Back to Journals » International Journal of General Medicine » Volume 13
Predictors of ST Depression Resolution in STEMI Patients Undergoing Primary PCI and Its Clinical Significance
Authors Ghaffari S , Kolahdouzan K , Rahimi M, Tajlil A
Received 17 April 2020
Accepted for publication 28 May 2020
Published 8 June 2020 Volume 2020:13 Pages 271—279
DOI https://doi.org/10.2147/IJGM.S258573
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Samad Ghaffari,1 Kasra Kolahdouzan,2 Mehran Rahimi,1 Arezou Tajlil1
1Cardiovascular Research Center, Tabriz University of Medical Sciences, Tabriz, Iran; 2Cancer Institute, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
Correspondence: Kasra Kolahdouzan
Imam Khomeini Hospital Complex, Cancer Institute, Keshavarz Boulevard, Tehran, Iran
Tel +98-9144083785
Email [email protected]
Purpose: ST depression resolution (STD-R) in ECG is a prognostic factor indicative of successful fibrinolysis or angioplasty in the treatment of ST elevation myocardial infarction (STEMI) and subsequent mortality. We conducted this study to determine the clinical significance of STD-R and its predictors in patients with anterior STEMI undergoing primary percutaneous intervention (PPCI).
Methods: Admission documents of all patients with diagnosis of anterior STEMI who were admitted to a specialty heart center and underwent PPCI since July 2018 until July 2019 were examined. The amount of ST elevation and depression in all 12 leads of a standard ECG at admission and 90 minutes after PPCI was measured and resolution was determined. All patients were followed-up for 10.8± 4.0 months.
Results: A total of 179 patients had ST depression besides elevation in the first ECG. Female gender, diabetes, not smoking, lower hemoglobin, and higher platelet counts were significantly more common in the group with less than 50% resolution of ST depression. STD-R < 50% was significantly associated with the incidence of in-hospital acute heart failure and major adverse cardiac events (MACE) (p value: 0.025 and 0.012, respectively) and resolution of ST elevation ≥ 50% was associated with reduced in-hospital mortality (p value < 0.0001). According to Kaplan–Meier curve, survival in the two groups of STE-R ≥ 50% and STE-R < 50% was significantly different (Log rank: 31.18, p value< 0.0001).
Conclusion: STD-R can be considered to have high predictive power, like STE-R for predicting incidence of in-hospital acute heart failure and major adverse cardiac events.
Keywords: ST elevation resolution, ST depression resolution, primary percutaneous intervention, major adverse cardiac events
Introduction
Cardiovascular diseases are the primary cause of mortality in the world and according to WHO statistics, about 17.9 million people die of cardiovascular diseases annually, which accounts for 31% of all global deaths.1 Myocardial infarction, being the main contributor to the cardiovascular diseases superfamily, is a term used when there is evidence of myocardial necrosis in a clinical setting consistent with acute myocardial ischemia.2
According to previous studies, ST segment elevation resolution (STE-R) in electrocardiogram is an important prognostic factor of successful fibrinolysis or angioplasty in the treatment of ST elevation myocardial infarction (STEMI).3–5 Due to the importance of STE-R in determining in-hospital and long-term prognosis of patients with myocardial infarction after thrombolysis or angioplasty,6,7 finding predictive factors for STE-R can be extremely valuable.
Incidence and amount of resolution of ST segment depression (STD-R) and its effect on mortality has also been studied and in some cases, it has been associated with superior prognostic value to STE-R in prediction of mortality.6,8-10
Regarding the fact that pathophysiologic mechanisms for incidence of ST elevation and ST depression are somewhat different,11–14 it is hypothesized that predictive factors for STE-R would also be different from STD-R predictive factors, and so determining these factors especially for STD-R would create the opportunity to identify high-risk patients before primary percutaneous cardiac interventions (PPCI).
Due to the prognostic importance of STD-R and as thus far no study has been conducted to determine the predictive factors for it, we decided to conduct the present study to assess the clinical importance and predictive factors for amount of ST depression resolution in ST elevation MI patients undergoing primary PCI.
