Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Preliminary study: comparative effects of lung volume therapy between slow and fast deep-breathing techniques on pulmonary function, respiratory muscle strength, oxidative stress, cytokines, 6-minute walking distance, and quality of life in persons with COPD
Authors Leelarungrayub J, Puntumetakul R , Sriboonreung T, Pothasak Y, Klaphajone J
Received 25 July 2018
Accepted for publication 30 September 2018
Published 5 December 2018 Volume 2018:13 Pages 3909—3921
DOI https://doi.org/10.2147/COPD.S181428
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Jirakrit Leelarungrayub,1 Rungthip Puntumetakul,2 Thanyaluck Sriboonreung,1 Yothin Pothasak,1 Jakkrit Klaphajone3
1Department of Physical Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand; 2Research Center in Back, Neck, Other Joint Pain and Human Performance (BNOJPH), Khon Kaen University, Khon Kaen, Thailand; 3Department of Rehabilitation Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Background: Lung volume therapy with the Voldyne® device can improve lung volume and has a nonsignificant benefit on respiratory muscle strength via the slow deep-breathing technique (SDBT); whereas respiratory muscle training with a respiratory muscle trainer via the fast deep-breathing technique (FDBT) has produced a significant improvement in people with COPD. Thus, the aim of this study was to compare the efficiency of lung volume therapy with the Voldyne® device with the SDBT and FDBT on pulmonary function, respiratory muscle strength, oxidative stress, cytokines, walking capacity, and quality of life (QoL) in people with COPD.
Methods: A total of 30 COPD patient volunteers with mild (stage I) to moderate (stage II) severity were randomized into two groups: SDBT (n=15) and FDBT (n=15). Pulmonary function (FVC, FEV1, and FEV1/FVC), maximal inspiratory mouth pressure (PImax), oxidative stress status (total antioxidant capacity [TAC], glutathione [GSH], malondialdehyde [MDA], and nitric oxide [NO]), inflammatory cytokines (tumor necrosis factor-alpha [TNF-α] and IL-6), 6-minute walking distance (6MWD), and total clinical COPD questionnaire (CCQ) score were evaluated before and after 4 weeks of training.
Results: All the parameters had no statistical difference between the groups before training. The PImax, TAC, IL-6, total QoL score, and 6MWD changed significantly in the SDBT group after the 4-week experiment as compared to those in the pre-experimental period, whereas FVC, FEV1, FEV1%, FEV1/FVC%, PImax, TAC, MDA, NO, TNF-α, IL-6, 6MWD, and total CCQ score changed significantly in the FDBT group as compared to those in the pre-experimental period. The FEV1%, PImax, TNF-α, IL-6, and total CCQ score differed significantly in the FDBT group in the post-experimental period as compared to those in the SDBT group.
Conclusion: This preliminary study concluded that the application of incentive spirometry with the Voldyne® device via fast deep breathing possibly improved respiratory muscle strength and QoL and reduced inflammatory cytokines, MDA, and NO better than that via slow deep breathing among people with COPD.
Keywords: COPD, cytokines, incentive spirometry, oxidative stress, 6-minute walking distance, quality of life
Introduction
COPD is currently a major and increasing health problem and will become the third most common disease leading to death worldwide, including Thailand, by 2020.1 Strong evidence has reported that pathophysiological changes are related to oxidative stress and inflammatory status in COPD,2 and endogenous oxidative stress is reportedly caused by ROS or reactive nitrogen species (RNS) generated by mitochondrial respiration and inflammatory responses to bacterial and viral infections within the lung.3 Both types of radicals are capable of causing oxidative damage to proteins, lipids, and DNA. Thus, a high level of lipid peroxide, malondialdehyde (MDA), or protein carbonyl and a low concentration of glutathione (GSH) or total antioxidant capacity (TAC) have been found in COPD patients3–5 and correlate significantly with disease severity or airflow obstruction.6 Previous reports have proposed that skeletal muscle wasting in COPD patients is related to the imbalance of oxidative stress status such as muscle atrophy and weight loss.7,8 Previous data showed that free radicals can be produced both at rest and during muscle contraction,9 which involves adaptation to the regular phenomena and influence of cellular processes in exercising muscles.10 In addition, a low level of ROS increases force production,11 whereas strong increases in ROS can cause contractile dysfunction, muscle atrophy and fatigue after strenuous exercise, aging, or diseases such as COPD, cancer, and heart failure.12,13 Previous evidence found that skeletal muscle fatigue or dysfunction correlated with the diaphragm muscle in COPD.14 Therefore, low physical activity levels and health-related quality of life (QoL) may be limited by dyspnea.15 In the case of the chronic inflammatory period in COPD, strong evidence indicated that many different cells and molecules respond to the inflammatory stage, especially the release of tumor necrosis factor-alpha (TNF-α) and IL-6.16 Previous data showed that the release of IL-6, which may attenuate TNF-α production, was induced by exercise,17 especially in COPD patients.18 Therefore, oxidative stress and inflammation are also provoked and have a high impact on patients with COPD.
