Back to Journals » Open Access Emergency Medicine » Volume 13
Predictors of Medication-Related Emergency Department Admissions Among Patients with Cardiovascular Diseases at Mbarara Regional Referral Hospital, South-Western Uganda
Authors Kiptoo J , Yadesa TM , Muzoora C, Namugambe JS , Tamukong R
Received 4 March 2021
Accepted for publication 11 June 2021
Published 29 June 2021 Volume 2021:13 Pages 279—290
DOI https://doi.org/10.2147/OAEM.S309508
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Joshua Kiptoo,1 Tadele Mekuriya Yadesa,1,2 Conrad Muzoora,3 Juliet Sanyu Namugambe,1,2 Robert Tamukong1,2
1Department of Pharmacy, Mbarara University of Science and Technology, Mbarara, Uganda; 2World Bank, ACE II, Pharmacy Biotechnology and Traditional Medicine Center, Mbarara University of Science and Technology, Mbarara, Uganda; 3Department of Internal Medicine, Mbarara University of Science and Technology, Mbarara, Uganda
Correspondence: Joshua Kiptoo Tel +256 778083875
Email [email protected]
Background: Medication-related emergency department admissions impose a huge and unnecessary burden on the healthcare system. We sought to determine the prevalence and predictors of medication-related emergency department admissions, among patients with cardiovascular diseases at Mbarara Regional Referral Hospital, Uganda.
Methods: Institutional research ethics approval was secured to conduct a cross-sectional study at the Mbarara Regional Referral Hospital emergency department, between February and September, 2020. All eligible and consenting patients were enrolled in a consecutive manner after a preliminary diagnosis was made by the attending physician. Structured questionnaire interview and comprehensive medication history reviews were used to identify medication therapy problems, in collaboration with a resident physician present on duty. We used sequential categorization for medication therapy problem(s). Descriptive and logistic regression analyses were used to determine prevalence and predictors of medication-related emergency department admissions.
Results: Out of the 128 patients interviewed, 105 (82%) patient admissions were associated with a medication therapy problem: ineffectiveness of drug therapy (53.3%, 56), medication non-adherence (42.9%, 45), and adverse drug reactions (3.8%, 4). Out of a total of 90 incidences of medication non-adherence, 34.4% (31/90) were due to lack of understanding of patient medication regimen, and 27.8% (25/90) due to unaffordable cost of medicines. Female gender (AOR = 4.31 [1.43, 13.03 at 95% CI]; P-value = 0.010]) and a history of tobacco use (AOR = 9.58 [1.14, 80.28 at 95% CI]; P-value = 0.037) were statistically significant predictors of medication-related emergency department admissions in adjusted analysis.
Conclusion: Four in five emergency department admissions were associated with medication-related causes, majorly due to ineffectiveness of drug therapy. Knowledge gap on patient medication regimens was the most prevalent cause for medication non-adherence. Female gender and previous or current tobacco use was an independent risk factor for medication-related admissions.
Keywords: adverse drug reaction, ineffective drug therapy, non-adherence, emergency department admission, cardiovascular, Uganda
Introduction
There is a huge public health concern regarding the increasing medication-related emergency department admissions due to failure to manage medication therapy problems (MTPs) among patients with cardiovascular disease in developing countries.1,2 MTPs include any undesirable event(s) experienced by a patient, which involves or is suspected to involve drug therapy, thereby interfering with achieving the desired goals of therapy and requires professional judgment to resolve.3 Optimization of out-patient follow-up management of cardiovascular disease and/or associated complications necessitates accurate and comprehensive diagnosis, treatment, and prevention of medication therapy problems.4 Medication-related ED (MRED) admissions associated with MTPs have been highly associated with patients on multiple cardiovascular medication,5 especially, antihypertensive and cardiac glycoside medications.6–8 These admissions impose an unnecessary extra expenditure on the healthcare system9 due to prescription cascades, laboratory costs,10 morbidity and mortality.11
Among the diverse categories of MTPs, medication non-adherence has been identified as the single most prevalent and costly cause of hospital emergency admission, resulting from drug treatment failure, sub-optimal disease management, and a compounded risk for disease complications.12 Similarly, ADR-associated ED admissions have previously been reported at 10.3% in Ethiopia,13 with the number of medications, comorbid states, and drug therapy changes within the preceding 3 months as strong predictors of ADR-related ED admissions.14 Actual or potential drug therapy ineffectiveness has been identified as a major cause of hospital admission,15,16 contributing up to 58% (76/135) of all hospital admissions in a local Ethiopian hospital.17 However, the burden in Uganda is largely unknown. By and large, there is limited published literature on MRED admissions due to ADR (adverse drug reaction), drug therapy ineffectiveness, or indication in developing countries, possibly due to the underdeveloped surveillance system (ADRs) and the limited human resource capacity to assess prescribed drug therapy effectiveness and indication in out-patient care.
