Back to Journals » Patient Preference and Adherence » Volume 17
Preferences for Rehabilitation in Persons with a History of Stroke: A Discrete Choice Experiment
Authors Noto S , Murata T, Saito S, Watanabe T, Kobayashi M
Received 1 May 2023
Accepted for publication 8 July 2023
Published 12 July 2023 Volume 2023:17 Pages 1611—1620
DOI https://doi.org/10.2147/PPA.S416699
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qizhi (Cathy) Yao
Shinichi Noto,1 Tatsunori Murata,2 Shota Saito,2 Takahiro Watanabe,3 Makoto Kobayashi2
1Department of Rehabilitation, Niigata University of Health and Welfare, Niigata, Japan; 2CRECON Medical Assessment Inc, Tokyo, Japan; 3Rehabilitation Center, Niigata University Medical and Dental General Hospital, Niigata, Japan
Correspondence: Shinichi Noto, Department of Rehabilitation, Niigata University of Health and Welfare, 1398 Shimami, Kita-ku, Niigata, Japan, Email [email protected]
Objective: To investigate the preferences of persons with a history of stroke for various attributes of rehabilitation using a discrete choice experiment (DCE).
Design: Cross-sectional study.
Setting: A web-based survey.
Participants: A total of 600 adults with a history of stroke who were not asked whether or not they had participated in previous rehabilitation.
Intervention: None.
Main Outcome Measures: Preference weights by attribute ie, treatment time (30 minutes, one hour, one and a half hours), treatment content (walking exercises, activities of daily living; ADL exercises), priority treatment of paralyzed limbs (upper extremity, lower upper extremity), treatment location (hospital visit, home visit), therapist gender, and out-of-pocket costs for stroke rehabilitation using discrete choice experiment.
Results: The most common self-reported diagnosis was cerebral infarction (408 patients, 68%). The mean age was 62.0 ± 9.8 years, and 515 (85.8%) were male. Of the five attributes, excluding out-of-pocket costs, the highest relative importance score was treatment location (0.331), followed by treatment time (0.304). Among the rehabilitation programs, the statistically significant coefficients calculated were one hour of therapy (0.173, 95% CI = 0.088– 0.258), hospital visits (0.241, 95% CI = 0.180– 0.303), and female therapists (0.186, 95% CI = 0.125– 0. 247). No significant differences were obtained regarding the treatment contents or the paralyzed limb to be treated.
Conclusion: A discrete choice experiment revealed that persons with a history of stroke prefer a one-hour hospital rehabilitation program with a female therapist, with cost being a major consideration for rehabilitation. The results of this study may provide useful information for rehabilitation professionals.
Keywords: stroke, rehabilitation, preference, physical therapy, occupational therapy
Introduction
Stroke was the second leading cause of death and disability-adjusted life years lost worldwide.1 About 1/3 of people who suffer a stroke are left with residual disabilities, placing a burden on their families and communities.2 Various guidelines3–5 for stroke rehabilitation have confirmed the necessity and effectiveness of various programs. Therefore, rehabilitation plays a very important role in stroke treatment. A comprehensive review summarized that programs had been implemented for sensory dysfunction, motor learning programs, unilateral neglect, flexibility and joint integrity, strength training, hypertonia, postural control, and gait training.6 The need to develop and share these diversities is also mentioned.7 In addition to these, transcranial magnetic stimulation8 and robot-assisted therapy9 have been developed in recent years, but traditionally, physiotherapy has been used to improve walking ability and occupational therapy to improve activities of daily living (ADL). Although the division of roles between the two is not generalized, both are indispensable. Therapy for recovery of a paralyzed limb can also be divided into upper and lower extremity therapy. Although these rehabilitation programs for stroke are implemented roughly as a set, it would be meaningful to identify patient preferences. In Japan, especially with regard to outpatient rehabilitation, in addition to rehabilitation conducted in hospitals, there is also home rehabilitation, which is conducted by visiting patients. Patients’ preferences and systems based on these variations in stroke rehabilitation are not fully taken into account.