Nowadays, conventional standard treatment and rehabilitation among COPD patients have been preferred to pulmonary rehabilitation with various programs such as respiratory therapy, education programs, psychological counseling, and general exercise.19,20 Moreover, the strengthening exercise program for both general extremities and respiratory muscles has been included, which suggests more improvement in physical exercise and ability to decrease exercise-induced oxidative stress damage.2,21 Respiratory muscle training (RMT), with specific devices, has confirmed the statistical efficiency of respiratory strength and other physical performances in COPD patients.22,23 Previous evidence suggests that training for a 5- to 10-week period with an inspiratory threshold loading device could increase peak inspiratory pressure (PImax) and lung volume by FVC or FEV1, as well as improve exercise capacity, dyspnea, and QoL.22,23 Unfortunately, the high cost of the RMT device dissuades many patients living in urban areas of low-economy countries from using it. Therefore, the RMT device is not used generally worldwide. However, conventional respiratory therapy for rehabilitation is still performed without a device for breathing training or with a specific device such as that in incentive spirometry (IS), especially for increasing lung volume and ventilation.24 It has been reported that in the case of high-risk pulmonary atelectasis post operation, prolonged bed rest, or restrictive lung defect, application of IS has been suggested.24 Nowadays, IS has been divided into two types, volume-oriented (Voldyne®) and flow-oriented (Triflo II®) devices, with different recommendations for use such as 10 breaths every 1–2 hours, 10 breaths five times a day, or 15 breaths every 4 hours. However, the guideline for using both devices has recommended slow deep breathing from normal exhalation. Previous evidence showed that Voldyne® IS improved chest wall volume more than Triflo II® IS in healthy adults,25,26 especially in patients who had suffered from a stroke.27 Voldyne® IS also increased chest wall volume more than Triflo II® IS in elderly subjects.28 Interesting results from a previous study by Paiva et al29 showed comparison between the inspiratory muscle trainer (IMT) with a threshold IMT® and Voldyne® for 30 days among healthy females. Although training with a threshold IMT® device presented more significant increase in PImax than that with Voldyne®, Voldyne® also showed a significant PImax improvement.29 This result is similar to that of a previous study by Ahmadi Hosseini et al who showed that 4 weeks of IS training with the slow deep-breathing technique (SDBT) in 15 COPD patients could increase PImax significantly, which was the same as training with the RMT device.30 Although the use of both devices has been instructed with slow and deep breathing,31 the IMT® device32 is preferred to the IS device, with fast and forced inspiration. The question remained as to whether PImax is more significant when using the IMT® device than when using the IS device, which may be due to different instructions and whether application of the Voldyne® device, with the fast deep-breathing technique (FDBT), can improve pulmonary function, respiratory muscle strength, and six-minute walking distance (6MWD). In addition, this device still causes oxidative stress and cytokine release among COPD patients. Previous evidence has shown that some adverse effects cause maximum sustainable voluntary ventilation to increase oxidative stress and cytokine release.33 This is consistent with an updated study of COPD patients performing slow-breathing yoga exercises, which increase inspiratory capacity and reduce dyspnea but do not involve oxidative stress or inflammation status.34 Therefore, the aim of this study was to evaluate the effects of lung volume therapy using the Voldyne® device with the FDBT and compare the outcomes with those of the SDBT.
Methods
Study design and subjects
The protocol in this study was approved by the ethic committee of the Faculty of Associated Medical Sciences, Chiang Mai University, Thailand (Study Code: AMSEC-60EX-060) and conducted in accordance with the Declaration of Helsinki (2001). The sample size of participants with COPD followed a previous study29 and was calculated by the G*Power (3.1.9.2) program with an effect size of 0.92, alpha error of 0.05, and power of 0.95. A minimum of 14 participants in each group was required for this study. A total of 30 COPD patients, who were living at home in Sansai district, Chiang Mai, Thailand, volunteered to take part in this study. Data collection and evaluation were performed at Ban Tor-Public Health Center, Sansai district, Chiang Mai, Thailand. All the participants signed a written consent form before the program started and were then divided randomly into two groups with matching stages between mild (stage I) and moderate (stage II) severity, after the repeated pulmonary function test according to the 2017 Global Initiative for Chronic Obstructive Lung Disease (GOLD),35 based on the value of predicted FEV1% and FEV1/FVC% ratio.
Furthermore, all the participants were permitted to receive medication in the form of either a long-acting inhaled bronchodilator or long-acting inhaled steroids prescribed by a physician if needed. All of them were ex-smokers and in stable clinical condition during the experiments. If they showed uncontrolled hypertension; unstable cardiac disease; recurrent symptoms of acute exacerbation or recurrent pneumothorax, thoracic, or chest pain including neuromuscular disorders; any liver or renal dysfunction; or endocrinal abnormalities, they were excluded from this study. Any supplements or special nutrients such as multi-vitamins or N-acetylcysteine compounds were not strictly prohibited, and the basic daily activities and behavioral aspects of the participants were controlled during the 4-week experiment. Health history and QoL were investigated by interview at baseline or on the pre-experimental day, and the characteristics such as height, weight, body mass index (BMI), and blood pressure were evaluated. Blood from the anterior cubital vein was taken and kept in sterile tube containing EDTA by a medical technologist for evaluating the complete blood count (CBC) by a fully automated Olympus AU400 Analyzer (Olympus Diagnostica GmbH, Umkirch, Germany) at the AMS Clinical Service Center, Faculty of Associated Medical Sciences, Chiang Mai University, Thailand. Residual blood from a previous collection was separated in order to determine the oxidative stress markers (TAC, GSH, MDA, and nitric oxide [NO]) and inflammatory cytokines (TNF-α and IL-6). Then, repeated evaluation of the pulmonary function stage was carried out using a spirometer (HI-105; Chest M.I., Inc, Tokyo, Japan) before evaluating the respiratory muscle strength from PImax (MicroRPM; Micro Medical Ltd., Kent, UK) and the 6MWD. All the participants were selected randomly into the SDBT or FDBT group.