For clinical pharmacists to effectively identify, assess, and quantify the burden of medication-related emergency department admissions among cardiovascular disease patients, there is need for a universal tool or definition to foster a global understanding of the subject. However, this is lacking at the moment, and several MRED admission categorization methods have been developed to that effect.18,19 However, sequential identification and categorization of medication-related causes of admission, involving issues with drug therapy indication, effectiveness, safety (ADR or dose too high), and adherence in that prioritized order, remains the most trusted system of classification in the literature.20,21 An MTP of non-adherence is only considered to have potentially resulted in ED admission (MRED) if the medication(s) in question are, firstly, indicated, effective, and safe for the patient. Similarly, an ADR-related admission is only considered if the prescribed medication(s) is indicated and effective for the treated disease condition. Several studies in Africa and related settings have initially narrowed the definition of MRED admissions, as resulting from individual MTPs; like ADRs,13,22 medication non-adherence,23 and/or a combination of only two or more varying MTPs,24 thus missing out on vital information on assessing clinically relevant medication use outcomes among CVD patients. Sequential categorization of MTPs as suggested by Cipolle et al tries to address the challenge of variations in definition and outcomes of research on “Medication or drug-related hospital/ED admissions/visits”, as evident in previously published literature. In our study, therefore, we operationalized medication-related ED (MRED) admissions, as causes of admissions related to either medication effectiveness, adherence, or adverse drug reactions for medications indicated. Medication-related problems associated with drugs not indicated were excluded.
Due to a dearth of research on MRED admissions in sub-Saharan Africa, this study sought to determine the prevalence and predictors of MRED admissions among patients with cardiovascular disease at MRRH, western Uganda. The study also aimed at identifying the different reasons for non-adherence to medication therapy.
Methods
Study Setting
The study was conducted at the Mbarara Regional Referral Hospital (MRRH) emergency department, Mbarara City, Uganda. MRRH is a 350-bed tertiary hospital and is considered the largest referral center in south-western Uganda. The hospital serves up to four million people from the neighboring districts and countries, like Burundi, DRC, and Tanzania. The hospital ED is a ten-bed facility that is majorly manned by residents under the guidance of senior hospital staff, and comprises both the surgical and medical units. The department runs 24/7 with an estimated annual admission of 4000 patients, both male and female patients ≥18 years of age.
Study Population
All patients admitted at the MRRH ED with a primary diagnosis of cardiovascular disease, between February and September, 2020.
Eligibility Criteria
Inclusion criteria: primary cardiovascular disease diagnosis, age ≥ 18 years, consenting to participate in the study. Exclusion criteria: mentally unstable or unconscious patients, infectious disease exacerbation(s), patients with less than 3 months of out-patient follow-up treatment of cardiovascular disease, incomplete medical records.
Study Design
We conducted a cross-sectional study, between February and September, 2020.
Sample Size Calculation
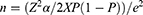
We used a single proportion formula to determine the sample size,25 as adopted from previous studies:
Using an estimate of 165 (N) patients admitted with cardiovascular disease at the MRRH ED in the previous 3 months, 5% margin of error (e), an estimated 50% prevalence (p) of MRED admission as no similar study has been done in Uganda or similar settings, and a 5% level of significance, we calculated a sample size (No) of 116 participants. By adding 10% for incomplete data or non-response, we obtained a sample size of 128 participants.
Sampling Technique
A consecutive sampling technique was employed involving every consecutive patient who fulfilled the eligibility criteria and consented to participate in the study.
Data Collection Procedure
Study participants were interviewed between 08:00 AM and 5:00 PM (EAT), Monday to Friday. Participants were subjected to a structured questionnaire and checklist interview as soon as the patient or attendant felt convenient and preliminary diagnosis was made by the attending physician. Participant socio-demographic data, history of presenting illness, past history, number of hospital admissions in the past one year, history of allergies and medication history (including over-the counter (OTC) and complementary and alternative medicines) was obtained by pharmacists.
A participant and prescription-oriented medication therapy review was done to identify out-patient MTPs, including medication non-adherence, ineffective drug therapy, and ADRs at the point of admission.
To assess the effectiveness of drug therapy, standard references (Uganda Clinical Guidelines-2016 and UpToDate) and an aggregated system of classification were used to assess appropriateness of prescribed drug(s), appropriateness of dosage form and regimen, issues of drug quality/expiry, and refractoriness of disease to drug therapy, in a prioritized manner.26
Using the Naranjo ADR causality algorithm, participants with definite and probable ADR causality scores (≥5) were considered ADR-related ED admissions.27
We used the Hill–Bone medication adherence scale to determine any non-adherence that had occurred while the patients were at home.28 The identified non-adherence was categorized using Cipolle et al's classification of causes of drug therapy problems.20
To identify individual MTPs associated with CVD exacerbation, leading to ED admission (MRED admissions), MTPs were sequentially categorized in the precedence of drug therapy indication, ineffectiveness of drug therapy, ADR, and medication non-adherence.20,21 Non adherence was only considered if drug therapy was indicated, effective, and no concerns of ADRs; similarly, ineffectiveness of drug therapy was only qualified if prescribed drug therapy is indicated.