Materials and Methods
Demographic and hospital data of all patients who were admitted with the diagnosis of ST elevation myocardial infarction to the emergency department (ED) of Shahid Madani specialty heart center in Tabriz, Iran, and underwent primary percutaneous cardiac intervention, were retrospectively collected from July 2018 to July 2019. This study was registered and approved by the national ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1395.1218) and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. All included patients provided written informed consent to review their medical records on admission to the hospital.
Exclusion criteria were: left bundle branch block (LBBB), pacemaker rhythm, receiving thrombolysis therapy before or during admission to emergency department and absence of ST elevation in the on-admission ECG.
Diagnostic criteria for ST elevation myocardial infarction were taken into account such as: chest pain lasting more than thirty minutes plus one of the following; ST segment elevation in J point in at least 2 associated leads greater than or equal to 0.2 mVs in V1, V2, V3 or greater than or equal to 0.1 mVs in other leads.
Standard electrocardiograms (25 mm per second recording speed and 1 mV per centimeter voltage) were recorded for all patients on admission and 90 minutes after primary PCI. The exact amount of elevation and depression of ST segment in both ECGs was measured with the help of computer magnification with an accuracy of 0.5 millimeters. Demographic data and clinical presentation on admission to ED and the time from chest pain initiation to ED and Cath Lab were recorded from patients’ clinical documents. Also, laboratory data and angioplasty records were gathered. All patients were followed up via telephone 6 to 17 months after discharge and their health status assessed, and if deceased, exact death time was recorded.
Statistical Methods
All data were analyzed using IBM SPSS Statistics Version 26. Normality of data distribution for quantitative data was assessed with Kolmogorov–Smirnov test. Simple frequency tests were used to determine frequency, mean and standard deviation. Multivariate analysis was used to test for significant correlation between independent and dependent variables and also, univariate analysis was conducted to check for correlation between independent variables with each of the dependent variables. For binary categorical data, chi squared test was used and for quantitative data, significance of difference between means in two groups (STD-R or STE-R greater or equal to 50%) was assessed with t-test for normally distributed independent variables and p<0.05 was considered as the significance cut-off. In-hospital acute heart failure, in-hospital death, major adverse cardiac events (MACE) and death during follow-up were this study’s outcomes with MACE being defined as occurrence of heart failure or death, and association of amount of STD-R and STE-R with these outcomes was assessed using Chi squared test with a significance level of p<0.05 after considering a cut off of 50% for amount of resolution.
All included patients in the study were distributed in two groups depending on resolution of sum of depressions on admission ECG; 1- STD-R <50%, and 2- STD-R ≥50%. Amount of resolution of sum of ST elevations and depressions was calculated using the following formulas:
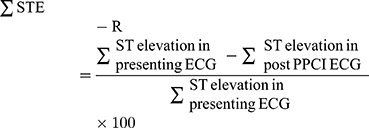
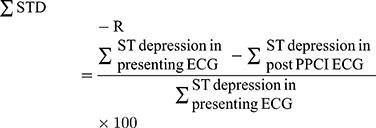
Similar formulas were used to measure STD-R and STE-R in a single lead with maximum depression or elevation in the first ECG.
Receiver operating curves (ROC curves) were plotted and their area under the curve (AUC) was calculated for primary outcomes (in-hospital death and MACE) in association to sum and single lead STD-R/STE-R. Also using ROC curves, we determined cut off points for resolution that concurrently had the highest specificity and sensitivity for prediction of the primary outcomes.
By using Kaplan–Meier curves, survival was compared between groups of STD-R/STE-R more or less than 50%. Significance of survival difference between groups was determined using log rank test with p value significance of less than 0.05.
Results
Among 237 patients with anterior STEMI who were admitted from July 2018 to July 2019 in Tabriz Shahid Madani specialty heart center and underwent primary PCI, after examining their clinical documents, we noticed that 15 cases had actually undergone rescue PCI and had received fibrinolysis in a previous first line center and so were excluded from the study. Finally, 222 patients (173 males and 49 females) constituted our study population. From these, 179 patients (80.6%) had concurrent ST segment depression in another lead besides ST elevation.