Lung volume training with Voldyne® incentive spirometry
This study was designed in two different protocols: the SDBT and FDBT and the volume-oriented IS with the Voldyne® 5000 (Sherwood Medical, St Louis, MO). The target volume for the participants was set individually from the maximal vital capacity (VC) and pulmonary function test in the pretest period. The participants in either the SDBT24 or the FDBT36 group were instructed to take two to three cycles of normal breaths and perform maximal inspiration until the piston plate reached the target mark, and then, they tried to sustain inflation for at least 3 seconds before normal exhalation. In all, 30 breaths in three sets, with 2- to 3-minute intervals for rest, were designed to avoid possible hyperventilation or provoked dyspnea, and the rate of breathing was fixed at 20 breaths/minute. The total time for this program was twice daily, morning and evening, for 30 days. The participants performing SDBT had slow inspiration after regular exhalation, whereas those performing FDBT had fast inspiration after forced maximal exhalation. Thus, severe dyspnea from the category ratio of th Borg scale37 should be monitored for self-control symptoms during performance of the FDBT. During 1 month of the experiment, all the participants became educated about diseases and were permitted to carry out normal daily activities, except for regular or heavy exercise, or they practiced pursed lip breathing in cases when they felt dyspnea. Moreover, the caregivers strictly controlled the IS device by rechecking with daily telephone calls and making individual daily recordings in a logbook.
Outcome evaluation
Pulmonary function test
FVC, FEV1%, and the FEV1/FVC ratio were assessed in either liter or comparison with the predicted normal value, which was evaluated from the FVC maneuver in pneumatic-flow sensor spirometry (HI-105), performed under instructions from the American Thoracic Society (ATS) pulmonary function test.38 All the participants were required to wear a nose clip while sitting on a chair with a back for support. Careful instructions and coaching were given to prevent air leaks from around the flange of the mouthpiece. Three cycles of slow normal breaths were taken before performing maximal inhalation and exhalation and returning to normal breath. All data were printed after the test was completed. The highest liter value of FEV1 and FVC was selected finally from three repeated measurements in not more than eight tests.
Respiratory muscle strength test
Respiratory muscle strength was evaluated by measuring the maximal inspiratory mouth pressure (MIP or PImax) at residual volume in sitting position by using a portable handheld mouth pressure meter (MicroRPM). All the participants were seated with nose clips on, and the flange of the mouthpiece was used in order to prevent air leaks, as required. A sharp, forceful effort was maintained in each test for a minimum of 3–4 seconds. Furthermore, the interval for rest between each effort was 1–3 minutes or more if dyspnea symptoms were presented. The highest data output in units of centimeter water (cmH2O) from three repeated efforts or a drop of more than 20% from the previous effort was the criterion for stopping the procedure.38,39
Oxidative stress and cytokine evaluation
Whole blood of 400 μL was taken from residual blood to evaluate the GSH by 5,5′-dithiobis-2-nitrobenzoic acid (DTNB) reagent,40 and the residual blood was used to separate plasma by centrifugation at 3,000× g for 10 minutes. Fresh plasma was used to evaluate the TAC by 2,2′-azino-bis (3-ethylbenzothiazoline-6-sulfonic acid) (ABTS) decolorization protocol41 and NO by Griess reagent.42 Other plasma was frozen for determining the inflammatory cytokines (TNF-α and IL-6) using human ELISA kits (Quantikine®; R&D systems, Inc., Minneapolis, MN) and MDA by thiobarbituric acid (TBA) reactive substances.43 All the parameters were evaluated experimentally at the Biomechanics Laboratory of the Department of Physical Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Thailand.
6MWD test
The 6MWD test was evaluated by following the guideline of the 2002 ATS.44 A modified protocol of the 20-meter straight walking test, with turn around points marked at the end by colored tape, was performed in an indoor corridor. Any vigorous activities and eating 2 hours before the test were avoided. Comfortable clothes and shoes could be worn during the test, and vital signs such as respiratory rate, oxygen saturation, heart rate, and blood pressure were evaluated before and after it for safety reasons. The participants were instructed to walk at a comfortable pace for 6 minutes under the supervision of a physiotherapist and allowed to stop and rest during the test if feeling strong or heavy dyspnea (equal to 6 from the maximal 10 of the Borg scale), in accordance with the guideline of the American College Society of Medicine (ACSM).45
QoL evaluation
QoL was assessed using the Clinical COPD Questionnaire (CCQ),46 which consisted of 10 questions in three domains: four items of symptoms, two items of mental state, and four items of functional state. The questions were asked 1 week before starting the test or before the experiments in this study, and the 7-point score from 0 to 6 was used. The CCQ held the total score in the main measurement of outcome, calculated as the mean sum of all items, whereas each item was calculated with the highest value presenting the worst health status and the lowest value presenting the best one.47
During 4 weeks of training, a self-reporting logbook was kept and rechecked by the caregivers, as well as reverified every 2 weeks of the experiment by a physical therapist using phone calls and personal appointments at Ban Tor-Public Health Center.
