Back to Journals » International Journal of Women's Health » Volume 12
Pregnancy During COVID-19 Outbreak: The Impact of Lockdown in a Middle-Income Country on Antenatal Healthcare and Wellbeing
Authors Muhaidat N , Fram K, Thekrallah F, Qatawneh A, Al-Btoush A
Received 3 September 2020
Accepted for publication 3 November 2020
Published 16 November 2020 Volume 2020:12 Pages 1065—1073
DOI https://doi.org/10.2147/IJWH.S280342
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Nadia Muhaidat,1 Kamil Fram,1 Fida Thekrallah,1 Ayman Qatawneh,1 Ala’a Al-Btoush2
1Department of Obstetrics and Gynecology, Faculty of Medicine, The University of Jordan, Amman 11942, Jordan; 2Department of Obstetrics and Gynecology, Queen Alia Military Hospital, Amman, Jordan
Correspondence: Nadia Muhaidat
Department of Obstetrics and Gynecology, Faculty of Medicine, The University of Jordan, Queen Rania Street, Amman, Jordan
Tel +962798385775
Email [email protected]
Introduction: Since the emergence of coronavirus disease 2019 (COVID-19) as a major worldwide health threat, countries have implemented preventative measures to limit the spread of the disease and reduce the strain on their health services. The Hashemite Kingdom of Jordan is one of the countries where relatively strict lockdown measures were enforced. This study aims to evaluate the impact of the lockdown circumstances in Jordan on antenatal care services and health circumstances of pregnant women during this period.
Participants and Methods: This study involved a cross-sectional survey of Jordanian women who are currently pregnant. An electronic survey was distributed among pregnant women in Jordan. A total of 944 completed responses were returned and analyzed. The sample size was statistically determined to be representative of the population.
Results: The results revealed a significant increase in the percentage of pregnant women not receiving antenatal care from 4% to 59.53% (p< 0.001) during the lockdown period, despite the fact that some of these women were suffering from significant underlying medical conditions or serious pregnancy complications that require close antenatal surveillance. The survey also demonstrated that the lockdown circumstances impacted the physical, social, and mental wellbeing of the participants.
Conclusion: Although the lockdown measures in Jordan have succeeded so far in relative containment of COVID-19, this research suggests that significant disruption to antenatal services has occurred and that the lockdown has affected the wellbeing of pregnant women in a number of aspects, which has the potential to cause antenatal health issues that are not directly related to the spread of COVID-19, but rather are a side effect of the way in which the outbreak is managed.
Keywords: pregnancy, coronavirus, COVID-19, cross-sectional studies, global health, Jordan, prenatal care
Plain Language Summary
Dr Muhaidat’s team conducted this study during the complete lockdown in the Hashemite Kingdom of Jordan, which extended from mid-March till the end of May 2020. The idea of this research was triggered by the observation that antenatal care services had become severely disrupted and disorganized during that time, and antenatal patients were facing variable degrees of difficulty in contacting their care providers or accessing care facilities. The team formulated an electronic questionnaire that was distributed to pregnant women in Jordan via a number of social media platforms, asking a number of questions to find out how and to which degree these women were able to get antenatal care, and how the lockdown circumstances impacted on their well-being in general. We found that there was a significant drop in antenatal care cover and that the lockdown affected the women’s nutritional and exercise choices, as well as their economic circumstances and wellbeing in ways that could potentially be detrimental to their overall health.
Introduction
A novel coronavirus outbreak was first identified in Wuhan, China in December 2019.1 It has since rapidly spread across the globe, to be declared a pandemic by the World Health Organization (WHO) on March 11, 2020.2
The first COVID-19 case was diagnosed in Jordan, a middle-income country in the Middle East,3 on March 2, 2020.4 The Jordanian government is considered to be among the “early movers” in the MENA region in terms of taking considerable action steps to limit the spread of COVID-19, as it launched a robust national response since mid-March 2020 to contain the threat of the pandemic,4,5 including the closure of all air and land borders, closing school, universities, private businesses and all non-essential public services, as well as imposing a mandatory curfew, and a high level of public compliance and support was achieved.4,6 This was justified by the concern that a mass outbreak of COVID-19 would strain the country’s limited health system resources, leading to further economic deterioration.7 Access to health care providers was restricted for non-emergency cases. These measures were partially eased from the end of May, 2020; however, partial curfews and restrictions persist to date.
