that in the CRP-low category, the ALB-high category and the GPS 0 or 1 category (87.7%, 86.6%, and 86.7%, respectively; p<0.001) (Figure 2B–D).
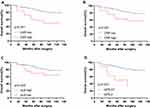 |
Figure 2 Kaplan–Meier survival curves of overall survival (OS) according to inflammation-based markers. Kaplan–Meier survival curves of OS according to CAR (A), CRP (B), ALB (C), and GPS (D). |
Univariate and Multivariate Analysis of OS
Univariate analysis indicated that ASA, PS score, CRP, ALB, CAR, GPS primary tumor size, tumor location, mitotic index, and NIH risk classification were all significantly correlated with OS (Table 2). The multivariable analysis determined that the CAR (HR 2.571, 95% CI 1.372–4.816; p=0.003) was an independent prognostic factor for overall survival after radical resection, followed by NIH risk classification (p<0.001) (Table 2).
 |
Table 2 Univariate and Multivariate Analysis of the Prognostic Factors for Overall Survival in Patients with GIST |
Survival Analysis of the Interaction Between CAR and Clinicopathological Factors
To further evaluate the prognostic value of CAR, we used univariate Cox regression for subgroup analysis to identify whether the effect of CAR on the overall survival of GIST patients was affected by other clinicopathological factors. In patients over the age of 60, there was a significant correlation between higher CAR and worse OS (p<0.001). This correlation is not significant in patients younger than the age of 60 (p=0.089). There was a strong association between higher CAR and worse OS in patients with tumors >5 cm (p=0.007). This association was not significant in patients with tumors ≤ 5 cm (p=0.892). There was a significant correlation between higher CAR and worse OS in patients with a mitotic index (per 50 HPF) >5 (p=0.001). This correlation was not significant in patients with a mitotic index (per 50 HPF) ≤ 5 (p=0.952). There was a clear relationship between higher CAR and worse OS in patients with non-gastric GIST (p=0.002). This relationship was not crucial in patients with gastric GIST (p=0.097). There was a significant correlation between higher CAR and worse OS in patients with moderate or high-risk (p=0.020). This correlation is not significant in patients with very low or low-risk (p=0.634) (Figure 3).
Subgroup Analysis According to NIH Risk Classification
In the intermediate or high-risk subgroup, the OS time of patients with high CAR was shorter (p = 0.001) (Figure 4B). However, there was no significant difference in overall survival between high and low CAR patients in a very low-risk or low-risk subgroup (p = 0.628) (Figure 4A).
Time-Dependent ROC Curve Analysis to Further Evaluate the Discriminating Ability of CAR
We conducted a time-dependent ROC analysis to evaluate the prediction accuracy of CAR, CRP, and GPS for OS (See Figure 5A). The AUC value of CAR at two years (0.601), and five years (0.629) was higher than that of CRP (2 years:0.593, p=0.077; and 5 years:0.618, p = 0.132) and GPS (2 year:0.566 p =0.398, and 5 years:0.619, p =0.903), but the difference was not significant.
Finally, we evaluated whether the combination of CAR and NIH risk classification could improve predicting prognosis accuracy. As presented in Figure 5B, the AUC value of CAR at two years (0.601,95% CI 0.491–0.711), and five years (0.629,95% CI 0.548–0.710) was lower than that of NIH risk classification (2 year:0.775, 95% CI 0.715–0.835, p=0.002; and 5 years:0.735, 95% CI 0.660–0.810, p = 0.069). However, when combined with CAR, the AUC value of the NIH risk classification increased (2-year OS 0.801, 95% CI 0.728–0.875, p=0.251; 5-year OS 0.777, 95% CI 0.696–0.857, p=0.011).
Discussion
This study set out to assess the prognostic value of preoperative CAR in GIST patients who underwent radical resection and compare it with proven markers of inflammation. The results show that preoperative CAR is an independent predictor for OS. Besides, CAR has better prognostic value in GIST patients with higher risk of recurrence. Moreover, Although the difference is not statically significant, CAR’s prediction accuracy appears to be superior to that of single systemic inflammation markers such as CRP and ALB, as well as compound markers such as GPS. Furthermore, CAR combined with NIH risk classification can effectively improve the prognostic prediction performance of standard NIH risk classification.
