Back to Journals » Patient Preference and Adherence » Volume 17
Preferred Conversation Topics with Respect to Treatment Decisions Among Individuals with Type 2 Diabetes
Authors Tichler A , Hertroijs DFL, Ruwaard D, Brouwers MCGJ, Hiligsmann M, de Jong JD, Elissen AMJ
Received 21 November 2022
Accepted for publication 14 January 2023
Published 17 March 2023 Volume 2023:17 Pages 719—729
DOI https://doi.org/10.2147/PPA.S397647
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Anna Tichler,1,2 Dorijn FL Hertroijs,1,2 Dirk Ruwaard,1,2 Martijn CGJ Brouwers,2,3 Mickaël Hiligsmann,1,2 Judith D de Jong,1,2,4 Arianne MJ Elissen1,2
1Department of Health Services Research, Faculty of Health, Medicine and Life Sciences (FHML), Maastricht University, Maastricht, the Netherlands; 2Care and Public Health Research Institute (CAPHRI), Maastricht University, Maastricht, the Netherlands; 3Department of Internal Medicine, Division of Endocrinology and Metabolic Disease, Maastricht University Medical Center+, Maastricht, the Netherlands; 4The Netherlands Institute for Health Services Research (NIVEL), Utrecht, the Netherlands
Correspondence: Anna Tichler, Department of Health Services Research, Faculty of Health, Medicine and Life Sciences (FHML), Maastricht University, P.O. Box 616, Maastricht, 6200 MD, the Netherlands, Tel +31433882193, Email [email protected]
Purpose: Greater knowledge of individuals’ needs and preferences can enhance shared decision-making, which is associated with improved quality of decisions and increased satisfaction. This study aimed to identify and prioritize the attributes (ie conversation topics) that individuals with type 2 diabetes find it most important to discuss with their healthcare provider regarding treatment decisions.
Patients and Methods: First, small group interviews were organized with adults with type 2 diabetes (N=8) treated in primary care to identify the attributes that they find important to discuss regarding treatment decisions. A five-step nominal group technique was applied during the interviews. An object best-worst scaling (BWS) survey was subsequently distributed to individuals with self-reported diabetes participating in the Dutch Health Care Consumer Panel of the Netherlands Institute for Health Services Research (N=600) to determine the relative importance score (RIS) of the identified attributes. A higher RIS indicates a higher level of perceived importance. Subgroup and latent class analyses were performed to explore whether individuals’ demographic and disease characteristics influenced their attribute preferences.
Results: A total of 21 attributes were identified during three small group interviews with individuals with type 2 diabetes. Respondents in the BWS survey (N=285) viewed “quality of life” (RIS=11.97), “clinical outcomes” (RIS=10.40), “long-term diabetes complications” (RIS=9.83) and “short-term adverse medication” (RIS=7.72) as the most important in the decision-making process for the treatment of type 2 diabetes. Some differences in attribute preferences were identified according to demographic and disease characteristics.
Conclusion: In general, individuals with type 2 diabetes not only want to discuss the biological effects of treatments, but also the impact of treatment on their quality of life. Healthcare providers should be aware that attributes are viewed differently by different individuals. This emphasizes the need for tailor-made healthcare decisions, which means eliciting and responding to individual preferences in the decision-making process.