For the purpose of a clear understanding of the differences associated with demographic, electrocardiographic, angiographic, laboratory data, and in-hospital complications of participants, they were categorized into two groups; 1- STD-R <50% and 2- STD-R ≥50% (Table 1).
Fifty-two patients had STD-R <50% (24 with STE-R <50%, 28 with STE-R ≥50%) and 127 had STD-R ≥50% (56 with STE-R <50%, 71 with STE-R ≥50%). Thirty-three (63.5%) patients with STD-R <50% were male whereas 154 (82.7%) patients with STD-R ≥50% were male (p value =0.016). Moreover, in the group with STD-R <50%, 36.5% had diabetes mellitus and 21.2% were smokers whereas in the group with STD-R ≥50% only 21.3% were diabetic (p value=0.038) but 55.1% were smokers (p value=0.0001).
In laboratory data, platelet to lymphocyte ratio in STD-R <50% was 186.84±248.89 vs. 136.90±63.01 in STD-R ≥50% (p value=0.051). Also, hemoglobin level was 14.58±2.05 (STD-R <50%) vs. 15.40±1.97 (STD-R ≥50%) with a p value of 0.013
In Table 2, factors associated with ST elevation resolution are shown from which we can refer to previous MI history, ventricular fibrillation on admission and high levels of triglyceride, cholesterol, and LDL.
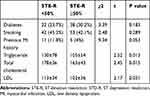 |
Table 2 Comparison of Patients Grouped as Having STE-R ≥50%, or STE-R <50% for Clinically Important Variables |
To determine the predictive factors of resolution of ST depression and elevation, multivariate and univariate logistic regression analyses were used, the results of which are shown in Table 3. In univariate analysis, factors like being a smoker (OR: 0.218 P<0.001), being non-diabetic (OR: 2.132 P value: 0.036), having higher levels of hemoglobin (OR: 1.225, P value: 0.016), and lower numbers of platelet count (OR: 0.994, P value: 0.016) were predictive of ≥50% resolution of ST depression.
 |
Table 3 Results of Univariate and Multivariate Regression Analyses to Determine Predictive Factors for Sum of ST Depression/Elevation Resolution of More Than 50% |
In Table 3, results of multivariate logistic regression analysis are also reported. In a multivariate model, being a non-smoker predicted independently, resolution of less than 50% of ST depression in study population with OR: 0.236, and p value=0.001. Also, according to the regression model, the odds for STD-R ≥50% decreased 5% for each 10,000 increase in platelet count (OR: 0.995, p value =0.050).
Moreover, only previous MI history had the independent predictive power for STE-R <50% with OR: 5.34, p value= 0.016), however, higher cholesterol levels (OR: 0.991, P value: 0.017) and LDL (OR: 0.990, P value: 0.034) were predictors of ST elevation resolution less than 50% in the univariate analysis.
Results for correlation of STD/STE resolution (≥50% or <50%) with outcomes such as in-hospital mortality, acute in-hospital heart failure, major adverse cardiac events (MACE), and death during follow-up are shown in Table 4.
The correlation of sigma STD-R <50% with incidence of acute heart failure and MACE was significant (p value= 0.025 and 0.012, respectively).
Also, correlation of STD-R <50% in a single lead with maximum primary depression on admission ECG with incidence of acute heart failure and MACE and also in-hospital mortality was statistically significant (p values: 0.04, 0.019, and 0.015 respectively).
In order to determine the difference of statistical diagnostic power for diagnosis of in-hospital mortality and probability of incidence of MACE between STD-R and STE-R (sigma or single lead), and also to determine cutoff points for maximum specificity and sensitivity for prediction of the previously mentioned outcomes, we produced receiver operating curves (ROC), as depicted in Figures 1 and 2.
In Figure 1A the area under the curve (AUC) for MACE in association with sigma STD/STE resolution respectively was 0.607±0.049/0.572±0.048 (p value: 0.028/0.136) and in Figure 1B the AUC for in-hospital mortality in relation to Sigma STD/STE resolution was respectively; 0.751±0.091/0.729±0.065 (p value: 0.011/0.021). In this curve in a cutoff point of 53% of STD-R, sensitivity and specificity were respectively 78% and 65%.
