Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
Pregnant Women’s Knowledge, Attitude, and Practice Towards the Prevention of Mother to Child Transmission of HIV/AIDS in Dil Chora Referral Hospital, Dire Dawa, Eastern Ethiopia: A Cross-Sectional Study
Authors Cherie S, Workie H , Kassie T, Bitew A , Samuel T
Received 7 July 2021
Accepted for publication 13 January 2022
Published 11 February 2022 Volume 2022:14 Pages 45—60
DOI https://doi.org/10.2147/HIV.S327904
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Solomon Cherie,1,2 Hailemariam Workie,3 Teshager Kassie,4 Aschalew Bitew,5 Tsion Samuel3
1Debre Markos University, College of Health and Medical Science, School of Medicine, Debre Markos, Ethiopia; 2Dire Dawa University, College of Health and Medical Science, School of Medicine, Dire Dawa, Ethiopia; 3Bahir Dar University, College of Medical, and Health Science, School of Health Sciences, Bahir Dar, Ethiopia; 4Haramaya University, College of Health and Medical Science, School of Nursing and Midwifery, Harar, Ethiopia; 5GAMBY Medical & Business College, Bahirdar, Ethiopia
Correspondence: Solomon Cherie, Debre Markos University, College of Health and Medical Science, School of Medicine, P.O. Box 269, Debre Markos, Ethiopia, Email [email protected]
Background: According to a WHO report, HIV/AIDS continues to be a major global public health issue, having claimed 36.3 million in 2021 and 37.7 million people living with HIV at the end of 2020, more than two-thirds of whom were in the WHO African Region including sub-Saharan Africa. Among sub-Saharan Africa, Ethiopia is one of the countries that face an HIV/AIDS epidemic with an estimated 90,000 HIV-positive pregnant women, 14,000 HIV-positive births, 800,000 AIDS orphans, and 28,000 AIDS deaths annually. Thus, this study assessed the knowledge, attitude, and practice of pregnant women towards the prevention of mother-to-child transmission of HIV.
Methods: A hospital-based cross-sectional study was conducted in Dil Chora Referral Hospital among 242 pregnant women. The simple random sampling method was used to collect the data and respondents were interviewed face to face by using a standard and structured questionnaire. The quality of the data was assured by questionnaire pretesting, translation, and retranslation. After the collection of the data, each questionnaire was thoroughly reviewed for consistency, and completeness by the data collectors, supervisor, and investigators. Then, the data were inserted into Epi Info v3.5 and analyzed using SPSS v24. Descriptive statistics were employed to examine the findings, and the result was presented using tables, charts, and graphs.
Results: Two-third (66.7%) of the pregnant women had good knowledge and the remaining one-third (33.3%) had poor knowledge towards mother to child transmission of HIV/AIDS and its prevention. A good attitude has been observed among a majority of the respondents (71%) towards the prevention of mother-to-child transmission of HIV/AIDS. Unlike the above, only half of the pregnant women (50%) had good practice towards the prevention of mothers to child transmission of HIV/AIDS.
Conclusion: This study found that half of pregnant women (50%) had poor practice and around one-third of them (29%) had negative attitudes towards the prevention of mother-to-child transmission of HIV/AIDS. Therefore, creating a positive attitude and good practice among pregnant women are the most important components for the prevention of mother-to-child transmission of HIV/AIDS.