In healthcare, over the recent years a growing interest in patient-reported health values has been seen, with concomitant increase in research on these values. Patient preference studies using discrete choice experiments (DCE) have increased over the past 20 years.10–12 The studies using those DCEs have ranged from evaluating clinical effectiveness, assessing health status, and setting treatment priorities, but only scattered studies investigating patient preferences for rehabilitation have been found. Boyde et al13 evaluated cardiac rehabilitation preferences and reported a strong preference for center-based programs over home-based programs and a preference for group rather than individual exercise. Napora et al14 also used DCE to study the preferences of upper extremity fracture patients for occupational therapy and found that patients were willing to pay $85 more per treatment if their range of motion improved by 40%. Gilbert et al15 reported that patients’ preferences in virtual consultations in an orthopedic rehabilitation setting were examined by DCE and found that they did not prefer to receive a 60-minute consultation at 2 pm from a therapist they did not know. With regard to stroke rehabilitation, Laver et al16 investigated stroke patients’ preferences for new approaches to rehabilitation, such as high-intensity therapy and virtual reality programs, and reported that they disliked overly intensive programs and computer-based therapy. In addition, Geidl et al17 reported a strong preference for light- and moderate-intensity exercise and a preference for shorter exercise durations with regard to patient preferences for stroke rehabilitation. Thus, while several studies have examined patient preferences for using DCE for rehabilitation, there are not enough studies with sufficiently large samples or that take into account a variety of other attributes related to stroke rehabilitation.
There is an increasing need to investigate patient preferences in assessing the value of health,18–20 and it would be meaningful to investigate the preferences of stroke patients for rehabilitation, which is an important need worldwide. In particular, stroke patients were considered to have a high need for outpatient rehabilitation to gain mobility and compensatory methods of activities of daily living even after discharge from the hospital. With the above background, this is the first attempt to investigate such preferences in stroke survivors on a large scale and is a significant study. In this study, we used DCE to extract attributes tailored to the Japanese rehabilitation system and examined the preferences of persons with a history of stroke.
Methods
To ensure the quality of the study design using DCE, we referred to the user guide by Lancsar & Louviere21 and the ISPOR task force22 and its good research practice.23 The important points are described in detail below.
Attributes and Levels Describing Stroke Rehabilitation
Attributes and levels used in the DCE were reviewed through interviews with two experts and a review of previous literature, and finally by health economists at the Centre for Health Economics and Quality of Life Research. In the literature search, we reviewed relevant articles based on the two systematic reviews on home rehabilitation.24,25 In addition, regarding the Japanese rehabilitation system, we reviewed the Japanese literature and picked up attributes from the relevant articles.26–28 As shown in Table 1, the attributes and levels were determined as treatment time (30 minutes, one hour, one and a half hours), treatment content (walking exercises, ADL exercises), priority treatment paralytic limb (upper extremity, lower extremity), treatment location (hospital visit, home visit), therapist gender, and out-of-pocket costs (7.5USD≈1000JPY, 22.6USD≈3000JPY, 37.7USD≈5000JPY). Regarding the level of treatment time, the guidelines for stroke rehabilitation17 recommend a minimum of 3 hours per day in acute inpatient facilities, but only outpatient rehabilitation in Japan can be provided for a minimum of 20 minutes, so we have included other attributes in this study to determine the level based on the current status of rehabilitation care in Japan. Therefore, the level of rehabilitation care in this study was determined based on the current status of rehabilitation care in Japan, including other attributes. Piloting was performed on three stroke patients undergoing rehabilitation at home to validate attributes and levels.
 |
Table 1 Finalized Attributes and Levels |
DCE Experiment Design
In this study, there are a total of 144 combinations of levels for each attribute in a full factorial design. To reduce the burden on respondents, we used the D-optimal design29 and selected the 48 choice sets to be used in the DCE with a modified Fedorov algorithm to optimize D-error using Ngene version 1.3; ChoiceMetrics Pty Ltd, Sydney, NSW, Australia. We divided the 48 choice sets into 3 blocks to reduce the number to 16 for each respondent. In the DCE, two hypothetical stroke rehabilitation programs were simultaneously presented to respondents based on a combination of levels selected one by one from each attribute, and respondents were asked to choose the option they preferred from the two hypothetical programs. For the 16 choice sets, respondents were randomly assigned to one of the blocks. Furthermore, as shown in Figure 1, we presented the choice set with an illustration for each option to reduce the burden on the respondent. The detailed procedure of the D-optimal design is added in the Supplementary File (Table S1).
 |
Figure 1 Example of DCE task. The respondent chooses the set of rehabilitation they prefer from the set of A or B attributes presented to them. |
Sample Size and Data Collection
The target sample size of this study was 600 persons with a history of stroke. We used D-error to assess the efficiency of DCE design. Ngene software was used to estimate D-error and the value of D-error in our design was 0.167.