Extensive studies have shown that systemic inflammation plays an essential regulatory role in malignant tumors’ occurrence and development.30–32 Inflammatory factors, including acute-phase proteins such as C-reactive protein and albumin, may come from the systemic response to malignant tumors or from the secretion of malignant cells.33 The interaction between host and tumor cells may lead to tumor progression or retraction.33 Therefore, several studies support the theory that changes in systemic inflammatory factors have a particular prognostic value for cancer.14–17 To predict the prognosis of patients with malignant tumors more accurately and facilitate clinical application, recent studies have verified some inflammatory indicators obtained by routine serum examination, such as CRP, albumin, GPS and CAR.34–37
However, relatively few studies on these markers’ prognostic significance in patients with GIST, let alone CAR. CAR was initially developed to identify critically ill patients in emergency medical wards and predict 90-day mortality in patients with sepsis.38 Recent studies have reported that CAR has potential prognostic value in hepatocellular carcinoma, gastric cancer, and other malignant tumors.39 However, the effect of CAR on the long-term survival of patients with GIST is not apparent. Few studies have explored the prognostic influence of preoperative CAR in GIST patients undergoing surgery.40 In the field of GIST surgery, the current research established the clinical value of the preoperative CAR.
The current research indicates that CAR is an independent prognostic factor for OS in multivariate analysis. Similar to the results of this study, previous studies have confirmed that CAR was an independent prognostic factor in patients with esophagogastric junction (AEG) and upper gastric cancer (UGC).41 Another retrospective study of radical resection of 455 gastric cancer cases is also consistent with our results.42 This similarity may result from the chronic systemic inflammation induced by GISTs, the systemic immune response, or changes in the tumor microenvironment.
GPS is recognized and proved to be one of the best prognostic assessments based on inflammation in different tumors, including GIST.43 Therefore, it is imperative to compare the prediction ability of CAR and GPS. In this study, CRP, ALB, and GPS were also critical prognostic factors in univariate analysis. However, after using forward stepwise regression to control confounding factors in multivariate analysis, CAR was still a significant prognostic factor while GPS was not. These results are in agreement with those of Takahiro Toyokawa et al.44 They compared the preoperative inflammatory biomarkers in 225 patients with stage ш gastric carcinoma who underwent R0 resection. The results indicated that CAR was an independent predictor affecting OS and cancer-specific survival (CSS), while GPS was not. They found that the AUC of CAR and GPS was similar.
Additionally, there was a strong association between CAR and GPS. The reason GPS did not become an independent prognostic factor in the multivariate analysis might be that it has a strong association with CAR and its predictive ability is weaker than that of CAR. Therefore, we found that compared with the proven inflammatory marker GPS, CAR could also precisely predict the survival of patients with GIST after radical surgery. These results suggest that CAR is a new and more potential inflammation-based prognostic score in GIST.
Moreover, the CAR in the current study showed reasonable clinical practicability in patients with different clinical characteristics. ASA-PS in patients over the age of 60, there was a significant correlation between higher CAR and worse OS. This correlation is not significant in patients younger than the age of 60. However, this study also shows that high CAR is related to the tumor’s high degree of malignancy. The tumor microenvironment of gastrointestinal stromal tumors is often characterized by apparent inflammatory cell infiltration, but the mechanism and process of the interaction between inflammation and tumor are complex. Little is known about the mechanism by which systemic inflammation regulates tumor behavior and the host state.