Keywords: knowledge, attitude, practice, PMTCT, pregnant women, HIV/AIDS, Dire Dawa
Background
The Human Immunodeficiency virus remains one of the most significant public health challenges in low- and middle-income countries.1 According to a WHO report, HIV/AIDS continues to be a major global public health issue, having claimed 36.3 million in 2021 and 37.7 million people living with HIV at the end of 2020, more than two-thirds of whom were in the WHO African Region including sub-Saharan Africa. In the same year, 1.5 million people acquired new HIV infection and 680,000 people died from HIV-related causes.2
Sub-Saharan Africa (SSA) has been the most seriously HIV stricken region, accounting for 71% of all new infections in adults and children, and about 90% of new infections among children globally.3 Among sub-Saharan Africa, Ethiopia is one of the countries that face an HIV/AIDS epidemic with estimated 90,000 HIV-positive pregnant women, 14,000 HIV-positive births, 800,000 AIDS orphans, and 28,000 AIDS deaths annually.4
Globally, estimated 1.3 million females living with HIV become pregnant each year. Therefore, it needs immediate identification followed by an offer of linkage to lifelong treatment and care, including support to remain in care and virally suppressed, along with partner services. Globally, 85% of these women and girls, from these, 88% among the 21 focus countries,1 had access to ART to prevent MTCT.5
Regardless of many trials, still there is no cure for HIV infection. However, HIV infection has become a manageable chronic health condition, enabling people living with HIV to lead long and healthy lives through increasing access to effective HIV prevention, diagnosis, treatment, and care, including for opportunistic infections.6
UNAIDS recommends redoubling efforts to reach the new proposed global 95–95–95 targets to avoid the worst-case scenario of half-million excess HIV-related deaths in sub-Saharan Africa, increasing HIV infections due to HIV service disruptions during COVID-19 and the slowing public health response to HIV.6
There might be a 25–35% risk of a baby acquiring HIV from an infected mother if there is no appropriate intervention for mother-to-child transmission of HIV. The transmission of HIV from mother-to-child transmission will occur during pregnancy, labor, and delivery, and breastfeeding7,8 with an estimation time and rate of the transmission 10–15% during delivery, 5–20% during breastfeeding, and 5–10% during pregnancy.9–12 But, the risk of HIV transmission can be lowered to 2% or less if a woman takes antiretroviral drugs during pregnancy and childbirth and her baby receives HIV drugs for 4–6 weeks after birth.13,14
Therefore, Prevention of Mother-to-Child Transmission (PMTCT) of HIV/AIDS plays a central role in declining new infections and accessing the services needed for HIV-infected women.15 PMTCT service includes HIV counseling and testing, antiretroviral drug therapy, comprehensive antenatal care and safer delivery practices, counseling and support, and appropriate infant feeding.16,17 Unlike these, several challenges are faced to prevent mother-to-child transmission of HIV/AIDS. Poor knowledge, unfavorable attitude, fear of disclosing their HIV status due to fear of discrimination, and poor counseling are the major challenges in fighting mother-to-child transmission of HIV/AIDS.13,18–20
One of the essential principles to avert the negative outcomes of HIV/AIDS is the prevention of mother-to-child transmission (PMTCT) of HIV/AIDS.21 For this purpose, in addition to the World Health Organization's virtual elimination of pediatric HIV,22 Ethiopia has been launched option B+ implementation since 2013. The main principle of option B+ is that all HIV-infected pregnant women receive triple antiretroviral drugs without initial CD4 testing.23 Regardless of the wide availability of PMTCT services, the mother’s knowledge of PMTCT is not satisfactory.20,24 Poor knowledge and practice and negative attitude of pregnant women about MTCT and PMTCT are the main challenges in Ethiopia for the full implementation of PMTCT service.25
Mothers’ positive attitude, good knowledge, and practice on the prevention of mother-to-child transmission of HIV are essential strategies to implement available prevention options of PMTCT.26,27 Mothers, who have a favorable attitude and adequate knowledge on PMTCT of HIV/AIDS, are more likely to undergo HIV testing and uptake of PMTCT services than women who have an unfavorable attitude and inadequate knowledge on PMTCT of HIV/AIDS.28,29 Therefore, the main objective of this study was to assess the knowledge, attitude, and practice of pregnant women on PMTCT of HIV/AIDS attending ANC follow-up in Dil Chora Referral Hospital, Ethiopia.
Methods
Study Area
The study was conducted in the Dire Dawa city administration. Dire Dawa administration is found 505 km far from Addis Ababa and 311 from Djibouti. The administration share border in the east, south-west, and north with Somali Regional State; and in the south with Oromia Regional State.
According to the 2007 Ethiopian census projection for 2012/13, the current total population of the Dire Dawa administration is 396, 423 (58% residing in urban whereas 42% in rural). There were two governmental and four private hospitals, 16 health centers, 5 higher clinics, 12 medium clinics, and 31 Health posts (governmental). According to EDHS 2011, ANC coverage of Dire Dawa was 59%. The ANC client load per month in each health center on average was 195 and in hospital 510. According to the Ethiopian Federal Ministry of Health (FMOH), Dire Dawa is one of the highly affected urban areas by HIV/AIDS.
Study Design and Participants Characteristics
A hospital-based quantitative cross-sectional study was conducted in Dil Chora Referral Hospital among selected pregnant women who were attending for ANC follow-up. All pregnant women who attended for ANC follow up during the study period were included for an interview and those who were unable to communicate due to hearing or speaking problems and those who have cognitive problems to give consent were excluded.
Sample Size Determination and Technique
The sample size (n) required for the study was determined using single population proportion formula ( ); whereas n = the required sample size, Za/2 (1.96): significance level at α = 0.05 with 95% confidence interval, p: knowledge of pregnant women towards MTCT of HIV attending ANC clinics of public health facilities in Addis Ababa, (2014) (79%)19 d: margin of error (5%) and 10% non-response rate. The calculated sample size was 255. However, the target population (N) was less than 10,000 (4846), so a correction formula was used. Therefore, the final required sample size was 242. A random sampling technique was used to choose these 242 respondents. As a result, all-volunteer respondents who fulfill the inclusion criteria were the sample population of the study until the intended sample size was fulfilled.