Keywords: shared decision-making, person-centered care, patient preferences, diabetes type 2
Introduction
The European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) both recommend a person-centered approach for treatment decisions relating to glucose-lowering drugs.1 A person-centered approach highlights the importance of careful consideration of an individual’s values, needs, and preferences when it comes to treatment decisions.2 This requires a collaborative relationship between the patient and healthcare provider.3 Shared decision-making (SDM) is the hallmark of person-centered care.4 SDM is an approach whereby “clinicians and patients share the best available evidence” to reach a consensus on a treatment course, informed by a careful consideration of individuals’ needs and preferences.5 SDM can result in increased satisfaction and improved treatment adherence.6 The use of SDM in treatment decisions for individuals with type 2 diabetes is also associated with higher quality decision-making, ie confidence regarding the decision-making process.7
Although there is good evidence to support the effectiveness of SDM, its application to support person-centered care in general practice remains limited.8 Healthcare providers are not always able to apply SDM successfully due to a lack of time, tools or training.9 Despite the recommendations of the EASD and ADA for a person-centered approach, healthcare providers tend to adhere strictly to the national guidelines when it comes to prescribing the available treatment options. This leaves limited scope for patients with diabetes to incorporate their personal circumstances, social context and preferences into the decision-making process.10 In addition, successfully applying SDM has proven difficult from the perspective of patients with diabetes. They do not always understand the information they are given by their healthcare provider, or are not used to making decisions about their own treatment.11 Moreover, people sometimes do not recognize the importance of their own preferences and often feel insecure about using medical information to participate in decision-making.12
Several studies in different countries have been performed to determine individuals’ preferences regarding glucose-lowering medication for type 2 diabetes.13,14 However, to our knowledge, no studies have focused on individuals’ preferences regarding discussion topics with respect to treatment decisions for type 2 diabetes. This study, therefore, aims to identify and rank the attributes (ie, conversation topics) that individuals with type 2 diabetes find it most important to discuss with their healthcare provider with respect to treatment decisions. Better knowledge of individuals’ preferences when it comes to these can support SDM and guide person-centered care. This research is part of a larger study, which aims to develop a patient decision aid (PDA) to enhance SDM and support a person-centered approach in the treatment of type 2 diabetes (September 2020, “Development and usability testing of a patient decision aid to enhance shared decision-making regarding treatment decision in type 2 diabetes”, Netherlands Trial Register ID: NL8948).
Materials and Methods
An exploratory sequential design that combined small group interviews with a best-worst scaling survey was used to identify and rank the attributes that are viewed as important with respect to treatment decisions for type 2 diabetes. The study was approved by the Dutch Clinical Research Foundation (NWMO20.03.015) and by the Medical Ethics Review Committee of the academic hospital of Maastricht (azM) and Maastricht University (020-2176). The study was conducted in agreement with the ethical standards described in the Declaration of Helsinki. Informed consent was obtained from all participants.
Setting
The study was conducted in the Netherlands, where most individuals with type 2 diabetes are treated in primary care.15 A general practitioner and practice/diabetes nurse provide treatment following the national guidelines for type 2 diabetes published by the Dutch College of General Practitioners (NHG).16 The guideline used to describe a treatment algorithm of first metformin followed by the sequential addition of sulfonylurea and insulin. In 2018 and 2021, the guidelines were updated significantly to allow new glucose-lowering drugs (eg, sodium-glucose co-transporter 2 inhibitors and glucagon-like peptide-1 receptor agonists) to be used to treat high-risk individuals. Individuals are considered high risk if they have previously suffered from cardiovascular diseases or heart failure, for example.16 The NHG guidelines make no recommendations regarding SDM or person-centered care.
Small Group Interviews
Participants
Small group interviews were held with individuals with type 2 diabetes in order to identify the attributes that they find it important to discuss with their healthcare provider with respect to treatment decisions. A convenience sampling method was used to recruit individuals for the small group interviews. These individuals were recruited through advertisements in local newspapers and by general practitioners who are part of the professional network of the research group. Individuals were eligible to participate in the small group interviews if they: 1) had been diagnosed with type 2 diabetes more than one year ago; 2) were being treated in primary care; 3) were 18 years or older; and 4) were not prescribed medication or being treated with metformin with or without sulfonylurea.
Design
Due to the restrictions associated with the COVID-19 pandemic, the small group interviews were held online (between October 2020 and January 2021) using Microsoft Teams and lasted approximately two hours. Two researchers from Maastricht University took turns to facilitate the discussion and take notes during the small group interviews. Each participant completed a questionnaire on demographic and background characteristics (eg, age, sex, education) and their current state of health (eg, duration of their diabetes, glucose-lowering treatment, most recent HbA1c level) at the start of the small group interview. A five-step nominal group technique (NGT) was applied during the small group interviews to ensure that each participant’s perspective was included.17 An overview of the five-step NGT can be found in Supplementary Figure S1. First, participants were asked to answer the following question individually: “Which topics do you feel are important to discuss with your healthcare provider when you need to make decisions about treatment options?” In the second step, each participant had the opportunity to share the topics they came up with. Subsequently, in the third step, researchers suggested topics that had not previously been mentioned. These were derived from: 1) the International Consortium for Health Outcomes Measurement (ICHOM) Standard Set of Outcomes for individuals with type 2 diabetes;18 2) a systematic literature review of the preferences of individuals with type 2 diabetes for pharmaceutical and non-pharmaceutical treatment attributes (Rehbock C, 2016); and 3) where applicable, previous small group interviews. In the fourth step, a group discussion was held about the significance of each attribute identified. The participants had often provided an initial description of the attribute when they shared their attributes in the first step. Other participants had the opportunity to respond to that description or add to it. A final description of the attributes was formulated by the researchers using the input from the participants and the literature. In the final step of the NGT, the participants were asked to rank the ten most important attributes individually. Saturation was reached when no new attributes were identified in a subsequent small group interview.