Redirecting health system resources towards responding to the outbreak, whilst maintaining delivery of essential health services not directly related to COVID-19 was one of the challenges facing health care policymakers.8 According to the WHO operational guidance to maintain essential health care during an outbreak, care during pregnancy has been identified as a high priority category.8
Women are at risk of exposure as they are usually primary caregivers within their families and communities. Furthermore, they form a substantial proportion of the frontline health care workers dealing with infected cases.9 Thus far, COVID-19 infection during pregnancy has not been associated with worse outcomes during pregnancy, and there is little evidence of vertical transmission from mother to fetus antenatally.10–14 Nevertheless, as part of the indirect impact of the pandemic, antenatal and obstetric services may be affected in several ways.15 Acute maternity and reproductive health services may be severely limited, due to staff deployment and shortages, as well as a reduction in available infrastructure such as operating theatres and spaces on wards. Access to antenatal care clinics may also be affected by the decrease in the number of available health care workers and clinic appointments, as well as the travel restrictions that are imposed to contain the disease spread.15
The health system in Jordan consists of public, semi-public and private sectors all participating in the provision of antenatal care services.4 According to the most recent UNICEF data from 2017, the majority of pregnant women in Jordan were provided with antenatal care during their pregnancies, with the antenatal care coverage of pregnant women aged 15–49 years from any provider being 91.5%.16 This research aims to identify how the lockdown circumstances in Jordan have affected antenatal care provision to pregnant women across the country, as well as studying the impact of the changes in care provision and overall change in living circumstances on the woman’s overall health and wellbeing.
Materials and Methods
Study Design and Population
This research involved a cross-sectional survey of women residing in Jordan who are currently pregnant. A link to an electronic survey questionnaire was distributed through several social network platforms, specifically women and motherhood groups in Jordan, in April 2020. Data collection did not involve direct contact with participants, as lockdown and social distancing measures prevented this.
Study Tool
The survey questionnaire was designed using Surveymonkey® online survey development software. The questions were formulated in Arabic language, Jordan’s official language and covered three main areas, firstly, participants’ demographic information, followed by information about the participants’ antenatal care provision and obstetric history, and finally COVID-19-related lockdown impact on the participants’ physical, social, and psychological wellbeing. Details of the content of the questionnaire are found in Tables 1–6. The face and content validity of the questionnaire was examined by an expert panel consisting of a group of consultant obstetricians at Jordan University Hospital (JUH), to ensure that the questions cover the data that is required to assess various aspects of antenatal care provision and antenatal health concerns during the lockdown period.
 |
Table 1 Socio-Demographic Characteristics of the Participants (n = 944) |
 |
Table 2 Obstetric History of Participants (n=944) and Number and Percentages of Participants Not Receiving Antenatal Care During Lockdown |
 |
Table 3 Comparison of Numbers and Percentages of Participants Not Receiving Antenatal Care Prior to and During Lockdown |
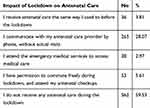 |
Table 5 Impact of Lockdown Circumstances on the Antenatal Care That the Participant is Currently Receiving |
 |
Table 6 Impact of Lockdown Circumstances on Participants’ Physical Wellbeing During Pregnancy |
Reliability of the questionnaire was determined by asking a group of 15 antenatal patients at JUH to answer the questionnaire twice 14 days apart. The participants’ responses were identical on both occasions with a reliability coefficient of 1.
Data Collection
Survey responses were collected online over a period of 8 days during which an electronic survey link was distributed on several social media women and motherhood groups in Jordan. Women were invited to participate in the survey if they were currently pregnant and residing in Jordan. The link introduction clarified that responses were anonymous, and participants would not be identified at any stage.