The above information was verified by a resident physician, who independently interviewed participants and conducted physical assessments whenever requested by the principle investigator.
Patients’ enrolment was stopped once the estimated sample size was interviewed.
Data Analysis and Interpretation
Respective participant data were entered and analyzed using statistical software (SPSS version 21, SPSS Inc., Chicago, IL, USA). Prevalence of MRED admissions was determined by dividing the number of MRED admissions by the total sample size. Descriptive analysis was done to determine the frequencies and percentages of the participants, disease, and drug-related factors. The relationship between the dependent (MRED admission) and independent variables were determined using odds ratios with a 95% confidence interval. Univariate and multivariate binary logistic regression analysis was done to determine predictors of MRED admissions. All variables with P-value > 0.25 during univariate analysis were excluded from further analysis. P-value <0.05 was considered significant for all analyses.
Ethical Consideration
This study was conducted in accordance with the Declaration of Helsinki.29 This study was approved by the faculty research ethics committee (FREC) and the Mbarara University of Science & Technology research ethics committee (MUST-REC).
Hospital administration of Mbarara Regional Referral Hospital (MRRH) granted permission for the study to be conducted at the hospital ED.
Informed written consent was obtained from individual patients prior to enrollment into the study.
Participant data were handled in a confidential manner throughout and after the study.
The data collectors adhered to the Ugandan Ministry of Health and MRRH protocols on COVID-19 during the study. This included: donning face masks at all times, sanitizing before and after handling individual patient material(s), maintaining appropriate social distancing during interview, quarantining all questionnaires in a safe and isolated cabin for a duration of 3 days prior to further processing, and regular COVID-19 testing of the data collectors.
Results
General Characteristics of the Participants
Out of the 128 study participants interviewed, 77 (60.2%) were females, 76 (59.4%) were <65 years of age (mean, 59.19; SD ±17.3 years), 84 (65.6%) were unemployed, 65 (50.8%) were uneducated, 89 (69.5%) were married, 85 (66.4%) had a history of present or current alcohol intake, 31 (24.2%) had a history of tobacco use, 69 (53.9%) lived 10 km or more from the nearby hospital, and 75 (58.6%) had been admitted ≤2 times in the past one year (Table 1).
 |
Table 1 Demographic Characteristics of Patients with Cardiovascular Diseases Admitted to the MRRH ED Between February and September, 2020 |
Drug and Disease Characteristics of the Participants
The majority (75, 58.6%) of the participants were admitted 2 or less times in the last one year, 10 (7.8%) had experienced drug allergies, 66 (51.6%) have had new prescribed medications in the last 3 months, 96 (75%) had at least three medications, 62 (49.6%) had a comorbid condition, and 102 (79.7%) had a primary diagnosis of a vascular disease, particularly hypertension (93.1%) (Table 2).
 |
Table 2 Prevalence of Drug and Disease-Related Factors of Patients with Cardiovascular Disease, Admitted at MRRH ED Between February and September, 2020 |
Primary Outcome: Prevalence of Medication-Related Emergency Department (MRED) Admissions
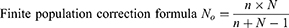
All MTPs due to non-cardiovascular medicines were neither considered as MTPs nor MRED admissions (in case of patient admission). MRED admissions were determined following a sequential identification of MTPs that could have potentially resulted into admission. During the 3-month study period, 82% (105/128) of patients enrolled were considered MRED admissions (Figure 1).
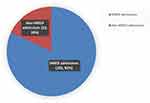 |
Figure 1 Prevalence of MRED admissions among patients with cardiovascular disease, admitted at MRRH ED between February and September, 2020. |
The MTPs associated with MRED admissions, include: ineffectiveness of drug therapy (53.3%, 56), non-adherence (42.9%, 45), and ADRs (3.8%, 4). An overall MTP incidence of 1.3 (161/128) was determined, with only 65.2% (105/161) of all identified MTPs potentially associated with patient admissions during the study period. Although some patients had more than one MTP, only the proceeding MTP in the sequential order of MTP categorization was considered as the potential cause of admission (Table 3).