Studies have found that CRP increases in patients with various tumors in recent years, which may be due to the systemic response to acute or chronic inflammation. As a typical manifestation of an acute response, the rapid increase of CRP is related to cytokines that promote inflammation, such as TNF-α and IL-6.33 Besides, DOG1 is a landmark protein of gastrointestinal stromal tumors (GIST), belonging to Ca2+-activated chloride channels and phospholipid disruptors. IL-6 can regulate cell death and tumorigenicity by regulating DOG1 and other signal transduction pathways.45 Moreover, the tumor microenvironment of GIST contains tumor-infiltrating immune cells, such as CD3+T cells. The type and number of tumor-infiltrating inflammatory cells are related to the malignant degree and prognosis of GIST. The prognosis of GIST patients with an increased number of CD3+T cells is better. The in-depth understanding of the mechanism of systemic inflammation provides an opportunity and theoretical basis for the development of an effective immunotherapy GIST.46 Therefore, CRP is increasingly widely used in monitoring cancer patients’ treatment and prognosis, including GIST.33
Albumin is closely related to nutritional status, and it is also a good indicator of immune status. Malnutrition is closely related to the decline of immune function, which will weaken the body’s antitumor immunity. Many studies have confirmed that hypoalbuminemia was correlated with poor prognosis in different tumors, including GIST.35,47,48
To sum up, high-risk GIST tumor cells have a high degree of malignancy, a high risk of tumor necrosis, and high tumor consumption, resulting in a high level of systemic inflammatory response characterized by increased CRP. The increase of CRP promotes tumor progression and metastasis through a variety of cytokines and signal transduction networks. Simultaneously, high-risk GIST will lead to severe malnutrition and even cachexia characterized by decreased serum albumin levels, weaken the immune system, and further accelerate tumor development. It explains why we observed different prognostic effects of CAR in high-risk and low-risk subgroups in the subgroup analysis. Because of the high risk of recurrence in patients with high CAR, perioperative TKI treatment may reduce recurrence and prolong survival. Besides, to detect these patients’ recurrence, early, more frequent follow-up should be considered.
Inevitably, several limitations should be noted. First of all, this is a single-center retrospective study in which samples are included. Data are collected for a relatively long time and may be affected by selection bias. Second, the limited sample size in this study is undoubtedly a drawback, as is the absence of an independent validation cohort; additionally, our results need confirmation in more extensive studies. Thirdly, although this study’s sample size is medium, there are only a small number of samples in some subgroups, which may affect observation results. Fourthly, current guidelines recommend that GIST patients who undergo R0 resection and have a moderate or high risk of recurrence receive adjuvant imatinib therapy. However, the situation of patients receiving TKI adjuvant therapy in this study has not been analyzed, which would inevitably lead to deviation in the process of survival analysis. Fifthly, the GIST in this study occurs in different organs, and its prognosis is significantly different, which may cause bias in statistical analysis. Finally, although the X-tile application can reduce the cut-off value fluctuation caused by the change of follow-up time, the optimal cut-off value of CAR may still change if the study population is different.42 Therefore, a universal threshold should be determined to distinguish GIST patients with a worse prognosis for further study. In the future, we will design more rigorous prospective studies, especially validation studies, to verify our preliminary results.
Conclusions
We determined that CAR is an independent prognostic factor for OS in patients with GIST after radical resection. CAR is significantly associated with CRP and GPS but weakly associated with ALB. The combination of CAR and NIH risk classification can effectively improve the accuracy of identifying high-risk patients with a worse prognosis. Therefore, CAR is a useful index to predict GIST’s prognosis and helps optimize postoperative treatment for patients with GIST in the future.
Data Sharing Statement
The original contributions proposed in the study are included in the article. For further inquiries, please contact the appropriate author.
Ethics Approval
This study involving human participants was reviewed and approved by the Beijing Hospital Ethics Committee.
Consent to Participate
The patient/participant provided a written informed consent form to participate in this study.
Consent for Publication (Including Appropriate Statements)
All authors contributed to this article and approved the submitted version for publication.
Acknowledgment
We are deeply grateful to all staff of the gastrointestinal department in the Beijing Hospital for their contributions and suggestions for this study.