Statistical analyses
All the data were analyzed statistically for normal distribution using the one-sample Kolomogorov–Smirnov test before presenting as mean, with SD, and minimal and maximal values. The characteristics between the two groups were analyzed by the independent t-test. The data of pulmonary function, PImax, oxidative stress parameters, cytokines, QoL, and 6MWD between the groups before and after 4 weeks of training were analyzed by two-way ANOVA measurement (two groups and two times). All statistical analyses were carried out using the SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA) for Windows. All the tests were used with significance at a P-value of <0.05. Moreover, the effect size from the results within a group with a Cohen value (d) was analyzed by the G*Power program 3.1.9.2, which showed three levels: small (d=0.2), moderate (d=0.5), and large (d>0.8). Therefore, the moderate to large effect size and the results of significant value indicated credible statistical analysis despite the small sample size in this study.48
Results
Characteristic results
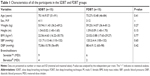
The results of CBC in all the participants were within the reference value in the pre-experimental period (data not shown). The two groups were well matched regarding age, weight, height, BMI, and blood pressure, with no significant difference between them (Table 1). All the parameters (FVC, FEV1, FEV1/FVC ratio, PImax, 6MWD, and total CCQ), all oxidative stress markers (TAC, GSH, NO, MDA, and cytokines), TNF-α, and IL-6 were not statistically different at the baseline data in either group (P>0.05; Figures 1–3). In addition, all the data showed normal distribution due to nonsignificant results from the one-sample Kolomogorov–Smirnov test (P>0.05). Therefore, the data were expressed as mean and SD.
Pulmonary function and respiratory muscle strength results
There were no statistical changes in any lung functions in the SDBT group, whereas FVC (L; P=0.001), FEV1 (L; P=0.000), and FEV1 (%; P=0.000) changed significantly in the FDBT group (Figure 1A–C) with a large effect size (d=1.0, d=1.15, and d=1.39), and the FEV1/FVC% (P=0.036; Figure 1D) had a moderate effect size (d=0.59; Table 2). The FVC (L), FEV1 (L), and FEV1/FVC% were not significantly different between the groups in the post-training period, except for the result of FEV1% (P=0.017). Regarding results for respiratory muscle, both training groups showed a significant increase in PImax, SDBT, P=0.01 and d=0.76, and FDBT, P=0.001 and d=1.15. PImax in the FDBT group was significantly higher than that in the SDBT group when compared with the post-training period (P=0.019; Table 2 and Figure 1E).
Oxidative stress and inflammatory cytokine results
There was no significant change in the GSH level in either group between the pre- and post-training periods. TAC significantly increased in both training techniques: SDBT, P=0.002 and FDBT, P=0.000 (Figure 2A), with a large effect size (d=0.99 and d=1.91, respectively; Table 3), but with no significant difference (P=0.237) between the groups in the post-training period. MDA and NO reduced significantly in only the FDBT group (P=0.005 and P=0.005, respectively; Figure 2B and C) with a large effect size (d=0.85 and d=2.60, respectively; Table 3), but there was no significant difference from those of the SDBT group. The result of TNF-α showed a significant change in the FDBT group (P=0.000; Figure 2D) with a large effect size (d=2.01; Table 3), whereas no change occurred in the SDBT group (P=0.059). Both groups showed a significant reduction in IL-6 levels (P=0.024 and P=0.000; Figure 2E) with a moderate effect size (d=0.68) and large effect size (d=2.08), respectively (Table 3). In addition, the IL-6 level in the post-training period was significantly lower in the FDBT group than in the SDBT group (P=0.017).
6MWD and QoL results
After 4 weeks of training, the 6MWD significantly increased in both groups (P=0.034 and P=0.000; Figure 3A) with a moderate effect size (d=0.63) and large effect size (d=1.87) in the SDBT group and FDBD group (Table 4), respectively, but there was no significant difference between the two groups in the post-training period (P=0.269). Regarding results for QoL, both techniques reduced the total QoL score significantly when compared with that of pre-training (P=0.003 and P=0.001; Figure 3B) with a large effect size (d=0.97 and d=1.10), as well as reduced the sub-item symptom score (P=0.028 and P=0.001) with a moderate effect size (d=0.66) and large effect size (d=1.07) in the SDBT and FDBT groups (Table 4), respectively. The FDBT group showed a reduction in sub-item mental and function scores (P=0.045 and P=0.026) with a large effect size (d=1.13) and moderate effect size (d=0.62), but there were no significant changes in the SDBT group. When comparing between the groups in the post-training period, the scores of total CCQ, symptom, and function were significantly different (P=0.021, P=0.017, and P=0.08, respectively; Table 4).