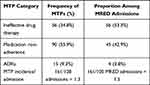 |
Table 3 Medication Therapy Problems Among MRED Admissions of Patients with Cardiovascular Disease, Admitted at MRRH ED Between February and September, 2020 |
Secondary Outcome: Leading Cause of Medication Non-Adherence
Overall, 90 (70.3%) study participants were not adhering to their prescribed medications while at home. Reasons for non-adherence included: inadequate understanding of medication use instructions (31, 34.4%), unaffordable cost of medicines (25, 27.8%), varying physician diagnosis (9, 10%), forgetting to take medicines (8, 8.9%), unavailability of prescribed medicines (8, 8.9%), and unwillingness to take medicines (2, 2.2%) (Figure 2).
 |
Figure 2 Causes of medication non-adherence among patients with cardiovascular disease, admitted at MRRH ED between February and September, 2020. |
Tertiary Outcome: Predictors of MRED Admissions
Univariate Analysis
Among the factors analyzed for possible association to MRED admissions, female gender (COR = 4.6 [1.7, 12.1 at 95% CI]; P-value = 0.002), a single marital status (COR = 0.09 [0.01, 0.93 at 95% CI]; P-value = 0.04), ≥3 medications (COR = 2.29 [0.88, 5.97 at 95% CI]; P-value 0.09), history of tobacco smoking (COR = 8.8 [1.13, 68.23 at 95% CI]; P-value = 0.04), and history of new drug prescriptions within the last 3 months (COR = 1.85 [0.74, 4.64 at 95% CI]; P-value = 0.19) qualified for multivariate analysis (Table 4).
 |
Table 4 Univariate Analysis of Patient, Disease and Drug-Related Factors Among Patients with Cardiovascular Disease, Admitted at the MRRH ED Between February and September, 2020 |
Multivariate Analysis
Female gender (AOR = 4.31 [1.43, 13.03 at 95% CI]; P-value = 0.010]) and a history of tobacco use (AOR = 9.58 [1.14, 80.28 at 95% CI]; P–value = 0.037) were determined to be significant predictors (P-value < 0.05) of MRED admissions among patients admitted with cardiovascular conditions. (Table 5). Female participants were about 4.3 times more likely to incur MRED compared to males whereas participants with history of tobacco use were about 9.5 times more likely to experience MRED admissions compared to non-users.
Discussion
Many pharmaco-epidemiological studies on medication-related hospital/ED admissions have been done under varied definitions in the majority of developed countries. However, as the burden of cardiovascular disease continuously increase in low and middle-income countries, there is a growing concern and call for further research to improve drug safety and effectiveness, especially among patients using cardiovascular drugs.30,31 Outcomes from our study reveal a serious public health threat of medication-related patient admissions in developing countries like Uganda. The findings suggest that four in five (82%) admissions among patients with cardiovascular disease were potentially associated with medication therapy problems. 53.3% (56/105) of all MRED admissions were directly related to ineffectiveness of prescribed drug(s), whereas 42.9% (45/105) and 3.8% (4/105) were potentially associated with non-adherence and ADRs respectively. Although our study finding is justified by a literature review associating medical chart reviews and studies conducted in African settings with a higher medication-related causes of admission,32 our prevalence still is significantly higher compared to previously published literature, reporting MRED prevalence of 1.3% to 64%.33–37 Also, the fact that clinical pharmacy residents were the primary data collectors, and the evidence of higher medication-related admissions among patients on multiple cardiovascular medications,5 tends to explain the high MRED prevalence in our study. Unlike in our study, several published study characteristics have consistently been associated with lower MRED prevalence, including settings with a higher socio-economic status23,37–39, meta-analyses and systematic review study outcomes,22,36,40, specific participant demographic characteristics (pediatrics, urban or semi-urban dwellers),36,41 and studies adopting only one or two MTPs to define the outcome variable.13,24,32,41
Ineffectiveness of therapy is one of the most common causes of medication-related ED admissions, due to failure to achieve clinical targets/responses by patients.15,16 Our study showed that more than half (53.3%) of all MRED admissions were directly associated with ineffectiveness of drug therapy. Our findings do not differ much from previous findings in a similar setting in Ethiopia, reporting a 58% (76/135) prevalence of ineffective drug therapy among hospital admissions.17 Two in every five MRED admissions were associated with non-adherence to prescribed medications in our study population. Although there exist socio-economic differences among the participant populations and study settings, the individual contribution of non-adherence to overall MRED admissions in our study, is comparable to similar studies, reporting between 14.5% and 47.34% MRED admission prevalence due to non-adherence.23,37,41,42 A study conducted in Ethiopia, like many other similar studies, report up to 69.7% non-adherence-associated MRED admissions.43 However, the majority of these studies consider only one MTP as a possible cause of admission, and neither utilized the model by Cipolle et al in assessing medication-related hospitalizations.20 An approximate 1 out of every 30 MRED (3.8%) admissions potentially resulted from ADRs. This finding does not significantly differ from previously published studies and literature reviews among patients using cardiovascular medicines, with individual ADR contributions as low as 3.3%.44–46