); whereas n = the required sample size, Za/2 (1.96): significance level at α = 0.05 with 95% confidence interval, p: knowledge of pregnant women towards MTCT of HIV attending ANC clinics of public health facilities in Addis Ababa, (2014) (79%)19 d: margin of error (5%) and 10% non-response rate. The calculated sample size was 255. However, the target population (N) was less than 10,000 (4846), so a correction formula was used. Therefore, the final required sample size was 242. A random sampling technique was used to choose these 242 respondents. As a result, all-volunteer respondents who fulfill the inclusion criteria were the sample population of the study until the intended sample size was fulfilled.
Measurement and Data Collection Procedure
Data were obtained in a face-to-face interview using a structured and standard questionnaire that contained socio-demographic and economic factors, mother’s knowledge, attitude, and practice of MTCT of HIV/AIDS and its prevention. Four trained BSc nurses and one MSc nurse were selected for data collection and supervision, respectively.
Data Quality Control
Qualities of data were assured by translation, retranslation, and pretesting of the questionnaire. A structured and standard questionnaire was used to interview the clients face to face. Two days of training were given for data collectors and supervisors about the purpose of the study, methods of data collection, ethical issues, and sampling procedure. Completeness and internal consistency were checked for each questionnaire. Before actual data collection, the questionnaire was pretested on 5% of pregnant mothers attending ANC. Findings from pretesting were utilized to modify and adjust the instrument and interviewing techniques. The questionnaire was translated into the local language (Amharic) and translated back into English to check the consistency of the questions.
Data Processing and Analysis
After the collection of the data, each questionnaire was thoroughly reviewed for consistency, and completeness by the data collectors, supervisors, and investigators. Then, the data were inserted into Epi Info version 3.5 and analyzed using SPSS version 24. Some data anomalies and outliers were cleaned by running descriptive (frequency). Descriptive statistics were employed to examine the findings, and the result was presented using tables, charts, and graphs.
Operational Definition
Good knowledge: Those pregnant women who answered above the mean of the knowledge questions were considered as having “good knowledge”; Poor knowledge: Those pregnant women who answered below the mean of the knowledge questions were considered as having “poor knowledge”; Good Attitude: Those pregnant women who answered above the mean of the attitude questions were assigned as having “good attitude”; Poor Attitude: Those women pregnant who answered below the mean of the attitude questions were assigned as having “poor attitude”; Good Practice: Those pregnant women who answered above the mean of the practice questions were considered as having “good practice”; poor practice: Those women who answered below the mean of the practice questions were considered as having “poor practice”.
Results
A total of 242 pregnant women were involved in the data collection with a 100% response rate. Thus, 242 respondents’ data were included in the analysis.
Sociodemographic and Socio-Economic Characteristics of the Study Participants
Out of the total respondents, 195 (80.6%) came from urban and 47 (19.4) from rural areas. One hundred sixteen (47.9%) were in the age groups of 26–35 years and 113 (46.7) were 15–26 age group, the rest were more than 35 years. Oromo was the major ethnicity [118 (48.8.0)] followed by Amhara [84 (34.7%)]. Around 1/10th (10.7%) of the pregnant women did not read and write at the time of data collection but 31.8% of them attended college/university (Table 1). Regarding religion, 106 (43.8%) of them were orthodox followers and 89 (36.8%) were Muslims (Figure 1).
 |
Table 1 Socio-Demographic Characteristics of Pregnant Mothers Attending ANC of Dil Chora Referral Hospital, Dire Dawa, East Ethiopian, 2017 |
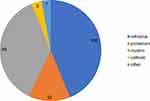 |
Figure 1 Pie chart showing the religious distribution of pregnant women who were attending ANC clinic in Dil Chora Referral Hospital in Dire Dawa, Ethiopia, 2017. |
The majority of the respondents were housewives (42.6%), followed by government employers [73 (30.2%)] and daily laborers [53 (21.9%)]. Nearly half of the respondents (48.8%), monthly income was more than 1000 Ethiopian Birr (ETB), but 16.9% of them had no income at all. More than two-thirds of the pregnant women (82.6%) were married but 31 (12.8%) were single. Only less than half of the women (45.5%) were attending antenatal care (ANC) during their third trimester of pregnancy (Table 1). Among the ANC attendants, 37 (15.3%), 55 (22H%), 66 (27.3%) and 84 (34.7%) had first, second, third, and fourth ANC Visit for their current pregnancy, respectively (Figure 2).