Author Contributions
GZ and XC conceptualized the study and planned the test. XC drafted the manuscript and assisted with the data collection and study. The manuscript was reviewed and edited by GZ, JC, and ZL. JC and ZL were used to conduct the clinical investigation and record the data.XC, JC and ZL conducted data analysis and interpretation. GZ and JC provided suggestions and valuable comments for revising the first draft of this article. All authors, including GZ, XC, JC, and ZL, have reviewed and agreed on all versions of the article before submitting, during revision, accepting the final version of the release and any major changes introduced during the proofreading phase. All authors, including GZ, XC, JC and ZL, have agreed to submit their articles to the journal. All authors, including GZ, XC, JC and ZL, agree to take responsibility and be responsible for the content of this article.
Funding
There is no funding support for this study.
Disclosure
We do not have any potential conflict of interest in financial or personal relationships that will be biased toward our work. Commercial parties directly or indirectly related to our terms’ subject matter have not received or will receive any form of benefit. The authors claim that they have no competing interests.
References
1. Patel N, Benipal B. Incidence of Gastrointestinal Stromal Tumors in the United States from 2001–2015: a United States Cancer Statistics Analysis of 50 States. Cureus. 2019;11(2):e4120. doi:10.7759/cureus.4120
2. Li J, Shen L. The current status of and prospects in research regarding gastrointestinal stromal tumors in China. Cancer. 2020;126 Suppl 9:2048–2053. doi:10.1002/cncr.32684
3. Etherington MS, DeMatteo RP. Tailored management of primary gastrointestinal stromal tumors. Cancer. 2019;125(13):2164–2171. doi:10.1002/cncr.32067
4. Akahoshi K, Oya M, Koga T, Shiratsuchi Y. Current clinical management of gastrointestinal stromal tumor. World j Gastroenterol. 2018;24(26):2806–2817. doi:10.3748/wjg.v24.i26.2806
5. Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002;33(5):459–465. doi:10.1053/hupa.2002.123545
6. Agaimy A. Gastrointestinal stromal tumors (GIST) from risk stratification systems to the new TNM proposal: more questions than answers? A review emphasizing the need for a standardized GIST reporting. Int J Clin Exp Pathol. 2010;3(5):461–471.
7. Sobin LH, Compton CC. TNM seventh edition: what’s new, what’s changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer. 2010;116(22):5336–5339. doi:10.1002/cncr.25537
8. Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008;39(10):1411–1419. doi:10.1016/j.humpath.2008.06.025
9. Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23(2):70–83. doi:10.1053/j.semdp.2006.09.001
10. Gold JS, Gönen M, Gutiérrez A, et al. Development and validation of a prognostic nomogram for recurrence-free survival after complete surgical resection of localised primary gastrointestinal stromal tumour: a retrospective analysis. Lancet Oncol. 2009;10(11):1045–1052. doi:10.1016/s1470-2045(09)70242-6
11. McDowell SAC, Quail DF. Immunological Regulation of Vascular Inflammation During Cancer Metastasis. Front Immunol. 2019;10:1984. doi:10.3389/fimmu.2019.01984
12. Fonseca GW, Farkas J, Dora E. Cancer Cachexia and Related Metabolic Dysfunction. Int J Mol Sci. 2020;21(7). doi:10.3390/ijms21072321
13. Tuomisto AE, Mäkinen MJ, Väyrynen JP. Systemic inflammation in colorectal cancer: underlying factors, effects, and prognostic significance. World j Gastroenterol. 2019;25(31):4383–4404. doi:10.3748/wjg.v25.i31.4383
14. Dupré A, Malik HZ. Inflammation and cancer: what a surgical oncologist should know. Eur j Surgical Oncol. 2018;44(5):566–570. doi:10.1016/j.ejso.2018.02.209