Analysis
Descriptive statistics were reported to present the characteristics of individuals with type 2 diabetes who participated in the small group interviews. Descriptive statistics were performed in RStudio version 1.4.1106.19 A list of attributes with their description was created. The top ten attributes ranked by each participant of the small group interviews were analyzed by awarding points (ie from ten points to the most important attribute to one point to the least important attribute). For each attribute, the mean importance score (MIS) was calculated by dividing the total number of points awarded per attribute by the total number of participants in all the small-group interviews. The attributes were ranked provisionally based on the MIS for each attribute.
Best-Worst Scaling Survey
Participants
The BWS survey was distributed among a large group of individuals with self-reported diabetes, in collaboration with the Netherlands Institute for Health Services Research (NIVEL). NIVEL distributed the survey by email to individuals with self-reported diabetes participating in the Dutch Health Care Consumer Panel (N=600).20 Members of the Dutch Health Care Consumer Panel are sampled at random to ensure a representative sample of the Dutch population. Two reminders were sent. The questionnaires were completed between 30 March 2021 and 21 April 2021.
Design
The survey consisted of a description of the attributes (as derived from the small group interviews) and sixteen choice tasks. Each choice task consisted of a different subset of four attributes. For each choice task, participants in the Dutch Health Care Consumer Panel were asked to identify the attribute that they found most important and least important with respect to treatment decisions. An example of a choice task is shown in Table 1. The participants were only able to choose the attribute that they found the most important and the attribute they found the least important. The choice tasks were generated using Sawtooth Software Web version 8.2.0.21 which creates a fractional and efficient design for the BWS object case using a programming-based algorithm.22 In addition to the choice tasks, respondents had the opportunity to add attributes that were not included in the survey. The user-friendliness and comprehensibility of the BWS survey were pilot-tested with three individuals with type 2 diabetes and four researchers, whose feedback resulted in minor textual revisions.
 |
Table 1 Example of a Best-Worst Scaling Choice Task |
The respondents were also sent questions concerning their diabetes (eg, duration, glucose-lowering treatments, most recent HbA1c level) and the Dutch version of the Set of Brief Screening Questions (SBSQ-D). The SBSQ-D was included in the survey to measure functional health literacy.23 The SBSQ-D questions can be found in Supporting Information Doc. S1.
Data Analysis
Only the BWS surveys completed by individuals with self-reported type 2 diabetes were included when analyzing the data. Descriptive statistics were reported to present demographic and background characteristics of individuals with type 2 diabetes who completed the BWS survey. Hierarchical Bayes analyses were performed to determine the mean relative importance scores (RIS) for each attribute. Hierarchical Bayes analysis estimates the individual utility scores based on the mean for the population in an iterative process.24 These analyses were performed with Sawtooth SSI Web version 8.2.0.21 The mean overall RIS was calculated for each attribute with its 95% confidence interval. A higher RIS indicates that the attribute has a higher level of perceived importance. The sum of the RIS of all attributes is 100. Attributes were ranked from most to least important based on their mean RIS.
Subgroup analyses were performed to explore whether individuals’ demographic and disease characteristics influence their attribute preferences. The analyses were based on sex, age, body mass index (BMI), education, medication, duration of diabetes and HbA1c value. The RIS for each subgroup was calculated for each attribute with its 95% confidence interval. No overlap in the 95% CI indicates a difference in attribute preferences between the groups.25 Subgroup analyses were performed in RStudio version 1.4.1106.19
To identify hidden heterogeneity between participants, a latent class analysis was conducted using the survey data.26 We ran different models using all the attributes identified, starting with a one-class model and increasing the number of classes stepwise. The number of classes was determined by comparing various model fit and diagnostic indicators for each model. The RIS for each class was calculated for each attribute with its 95% confidence interval. Latent class analysis was performed in Mplus software (version 8.6).27 For further details of the conducted analysis, please see Supporting Information Doc. S2.