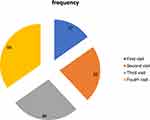 |
Figure 2 Number of ANC visits by pregnant women who were attending ANC clinic in Dil Chora hospital, Dire Dawa, Ethiopia, 2017 (n=242). |
The Knowledge of Pregnant Mothers Towards Mother to Child Transmission of HIV/AIDS and Its Prevention
All of the respondents heard about HIV/AIDS and more than half of them (52.9%) got information from mass media. The majority of the women [232 (95.9%)] knew at least one way of HIV transmission methods and [236 (97.5%)] knew at least one way of HIV prevention methods. Of the 236 respondents (who knew about prevention methods), 201 (85.1%) of them responded that condom use is one of the methods to prevent HIV transmission. One hundred sixty-six (70.3%) of the respondents knew condom has an advantage for the prevention of HIV from mother to her baby. Of these respondents, 97.5% knew that condoms were used to protect the mother from being infected by HIV, 95.8% to decrease the risk of having HIV infected baby, and 95.8% to prevent unwanted pregnancy and STI.
All of the respondents knew that HIV transmits from mother to child. Concerning the time of transmission of the virus from the infected mother to her child, 194 (80.2%) responded that it could be during pregnancy, 168 (69.4%) during labor and delivery, 172 (71.9%) through breastfeeding, and 48 (19.8%) during care provision (Table 2, Figures 3–Figure 5).
 |
Table 2 Mothers' response about the time of transmission of the virus from the infected mother to her child attending ANC clinic at Dilchora Referral Hospital, Dire Dawa, Ethiopia, 2017 |
 |
Figure 3 Knowledge of pregnant mother towards the prevention methods of HIV/AIDS in Dil Chora Referral Hospital, Dire Dawa, Ethiopia, 2017. |
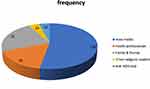 |
Figure 4 Pregnant mothers’ source of information about HIV/AIDS in Dil Chora Referral Hospital ANC clinic, 2017. |
 |
Figure 5 Knowledge about the time of MTCT of a pregnant mother who attending ANC clinic in Dil Chora Referral Hospital, Dire Dawa, 2017. |
From all respondents, the majority of them (98.8%) replied that testing of HIV has an advantage for PMTCT. Of these mothers, 96.2% said that to know the status, 92.1% to start ART drug early if the result is positive and 73.2% to protect others.
Concerning HIV/AIDS medication, 206 (85%) of women knew ART drugs given to HIV-positive pregnant mothers to reduce risk of HIV transmission. Two hundred seventeen (89.7%) of women knew that the risk of MTCT of HIV was prevented by providing ART during pregnancy, by cesarean section delivery 8 (36.4%) and by providing ART drugs to the newborn 117 (48.3%). But, only half of them (50.8%) knew ART prophylaxis could be started in the first trimester, and 45% of them do not remember when it started (Table 3 and Figure 6).
 |
Figure 6 Knowledge of pregnant mothers about the time of ART prophylaxis started to PMTCT in Dil Chora Referral Hospital, Dire Dawa, Ethiopia, 2017. |
The Attitude of Pregnant Mothers Towards Mother to Child Transmission of HIV/AIDS and Its Prevention
Around one-third of the respondents [83 (34.3%)] fear testing HIV/AIDS due to fear of social isolation after the result. However, all of the respondents agreed that every pregnant woman gets tested for HIV and if a woman is infected with HIV, then she should not get pregnant again. All mothers support ANC follow-up and PMTCT strategies.
Again, most respondents had a good attitude towards protective methods for mother-to-child transmission of HIV/AIDS. Two hundred six (85.1%) of respondents agreed that using protective gears (condoms) during pregnancy and breastfeeding can reduce mother-to-child transmission of HIV/AIDS, respectively. Others [238 (98.3%)] agreed that Obstetric care during labor and delivery reduces mother-to-child transmission of HIV/AIDS (Table 4).
 |
Table 3 Knowledge of Pregnant Mothers Towards Mother to Child Transmission of HIV/AIDS and Its Prevention Attending ANC Clinic at Dil Chora Referral Hospital, Dire Dawa, Ethiopia, 2017 |
 |
Table 4 Attitude of Pregnant Mothers Towards Mother to Child Transmission of HIV/AIDS and Its Prevention Attending ANC Clinic at Dil Chora Referral Hospital, Dire Dawa, Ethiopia, 2017 |
 |
Table 5 Practice of Pregnant Mothers Towards Mother to Child Transmission of HIV/AIDS and Its Prevention Attending ANC Clinic at Dil Chora Referral Hospital, Dire Dawa, Ethiopia, 2017 |
The Practice of Pregnant Mothers Towards Mother to Child Transmission of HIV/AIDS and Its Prevention
Two hundred thirty-eight (98.3%) of women have been tested for HIV/AIDS. From those, [206 (85.1%)] were tested at their current pregnancy, 56 (23.1%) during the previous pregnancy, 118 (48.8) during the marriage, and 53 (21.9%) tested at a time of medical illness. The majority of pregnant mothers (228 (95.8%)) get tested at a health institution. But, less than half of respondents (44.1%) tested every 3 months, and (39.1%) tested more than three times. Pretest and posttest counseling was given to 205 (86.1%) and 208 (84.4%) pregnant mothers, respectively (Table 5 and Figure 7).