Discussion
The results of this study offer a preliminary presentation of the different effects of instruction for IS application between the SDBT and FDBT. Previous recommendations of IS application can improve lung volume by slow deep inspiration from functional residual capacity (FRC) or at the end of regular exhalation according to the American Association for Respiratory Care (AARC) Clinical Practice Guideline.24 It has been proposed that the clinical benefit of IS improves lung volume and prevents atelectasis in various conditions such as post coronary artery bypass grafting (CABG).24 The Voldyne® device, which is classified as volume-oriented IS, seems to have more benefits than flow-oriented IS such as the Triflo® II device.25 Previous data reported that the Voldyne® device improved chest wall volume in healthy adults,26 elderly subjects,27 and patients with stroke.28 In 2015, the study of Paiva et al29 showed that the Voldyne® device can be applied for training the strength of respiratory muscles in healthy females25 and COPD patients.30 PImax is the principle parameter of respiratory muscle strength, and it must be evaluated and increased after application. Unfortunately, increasing PImax after applying the Voldyne® device was not similar to training with a threshold IMT® device. Therefore, different instructions may be provided for IS and threshold IMT® devices.32 All the participants in this study were instructed to take two to three cycles of normal breaths before slow or fast deep inspiration or breathing from residual volume in 30 continuous breaths. Rest intervals of 2–3 minutes were permitted in each cycle of 10 breaths, at the slow rate of 20 breaths per minute, for preventing dyspnea symptoms. The visual target for maximal effort in all the participants was at the maximal volume in the piston plate marked beside the Voldyne® device, which had been fixed closely in order to equal the maximal VC from the pulmonary function test in the pre-experimental period.
Although the number of participants with COPD was small in this study (15 in each group), it may be enough for statistical results, as a previous study was carried out with 13 COPD patients.29 Furthermore, Heydari et al49 also had 30 COPD patients divided into two groups (n=15) to study the efficiency of inspiratory-resistive muscle training using incentive spirometry within 4 weeks of training.
The main parameters were PImax, which indicated the respiratory muscle strength and pulmonary function; FVC; FEV1; and FEV1/FVC in either liter or percentage of the predicted values. The results showed that both the SDBT and FDBT increased PImax significantly, with a large effect size, but PImax increased more with the FDBT than with the SDBT. Although the mechanism of the FDBT improves PImax better than the SDBT, this is still unclear. However, the high forcing technique in the FDBT is the same as that performed in the RMT device and is possibly expected to induce respiratory muscle strength quickly. Regarding results of the lung function, the SDBT did not improve any of the pulmonary parameters, whereas the FDBT improved them significantly, except for FVC%. When comparing the data between the two tests in the post-experimental period, the FEV1% showed a significant difference. Thus, the FDBT did not affect any of the pulmonary function parameters, except FEV1%. These results are similar to those in a previous study in 2015 by Heydari et al,49 who compared incentive spirometry with the inspiratory muscle training program, and the result showed improvement in peak expiratory flow rate (PEFR). The improvement of lung function in the FDBT group could be explained from the instruction of fast, quick, and deep breathing, which may stimulate respiratory muscle function; thus, the PImax result in the FDBT group showed a higher increase than that in the SDBT group. Although previous evidence suggested that both IS volume and flow-oriented IS can encourage the subject to inhale to lung capacity through maximal inspiration, aided by visual feedback, these maneuvers increase transpulmonary pressure and lung volume and induce greater lower inspiratory muscle activity.50 However, volume-oriented IS has more effect on chest wall volume in elderly people than flow-oriented IS.28 Therefore, the Voldyne® device is classified in the volume-oriented IS possibly because of having more effect on chest wall volume. Another mechanism of increased PImax may be explained by a previous study on animals by Rollier et al51 who found that low load inspiratory muscle training increased diaphragmatic fiber dimensions in a rat model. Thus, breathing exercise with IS in either the SDBT or FDBT is the same as low load inspiratory muscle training. Unfortunately, it is still unclear why the FDBT increased respiratory muscle strength more than the SDBT because respiratory muscle activation should be evaluated directly with surface electromyography (EMG).
COPD has high potential of oxidative stress and inflammation,2 and whether it may be induced by the FDBT is a concern. Oxidative stress markers such as MDA, GSH, and TAC3,30 and inflammatory markers such as TNF-α and IL-616 can be evaluated in COPD patients.18 The SDBT possibly does not affect oxidative stress because of its non-aggressive protocol, which is similar to that in a previous study of slow-breathing yoga exercises in COPD patients.34 While previous evidence proposed that maximum sustainable voluntary ventilation increases oxidative stress and cytokine release,33 the FDBT may affect oxidative stress, and this should be evaluated. Results from this study showed that TAC had a low increase level but presented with a significantly large effect size from both the SDBT and FDBT. However, there was no statistical difference between the two groups in the post-experimental period. In their earlier interesting study, Martarelli et al52 found improvement in antioxidant defenses and decreased oxidative stress via the cortisol and melatonin hormone pathway from diaphragmatic breathing exercise, which may support the result of TAC in this study. In addition, MDA and NO levels decreased significantly in only the FDBT group after the experiment, but there was no significant difference between the groups in the post-experimental period. However, the improvement of MDA and NO from the FDBT is very interesting and should be studied further. A previous study in hemodialysis patients showed that RMT did not affect the MDA level;53 thus, some mechanisms may reduce MDA and NO production. Interesting results of MDA and NO levels, when applied to the FDBT, significantly reduced both parameters with possible clinical benefits because high NO and MDA are related to disease severity and airflow obstruction.6 Therefore, reduction of NO and MDA in this study possibly helped to prevent exacerbation of the disease. Furthermore, the result of significant TNF-α reduction in the FDBT and IL-6 in both groups is also very interesting and cannot be explained. However, some evidence reported that the signaling pathway of TNF-α release is sensitive to ROS.54 Moreover, IL-6 has been claimed to affect airway limitation and emphysema progression.55 Thus, reduction of plasma IL-6 in this study possibly delays the disease progression in the clinic. However, further study on the mechanisms involved in changes in both cytokines by the FDBT is still needed. Previous evidence reported that these cytokines did not respond to either the high or low intensity of IMT in patients with chronic heart failure for 10 weeks.56 However, this study was performed with COPD patients who had a different condition. Therefore, a study of the FDBT on oxidative stress and cytokine response, especially antioxidant enzymes or the signaling pathway on cytokine release, should be carried out.