Sampling
The inclusion criteria for this study were for the women to: be currently pregnant, reside in any city or town within the Hashemite Kingdom of Jordan, and provide a complete response to the questionnaire.
The sample size was calculated using the Sample Size Calculator of the Epi Info 7 software. According to the Jordanian Department of Statistics, the most recent crude number of deliveries per year from 2018 was 226,820 deliveries.17 This number was taken as an estimate of the number of pregnancies per year. Due to the limited previous information regarding the effect of the lockdown circumstances on various aspects of women’s antenatal health, it was assumed that women would be affected adversely with a frequency of 50%. To achieve a 99% confidence interval, with a margin of error of 5%, and design effect of 1.0, the desired sample size was calculated to be 662. The survey link was closed once the number of completed responses exceeded this target.
Research Aims
This survey aims to identify a number of aspects related to the circumstances of pregnant women during the COVID-19 pandemic. The focus was to examine how these women were affected by the changes to the way of life within their communities as a result of lockdown and social distancing requirements.
Firstly, it aims to assess the woman’s access to antenatal care during lockdown and whether there is any disruption to her usual antenatal follow up schedule.
Furthermore, it also aims to examine the effect of lockdown on aspects of nutrition and physical activity during pregnancy, as well as access to medications and dietary supplements.
Finally, it aims to assess the impact of lockdown on socio-economic factors such as employment and income, and on the woman’s subjective mental state.
Statistical Analysis
We used SPSS version 21.0 (Chicago, USA) in our analysis. Count (frequency) was used to represent nominal variables. Chi-square test followed by Z-test for proportions was performed to analyze the difference between those who had access to ANC during the curfew and those who did not in regard to other variables. We adopted a p value of 0.05 as a significant threshold.
Results
A total of 1223 responses were submitted. Of these 944 were complete, the other 279 were omitted due to incomplete responses (completion rate 77.2%).
Demographics
Table 1 details some demographic and social characteristics of the participants in this survey. Almost half of the participants (41.31%) belonged to the 25–29-year age group, followed by 28.81% in the 30–34-year group. Only a minority of the patients were found in the age groups representing extremes of reproductive age (0.42% 15–19 years and 2.22% 40 years and above).
Over three-quarters of participants had higher education, ie Community College Diploma, Bachelor Degree, or Postgraduate Degree. The remainder had either primary or secondary education, no participants were illiterate.
About half of the participants (53.18%) were residents of the Jordanian capital, Amman. 81.78% of participants resided in the middle region of Jordan (Amman, Balqa, Zarqa and Madaba), 13.13% in the north region (Irbid, Ajloun, Jerash and Mafraq), and only 5.09% were from the south region (Aqaba, Karak, Tafeeleh and Ma’an).
Of the 944 pregnant women that took part in the survey, 38.56% reported that they used to be in some form of employment before lockdown, compared to only 16% during lockdown.
Antenatal Care Prior to Lockdown
Most participants had an antenatal care provider prior to the lockdown. Three quarters (74.68%) would book with obstetricians in the private health sector, compared to 12.92% attending the public sector with includes the Ministry of Health and University Hospitals, and 7.73% attending the Armed Forces Health Services. A small minority attended UNRWA (United Nations Relief and Works Agency for Palestine Refugees in the Near East) clinics. Only about 4% reported that they had had no antenatal care provider prior to lockdown.
Obstetric History
A number of factors regarding the participants’ obstetric histories were examined (Table 2). Almost half of the participants (45.34%) were in the third trimester of pregnancy, followed by about a third in the second trimester (35.06%), and the remaining participants in the first trimester.
Just under a third of participants (31.89%) were pregnant for the first time. The remaining participants had had one or more previous pregnancies. Of those, 41.21% had been delivered by caesarean section previously, and 3.58% had had previous instrumental deliveries.
Many participants reported having pre-existing medical conditions that would have to be taken into consideration when planning their antenatal care and would require increased surveillance during pregnancy. The most frequently reported condition was hypothyroidism (5.19%), followed by respiratory disease (4.13%), hypertension (3.5%), and diabetes (2.44%). Other less frequently reported conditions are listed in Table 2.