Prevalence of MRED admissions across the different participant strata was significantly higher among participants of the female gender (54.7%), those with a positive history of new drug prescribed within past 3 months (44.5%), uneducated (40.6%), married (54.7%), unemployed/students (54.7%), diagnosis of primary disease within the past 2 years (48.4%), and age < 65 years (46.9%). Previous studies conducted in similar settings associated poor socio-economic status and literacy levels with high MRED prevalence.47,48 However, although old age (>65 years) is a known predictor of MRED admissions,49 our results state otherwise. This can be explained by the small sample size and the larger younger population in our setting (Table 1). According to categorized outcomes of all participant diagnoses on admission (Table 1), 79% of all MRED admissions had vascular disease diagnosis, of which 7 in every 10 (74%) ED admissions presented with uncontrolled hypertension (with or without complications) and considered MRED admissions. Previous studies implicate hypertensive patients as more likely to visit the ED due to non-adherence (AOR = 11.06, 95% CI: 3.99–30.61), thus MRED admission.8,41 The low levels of medication adherence among hypertensive patients has been prior reported as resulting from patients' knowledge gaps on their medicines and disease, poor health-seeking behaviors among the general population, mistrust of the healthcare system, inaccessibility to medicines in public hospitals, and poor continuum of care among patients with cardiovascular diseases in Uganda.50–53
Previous studies have established an association between medication non-adherence with a complicated cardiovascular disease course (AOR = 2.062, 95% CI: 1.030–4.129), ED admission (OR = 7.5 [95% CI: 5.3, 11.0)23 and an all cause-mortality (RR 0.71, 95% CI: 0.64–0.78).54–56 Our study identified an overall 70.3% (90/128) prevalence of non-adherence. This implies that 7 out of every 10 cardiovascular disease ED admissions were non-adherent to their prescribed medications. Our finding is consistent with previous reports of 63.35% (95% CI: 38.78–87.91) prevalence of medication non-adherence, and as the most likely cause of MRED admissions among patients with cardiovascular disease (AOR = 11.06, 95% CI: 3.99–30.61).41,57,58 Likewise, previous studies in Ethiopia, DRC, and Uganda report that up to 73.2% patients are non-adherent to their medications due to inadequate understanding of medication use instructions (AOR = 7.67, 95% CI = 2.48–23.73, P-value < 0.001) (OR = 1.7; 95% CI 1.1–2.7).59–61 The leading cause of medication non-adherence was the inadequate understanding of medication use instructions among patients (31, 34.4%). This is anticipated as the majority (109, 85.5%) of our participants were uneducated, coupled with the under-resourced health care associated with limited essential medicines in the hospitals.48,52,62 This demonstrates an urgent need to utilize pharmacist-led comprehensive patient counseling, and strengthen transition-of-care systems, as reported to reduce MRED admissions to as low as 3% (P-value = 0.002) in previous similar studies.49,63
Our predictive analysis results show that the female gender (AOR = 4.31 [1.43, 13.03 at 95% CI]; P-value = 0.010) and present or past tobacco users (AOR = 9.58 [1.14, 80.28 at 95% CI]; P–value = 0.037), were at least 4 and 9 times more likely to be admitted to ED due to medication therapy problems respectively. These are consistent with previously published studies, identifying female gender8,64 and tobacco use or smoking65 as predictors of MRED admissions. Although 66.7% (70/105) of all MRED admissions were females in our study, previous studies have suggested otherwise, with an expected lower CVD risk among females, owing to the potential cardio-protective role of estrogen (reduction of oxidative stress levels),66 higher anti-oxidant potential,67 and the good health seeking behaviors.68 However, the female gender has also been associated with the increasingly high non-traditional CVD risks (eg depression, gestational diabetes, acute and chronic emotional stress, menopause, hypertensive disorders of pregnancy etc.),69 and the increasing psychosocial and economic pressures (financial dependence, high family responsibilities, discriminative cultural norms),70 which is most likely in our community setting. Smoking is one of the leading modifiable risk factors of CVD, and has been associated with development and progression of CVD through different pathophysiological processes of endothelial dysfunction, atherogenesis and atherosclerosis, hemodynamic effects, inflammation, hypercoagulable state, and dyslipidemia.71 This could primarily lead to disease refractoriness to drug therapy, or influence the pharmacokinetics of certain CVD drugs used by patients in the out-patient settings, thus leading to medication-related ED admissions.
Because of the short study duration and, thus, smaller study population, a random sampling technique was not used. The potential recall bias and incomplete information were the other important limitations of the study. There is also a possibility that some medication, disease, or patient-related factors failed to qualify for multivariate analysis due to the smaller number of participants, and the limitations/restrictions owing to interruptions by the SARS-CoV-2 pandemic, on patient enrollment. The poor documentation habits in our study setting would have further compromised on the quality of data and outcomes.
Conclusion
Ineffectiveness of drug therapy is the largest sole cause of MRED admissions among patients admitted with cardiovascular diseases. Patients understanding gap of the disease and treatment constitute the largest reason of medication non-adherence. Participants of the female gender, and those with a history of tobacco use were more likely to be admitted due to medication-related causes.