We conducted a survey of Japanese persons with a history of stroke, in which they were asked to complete a web-based questionnaire. In April 2022, the survey was administered by Rakuten Insight Inc. This research company has approximately two thousand people with a history of stroke panel throughout Japan, and 600 were recruited from that target persons on a first-come, first-served basis. Participants were eligible if they were aged 18 years or older who resided in Japan and had a previous diagnosis of stroke. Because almost all stroke patients in the Japanese health care system receive previous rehabilitation, we did not ask whether or not they participated in rehabilitation as a sample selection criterion.
Instrumental Design
In addition to demographic information, we asked the subjects about the diagnosis of stroke, duration of stroke, current symptoms, and ADL level using the Barthel Index.30 In addition, health-related quality of life was assessed using the EQ-5D-5L.31 Response to the burden of the survey was assessed by a pilot testing.
Ethical Procedures and Consent Formation
This study was conducted with the approval of the Ethical Review Committee of Niigata University of Health and Welfare (18794-220207) and conducted by the Declaration of Helsinki. Consent for participants was obtained through a web-based survey process that included a section asking for explanation and consent, and only those who gave their consent were allowed to respond.
Statistical Analysis
The information on the choice of stroke rehabilitation in the choice experiment collected by the DCE method was analyzed for the influence of attributes or levels on the respondents’ choice by regression analysis using the conditional logit model.32 This model is based on random utility theory, as expressed in the following equation:
wherein the utility, Uij that an individual i derives from choosing healthcare option j, is specified and Xij is a vector of design attributes, β is a vector of coefficients to be estimated and εij is an unobservable error term, which is assumed to be an independently and identically distributed type 1 extreme value. In the conditional logit model, all attributes except cost were dummy coded, with one level being omitted. In the conditional logit model, all attributes were dummy coded (categorical) and one level (reference level) was omitted. The effect of attribute on the probability of choosing stroke rehabilitation in the choice experiment was calculated as an interpretation of estimates for each attribute level. Statistical analyses were performed using Stata statistical software version 15.0; StataCorp, College Station, TX, USA.The relative importance (RI) of each attribute was calculated by determining the differences between the maximum and minimum coefficients of each attribute, which were then normalized, presented as percentages, and ranked.
Results
Characteristics of the Participants
Of the approximately 2000 persons on the Rakuten Insight Inc. stroke panel, 600 participated on a first-come, first-served basis. Table 2 shows the demographic and health characteristics of the participants. Of the total, 85.8% were male (n=515). The most common age group was 60–69 years, and the mean age of all participants was 62.0 (SD: standard deviation=9.8) years. The most common stroke diagnosis was cerebral infarction in 408 participants (68.0%) and cerebral hemorrhage in 136 participants (22.7%). The mean Barthel Index for all participants was 97.8 (SD = 8.1), and the mean EQ-5D-5L score was 0.89 (SD = 0.15).
 |
Table 2 Demographic Factors of the Study Participants |
Participant Preferences by DCE
Table 3 presents the results of the mixed logit model. The factors included in the DCE indicate the coefficient for each factor relative to the reference level. A higher coefficient value indicates a preference for that factor level relative to the reference level (eg, one hour is preferred over 30 minutes for treatment time, and a hospital visit is preferred over a home visit for treatment location. The results show that participant preferences are influenced by the four attributes included in the experiment (treatment time (coefficient=0.083), treatment location (coefficient=0.121), therapist gender (coefficient=0.093), and cost (coefficient=0.854)), with cost having a particularly strong influence. On the other hand, we find that the treatment and the preferred priority treatment paralytic limb are less affected. Persons with a history of stroke prefer to have one hour of treatment performed by a female therapist on an outpatient basis, and no clear preference was shown for walking exercise versus ADL exercise. Figure 2 shows the weights of preference for the levels of attributes, with the weighting of the vertical axis indicating the degree to which one attribute was selected.
 |
Table 3 Conditional Logit Results |
 |
Figure 2 Preference weights for attribute levels. The greater the preference weight, the greater the preference for the condition of that attribute. |
Excluding cost, three attributes accounted for a large proportion of relative importance as shown in Figure 3: treatment location (RI = 35.5%), gender of therapist (RI = 27.4%), and treatment time (RI = 25.4%).
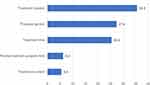 |
Figure 3 Relative importance of attributes excluding cost. A larger percentage indicates greater relative importance in the five attributes. |
Additionally, stratified analysis by sex and age group (60<, ≤60) of the participants was also performed, but no differences in preference trends were found. In particular, females (coefficient 0.497; SE: standard error = 0.087) preferred a female therapist more than did males (coefficient 0.140; SE 0.033) in terms of therapist gender (Tables S2–S5).