15. Jagadesham VP, Lagarde SM, Immanuel A, Griffin SM. Systemic inflammatory markers and outcome in patients with locally advanced adenocarcinoma of the oesophagus and gastro-oesophageal junction. Br J Surg. 2017;104(4):401–407. doi:10.1002/bjs.10425
16. Gunnarsson U, Strigård K, Edin S. Association between local immune cell infiltration, mismatch repair status and systemic inflammatory response in colorectal cancer. J Transl Med. 2020;18(1):178. doi:10.1186/s12967-020-02336-6
17. Zhang K, Hua Y-Q, Wang D. Systemic immune-inflammation index predicts prognosis of patients with advanced pancreatic cancer. J Transl Med. 2019;17(1):30. doi:10.1186/s12967-019-1782-x
18. Fonseca GW, Farkas J, Dora E. Serum interleukin-6 and C-reactive protein are associated with survival in melanoma patients receiving immune checkpoint inhibition. J Immunotherapy Cancer. 2020;8. doi:10.1136/jitc-2020-000842
19. Baitar A, Kenis C, Decoster L. The prognostic value of 3 commonly measured blood parameters and geriatric assessment to predict overall survival in addition to clinical information in older patients with cancer. Cancer. 2018;124(18):3764–3775. doi:10.1002/cncr.31580
20. Chan SL, Chan AWH, Chan AKC. Systematic evaluation of circulating inflammatory markers for hepatocellular carcinoma. Liver Int. 2017;37(2):280–289. doi:10.1111/liv.13218
21. Dolan RD, McMillan DC. The prevalence of cancer associated systemic inflammation: implications of prognostic studies using the Glasgow Prognostic Score. Crit Rev Oncol Hematol. 2020;150:102962. doi:10.1016/j.critrevonc.2020.102962
22. McSorley ST, Black DH, Horgan PG, McMillan DC. The relationship between tumour stage, systemic inflammation, body composition and survival in patients with colorectal cancer. Clin nutrition. 2018;37(4):1279–1285. doi:10.1016/j.clnu.2017.05.017
23. Arigami T, Uenosono Y, Ishigami S. Clinical significance of the glasgow prognostic score in patients with gastrointestinal stromal tumors. Anticancer Res. 2016;36(12):6687–6690. doi:10.21873/anticanres.11279
24. Ishibashi Y, Tsujimoto H, Einama T. Correlation Between Immunoinflammatory Measures and Periostin Expression in Esophageal Squamous Cell Carcinoma: a Single-Center, Retrospective Cohort Study. Ann Surg Oncol. 2020. doi:10.1245/s10434-020-08765-3
25. Kudou K, Saeki H, Nakashima Y. C-reactive protein/albumin ratio is a poor prognostic factor of esophagogastric junction and upper gastric cancer. J Gastroenterol Hepatol. 2019;34(2):355–363. doi:10.1111/jgh.14442
26. Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Shibuya N, Kubota K. Clinical Significance of the C-Reactive Protein to Albumin Ratio for Survival After Surgery for Colorectal Cancer. Ann Surg Oncol. 2016;23(3):900–907. doi:10.1245/s10434-015-4948-7
27. Li J, Ye Y, Wang J, et al. Chinese consensus guidelines for diagnosis and management of gastrointestinal stromal tumor. Chine j Cancer Res. 2017;29(4):281–293. doi:10.21147/j.issn.1000-9604.2017.04.01
28. Sankar A, Johnson S, Beattie W, Tait G, Wijeysundera D. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth. 2014;113(3):424–432. doi:10.1093/bja/aeu100
29. McMillan D. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–540. doi:10.1016/j.ctrv.2012.08.003
30. Njunge L, Estania A, Guo Y, Liu W, Yang L. Tumor progression locus 2 (TPL2) in tumor-promoting Inflammation, Tumorigenesis and Tumor Immunity. Theranostics. 2020;10(18):8343–8364. doi:10.7150/thno.45848
31. Hamarsheh S, Zeiser R. NLRP3 Inflammasome Activation in Cancer: a Double-Edged Sword. Front Immunol. 2020;11:1444. doi:10.3389/fimmu.2020.01444