Because most admissions were related to the medication therapy problems experienced at home, there is clear need to focus on optimization of chronic care in Uganda and related settings.
Ethical Approval
This study was approval by the Mbarara University of Science and Technology Research and Ethics Committee (MUST-REC) with a letter with Ref. No. MUREC1/7.
Acknowledgments
The authors are sincerely grateful to the patients and caregivers that offered to participate in this study. And most importantly, the authors are thankful for the support and approval granted by the administration of Mbarara Regional Referral Hospital (MRRH) for allowing us to conduct the study. We are sincerely grateful for all the support offered by Dr. Kushemererwa Oliver, a clinical pharmacy resident at Mbarara University of Science & Technology.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The authors received no specific funding for this work.
Disclosure
The authors declare no conflicts of interest.
References
1. Niriayo YL, Kumela K, Kassa TD, Angamo MT, Frey R. Drug therapy problems and contributing factors in the management of heart failure patients in Jimma University Specialized Hospital, Southwest Ethiopia. PLoS One. 2018;13(10):e0206120. doi:10.1371/journal.pone.0206120
2. Wang C-L, Ding S-T, Hsieh M-J, et al. Factors associated with emergency department visit within 30 days after discharge. BMC Health Serv Res. 2016;16(1):190.
3. Cipolle LMSPCMRJ. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management Services. Mc-Graw Hill; 2020.
4. Niquille A, Bugnon O. Relationship between drug-related problems and health outcomes: a cross-sectional study among cardiovascular patients. Pharmacy World Sci. 2010;32(4):512–519.
5. Sikdar KC, Alaghehbandan R, Macdonald D, et al. Adverse Drug Events in Adult Patients Leading to Emergency Department Visits. Annals Pharmacother. 2010;44(4):641–649.
6. Green L, et al. Combination Pharmacotherapy for Cardiovascular Disease. Ann Intern Med. 2005;143(8):593–599.
7. Public Health Research Working Group. Combination pharmacotherapy for cardiovascular disease. Ann Intern Med. 2005;143(8):593.
8. Malhotra S, Karan RS, Pandhi P, Jain S. Drug related medical emergencies in the elderly: role of adverse drug reactions and non-compliance. Postgrad Med J. 2001;77(913):703–707.
9. Cutler RL, Torres-Robles A, Wiecek E, et al. Pharmacist-led medication non-adherence intervention: reducing the economic burden placed on the Australian health care system. Patient Prefer Adherence. 2019;13:853.
10. Sultana J, Cutroneo P, Trifirò G. Clinical and economic burden of adverse drug reactions. J Pharmacol Pharmacother. 2013;4(Suppl1):S73.
11. Katusiime B, Semakula D, Lubinga SJ. Adverse drug reaction reporting among health care workers at Mulago National Referral and Teaching hospital in Uganda. Afr Health Sci. 2015;15(4):1308–1317.
12. Zed PJ. Drug-related visits to the emergency department. J Pharm Pract. 2005;18(5):329–335.
13. Angamo MT, Curtain CM, Chalmers L, Yilma D, Bereznicki L. Predictors of adverse drug reaction-related hospitalisation in Southwest Ethiopia: a prospective cross-sectional study. PLoS One. 2017;12(10):e0186631.
14. Nair NP, Chalmers L, Connolly M, et al. Prediction of hospitalization due to adverse drug reactions in elderly community-dwelling patients (The PADR-EC Score). PLoS One. 2016;11(10):e0165757.
15. Westberg SM, Derr SK, Weinhandl ED, et al. Drug therapy problems identified by pharmacists through comprehensive medication management following hospital discharge. J Pharm Technol. 2017;33(3):96–107.
16. Al Hamid A, Aslanpour Z, Aljadhey H, Ghaleb M. Hospitalisation resulting from medicine-related problems in adult patients with cardiovascular diseases and diabetes in the United Kingdom and Saudi Arabia. Int J Environ Res Public Health. 2016;13(5):479.
17. Gelchu T, Abdela J. Drug therapy problems among patients with cardiovascular disease admitted to the medical ward and had a follow-up at the ambulatory clinic of Hiwot Fana Specialized University Hospital: the case of a tertiary hospital in eastern Ethiopia. SAGE Open Med. 2019;7:2050312119860401.
18. Leendertse AJ, Egberts AC, Stoker LJ. van den Bemt PM. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med. 2008;168(17):1890–1896.
19. Bonnet‐Zamponi D. d’Arailh L, Konrat C, et al. Drug-related readmissions to medical units of older adults discharged from acute geriatric units: results of the optimization of medication in age D multicenter randomized controlled trial. J Am Geriatrics Soc. 2013;61(1):113–121.
20. Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management. McGraw Hill Professional; 2012.