 |
Figure 7 Time of testing of HIV/AIDS among pregnant mothers who attending ANC clinic in Dil Chora Referral Hospital, Dire Dawa, 2017. |
Knowledge, Attitude, and Practice of Pregnant Mothers Towards Mother to Child Transmission of HIV/AIDS and Its Prevention
As stated in the section of operational definition, knowledge of the pregnant women was assessed by asking them about mother to child transmission of HIV/AIDS, its prevention, and so on. Those mothers who answered above the mean of the knowledge questions were considered as having “good knowledge” and answered below the mean considered as having “poor knowledge”.
Also, the attitude of the pregnant women was assessed whether they agree or disagree on the importance of HIV testing during pregnancy, ANC follow-up, PMTCT of HIV, and so on. Mothers who answered above the mean questions were assigned as having a “positive attitude” and those who answered below the mean were assigned as having a “negative attitude”.
As with knowledge and attitude, the practice of pregnant women was assessed by asking them whether they were tested for HIV, the frequency of HIV testing, their effort on prevention of MTCT of HIV, and so on. Those pregnant women who answered above the mean questions were considered as having “good practices”, whereas those who did not were assigned as having “poor practice”.
Based on the above preliminary criteria, two-third (66.7%) of the pregnant women had good knowledge and the remaining one-third (33.3%) had poor knowledge towards the prevention of mother to child transmission of HIV/AIDS. Regarding attitude, a majority of the respondents (71%) had a good attitude, and the remaining (29%) of the respondents had negative attitudes towards the prevention of mother to child transmission of HIV/AIDS. But, only half of the pregnant mothers (50%) had good practice towards the prevention of mother-to-child transmission of HIV/AIDS.
Discussion
In this study, two-thirds (66.7%) of the pregnant women had good knowledge towards the prevention of mother-to-child transmission of HIV/AIDS. The finding of this study is consistent with research conducted in Cente, Katsina State, Nigeria (65%), South, Ethiopia (65.9%).30,31
Unlikely, however, the knowledge of pregnant mothers towards the prevention of mother-to-child transmission of HIV/AIDS in this study was lower than other similar cross-sectional studies conducted in Mekelle-Ethiopia (96.25%), and Hawassa Referral Hospital, South Ethiopia (82.3%).15,32 However, it is significantly greater than a study done in Meket District, Northeast Ethiopia (19%), Srinagar District, North India (50.8%), Mecha district, Northwest Ethiopia (22.4%), Juba Teaching Hospital, South Sudan (30.7%) and Lagos Nigeria (8.3%).33–37 This might be due to the difference in the study setting, accessibility of information, utilization of the service, and availability of health facilities.
This study has shown that most of the respondents (71%) had a good attitude towards the prevention of mother-to-child transmission of HIV/AIDS. It is more similar to a study conducted in Mekelle-Ethiopia, Katsina State-Nigeria, and South-Ethiopia.30–32 This finding was slightly lower than studies conducted in Ambo-Ethiopia (93.6%), Hawassa-Ethiopia (97.4%), Srinagar District-North India (96.4%), and Hawassa-Ethiopia (93.3%)15,37–39 but much higher than compared to a study done in Southwestern Nigeria (28.73%), Juba Teaching Hospital, South Sudan (51%).36 This might be explained due to the difference in the geographical area, study period, and sample size.
Regarding HIV/AIDS testing, 238 (98.3%) of the respondents have been tested for HIV/AIDS. The finding is in line with studies conducted in Northern Tanzania, Ambo-Ethiopia, Hosanna-southern Ethiopia, and Hawassa-Ethiopia (98%, 100%, 100%, and 96.0% respectively).15,38–40 Yet, it was much different from the study done in Abidjan-Côte d’Ivoire, Benue-Nigeria, Juba-South Sudan, Srinagar District-North India (91.4%), and Bobo-Dioulasso Burkina Faso (58.4%, 55.7%, 78.4%, 91.5%, and 81.8% respectively).36,37,41,42 This could be due to the difference between this and the later studies, in that as awareness and knowledge increase; the habit of HIV/AIDS testing also increases.