Results
Small Group Interviews
Table 2 shows the characteristics of the participants in the small-group interviews. We conducted three small group interviews and one in-depth interview (hereinafter referred to as the small group interviews) with a total of eight individuals with type 2 diabetes. Most of the participants were men (62.5%), and the participant’s mean age was 65 (±5) years. Saturation was reached after three small group interviews, ie no new attributes were identified. The participants identified a list of 21 attributes, which they found to be important to discuss with respect to treatment decisions. “Quality of life” received the highest mean importance score (MIS=5.75), followed by “long-term diabetes complications” (MIS=5.50), “short-term adverse medication events” (MIS=5.25), “clinical outcomes” (MIS=4.38), “lifestyle” (MIS=3.88) and “method of administration of medication” (eg oral, injection or insulin pump) (MIS=3.75). The attributes of “social support”, “out-of-pocket costs” and “manufacturer of the medication” were seen as not important (MIS=0.00). Supplementary Tables S1 and S2 provide an overview of the identified attributes with their descriptions and mean importance scores.
 |
Table 2 Characteristics of the Individuals with Type 2 Diabetes Who Participated in the Small Group Interviews (N=8) and Who Completed the Object Case Best-Worst Scaling Survey (N=285) |
Best-Worst Scaling Survey
Table 2 shows the characteristics of the participants in the BWS survey. The survey was returned by 350 individuals (response rate = 58%) of which 285 surveys were included in the analysis. A total of 65 surveys were excluded because 54 respondents did not have diabetes or had diabetes type 1. Eleven respondents did not complete the survey. The majority of survey respondents who completed the survey were men (N=285; 64%), and the mean age of the respondents was 72 (±8) years. With regard to functional health literacy, the majority of the respondents indicated they never have help when reading material provided by their general practitioner (75%) and never had problems learning about their medical condition (54%).
The BWS survey included all the attributes identified in the small group interviews, along with their description. The mean relative importance score (RIS) for each attribute was determined using Hierarchical Bayes analyses. Table 3 shows the overall mean RIS for each attribute with its 95% confidence intervals. Attributes are ranked from most to least important with respect to treatment decisions for type 2 diabetes. “Quality of life” is ranked as the most important attribute. “Clinical outcomes” (eg changes in HbA1c value) is ranked second, followed by “long-term diabetes complications”, “short-term adverse medication events” and “lifestyle”. The attributes “manufacturer of medication” and “experiences of other individuals” were ranked as the least important. Four respondents identified “monitoring frequency” (ie of the fundus and feet) as an additional relevant attribute.
 |
Table 3 Relative Importance Score (RIS) for Attributes with Respect to Treatment Decisions in Type 2 Diabetes, Derived from the Object Case Best-Worst Scaling Survey (N=285) |
Subgroup Analysis
Subgroup analyses revealed some heterogeneity between the attribute preferences of individuals with different demographic and disease characteristics (Tables S3–S9). For example, “medication withdrawal” was viewed as less important in the decision-making process by individuals aged over 75 years (RIS 5.16; 95% CI 4.48–5.85) compared to those aged 60–75 years (RIS 6.47; 95% CI 5.88–7.06) and those aged under 60 years (RIS 8.39; 95% CI 6.58–10.20). “Frequency of medication intake” was viewed as more important by individuals with a lower education (RIS 3.29; 95% CI 2.70–3.88) compared to those with a higher level of education (RIS 1.86; 95% CI 1.49–2.22). Individuals with HbA1c values under 53 mmol/mol (<7.0%) view “alternatives to medication” as more important (RIS 5.03; 95% CI 4.09–5.97) than individuals with HbA1c values over 64 mmol/mol (>8.0%) (RIS 3.08; 95% CI 2.14–4.01).
Latent Class Analysis
A two-class model was chosen based on model fit and diagnostic indicators (Table S10). The ranking of attributes for each class revealed preference differences, indicating heterogeneity within the survey data (Table 4). For example, “lifestyle” was ranked second in class 1 but eighth in class 2. “Short-term adverse medication events” was ranked ninth in class 1 but fourth in class 2. Table S11 shows the demographic and background differences between the two classes. Overall, class 1 consists of individuals who are slightly older on average and have a lower level of education. Class 1 also includes a higher percentage of individuals who do not use medication and a lower percentage of individuals with HbA1c values under 53 mmol/mol (<7.0%).