In Figure 2A, the AUC for MACE in relation to STD/STE resolution in a single lead with maximum ST deviation in the presenting electrocardiogram respectively was 0.607±0.049/0.553±0.049 (p value: 0.026/0.275). In Figure 2B, the AUC for in-hospital mortality in relation to STD/STE resolution in a single lead with maximum ST deviation in presenting electrocardiogram respectively was 0.769±0.096/0.648±0.104 (p value: 0.007/0.135). In this curve in a cutoff point of 54% of STD-R, sensitivity and specificity were respectively 78% and 74%.
As depicted in Figure 3, Kaplan–Meier survival curves were created for comparison of mortality and survival in different groups of ST deviation in accord with a cutoff of 50%. Patients with STE-R ≥50%, had a significantly longer survival time compared to those with a less than 50% STE-R (log rank: 31.18, p value <0.0001), however, a significant survival association of STD-R was not observed (log rank: 0.372, p value: 0.83).
Discussion
To rationalize briefly the reasons for ST segment depression occurrence while myocardial infarction besides ST segment elevation in other leads, the following reasons have been elaborated on: 1) reciprocal picture of ST elevation that is described as a benign electrical phenomenon associated with the time since beginning of symptoms that does not predict adverse events,11,13 2) larger infarct size12(in anterior STEMI, inferior ST depression is associated with larger infarct size), 3) ischemia at a distance from the initial infarct location14(associated with a higher risk of fatal arrhythmias and latent morbidity), 4) posterior wall injury in patients with inferior infarct.15
Previous studies have revealed a predictive role for amount of ST depression in acute anterior MI patients in in-hospital mortality,16 however, the prominent characteristic of this study is the parallel survey of resolution of both elevation and depression of ST segment and comparison of these two in incidence of in-hospital outcomes such as death and acute heart failure and also out of hospital outcome, ie, mortality in one year follow-up time. Moreover, we analyzed both sigma ST depression/elevation resolution and resolution in a single lead with maximum deviation in the presenting ECG. The reason for selection of ST depression resolution for analysis (and not just ST elevation resolution) in spite of the fact that most previous studies studied it for its effect on in-hospital major adverse cardiac events and 1 year follow-up mortality, was that a few studies had noted that it might have a better prognostic power in short and long time mortality.8–10,17
As seen in Table 4 of this study, less than 50% resolution of ST elevation (sum and single lead) is significantly associated with higher in-hospital mortality, which is in accord with previous studies. Also, less than 50% resolution of ST depression (sum and single lead) was significantly associated with incidence of in-hospital acute heart failure and also major adverse cardiac events. In this study, STD-R <50% had a significant association with occurrence of heart failure but not mortality. Elaboration of these findings could be that ST depression results from “ischemia at a distance”14 and the extent of coronary artery disease and so the larger area of ischemia and necrosis responsible for longer lasting ST depression, made these patients with STD-R <50% more susceptible to heart failure. However, the lower mortality rate in this group might stem from the fact that the present study’s follow-up time was only one year and with longer follow-up periods, results might be different.
In this study, patients were categorized into two groups of STD-R ≥50% and STD-R <50% and different variables in these two groups were compared with each other. Female sex, diabetes, not smoking, lower hemoglobin levels, higher platelet numbers, and higher platelet to lymphocyte ratio were more frequent in the group with STD-R less than 50%.
The fact that smoking correlated with more ST depression resolution might be due to the fact that smokers were younger and had better outcome than the older non-smokers who had more comorbidities and cardiovascular risk factors.