Two hundred forty-two of the participants knew that HIV transmits from mother to child. Concerning the time of transmission of the virus from the infected mother to her child, 194 (80.2%) responded that it could be during pregnancy, 168 (69.4%) during labor and delivery, and 172 (71.9%) through breastfeeding. However, a similar cross-sectional study done in Gondar town, NorthWest Ethiopia showed that only 35.9% of participants replied it occurs during pregnancy, 33.6% during labor, and 24.9% during breastfeeding.43 A possible explanation of this huge discrepancy might be due to the time gap between the studies and the expansion of media. Nowadays, there is a high expansion of media in the country and following this, pregnant mothers can get plenty of information about the mother-to-child transmission mechanism of HIV/AIDS.
In conclusion, the concerned bodies should work to fill the gaps of pregnant mothers’ knowledge, attitude, and practice towards the prevention of mother to child transmission of HIV/AIDS.
Conclusions
The study found that 66.7% of pregnant women had good knowledge but half of them (50%) had poor practice and around one-third of the pregnant women (29%) had negative attitudes towards the prevention of mother-to-child transmission of HIV/AIDS.
There was an encouraging level of knowledge but the attitude and practice of mothers were not satisfactory towards mother-to-child transmission of HIV/AIDS and its prevention. These imply that big and collaborative effort is needed to compact mother-to-child transmission of HIV/AIDS. Therefore, increasing knowledge and creating a positive attitude and practice among pregnant women are the most important components for the prevention of mother-to-child transmission of HIV/AIDS.
Strength and Limitation of the Study
There was no same study in the study area so that it can be used as a baseline for other studies. It also helps to conduct an interventional study in a particular area.
It was not possible to establish a temporal relationship between the exposure and outcome variable as this study design was a cross-sectional study. The result may not be representative of entire pregnant mothers in Ethiopia due to the small sample size. We recommend other researchers conduct a study to test the relationship between the variables that affect knowledge, attitude, and practice of pregnant women towards the prevention of mother-to-child transmission of HIV.
Abbreviations
AIDS, acquired immune deficiency syndrome; ANC, antenatal care; ART, antiretroviral therapy; ARV, anti-retro viral; EDHS, Ethiopian Demographic and Health Statistics; EPHA, Ethiopian Public Health Association; FMOH, Federal Ministry of Health; HIV, human immune deficiency virus; IEC, information, education, and communication: knowledge, attitude and practice; MCH, maternal and child health; MOH, Ministry of Health; MTCT, mother to child transmission; PMTCT, prevention of mother to child transmission; UNAIDS, Joint United Nations Program on HIV/AIDS; UNICEF, United Nation Children’s Fund; VCT, voluntary counseling and testing; WHO, World Health Organization.
Data Sharing Statement
Data will be available upon consortium approval.
Ethical Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki. First ethical clearance and approval to conduct this study were obtained from the research and ethical committee of the College of Health and Medical Science, Dire Dawa university. And then, permission was taken from Dil Chora Referral Hospital to collect data. Voluntary informed written consent was taken from each study subject before the interview after the purpose of the study was explained to them. If participants were under the age of 16 years old, consent was obtained from the parents/guardians Confidentiality of the information was assured and privacy of the respondent was maintained.
Acknowledgments
We would like to thank Dire Dawa University for giving me the chance to conduct this research. Our gratitude goes to Dil Chora Referral Hospital staff for giving us the permission and unreserved collaboration to conduct this research in their hospital. Our sincere gratitude and appreciation are forwarded to data collectors and participants without whom it would not be realized. We are also very glad to be in a position to acknowledge Mr. Hayal Wubetu Mure for English editing to correct the grammar and flow of our manuscript.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval for the version to be published, agreed to the submitted journal, and agree to be accountable for all aspects of the work.
Funding
This research did not receive grants from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
All authors declared that they have no competing interest.
References
1. World Health Organization. HIV/AIDS; 2021. Available from: https://www.who.int/news-room/facts-in-pictures/detail/hiv-aids.
2. World Health Organization. HIV/AIDS: key facts; 2021 [updated July 14, 2021]. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
3. World Health Organization, UNAIDS. AIDS Epidemic Update: December 2009. Regional Office Europe: WHO; 2009.
4. Government of Ethiopia MoH. Health sector development programme IV. Annual performance report. Addis Ababa; 2010.
5. World Health Organization. Mother-to-child transmission of HIV; 2021. Available from: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/prevention/mother-to-child-transmission-of-hiv.