In addition, the clinical efficiency from both techniques has been studied with 6-minute walking capacity and QoL. The 6MWD provides information regarding functional capacity and response to training. Previous evidence suggested that a distance of <350 m is associated with a higher mortality in COPD patients,57 and previous data claimed that the clinically important difference for 6MWD should be 53 m.58,59 Therefore, IS application in the FDBT increased the 6MWD from 307.87±70.41 m to 362±67.58 m, which indicated a clinically significant improvement as compared to that in the SDBT (303.14±121.01 m–324.50±108.66 m). Dominant response to the 6MWD in the FDBT group is related possibly to the results of PImax, oxidative stress, and cytokines, when compared with SDBT results. This hypothesis can be believed because of a previous study that found association between the 6MWD and inspiratory VC.60 Therefore, increased 6MWD may be the result of increased PImax data. Finally, the QoL confirmed efficiency of the training, and both groups had a significantly decreased score that showed improvement in QoL. The CCQ was used in this study because of its short items and time-saving interview, with only 10 items consisting of symptom, mental state and functional state. Previous evidence showed that the CCQ significantly correlated with the St George’s Respiratory Questionnaire (SGRQ), COPD assessment (CAT), and modified Medical Research Council scale.61 The results showed improvement in the total CCQ score, which was the same as that in the sub-item symptom score. The mental score was not significantly different in either group. However, the sub-item function score showed a significant improvement in the FDBT group. Moreover, the total CCQ score, symptoms, and function in the FDBT group were significantly different to those in the SDBT group in the post-experimental period. Therefore, significant changes possibly correlate with FEV1%, PImax, oxidative stress, and cytokines.
Clinical application and limitations
This preliminary study design did not include control participants, but they might not have been necessary as the COPD patients were in a stable condition. Berodual® and Seretide™ bronchodilators were used in both groups depending on occasional symptom aggravation. The influence of medications during lung volume therapy may have impacted the results, thus, should be studied in the future. In addition, this study aimed to show the clinical benefits of lung volume therapy with the Voldyne® device between slow and fast deep breathing. Therefore, the significant difference between the two groups was enough. The fast deep-breathing protocol twice daily for 30 days in the COPD patients had more clinical benefits in FEV1, PImax, QoL, and walking distance than the slow deep-breathing protocol. Instruction of IS with fast, quick, and deep breathing maneuver, as in the RMT protocol, can be applied in the clinic. Improvement of PImax and FEV1 is very challenging when compared with the conventional SDBT. However, most of the participants in this study were classified as stage II (moderate severity), and the low sample size with mixed females and males was a limitation. Application of IS with FDBT to other stages such as severe COPD or patients diagnosed with predominant emphysema is also not predicted. Future research regarding the study of COPD patients, with a larger sample size, varied severity, and combination medications, is still needed for possible application in various conditions.
Conclusion
This preliminary study of patients with COPD can conclude that application of incentive spirometry with the Voldyne® device via fast deep breathing seems to improve respiratory muscle strength and QoL and reduce inflammatory cytokines, MDA, and NO better than that via slow deep breathing.
Acknowledgments
This study was given a grant from the Research Center in Back, Neck, Other Joint Pain and Human Performance (BNOJPH), Khon Kaen University, Khon Kaen, Thailand. The authors thank all the participants and caregivers for their assistance in helping to control and organize the training with good consistency. Thanks also go to all the physical therapists at Sansai Hospital, Chiang Mai, who organized space for collecting data.
Disclosure
The authors report no conflicts of interest in this work.