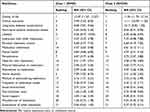 |
Table 4 Latent Class Analysis: Attribute Ranking for the Two Identified Classes |
Discussion
The aim of this study has been to improve our understanding of which attributes individuals with type 2 diabetes view as the most important to discuss with their healthcare provider with respect to treatment decisions. During the small-group interviews, a total of 21 attributes were identified and subsequently ranked in a best-worst scaling survey. As a group, individuals with type 2 diabetes appear to view “quality of life”, “clinical outcomes”, “long-term diabetes complications” and “short-term adverse medication events” as the most important subjects for discussion in the decision-making process around treatment options. The attributes “manufacturer of medication” and “experiences of other individuals” were ranked as the least important. Some heterogeneity in attribute preferences between individuals with different demographic and disease characteristics was identified.
Of all the attributes included in our BWS survey, “quality of life”, “clinical outcomes”, “long-term diabetes complications”, “short-term adverse medication events” and “lifestyle” are valued as the most important topics for discussion with respect to treatment decisions. This is fairly consistent with findings from other preference studies regarding the treatment of type 2 diabetes. A systematic literature review by Toroski et al14 aimed to evaluate the preferences of patients and healthcare providers with respect to type 2 diabetes treatment options. The review showed that individuals with type 2 diabetes view changes in blood glucose and HbA1c levels, adverse events (eg hypoglycemia events, gastrointestinal complications, and cardiovascular effects) and weight change as the most important attributes for type 2 diabetes treatment. The preference studies included in the systematic literature review focused solely on attributes related to type 2 diabetes medication and, unlike our study, they did not include “quality of life” and “lifestyle” as attributes. The attributes in those studies were derived from a literature review or an expert group of healthcare providers. Our approach of including input from patients (eg from the small-group interviews) meant that it was possible to identify attributes related to individuals’ personal and social context. Our study has shown that patients with type 2 diabetes view these attributes as important in relation to treatment decisions. Indeed, “quality of life” was ranked as the most important of all the attributes. Diabetes and its treatment have an impact on the life of the individual that goes beyond the effects on glycemic control and the progression of the condition.28 For example, individuals with type 2 diabetes may find that diabetes impacts negatively on their self-confidence, and that they experience frequent stress as a result of having to manage their condition, which can affect their quality of life. This could explain why individuals with type 2 diabetes view “quality of life” as the most important attribute to discuss with their healthcare provider with respect to treatment decisions. A study by Ruissen et al found that healthcare providers also recognize the importance of discussing person-related factors in the diabetes treatment decision-making process.29 Patient’s preferences and quality of life were reported as key factors relevant for diabetes treatment decisions according to secondary care healthcare providers. Therefore, not only the biological effects of a treatment needs to be discussed (which is standard) during the decision-making process, but also the impact of a treatment on a patient’s quality of life.
Subgroup analysis revealed some heterogeneity in attribute preferences between individuals with different demographic and disease characteristics, including age, level of education, HbA1c value and medication use. This is consistent with another study that also found differences in attribute preferences between individuals with different disease characteristics (eg medication use).30 Latent class analysis identified two classes in the survey data for which the attribute rankings were different. Minor differences were observed in the characteristics of individuals between the two classes. This indicates that individuals with similar characteristics may have different preferences. Both the subgroup analysis and latent class analysis confirmed that individuals with type 2 diabetes may find it important to discuss different attributes with respect to treatment decisions. It is therefore important for healthcare providers to incorporate individual preferences into the decision-making process, and this also highlights the need for shared decision-making. The importance of personalizing type 2 diabetes care is also recognized by the EASD and ADA. They recommend tailoring diabetes care by taking individuals’ social, medical and personal factors into account.2,31 Patient decision aids (PDAs) are useful, evidence-based tools that are designed to help individuals and healthcare providers navigate the decision-making process around treatment options.32 They can facilitate communication between individuals and healthcare providers and promote (efficient) SDM. The findings of this study will be used to develop a PDA for individuals with type 2 diabetes and their healthcare providers specifically for treatment-related decisions.