6. World Health Organization. HIV/AIDS, Key facts; 2021 [updated November 30, 2021]. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
7. World Health Organization. Global Guidance on Criteria and Processes for Validation: Elimination of Mother-To-Child Transmission of HIV and Syphilis.
8. Myer L, Essajee S, Broyles LN, et al. Pregnant and breastfeeding women: a priority population for HIV viral load monitoring. PLoS Med. 2017;14(8):e1002375. doi:10.1371/journal.pmed.1002375
9. UNAIDs, UNICeF, World Health Organization. Global HIV/AIDS response: epidemic update and health sector progress towards universal access: progress report 2011. Geneva Switzerland; 2011.
10. Dunn DT, Newell ML, Ades AE, Peckham CS. Risk of human immunodeficiency virus type 1 transmission through breastfeeding. Lancet. 1992;340(8819):585–588. doi:10.1016/0140-6736(92)92115-V
11. De Cock KM, Fowler MG, Mercier E, et al. Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy and practice. JAMA. 2000;283(9):1175–1182. doi:10.1001/jama.283.9.1175
12. Lomborg B. RethinkHIV: Smarter Ways to Invest in Ending HIV in Sub-Saharan Africa. Cambridge University Press; 2012.
13. Center for Disease Control and prevention. HIV among pregnant women, infants, and children; 2017. Available from: https://www.cdc.gov/hiv/group/gender/pregnantwomen/index.html.
14. Kourtis AP, Lee FK, Abrams EJ, Jamieson DJ, Bulterys M. Mother-to-child transmission of HIV-1: timing and implications for prevention. Lancet Infect Dis. 2006;6(11):726–732. doi:10.1016/S1473-3099(06)70629-6
15. Abajobir AA, Zeleke A. Knowledge, attitude, practice and factors associated with prevention of mother-to-child transmission of HIV/AIDS among pregnant mothers attending antenatal clinic in Hawassa referral hospital, South Ethiopia. J AIDS Clin Res. 2013;4(6):2–7.
16. Central statistical agency, ICF. Demographic health survey (DHS). Maryland, USA: International Calverton; 2012.
17. World Health Organization. WHO guidelines approved by the guidelines review committee. Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants: Recommendations for a Public Health Approach: 2010 Version. Geneva: WHO; 2010.
18. Adedimeji A, Abboud N, Merdekios B, Shiferaw M. A qualitative study of barriers to effectiveness of interventions to prevent mother-to-child transmission of HIV in Arba Minch, Ethiopia. Int J Popul Res. 2012;2012:7. doi:10.1155/2012/532154
19. Deressa W, Seme A, Asefa A, Teshome G, Enqusellassie F. Utilization of PMTCT services and associated factors among pregnant women attending antenatal clinics in Addis Ababa, Ethiopia. BMC Pregnancy Childbirth. 2014;14:328. doi:10.1186/1471-2393-14-328
20. Abiodun MO, Ijaiya MA, Aboyeji PA. Awareness and knowledge of mother-to-child transmission of HIV among pregnant women. J Natl Med Assoc. 2007;99(7):758–763.
21. Hassan F, Renju J, Songo J, et al. Implementation and experiences of integrated prevention of mother-to-child transmission services in Tanzania, Malawi and South Africa: a mixed methods study. Glob Public Health. 2021;16(2):201–215. doi:10.1080/17441692.2020.1839927
22. World Health Organization. Global guidance on criteria and processes for validation: elimination of mother-to-child transmission of HIV and syphilis; 2017.
23. UNICEF. Survival and health. Ethiopia has launched option B+: Ethiopia; 2014:2104.
24. Teshale AB, Tessema ZT, Alem AZ, et al. Knowledge about mother to child transmission of HIV/AIDS, its prevention and associated factors among reproductive-age women in sub-Saharan Africa: evidence from 33 countries recent demographic and health surveys. PLoS One. 2021;16(6):e0253164. doi:10.1371/journal.pone.0253164
25. Sama CB, Feteh VF, Tindong M, Tanyi JT, Bihle NM, Angwafo FF
26. Alemu YM, Habtewold TD, Alemu SM. Mother’s knowledge on prevention of mother-to-child transmission of HIV, Ethiopia: a cross sectional study. PLoS One. 2018;13(9):e0203043. doi:10.1371/journal.pone.0203043
27. Harrison NE, Oruka KE, Agbaim UC, Adegbite OA, Okeji NAE. Evaluating the knowledge of HIV transmission and prevention of mother to child transmission (PMTCT) of HIV among HIV-positive mothers accessing care in military hospital in Lagos, Nigeria. World J AIDS. 2021;11(1):25. doi:10.4236/wja.2021.111003
28. Alemu YM, Ambaw F, Wilder-Smith A. Utilization of HIV testing services among pregnant mothers in low income primary care settings in northern Ethiopia: a cross sectional study. BMC Pregnancy Childbirth. 2017;17(1):199. doi:10.1186/s12884-017-1389-2