In addition to pre-existing conditions, participants also reported a number of pregnancy complications with variable frequencies. The most frequently reported of these was gestational hypertensive disease (10.17%), followed by placenta previa (5.08%), gestational diabetes (3.81%), and vaginal bleeding (3.81%). A full list of encountered pregnancy complications is detailed in Table 2.
Antenatal Care During Lockdown
This study found a significant difference in the number of participants receiving ANC (p< 0.001), as only 38 (4%) not receiving ANC before curfew compared to 562 (59.5%) after the curfew (Table 3). There was no significant difference in those who received ANC and those who did not with regard to age (p= 0.873), education (p= 0.477), residence (0.07), or trimester of pregnancy (p= 0.356), as demonstrated in Table 4.
Most participants reported that the way in which they received antenatal care had changed since the beginning of the COVID-19 lockdown (Table 5). Strikingly, over half (59.53%) were not receiving any antenatal care during lockdown. Over a quarter (28.07%) were only communicating with their care provider over phone without actual antenatal visits. 5.61% had permits that allowed them to move freely during the curfew and were able to attend their antenatal checkups, whereas 2.97% used emergency medical services such as attending emergency departments as an alternative to attending antenatal clinics. Only 3.81% reported that their antenatal care schedule had been unchanged during lockdown.
Physical, Social and Psychological Wellbeing During Lockdown
The majority of participants (59.85%) reported that the lockdown had not affected their diet. However, just over a fifth (21.61%) felt that their diet had worsened due to less healthy food choices. On the other hand, 18.54% stated that their diet had improved, as they were more conscious about healthy eating. Just under half of participants had difficulties with obtaining medications and dietary supplement they required during their pregnancies. 29.56% found it more difficult to access them but eventually managed, whereas 17.27% were not able to get their medications and supplements at all. Over half of participants (56.04%) stated that they did not perform physical exercise during pregnancy regardless of the lockdown. However, over a third (35.91%) were less physically active than before lockdown, compared to 6.04% who maintained the same level of physical activity as before, and 2.01% who increased their level of physical activity. These findings are summarized in Table 6.
Social circumstances during lockdown were evaluated as detailed in Table 7. As previously mentioned, the number of participants in employment had dropped by more than half after lockdown. Furthermore, 60.59% reported a drop in their families’ incomes during lockdown.
 |
Table 7 Impact of Lockdown Circumstances on Participants’ Economic Circumstances During Pregnancy |
Participants were questioned about the effect of lockdown on their subjective psychological wellbeing (Table 8). More than one option could be selected. 18.33% had not noticed a difference, while 4.56% felt that their mental state is better than before lockdown. 43.43% had an increased sense of boredom, 42.37% felt sadder or more depressed, and 15.36% felt angrier than before. Alarmingly seven participants had thoughts of self-harm, and nine had suicidal thoughts.
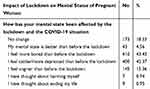 |
Table 8 Impact of Lockdown Circumstances on Participants Psychological Wellbeing |
Discussion
This study reveals that the lockdown circumstances that were experienced by pregnant women in Jordan over a period extending for two and a half months to combat the spread of COVID-19, led to a significant drop in the percentage of women receiving any form of antenatal care, regardless of their age, education level, area of residence, or stage of pregnancy.