Univariate and multivariate logistic regression analyses were undertaken to determine the predictive factors for less than 50% resolution of elevation and depression of ST segment; the qualitative variables predicting STD-R <50% were: female gender, not smoking, and having diabetes mellitus. Also, the results for quantitative results were as follows; for each 1 mg/dL increase in hemoglobin level the probability of having STD-R ≥50% increased for 22.5% and for each 10,000 increase in platelet numbers, the probability of STD-R ≥50% decreased for 6%. Similar results were acquired in multivariate regression analysis only for cigarette smoking and platelet numbers. However, for STE-R among qualitative variables, only previous history of MI had an independent predictive value for STE-R <50% in both univariate and multivariate analyses. Moreover, in univariate analysis, higher levels of cholesterol, triglyceride, and LDL predicted a less than 50% ST elevation resolution.
In this study patients were followed up after discharge for 10.8±4 (6 to 17) months. Regarding the Kaplan–Meier curves plotted, based on percent of STD/E resolution more or less than 50%, those patients with less than 50% resolution had higher mortality rates. The outstanding point in this regard is that patients with less than 50% resolution of ST depression had a higher early in-hospital mortality and in the following one year follow-up period they did not have a significantly higher mortality rate than the group with more than 50% resolution. Few studies were found in the literature with similar investigations from which we can point out a study by Kozuc et al8 in 2007 which had a relatively longer 5 year follow-up time. According to the survival curves drawn for 3 groups of complete, partial, and incomplete resolution of ST depression, significant difference between survival rates was detected only after 500 days of admission to hospital. Besides, in a study by De Luca et al17 in 2005, patients with ST depression resolution less than 50% had mortality only in the first 30 days after admission and mortality was very low in the 1 year follow-up time in this group. In another study conducted by Reinstadler et al18 in 2015, they defined another group that had a resolution of less than zero which included the patients that had a greater sum depression in post-angioplasty ECG than the presenting ECG. Similar to the aforementioned studies, the group with less than 50% resolution had significantly higher mortality rates only in the first 2 weeks and in the following one year follow-up, their mortality rates were not higher than the group with more than 50% resolution, however, the group with less than 0% resolution had significantly higher mortality in the 1-year follow-up period than the other two groups (Log rank p value <0.001).
Another outstanding feature of this study was the plotting of ROC curves and the area under the curve (AUC) for in-hospital major adverse cardiac events and in-hospital mortality in relation to resolution of elevation and depression of ST segment, and, as seen in Figures 1 and 2, sum STD-R and STD-R in a single lead with maximum primary depression was an appropriate predictor especially for in-hospital mortality in all cases. Also, in ROC curves for in-hospital mortality in relation to STD-R, a cut-off point of about 54% for resolution of depression (both sum and single lead), had a sensitivity of 78% for both and a specificity of 65% and 74% respectively for ∑STD-R and STD-R in a single lead. For this reason, selection of a cut-off point of 50% for amount of ST segment depression resolution has an appropriate predictive power regarding in-hospital mortality.
Although both calculation methods of ST depression resolution (sum of depressions, or depression in a single lead with maximum initial depression) could predict occurrence of MACE and in-hospital mortality, from a clinical point of view, it might be easier to detect the lead with maximum depression in initial ECG and calculate the resolution of depression after PPCI. Thus, the clinician should readily be capable of determining whether their patient has a resolution of more or less than 50%. This valuable prognostic information can easily determine those patients who require a more thorough treatment and follow-up plan.
Limitations
We believe that an important limitation of this study was the fact that follow-up period for assessment of patient survival was not appropriately long and in order to get more significant results regarding the association of ST segment depression resolution and long term mortality, it would be reasonable to design a prospective cohort study with a larger sample size.
Conclusion
The results of this study show that ST segment depression resolution of less than 50% has a statistically significant correlation with incidence of in-hospital acute heart failure and major adverse cardiac events. Also, this variable has a good predictive power with relatively high specificity and sensitivity for mortality in a level of 50% for both calculation forms of either resolution of sum of ST segment depressions or resolution of ST depression in a single lead with maximum primary depression.