32. Tuomisto A, Mäkinen M, Väyrynen J. Systemic inflammation in colorectal cancer: underlying factors, effects, and prognostic significance. World j Gastroenterol. 2019;25(31):4383–4404. doi:10.3748/wjg.v25.i31.4383
33. Bruserud O, Aarstad H, Combined C-Reactive TT. Protein and novel inflammatory parameters as a predictor in cancer-what can we learn from the hematological experience? Cancers. 2020;12(7):1966. doi:10.3390/cancers12071966
34. Aarstad H, Guðbrandsdottir G, Hjelle K, et al. The biological context of C-reactive protein as a prognostic marker in renal cell carcinoma: studies on the acute phase cytokine profile. Cancers. 2020;12(7):1961. doi:10.3390/cancers12071961
35. Almasaudi A, Dolan R, Edwards C, McMillan D. Hypoalbuminemia Reflects nutritional risk, body composition and systemic inflammation and is independently associated with survival in patients with colorectal cancer. Cancers. 2020;12(7):1986. doi:10.3390/cancers12071986
36. Park J, Watt D, Roxburgh C, Horgan P, Colorectal Cancer MD, Inflammation S. Outcome: staging the Tumor and Staging the Host. Ann Surg. 2016;263(2):326–336. doi:10.1097/sla.0000000000001122
37. Xu B, Lu J, Zheng Z, et al. The predictive value of the preoperative C-reactive protein-albumin ratio for early recurrence and chemotherapy benefit in patients with gastric cancer after radical gastrectomy: using randomized Phase III trial data. Gastric Cancer. 2019;22(5):1016–1028. doi:10.1007/s10120-019-00936-w
38. Ranzani O, Zampieri F, Forte D, Azevedo L, Park M. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS One. 2013;8(3):e59321. doi:10.1371/journal.pone.0059321
39. Chen J, Fang A, Chen M, et al. A novel inflammation-based nomogram system to predict survival of patients with hepatocellular carcinoma. Cancer Med. 2018;7(10):5027–5035. doi:10.1002/cam4.1787
40. Xu HJ, Ma Y, Deng F, Ju WB, Sun XY, Wang H. The prognostic value of C-reactive protein/albumin ratio in human malignancies: an updated meta-analysis. Onco Targets Ther. 2017;10:3059–3070. doi:10.2147/ott.S137002
41. Kudou K, Saeki H, Nakashima Y, et al. C-reactive protein/albumin ratio is a poor prognostic factor of esophagogastric junction and upper gastric cancer. J Gastroenterol Hepatol. 2019;34(2):355–363. doi:10.1111/jgh.14442
42. Liu X, Sun X, Liu J, et al. Preoperative C-Reactive Protein/Albumin Ratio Predicts Prognosis of Patients after Curative Resection for Gastric Cancer. Transl Oncol. 2015;8(4):339–345. doi:10.1016/j.tranon.2015.06.006
43. Arigami T, Uenosono Y, Ishigami S, et al. Clinical Significance of the Glasgow Prognostic Score in Patients with Gastrointestinal Stromal Tumors. Anticancer Res. 2016;36(12):6687–6690. doi:10.21873/anticanres.11279
44. Toyokawa T, Muguruma K, Yoshii M, et al. Clinical significance of prognostic inflammation-based and/or nutritional markers in patients with stage III gastric cancer. BMC Cancer. 2020;20(1):517. doi:10.1186/s12885-020-07010-0
45. Kunzelmann K, Ousingsawat J, Benedetto R, Cabrita I, Schreiber R. Contribution of Anoctamins to Cell Survival and Cell Death. Cancers. 2019;11:3. doi:10.3390/cancers11030382
46. Tan Y, Trent J, Wilky B, Kerr D, Rosenberg A. Current status of immunotherapy for gastrointestinal stromal tumor. Cancer Gene Ther. 2017;24(3):130–133. doi:10.1038/cgt.2016.58
47. Hompland I, Ø B, Hølmebakk T, et al. Prediction of long-term survival in patients with metastatic gastrointestinal stromal tumor: analysis of a large, single-institution cohort. Acta oncologica. 2017;56(10):1317–1323. doi:10.1080/0284186x.2017.1330555
48. Jung A, Roh J, Kim J, et al. Prognostic value of body composition on recurrence and survival of advanced-stage head and neck cancer. Eur j Cancer. 2019;116:98–106. doi:10.1016/j.ejca.2019.05.006
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.