21. Pellegrin KL, Lee E, Uyeno R, Ayson C, Goo R. Potentially preventable medication-related hospitalizations: a clinical pharmacist approach to assessment, categorization, and quality improvement. J Am Pharmacists Assoc. 2017;57(6):711–716.
22. Oscanoa T, Lizaraso F, Carvajal A. Hospital admissions due to adverse drug reactions in the elderly. A meta-analysis. Eur J Clin Pharmacol. 2017;73(6):759–770.
23. Jatau I, Aung M, Tuan Kamauzaman TH, Ab Rahman AF, Jatau Abubakar I. Emergency department visit due to medication non-adherence at a teaching hospital in Malaysia 2016. 23–28 p.
24. Yee JL, Hasson NK, Schreiber DH. Drug-related emergency department visits in an elderly veteran population. Annals Pharmacother. 2005;39(12):1990–1995.
25. Naing L, Winn T, Rusli B. Practical issues in calculating the sample size for prevalence studies. Arch Orofacial Sci. 2006;1:9–14.
26. Basger BJ, Moles RJ, Chen TF. Development of an aggregated system for classifying causes of drug-related problems. Annals Pharmacother. 2015;49(4):405–418.
27. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–245.
28. Culig P, Leppée M. From Morisky to Hill-Bone; Self-reports scales for measuring adherence to medication. Coll Antropol. 2014;38(1):55–62.
29. WMA DECLARATION OF HELSINKI. Ethical principles for medical research involving human subjects [Online]. [press release]. 2018.
30. Hohl CM, Zed PJ, Brubacher JR, Abu-Laban RB, Loewen PS, Purssell RA. Do emergency physicians attribute drug-related emergency department visits to medication-related problems? Ann Emerg Med. 2010;55(6):493–502.e4.
31. Al Hamid A, Ghaleb M, Aljadhey H, Aslanpour Z. A systematic review of hospitalization resulting from medicine-related problems in adult patients. Br J Clin Pharmacol. 2014;78(2):202–217.
32. Leendertse AJ, Visser D, Egberts AC. van den Bemt PM. The relationship between study characteristics and the prevalence of medication-related hospitalizations. Drug Safety. 2010;33(3):233–244.
33. Ayalew MB, Tegegn HG, Abdela OA. Drug Related Hospital Admissions; A Systematic Review of the Recent Literatures. Bulletin of Emergency & Trauma. 2019;7(4):339.
34. El Morabet N, Uitvlugt EB, van den Bemt BJF, van den Bemt PMLA, Janssen MJA, Karapinar-çarkit F. Prevalence and Preventability of Drug-Related Hospital Readmissions: a Systematic Review. J Am Geriatr Soc. 2018;66(3):602–608.
35. Nickel CH, Ruedinger JM, Messmer AS, et al. Drug-related emergency department visits by elderly patients presenting with non-specific complaints. Scand J Trauma Resusc Emerg Med. 2013;21(1):15.
36. Zed PJ, Haughn C, Black KJ, et al. Medication-related emergency department visits and hospital admissions in pediatric patients: a qualitative systematic review. J Pediatr. 2013;163(2):477–483.
37. Cooper JB, Jeter E, Sessoms CJ. Rates and Types of Medication-Related Problems in Patients Rehospitalized Within 30 Days of Discharge From a Community Hospital. J Pharm Technol. 2020;36(2):47–53.
38. Zed PJ, Abu-Laban RB, Balen RM, et al. Incidence, severity and preventability of medication-related visits to the emergency department: a prospective study. Cmaj. 2008;178(12):1563–1569.
39. Ajdukovic M, Crook M, Angley C, et al. Pharmacist elicited medication histories in the Emergency Department: identifying patient groups at risk of medication misadventure. Pharm Pract. 2007;5(4):162–168.
40. Mongkhon P, Ashcroft DM, Scholfield CN, Kongkaew C. Hospital admissions associated with medication non-adherence: a systematic review of prospective observational studies. BMJ Qual Saf. 2018;27(11):902–914.
41. Heaton PC, Tundia NL, Luder HR. US emergency departments visits resulting from poor medication adherence: 2005–07. J Am Pharmacists Assoc. 2013;53(5):513–519.
42. Dhar L, Earnest J, Ali M. A systematic review of factors influencing medication adherence to hypertension treatment in developing countries. Open J Epidemiol. 2017;7(03):211–250.
43. Seid E, Engidawork E, Alebachew M, Mekonnen D, Berha AB. Evaluation of drug therapy problems, medication adherence and treatment satisfaction among heart failure patients on follow-up at a tertiary care hospital in Ethiopia. PLoS One. 2020;15(8):e0237781.
44. Kongkaew C, Hann M, Mandal J, et al. Risk factors for hospital admissions associated with adverse drug events. Pharmacotherapy. 2013;33(8):827–837.