Discussion
This study reports on the preferences of people with a history of stroke rehabilitation. The purpose of this study was not only to examine the preferences of people with a history of stroke for stroke rehabilitation programs, but also to understand their perceptions of such rehabilitation. We found that preferences for treatment time, treatment location, and therapist gender were stronger than the conscious claims of stroke rehabilitation specialists regarding their expertise. These findings provide important evidence for future stroke rehabilitation decision making because of the perspective of patient preferences.
First, we discuss the fact that the attribute that showed the largest weight among the attributes with respect to the preference weights was out-of-pocket costs. It is reasonable to assume that the level of out-of-pocket costs varied by a factor of 3 or 5 based on a standard of 7.5USD (1000JPY), which had a significant impact on the choice of DCE. In Japanese studies that have examined willingness-to-pay using DCEs, the range of their out-of-pocket cost levels has been set within a factor of 2 at most.33 In many studies that set the level of out-of-pocket costs at three times or more, the preference weights are much larger than for other attributes.34–36 The decision to use the current study design was based on the fact that the Japanese healthcare system has a 1- to 3-fold difference in the amount of out-of-pocket costs depending on the patient’s age and that rehabilitation services are increasingly being provided outside the healthcare system, albeit partially, at one’s own expense. Additionally, many of the participants in this study were more than two years from the onset of the disease, suggesting that cost may have been more important than the need for rehabilitation services. Because of this strong influence of cost, the impact of other attributes may have been relatively underestimated. Since the original purpose of this study was to examine preferences regarding the content of stroke rehabilitation, the analysis was conducted after excluding out-of-pocket costs.
Next, we discuss how the preferences of people with a history of stroke for rehabilitation programs are more strongly influenced by location, time, and therapist gender than by treatment content with respect to attributes excluding out-of-pocket costs. In the Japanese health care system, almost all patients receive both physical therapy and occupational therapy at the same time, and there is no choice. In addition, ADL exercises may be performed by a physical therapist in addition to an occupational therapist, and people with a history of stroke may not understand the difference between the two. Furthermore, people with a history of stroke did not express any preference as to which paralyzed limb they thought should be treated first. This is very interesting because it suggests stroke survivors seek improvement in the upper and lower extremities.
A notable finding emerged from the results of this study. People with a history of stroke prefer female therapists, regardless of participant demographics. From a gender equality perspective, it may not be appropriate to specify gender and ask about preference for one or the other. Still, this study was conducted solely as a survey of preferences. On the other hand, there have been reports on the gender of physicians. For example, Tsugawa et al37 examined the differences in mortality and readmission rates between male and female physicians in patients with medical conditions and reported that female physicians performed better on both measures. They also reported that female physicians adhere more to clinical guidelines38 and communicate in a more patient-centered manner than did male physicians,39 which could be the basis for these findings. On the other hand, there is also a report that female physicians are evaluated more strictly,40 which may be a matter of interpretation. However, the results of the present study are not simply comparable to those of physiotherapists and occupational therapists, but they should provide encouragement to female therapists engaged in clinical practice and academic medicine as a clear selection shown by those with a history of stroke.
Study Limitations
Limitations of this study are as follows. First, most of the participants in the study had a history of stroke more than two years after the onset of the stroke. Therefore, many of them could not recall the rehabilitation they had previously received or did not currently require much rehabilitation. There was also a significant male bias among the participants. As shown in the supplementary stratified analysis, we did not identify any significant difference in trend between the two groups in this respect. Still, since there is no such gender difference in stroke patients, we believe this could have influenced the results in no small way. Second, the participants had a high level of independence in ADLs, and many of them did not have a high need for rehabilitation. Since their needs for both quantity and quality of rehabilitation may be different if their level of independence is lower, we would like to conduct a similar study with stroke patients soon after the onset of stroke in the future. Third, since the survey was conducted via the Internet, it is not clear whether the attributes and levels of rehabilitation were fully understood. In future surveys, we would like to examine the level of understanding of these attributes. Finally, although this study was conducted on stroke rehabilitation, it is not clear whether the results can be generalized to rehabilitation for other diseases.