These changes in antenatal care provision and coverage may lead to pregnancy-related health issues. According to Riley et al, 2020, a reduction of only 10% in the provision of pregnancy-related and newborn health services in low- and middle-income countries during the COVID-19 outbreak could lead to catastrophic increases in the number of maternal and neonatal deaths, as well as women experiencing major obstetric complications and newborns experiencing major complications without receiving appropriate care.18
Looking at the effect of previous infectious outbreaks such as Ebola in Sierra Leone, for example, antenatal care coverage dropped leading eventually to an increase in maternal and neonatal deaths as well as stillbirth rates due to pregnancy complications aggravated by the lack of proper health care during pregnancy rather than due to contracting the infection itself.19 During the COVID-19 outbreak, a study from Nepal revealed a reduction in the number of hospital births, as well as a rise in stillbirths and neonatal mortality during lockdown.20
This significant loss of antenatal care provision is even more alarming taking into consideration that it did not spare those groups of pregnant women that also suffer pre-existing medical conditions that could significantly compromise their or their babies’ health during pregnancy, and those that developed pregnancy complications that put them at risk of adverse pregnancy outcomes. For most of these women, the percentage receiving any antenatal care ranged from 0% to 50% at most, despite the fact that, ideally, they require increase surveillance and more frequent monitoring (Table 2). For example, half of the women suffering from cardiac disease and over half of those with respiratory diseases and diabetes were not receiving any antenatal surveillance. Out of those suffering from pre-existing hypertensive disease, 42% were lost to follow up. A pregnant woman with breast cancer was also not receiving antenatal care. For women affected by pregnancy complications, the most common of which were gestational hypertension, placenta previa, gestational diabetes, and vaginal bleeding, antenatal care coverage generally did not exceed 50% for most categories.
The reorganization of healthcare provision as well as travel restrictions during lockdown also led to a change in the way that antenatal care was offered to those that could access their providers, shifting from the usual clinic appointment to telephone consultations or emergency department visits, meaning that a substantial part of the patient’s antenatal care, such as direct contact with an obstetrician or midwife, adequate physical and ultrasound examination, and the regularity of the follow-up schedule was noticeably disrupted. This further raises concerns regarding potential adverse outcomes resulting from missed opportunities for prevention or early intervention.
Several general health and wellbeing aspects related to antenatal health were affected during lockdown. Over a fifth reported a decline in their diet quality due to lack of healthy food choices, whereas just under a fifth stated that they were more conscious about their diet choices and had actually improved the quality of their diet. Just under half of the participants in this study reported difficulties related to accessing their regular dietary supplements and medications, and over a third reported decreased physical activity levels compared to pre-lockdown. These findings raise additional concerns regarding the ability to maintain a healthy lifestyle during pregnancy in the presence of lockdown restrictions that limit access to healthy and variable food options, prescription and over the counter medications, and exercise opportunities, such as being able to go for a walk or to the gym.
The economic impact related to the management of the pandemic also affected pregnant women in Jordan, with a drop in employment by half, and a drop in family income for the majority of participants. This may lead to financial difficulties that further interfere with the woman’s ability to prioritize her health and maintain a healthy lifestyle throughout pregnancy.
Finally, the majority of participants subjectively reported some form of decline in their mental wellbeing ranging from boredom and sadness to anger and depression, and in a few alarming cases thoughts of self-harm or suicide, highlighting the potentially negative psychological impact of lockdown circumstances on the pregnant woman who is already experiencing a psychologically challenging phase of her life.
The above-mentioned physical, social and mental challenges of lockdown circumstances on antenatal health are further complicated by the lack of antenatal care experienced by a significant number of participants, where the chance to intervene in order to prevent or correct adverse physical or mental outcomes is lost.
Limitations
The authors acknowledge that this study is not without limitations. Some of Jordan’s geographical areas are under-represented in this survey, these are mostly areas with poorer socio-economic circumstances, and less advanced medical services. The survey was only available to those women that have access to social media; hence, again, the most deprived could potentially be under-represented. It is, therefore, possible that the actual impact of the lockdown on antenatal care is even more marked than what was found in this study.
Almost half of the participants were in the third trimester of their pregnancy, whereas a third were in the second trimester, and less than a fifth in the first trimester, which indicates that women in the earlier stages of their pregnancy could be under-represented in this study.
This study represents the finding of one middle-income country; further similar research of countries with similar circumstances is required for the results to be generalized.