29. Barrett H. The African HIV/AIDS Epidemic. In: Handbook of African Development. Routledge; 2018:145.
30. Ezenkiri JN, Ezeani U, Okonkwo IM. Knowledge and attitudes towards preventive measures of mother-to-child transmission of HIV/AIDS among expectant mothers at the federal medical centre, Katsina State, Nigeria. J Med Sci Clin Res. 2020;8:128–135. doi:10.18535/jmscr/v8i9.25
31. Hailu D, Nigussie W, Gudeta TA, Abdu M, Molla Y, Assefaw G. Assessment of Knowledge and attitude towards prevention of mother-to child transmission of HIV/AIDS among antenatal care client in mizan-aman town public health facilities, benchi-maji zone, South Nation Nationalities and people region, Southwest Ethiopia, 2017. Child Health J. 2018;15(280):2.
32. Yitayih G, Fantahun A. Assessment of knowledge, attitude and practice of HIV prevention of mother to child among pregnant women attending Ayder referral hospital, Mekelle, Ethiopia. Int J Med Biomed Sci. 2014;2(2):29–33.
33. Birhane T, Assefa tessema G, Addis alene K, Dadi AF. Knowledge of pregnant women on mother-to-child transmission of HIV in Meket district, Northeast Ethiopia. J Pregnancy. 2015;2015:6. doi:10.1155/2015/960830
34. Balogun M, Odeyemi K. Knowledge and practice of prevention of mother-to-child transmission of HIV among traditional birth attendants in Lagos State, Nigeria. Pan Afr Med J. 2010;5:7.
35. Liyeh TM, Cherkose EA, Limenih MA, Yimer TS, Tebeje HD. Knowledge of prevention of mother to child transmission of HIV among women of reproductive age group and associated factors at Mecha district, Northwest Ethiopia. BMC Res Notes. 2020;13(1):166. doi:10.1186/s13104-020-05005-5
36. Thidor GTY, August F. Prevention of mother-to-child transmission of HIV: kno wledge, attitudes and pr actice among pregnant women at Juba teaching hospital. South Sudan Med J. 2019;12(1):12–16.
37. Mukhtar M, Quansar R, Bhat SN, Khan S. Knowledge, attitude and practice regarding mother-to-child transmission of HIV, its prevention, and associated factors among antenatal women attending a health care facility in district Srinagar, North India: a cross sectional study. Int J Community Med. 2020;7(7):2622. doi:10.18203/2394-6040.ijcmph20202987
38. Gurmu T, Bachu T, Jimma L, Minyahil A, Gobezie T, Hunduma D. Knowledge, attitude and practice towards PMTCT of HIV among women attending Ambo Hospital ANC Clinic, West Ethiopia. J AIDS Clin Res. 2015;6(1):407.
39. Tigabu W, Dessie G. Knowledge, attitude and practice towards prevention of mother to child transmission (PMTCT) of HIV/AIDS among pregnant mothers at Nigist Eleni Mohammed Memorial General Hospital (NEMMGH), Hosanna, Southern Ethiopia. J HIV/AIDS Infect Dis. 2018;4(101):1–11.
40. Falnes EF, Tylleskär T, de Paoli MM, Manongi R, Engebretsen IM. Mothers’ knowledge and utilization of prevention of mother to child transmission services in northern Tanzania. J Int AIDS Soc. 2010;13(1):36. doi:10.1186/1758-2652-13-36
41. Cartoux M, Msellati P, Meda N, et al. Attitude of pregnant women towards HIV testing in Abidjan, Cote d’ivoire and Bobo-Dioulasso, Burkina Faso. DITRAME Study Group (ANRS 049 Clinical Trial). Diminution de la Transmission Mere Enfant du VIH. Agence nationale de recherches sur le SIDA. AIDS. 1998;12(17):2337–2344. doi:10.1097/00002030-199817000-00016
42. Hembah-Hilekaan SK, Swende TZ, Bito TT. Knowledge, attitudes and barriers towards prevention of mother-to-child transmission of HIV among women attending antenatal clinics in Uyam district of Zaki-Biam in Benue State, Nigeria. Afr J Reprod Health. 2012;16(3):28–35.
43. Malaju MT, Alene GD. Determinant factors of pregnant mothers’ knowledge on mother to child transmission of HIV and its prevention in Gondar town, North West Ethiopia. BMC Pregnancy Childbirth. 2012;12(1):73. doi:10.1186/1471-2393-12-73
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