Conclusions
This study is the first full-scale investigation of preferences for stroke rehabilitation, showing that persons with a history of stroke prefer to be treated by a female therapist (coefficient=0.093) for one hour (coefficient=0.083) in the hospital, with out-of-pocket costs being the most important factor (coefficient=0.854). However, they showed no significant preference for walking exercise versus ADL exercise or for the limb that should be treated as a priority. These results suggest a realistic preference among persons with a history of stroke, but also suggest the possibility of insufficient understanding of treatment content and the need for more shared decision-making.
Abbreviations
ADL, activities of daily living; DCE, discrete choice experiments; RI, relative importance; SD, standard deviation; CI, confidence interval; SE, standard error.
Acknowledgments
The abstract of this paper was presented at the ISPOR Europe 2022 as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Value in Health: Hyperlink with https://doi.org/10.1016/j.jval.2022.09.2174. We would like to thank Honyaku Center Inc. for English language editing.
Funding
This study was funded by Grant-in-Aid for Scientific Research (KAKENHI) from Japan Society for the Promotion of Science (21H03172).
Disclosure
Dr Shinichi Noto reports grants from Japan Society for the Promotion of Science, during the conduct of the study. The authors declare that they have no other competing interests.
References
1. Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. doi:10.1016/S1474-4422(21)00252-0
2. World Health Organization (WHO). The Atlas of Heart Disease and Stroke. Geneva: World Health Organization (WHO); 2004.
3. Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98–e169. doi:10.1161/STR.0000000000000098
4. The National Institute for Health and Care Excellence. Stroke rehabilitation in adults. Available from: https://www.nice.org.uk/guidance/cg162.
5. Gladstone DJ, Lindsay MP, Douketis J, et al. Canadian stroke best practice recommendations: secondary prevention of stroke update 2020. Can J Neurol Sci. 2022;49(3):315–337. doi:10.1017/cjn.2021.127
6. Shahid J, Kashif A, Shahid MK. A comprehensive review of physical therapy interventions for stroke rehabilitation: impairment-based approaches and functional goals. Brain Sci. 2023;13(5):717. doi:10.3390/brainsci13050717
7. Morone G, Pichiorri F. Post-stroke rehabilitation: challenges and new perspectives. J Clin Med. 2023;12(2):550. doi:10.3390/jcm12020550
8. Starosta M, Cichoń N, Saluk-Bijak J, Miller E. Benefits from repetitive transcranial magnetic stimulation in post-stroke rehabilitation. J Clin Med. 2022;11(8):2149. doi:10.3390/jcm11082149
9. Straudi S, Baluardo L, Arienti C, et al. Effectiveness of robot-assisted arm therapy in stroke rehabilitation: an overview of systematic reviews. NeuroRehabilitation. 2022;51(4):559–576. doi:10.3233/NRE-220027
10. de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–172. doi:10.1002/hec.1697
11. Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. Pharmacoeconomics. 2019;37(2):201–226. doi:10.1007/s40273-018-0734-2
12. Vass C, Boeri M, Karim S, et al. Accounting for preference heterogeneity in discrete-choice experiments: an ISPOR Special Interest Group report. Value Health. 2022;25(5):685–694. doi:10.1016/j.jval.2022.01.012
13. Boyde M, Rankin J, Whitty JA, et al. Patient preferences for the delivery of cardiac rehabilitation. Patient Educ Couns. 2018;101(12):2162–2169. doi:10.1016/j.pec.2018.07.010
14. Napora JK, Demyanovich H, Mulliken A, et al. Patients’ preferences for occupational therapy after upper extremity fractures: a discrete choice experiment. BMJ Open. 2020;10(10):e039888. doi:10.1136/bmjopen-2020-039888
15. Gilbert AW, Mentzakis E, May CR, et al. Patient preferences for use of virtual consultations in an orthopaedic rehabilitation setting: results from a discrete choice experiment. J Health Serv Res Policy. 2022;27(1):62–73. doi:10.1177/13558196211035427
16. Laver K, Ratcliffe J, George S, et al. Preferences for rehabilitation service delivery: a comparison of the views of patients, occupational therapists and other rehabilitation clinicians using a discrete choice experiment. Aust Occup Ther J. 2013;60(2):93–100. doi:10.1111/1440-1630.12018
17. Geidl W, Knocke K, Schupp W, Pfeifer K. Measuring stroke patients’ exercise preferences using a discrete choice experiment. Neurol Int. 2018;10(1):6993. doi:10.4081/ni.2018.6993