References
Cosio MG, Saetta M, Agusti A. Immunologic aspects of chronic obstructive pulmonary disease. N Engl J Med. 2009;360(23):2445–2454. | ||
Domej W, Oettl K, Renner W. Oxidative stress and free radicals in COPD – implications and relevance for treatment. Int J Chron Obstruct Pulmon Dis. 2014;9:1207–1224. | ||
Kirkham PA, Barnes PJ. Oxidative stress in COPD. Chest. 2013;144(1):266–273. | ||
Ahmad A, Shameem M, Husain Q. Altered oxidant-antioxidant levels in the disease prognosis of chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2013;17(8):1104–1109. | ||
Nadeem A, Raj HG, Chhabra SK. Increased oxidative stress and altered levels of antioxidants in chronic obstructive pulmonary disease. Inflammation. 2005;29(1):23–32. | ||
ben Anes A, Fetoui H, Bchir S, et al. Increased oxidative stress and altered levels of nitric oxide and peroxynitrite in Tunisian patients with chronic obstructive pulmonary disease: correlation with disease severity and airflow obstruction. Biol Trace Elem Res. 2014;161(1):20–31. | ||
Rahman I, Morrison D, Donaldson K, Macnee W. Systemic oxidative stress in asthma, COPD, and smokers. Am J Respir Crit Care Med. 1996;154(4 Pt 1):1055–1060. | ||
Barreiro E. Protein carbonylation and muscle function in COPD and other conditions. Mass Spectrom Rev. 2014;33(3):219–236. | ||
Reid MB, Haack KE, Franchek KM, Valberg PA, Kobzik L, West MS. Reactive oxygen in skeletal muscle. I. Intracellular oxidant kinetics and fatigue in vitro. J Appl Physiol. 1992;73(5):1797–1804. | ||
Steinbacher P, Eckl P. Impact of oxidative stress on exercising skeletal muscle. Biomolecules. 2015;5(2):356–377. | ||
Smith MA, Reid MB. Redox modulation of contractile function in respiratory and limb skeletal muscle. Respir Physiol Neurobiol. 2006;151(2–3):229–241. | ||
Reid MB. Free radicals and muscle fatigue: Of ROS, canaries, and the IOC. Free Radic Biol Med. 2008;44(2):169–179. | ||
Vollaard NB, Shearman JP, Cooper CE. Exercise-induced oxidative stress: myths, realities and physiological relevance. Sports Med. 2005;35(12):1045–1062. | ||
Supinski G, Nethery D, Dimarco A. Effect of free radical scavengers on endotoxin-induced respiratory muscle dysfunction. Am Rev Respir Dis. 1993;148(5):1318–1324. | ||
Lacasse Y, Martin S, Lasserson TJ, Goldstein RS. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane systematic review. Eura Medicophys. 2007;43(4):475–485. | ||
Heidari B. The importance of C-reactive protein and other inflammatory markers in patients with chronic obstructive pulmonary disease. Caspian J Intern Med. 2012;3(2):428–435. | ||
Petersen AM, Pedersen BK. The role of IL-6 in mediating the anti-inflammatory effects of exercise. J Physiol Pharmcol. 2006;57:43–51. | ||
van Helvoort HA, van de Pol MH, Heijdra YF, Dekhuijzen PN. Systemic inflammatory response to exhaustive exercise in patients with chronic obstructive pulmonary disease. Respir Med. 2005;99(12):1555–1567. | ||
Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary rehabilitation; Joint ACCP/AACVPR Evidence-based clinical practice guidelines. Chest. 2007;313:4S–42S. | ||
Mikelsons C. The role of physiotherapy in the management of COPD. Respir Med. 2008;4(1):2–7. | ||
Mercken EM, Hageman GJ, Schols AM, Akkermans MA, Bast A, Wouters EF. Rehabilitation decreases exercise-induced oxidative stress in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;172(8):994–1001. | ||
Geddes EL, Reid WD, Crowe J, O’Brien K, Brooks D. Inspiratory muscle training in adults with chronic obstructive pulmonary disease: a systematic review. Respir Med. 2005;99(11):1440–1458. | ||
Leelarungrayub J, Pinkaew D, Puntumetakul R, Klaphajone J. Effects of a simple prototype respiratory muscle trainer on respiratory muscle strength, quality of life and dyspnea, and oxidative stress in COPD patients: a preliminary study. Int J Chron Obstruct Pulmon Dis. 2017;12:1415–1425. | ||
Restrepo RD, Wettstein R, Wittnebel L, Tracy M. Incentive spirometry: 2011. AARC Clinical practice guideline. Respir Med. 2011;56:1600–1604. | ||
Paisani DM, Lunardi AC, da Silva CC, Porras DC, Tanaka C, Carvalho CR. Volume rather than flow incentive spirometry is effective in improving chest wall expansion and abdominal displacement using optoelectronic plethysmography. Respir Care. 2013;58(8):1360–1366. | ||
Parreira VF, Tomich GM, Britto RR, Sampaio RF. Assessment of tidal volume and thoracoabdominal motion using volume and flow-oriented incentive spirometers in healthy subjects. Braz J Med Biol Res. 2005;38(7):1105–1112. | ||
Lunardi AC, Porras DC, Barbosa RC, et al. Effect of volume-oriented versus flow-oriented incentive spirometry on chest wall volumes, inspiratory muscle activity, and thoracoabdominal synchrony in the elderly. Respir Care. 2014;59(3):420–426. | ||
Lima IN, Fregonezi GA, Melo R, et al. Acute effects of volume-oriented incentive spirometry on chest wall volumes in patients after a stroke. Respir Care. 2014;59(7):1101–1107. | ||
Paiva DN, Assmann LB, Bordin DF, et al. Inspiratory muscle training with threshold or incentive spirometry: Which is the most effective? Rev Port Pneumol. 2015;21(2):76–81. | ||
Ahmadi Hosseini SH, Farzac M, Heydari A. Comparing the effect of resistive inspiratory muscle training and incentive spirometry on respiratory pattern in COPD patients. Evi Based Care J. 2016;6:45–54. | ||