Acknowledgments
The authors would like to thank all physicians at Shahid Madani Hospital responsible for treatment of ST elevation MI patients enrolled in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Available from: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
2. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Glob Heart. 2012;7(4):275–295. doi:10.1016/j.gheart.2012.08.001
3. Schroder R, Dissmann R, Bruggemann T, et al. Extent of early ST segment elevation resolution: a simple but strong predictor of outcome in patients with acute myocardial infarction. J Am Coll Cardiol. 1994;24(2):384–391. doi:10.1016/0735-1097(94)90292-5
4. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction–executive summary. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004;44(3):671–719. doi:10.1016/j.jacc.2004.07.002
5. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. doi:10.1093/eurheartj/ehx393
6. Tjandrawidjaja MC, Fu Y, Westerhout CM, et al. Resolution of ST-segment depression: a new prognostic marker in ST-segment elevation myocardial infarction. Eur Heart J. 2010;31(5):573–581. doi:10.1093/eurheartj/ehp494
7. Wong CK, de la Barra SL, Herbison P. Does ST resolution achieved via different reperfusion strategies (fibrinolysis vs percutaneous coronary intervention) have different prognostic meaning in ST-elevation myocardial infarction? A systematic review. Am Heart J. 2010;160(5):
8. Kozuch M, Dobrzycki S, Nowak K, et al. Lack of ST-segment depression normalization after PCI is a predictor of 5-year mortality in patients with ST-elevation myocardial infarction. Circ J. 2007;71(12):1851–1856. doi:10.1253/circj.71.1851
9. Shah A, Wagner GS, Califf RM, et al. Comparative prognostic significance of simultaneous versus independent resolution of ST segment depression relative to ST segment elevation during acute myocardial infarction. J Am Coll Cardiol. 1997;30(6):1478–1483. doi:10.1016/S0735-1097(97)00331-8
10. Wong CK, Gao W, White HD. Resolution of ST depression after fibrinolysis can be more important than resolution of ST elevation for many patients with inferior STEMIs. Int J Cardiol. 2015;182:232–234. doi:10.1016/j.ijcard.2014.12.117
11. Camara EJ, Chandra N, Ouyang P, Gottlieb SH, Shapiro EP. Reciprocal ST change in acute myocardial infarction: assessment by electrocardiography and echocardiography. J Am Coll Cardiol. 1983;2(2):251–257. doi:10.1016/S0735-1097(83)80160-0
12. Haraphongse M, Tanomsup S, Jugdutt BI. Inferior ST segment depression during acute anterior myocardial infarction: clinical and angiographic correlations. J Am Coll Cardiol. 1984;4(3):467–476. doi:10.1016/S0735-1097(84)80089-3
13. Mukharji J, Murray S, Lewis SE, et al. Is anterior ST depression with acute transmural inferior infarction due to posterior infarction? A vectorcardiographic and scintigraphic study. J Am Coll Cardiol. 1984;4(1):28–34. doi:10.1016/S0735-1097(84)80314-9
14. Tzivoni D, Chenzbraun A, Keren A, et al. Reciprocal electrocardiographic changes in acute myocardial infarction. Am J Cardiol. 1985;56(1):23–26. doi:10.1016/0002-9149(85)90559-4
15. Ruddy TD, Yasuda T, Gold HK, et al. Anterior ST segment depression in acute inferior myocardial infarction as a marker of greater inferior, apical, and posterolateral damage. Am Heart J. 1986;112(6):1210–1216. doi:10.1016/0002-8703(86)90350-9
16. Hayiroglu MI, Keskin M, Uzun AO, Turkkan C, Tekkesin AI, Kozan O. What is the predictive value of ST segment depression in inferior leads in first acute anterior myocardial infarction? J Electrocardiol. 2018;51(3):524–530. doi:10.1016/j.jelectrocard.2017.12.006
17. De Luca G, Maas AC, van ‘T Hof AW, et al. Impact of ST-segment depression resolution on mortality after successful mechanical reperfusion in patients with ST-segment elevation acute myocardial infarction. Am J Cardiol. 2005;95(2):234–236. doi:10.1016/j.amjcard.2004.09.008
18. Reinstadler SJ, Baum A, Rommel KP, et al. ST-segment depression resolution predicts infarct size and reperfusion injury in ST-elevation myocardial infarction. Heart. 2015;101(22):1819–1825. doi:10.1136/heartjnl-2015-307876
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