Conclusion
The impact of the COVID-19 outbreak on global health has been immense. Whilst the light has been shed largely on the direct impact of the viral infection, hidden collateral damage resulting as a side effect of the management of the pandemic has also been significant. In Jordan, a country with strict lockdown and social distancing regulations, pregnant women have experienced a significant decline in effective antenatal care provision, potentially affecting the outcomes of their pregnancies adversely, especially if associated with pre-existing medical conditions or pregnancy-related complications. It has also proven difficult for large groups of pregnant women to maintain overall physical and mental wellbeing due to the multiple restrictions and economic shortfalls imposed by the lockdown. Although pregnant women may not be at a significantly increased risk of suffering adverse outcomes from COVID-19 infection, it seems that they may be a key category of side effect victims of this pandemic.
Data Sharing Statement
The raw data supporting the results of this study are represented in the tables included and can be made available by the corresponding author upon request.
Compliance with Ethical Standards
This research was granted ethical approval by the Institutional Review Board (IRB) of Jordan University Hospital in accordance with the Helsinki Declaration (reference 1012020/8629). Responses were anonymous, hence participant confidentiality was protected. Participation was voluntary and participants could withdraw from submitting their response at any point prior to final submission; therefore, a complete submitted response was considered consent to participation. No compensation was given in return for participation.
Acknowledgment
The authors would like to acknowledge all the participants in this survey for sharing their information and taking the time to respond to the questionnaire.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all the aspects of the work.
Funding
No funding was provided for this study.
Disclosure
The authors report no financial or non-financial conflicts of interest in this work.
References
1. Zu ZY, Jiang MD, Xu PP, et al. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020:200490.
2. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160.
3. World bank. World bank country and lending groups. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
4. Ayadi R Covid-19 in the Mediterranean and Africa; April, 2020.
5. Woertz E. COVID-19 in the Middle East and North Africa: reactions, vulnerabilities, prospects; 2020.
6. Parker-Magyar EK Transparency and repression in Jordan’s response to COVID-19. The COVID-19 Pandemic in the Middle East and North Africa; April, 2020:73.
7. Hartnett AS, al-Natour E, al-Ajlouni L. Drastic measures: coercive enforcement and economic effects of pandemic suppression in Jordan. The COVID-19 Pandemic in the Middle East and North Africa; April 2020:65.
8. World Health Organization. Maintaining essential health services: operational guidance for the COVID-19 context interim guidance. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-essential-health-services-2020.1https://www.who.int/publications-detail/covid-19-operationalguidance-for-maintaining-essential-health-services-during-anoutbreak.
9. Wenham C, Smith J, Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846–848. doi:10.1016/S0140-6736(20)30526-2
10. Schwartz DA. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020;144(7):799–805. doi:10.5858/arpa.2020-0901-SA
11. Li N, Han L, Peng M, et al. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study. Clin Infect Dis. 2020.
12. Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi:10.1016/S0140-6736(20)30360-3
13. Fan C, Lei D, Fang C, et al. Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin Infect Dis. 2020.
14. Alzamora MC, Paredes T, Caceres D, Webb CM, Valdez LM, La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. 2020;37(8):861. doi:10.1055/s-0040-1710050
15. Hussein J. COVID-19: what implications for sexual and reproductive health and rights globally?
16. UNICEF data warehouse, cross sector: Jordan. Available from: https://data.unicef.org/resources/data_explorer/unicef_f/?ag=UNICEF&df=GLOBAL_DATAFLOW&ver=1.0&dq=JOR.MNCH_ANC4.&startPeriod=1970&endPeriod=2020.
17. Jordanian Department of Statistics. Jordan statistical yearbook 2018. Available from http://dosweb.dos.gov.jo/databank/yearbook/YearBook_2018.pdf.
18. Riley T, Sully E, Ahmed Z, Biddlecom A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries. Int Perspect Sex Reprod Health. 2020;46:73–76. doi:10.1363/46e9020
19. Sochas L, Channon AA, Nam S. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plan. 2017;32(suppl_3):iii32–iii39. doi:10.1093/heapol/czx108
20. Ashish KC, Gurung R, Kinney MV, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. 2020;8(10):e1273–e1281.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