Beaumont M, Mialon P, Le Ber-Moy C, et al. Inspiratory muscle training during pulmonary rehabilitation in chronic obstructive pulmonary disease: A randomized trial. Chron Respir Dis. 2015;12(4):305–312. | ||
Gosselink R, de Vos J, van den Heuvel SP, Segers J, Decramer M, Kwakkel G. Impact of inspiratory muscle training in patients with COPD: what is the evidence? Eur Respir J. 2011;37(2):416–425. | ||
Mills DE, Johnson MA, Mcphilimey MJ, et al. Influence of oxidative stress, diaphragm fatigue, and inspiratory muscle training on the plasma cytokine response to maximum sustainable voluntary ventilation. J Appl Physiol. 2014;116(8):970–979. | ||
Kaminsky DA, Guntupalli KK, Lippmann J, et al. Effect of Yoga Breathing (Pranayama) on Exercise Tolerance in Patients with Chronic Obstructive Pulmonary Disease: A Randomized, Controlled Trial. J Altern Complement Med. 2017;23(9):696–704. | ||
Global Initiative for Chronic Obstructive Lung Disease [homepage on the Internet]. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. 2017. Available from: https://goldcopd.org. Accessed November 16, 2018. | ||
Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969;99(5):696–702. | ||
Borg G. Borg’s perceived exertion and pain scales. Champaign, IL: Human Kinetics; 1998. | ||
American Thoracic Society (ATS). Standardization of spirometry, 1994 update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:1107–1136. | ||
Evans JA, Whitelaw WA. The assessment of maximal respiratory mouth pressures in adults. Respir Care. 2009;54(10):1348–1359. | ||
Leelarungrayub J, Yankai A, Pinkaew D, Puntumetakul R, Laskin JJ, Bloomer RJ. A preliminary study on the effects of star fruit consumption on antioxidant and lipid status in elderly Thai individuals. Clin Interv Aging. 2016;11:1183–1192. | ||
Re R, Pellegrini N, Proteggente A, Pannala A, Yang M, Rice-Evans C. Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Radic Biol Med. 1999;26(9–10):1231–1237. | ||
Leelarungrayub J, Laskin JJ, Bloomer RJ, Pinkaew D. Consumption of star fruit juice on pro-inflammatory markers and walking distance in the community dwelling elderly. Arch Gerontol Geriatr. 2016;64:6–12. | ||
Chirico S. High-performance liquid chromatography-based thiobarbituric acid tests. Methods Enzymol. 1994;233:314–318. | ||
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. | ||
American College of Sport Medicine (ACSM). ACSM’s guidelines for exercise testing and prescription. Philadelphia, PA. Lippincott Williams & Wilkins. 2004:110–112. | ||
Reda AA, Kotz D, Kocks JW, Wesseling G, van Schayck CP. Reliability and validity of the clinical COPD questionnaire and chronic respiratory questionnaire. Respir Med. 2010;104(11):1675–1682. | ||
van der Molen T, Willemse BW, Schokker S, Ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes. 2003;1:13. | ||
Sullivan GM, Feinn R. Using effect size-or why the p value is not enough. J Grad Med Educ. 2012;4(3):279–282. | ||
Heydari A, Farzad M, Ahmadi Hosseini SH. Comparing Inspiratory Resistive Muscle Training with Incentive Spirometry on Rehabilitation of COPD Patients. Rehabil Nurs. 2015;40(4):243–248. | ||
Tomich GM, França DC, Diório AC, Britto RR, Sampaio RF, Parreira VF. Breathing pattern, thoracoabdominal motion and muscular activity during three breathing exercises. Braz J Med Biol Res. 2007;40(10):1409–1417. | ||
Rollier H, Bisschop A, Gayan-Ramirez G, Gosselink R, Decramer M. Low load inspiratory muscle training increases diaphragmatic fiber dimensions in rats. Am J Respir Crit Care Med. 1998;157(3 Pt 1):833–839. | ||
Martarelli D, Cocchioni M, Scuri S, Pompei P. Diaphragmatic breathing reduces exercise-induced oxidative stress. Evid Based Complement Alternat Med. 2011;2011(932430):1–10. | ||
Campos NG, Marizeiro DF, Florêncio ACL, et al. Effects of respiratory muscle training on endothelium and oxidative stress biomarkers in hemodialysis patients: A randomized clinical trial. Respir Med. 2018;134:103–109. | ||
Vassilakopoulos T, Zakynthinos S, Roussos C. Strenuous resistive breathing induces proinflammatory cytokines and stimulates the HPA axis in humans. Am J Physiol. 1999;277(4):R1013–R1019. | ||
Luo Y, Zheng SG. Hall of Fame among Pro-inflammatory Cytokines: Interleukin-6 Gene and Its Transcriptional Regulation Mechanisms. Front Immunol. 2016;7:604. | ||
Laoutaris ID, Dritsas A, Brown MD, et al. Immune response to inspiratory muscle training in patients with chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2007;14(5):679–686. | ||
Rasekaba T, Lee AL, Naughton MT, Williams TJ, Holland AE. The six-minute walk test: a useful metric for the cardiopulmonary patient. Intern Med J. 2009;39(8):495–501. | ||
Redelmeier DA, Bayoumi AM, Goldstein RS, Guyatt GH. Interpreting small differences in functional status: the Six Minute Walk test in chronic lung disease patients. Am J Respir Crit Care Med. 1997;155(4):1278–1282. | ||
Hill K, Jenkins SC, Philippe DL, et al. High-intensity inspiratory muscle training in COPD. Eur Respir J. 2006;27(6):1119–1128. | ||
Kerti M, Balogh Z, Kelemen K, Varga JT. The relationship between exercise capacity and different functional markers in pulmonary rehabilitation for COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:717–724. | ||
Jo YS, Park S, Kim DK, Yoo CG, Lee CH. The cutoff point of clinical chronic obstructive pulmonary disease questionnaire for more symptomatic patients. BMC Pulm Med. 2018;18(1):38. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.