18. Ozdemir S, Lee JJ, Chaudhry I, Ocampo RRQ. A systematic review of discrete choice experiments and conjoint analysis on genetic testing. Patient. 2022;15(1):39–54. doi:10.1007/s40271-021-00531-1
19. Zartab S, Nikfar S, Karimpour-Fard N, et al. A systematic review of discrete choice experiment studies in rheumatoid arthritis biological medicines. Mediterr J Rheumatol. 2021;32(2):104–111. doi:10.31138/mjr.32.2.104
20. Tünneßen M, Hiligsmann M, Stock S, Vennedey V. Patients’ preferences for the treatment of anxiety and depressive disorders: a systematic review of discrete choice experiments. J Med Econ. 2020;23(6):546–556. doi:10.1080/13696998.2020.1725022
21. Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–677. doi:10.2165/00019053-200826080-00004
22. Reed Johnson F, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13. doi:10.1016/j.jval.2012.08.2223
23. Janssen EM, Hauber AB, Bridges JFP. Conducting a discrete-choice experiment study following recommendations for good research practices: an application for eliciting patient preferences for diabetes treatments. Value Health. 2018;21(1):59–68. doi:10.1016/j.jval.2017.07.001
24. Siemonsma P, Döpp C, Alpay L, et al. Determinants influencing the implementation of home-based stroke rehabilitation: a systematic review. Disabil Rehabil. 2014;36:2019–2030. doi:10.3109/09638288.2014.885091
25. Qin P, Cai C, Chen X, Wei X. Effect of home-based interventions on basic activities of daily living for patients who had a stroke: a systematic review with meta-analysis. BMJ Open. 2022;12(7):e056045. doi:10.1136/bmjopen-2021-056045
26. Shinohara T, Tsuchida N, Yamane T, et al. Association between patients’ state upon admission and decline in activities of daily living. J Phys Ther Sci. 2019;31(10):813–818. doi:10.1589/jpts.31.813
27. Takamatsu K, Hiramatsu Y, Fujita N, et al. Longitudinal changes in functional Independence measure motor subscores of patients with stroke discharged to home from a convalescence rehabilitation ward. Rigakuryoho Kagaku. 2022;37(2):153–157. in Japanese. doi:10.1589/rika.37.153
28. Yoshino T, Iijima S. Physical therapy for stroke outpatients: differing therapeutic aims of patients and therapists may prolong outpatient therapy. J Jpn Phys Ther Assoc. 2003;30(5):296–303. in Japanese.
29. Jonker MF, Bliemer MCJ. On the optimization of Bayesian D-efficient discrete choice experiment designs for the estimation of QALY tariffs that are corrected for nonlinear time preferences. Value Health. 2019;22(10):1162–1169. doi:10.1016/j.jval.2019.05.014
30. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65.
31. Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736. doi:10.1007/s11136-011-9903-x
32. McFadden D. Conditional logit analysis of qualitative choice behavior. In: Zarembka P, editor. Frontiers in Econometrics. New York: Academic Press; 1974:105–142.
33. Tada Y, Ishii K, Kimura J, et al. Patient preference for biologic treatments of psoriasis in Japan. J Dermatol. 2019;46(6):466–477. doi:10.1111/1346-8138.14870
34. Zhao J, Wang H, Li X, et al. Importance of attributes and willingness to pay for oral anticoagulant therapy in patients with atrial fibrillation in China: a discrete choice experiment. PLOS Med. 2021;18(8):e1003730. doi:10.1371/journal.pmed.1003730
35. Thach A, Sutphin J, Coulter J, et al. Patient preferences for treating “OFF” episodes in Parkinson’s disease: a discrete choice experiment. Patient Prefer Adherence. 2021;15:1187–1196. doi:10.2147/PPA.S301644
36. Mansfield C, Gebben DJ, Sutphin J, et al. Patient preferences for preventive migraine treatments: a discrete-choice experiment. Headache. 2019;59(5):715–726. doi:10.1111/head.13498
37. Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206–213. doi:10.1001/jamainternmed.2016.7875
38. Berthold HK, Gouni-Berthold I, Bestehorn KP, et al. Physician gender is associated with the quality of type 2 diabetes care. J Intern Med. 2008;264(4):340–350. doi:10.1111/j.1365-2796.2008.01967.x
39. Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756–764. doi:10.1001/jama.288.6.756
40. Rogo-Gupta LJ, Haunschild C, Altamirano J, et al. Physician gender is associated with press Ganey patient satisfaction scores in outpatient gynecology. Womens Health Issues. 2018;28(3):281–285. doi:10.1016/j.whi.2018.01.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