This study has some strengths and limitations. One strength of our study is the exploratory sequential design that we used to identify and prioritize attributes for the treatment of type 2 diabetes. Previous preference studies for type 2 diabetes focused on treatment attributes that had been identified through a literature review or by an expert group of healthcare providers. Our approach involved small-group interviews with individuals with type 2 diabetes, which enabled us to identify the treatment attributes and attributes relating to their personal context that they viewed as important. However, the first limitation of our study is the limited sample size of those small-group interviews, which could have led to an incomplete list of attributes. Nevertheless, the small groups allowed for full participation and interaction between participants and, saturation was reached during the small group interviews. The respondents of the BWS survey were also able to add any attributes that were not included in the BWS survey and this only led to the identification of one additional attribute. Another limitation of our study is the creation and use of one version of the BWS survey. Multiple versions of the questionnaire are often used, which increases the variation within sets, ultimately leading to the reduction of potential context biases.22 However, our BWS survey had an almost perfect balance for the one-way frequencies. An exact balance is preferable but not a requirement, and Hierarchical Bayes analysis and latent class analysis do not require perfect balance to achieve unbiased estimates of parameters.22 The analysis of the SBSQ-D questions revealed that respondents in the BWS survey generally had high health literacy. It is possible that our sample of individuals with type 2 diabetes had a better understanding of that condition and the various treatment options available. In the Netherlands, 24.5% of the total population has poor or limited health literacy.33 The results should therefore only be generalized with caution. Additionally, there were more male respondents in the BWS survey (64%) than females. This is somewhat higher than the 53% of the Dutch population with type 2 diabetes.34
Conclusion
In conclusion, our study provides an insight into which information individuals with type 2 diabetes, in general, see as the most important to discuss with their healthcare provider when it comes to making informed treatment decisions. Healthcare professionals need to provide information about “clinical outcomes”, “long-term diabetes complications” and “short-term medication adverse events”, as part of the shared decision-making process, since these attributes were viewed as the most important. The findings of this study also emphasize that in the decision-making process, healthcare providers should focus not only on the biological effects of treatment and the progression of diabetes (which is standard), but also on the impact of treatment on the patient’s quality of life. It should be noted that a limitation of the study is the limited sample size of the small-group interviews. It is therefore possible that we missed attributes that individuals with type 2 diabetes want to discuss with their healthcare provider with respect to treatment decisions. Furthermore, our study showed variation among individuals with type 2 diabetes with respect to which topics they view as important to discuss in the decision-making process. This highlights the importance of tailored healthcare decision-making, which implies that individuals’ preferences should be elicited as part of the decision-making process.
Data Sharing Statement
All authors of this had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Data Generation
The datasets of the current study are generated and/or analyzed and owned by the authors of this paper.
Acknowledgments
We acknowledge and thank MSD BV The Netherlands as the sponsor of this study, financial funding and involvement in the study design, writing of the protocol, ethical approval and review of the manuscript. The data collection, analysis, interpretation of data and writing were done by the authors independent from the sponsor.
Disclosure
The authors report no conflicts of interest in this work.
References
1. American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S111–S124. doi:10.2337/dc21-S009
2. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–2701. doi:10.2337/dci18-0033
3. American Diabetes Association. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S40–S52. doi:10.2337/dc21-S004
4. Barry MJ, Edgman-Levitan S. Shared decision making — the pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–781. doi:10.1056/NEJMp1109283
5. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. doi:10.1007/s11606-012-2077-6
6. Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making. 2014;35(1):114–131. doi:10.1177/0272989X14551638
7. Saheb Kashaf M, McGill ET, Berger ZD. Shared decision-making and outcomes in type 2 diabetes: a systematic review and meta-analysis. Patient Educ Couns. 2017;100(12):2159–2171. doi:10.1016/j.pec.2017.06.030
8. Elwyn G, Frosch DL, Kobrin S. Implementing shared decision-making: consider all the consequences. Implement Sci. 2016;11(1):114. doi:10.1186/s13012-016-0480-9
9. Bae J-M. Shared decision making: relevant concepts and facilitating strategies. Epidemiol Health. 2017;39:e2017048. doi:10.4178/epih.e2017048
10. Rutten GEHM, van Vugt HA, de Weerdt I, de Koning E. Implementation of a structured diabetes consultation model to facilitate a person-centered approach: results from a nationwide Dutch study. Diabetes Care. 2018;41(4):688–695. doi:10.2337/dc17-1194
11. Steenbergen M, de Vries J, Arts R, Beerepoot LV, Traa MJ. Barriers and facilitators for shared decision-making in oncology inpatient practice: an explorative study of the healthcare providers’ perspective. Support Care Cancer. 2022;30(5):3925–3931. doi:10.1007/s00520-022-06820-1
12. Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94(3):291–309. doi:10.1016/j.pec.2013.10.031
13. Flood EM, Bell KF, de la Cruz MC, Ginchereau-Sowell FM. Patient preferences for diabetes treatment attributes and drug classes. Curr Med Res Opin. 2017;33(2):261–268. doi:10.1080/03007995.2016.1253553
14. Toroski M, Kebriaeezadeh A, Esteghamati A, Karyani AK, Abbasian H, Nikfar S. Patient and physician preferences for type 2 diabetes medications: a systematic review. J Diabetes Metab Disord. 2019;18(2):643–656. doi:10.1007/s40200-019-00449-4
15. Bakker K, Bilo HJ. Diabetes care in The Netherlands: now and in the future. Pract Diabetes Int. 2004;21(2):88–91. doi:10.1002/pdi.595
16. Nederlands Huisartsen Genootschap. NHG-standaard diabetes mellitus type 2 (version 5.5); 2021.
17. Delbecq AL, Van de Ven AH, Gustafson DH. Group Techniques for Program Planning: A Guide to Nominal Group and Delphi Processes. Scott, Foresman; 1975.
18. International Consortium for Health Outcomes Measurement. The ICHOM standard set for adults who live with type 1 and 2 diabetes; 2018.
19. RStudio: integrated development for R [computer program]. Version 1. 4.1106. Boston, MA: RStudio, PBC; 2020.
20. Brabers AEM, de Jong JD. Nivel Consumentenpanel Gezondheidszorg: Basisrapport Met Informatie Over het Panel 2022. Utrecht: Nivel; 2022.
21. Sawtooth Software [computer program]. Utah, USA: Provo; 2021.
22. Sawtooth Software Inc. The MaxDiff system technical paper; 2013.
23. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594.
24. Johnson RM. Understanding HB: An Intuitive Approach. Sawtooth Software Inc; 2000.
25. Carlin JB, Doyle LW. Comparison of means and proportions using confidence intervals. J Paediatr Child Health. 2001;37(6):583–586. doi:10.1046/j.1440-1754.2001.00771.x
26. Weller BE, Bowen NK, Faubert SJ. Latent Class Analysis: a Guide to Best Practice. J Black Psychol. 2020;46(4):287–311. doi:10.1177/0095798420930932
27. Muthén LK, Muthén BO. Mplus User’s Guide.
28. Gopisetty D, Levine B, Liu N, et al. How does diabetes affect daily life? A beyond-A1C perspective on unmet needs. Clin Diabetes. 2018;36(2):133–137. doi:10.2337/cd17-0093
29. Ruissen MM, Sont JK, van Vugt HA, Kunneman M, Rutten G, de Koning EJP. Key factors relevant for healthcare decisions of patients with type 1 and type 2 diabetes in secondary care according to healthcare professionals. Patient Prefer Adherence. 2022;16:809–819. doi:10.2147/PPA.S354686
30. Mansfield C, Sikirica MV, Pugh A, et al. Patient preferences for attributes of type 2 diabetes mellitus medications in Germany and Spain: an online Discrete-Choice Experiment Survey. Diabetes ther. 2017;8(6):1365–1378. doi:10.1007/s13300-017-0326-8
31. Williams DM, Jones H, Stephens JW. Personalized type 2 diabetes management: an update on recent advances and recommendations. Diabetes Metab Syndr Obes. 2022;15:281–295. doi:10.2147/DMSO.S331654
32. Elwyn G, O’Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333(7565):417. doi:10.1136/bmj.38926.629329.AE
33. Willems AEM, Heijmans M, Brabers AEM, Rademakers J. Gezondheidsvaardigheden in Nederland: Factsheet Cijfers 2021. Utrecht: Nivel; 2022.
34. Nielen M, Poos R, Korevaar J. Diabetes Mellitus in Nederland. Prevalentie En Incidentie: Heden, Verleden En Toekomst. Utrecht: Nivel; 2020.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