45. Chan SL, Ang X, Sani LL, et al. Prevalence and characteristics of adverse drug reactions at admission to hospital: a prospective observational study. Br J Clin Pharmacol. 2016;82(6):1636–1646.
46. Pedrós C, Formiga F, Corbella X, Arnau JM. Adverse drug reactions leading to urgent hospital admission in an elderly population: prevalence and main features. Eur J Clin Pharmacol. 2016;72(2):219–226.
47. Thwe AIJMM, Ab ATHTK, Ab F FACTORS ASSOCIATED WITH DRUG-RELATED EMERGENCY DEPARTMENT VISIT: a SYSTEMATIC REVIEW.
48. Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. The Lancet. 2011;378(9798):1231–1243.
49. Linkens A, Milosevic V, van der Kuy P, Damen-Hendriks V, Mestres Gonzalvo C, Hurkens K. Medication-related hospital admissions and readmissions in older patients: an overview of literature. Int J Clin Pharm. 2020;1–9.
50. Rogers HE, Akiteng AR, Mutungi G, Ettinger AS, Schwartz JI. Capacity of Ugandan public sector health facilities to prevent and control non-communicable diseases: an assessment based upon WHO-PEN standards. BMC Health Serv Res. 2018;18(1):606.
51. Chang H, Hawley NL, Kalyesubula R, et al. Challenges to hypertension and diabetes management in rural Uganda: a qualitative study with patients, village health team members, and health care professionals. Int J Equity Health. 2019;18(1):38.
52. Armstrong-Hough M, Kishore SP, Byakika S, Mutungi G, Nunez-Smith M, Schwartz JI. Disparities in availability of essential medicines to treat non-communicable diseases in Uganda: a Poisson analysis using the Service Availability and Readiness Assessment. PLoS One. 2018;13(2):e0192332.
53. Stephens JH, Alizadeh F, Bamwine JB, et al. Managing hypertension in rural Uganda: realities and strategies 10 years of experience at a district hospital chronic disease clinic. PLoS One. 2020;15(6):e0234049.
54. Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–2948.
55. Leslie KH, McCowan C, Pell JP. Adherence to cardiovascular medication: a review of systematic reviews. J Public Health (Bangkok). 2018;41(1):e84–e94.
56. Gebremichael GB, Berhe KK, Zemichael TM. Uncontrolled hypertension and associated factors among adult hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018. BMC Cardiovasc Disord. 2019;19(1):121.
57. Michalsen A, König G, Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart. 1998;80(5):437–441.
58. Jø N, Shrestha AD, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low-and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens. 2017;31(1):14–21.
59. Mugwano I, Kaddumukasa M, Mugenyi L, et al. Poor drug adherence and lack of awareness of hypertension among hypertensive stroke patients in Kampala, Uganda: a cross sectional study. BMC Res Notes. 2016;9(1):3.
60. Hareri HA, Abebe M. Assessments of adherence to hypertension medications and associated factors among patients attending tikur anbessa specialized hospital renal unit, Addis Ababa, Ethiopia 2012. Int J Nurs Sci. 2013;3(1):1–6.
61. Lulebo AM, Mutombo PB, Mapatano MA, et al. Predictors of non-adherence to antihypertensive medication in Kinshasa, Democratic Republic of Congo: a cross-sectional study. BMC Res Notes. 2015;8(1):526.
62. Ostini R, Kairuz T. Investigating the association between health literacy and non-adherence. Int J Clin Pharm. 2014;36(1):36–44.
63. Cunningham S, Kinsey JD. Pharmacist-Led Discharge Medication Counseling and its Corresponding Impact on Medication Adherence and Hospital Readmission Rates. Inov Pharm. 2020;11(3):6.
64. Thwe AIJMM, Ab ATHTK, Ab F Factors associated with drug-related emergency department visit: a systematic review. 2016.
65. Bernstein J, Bernstein E, Belanoff C, et al. The association of injury with substance use disorder among women of reproductive age: an opportunity to address a major contributor to recurrent preventable emergency department visits? Acad Emerg Med. 2014;21(12):1459–1468.
66. Barp J, Araújo A, Fernandes T, et al. Myocardial antioxidant and oxidative stress changes due to sex hormones. Braz J Med Biol Res. 2002;35(9):1075–1081.
67. Bhatia K, Elmarakby AA, El-Remessey A, Sullivan JC. Oxidative stress contributes to sex differences in angiotensin II-mediated hypertension in spontaneously hypertensive rats. Am J Physiol Regulator Integrative Comp Physiol. 2012;302(2):R274–R82.
68. Aboyade O, Beauclair R, Mbamalu O, Puoane T, Hughes G. Health-seeking behaviours of older black women living with non-communicable diseases in an urban township in South Africa. BMC Complement Altern Med. 2016;16(1):410.
69. Garcia M, Mulvagh SL, Bairey Merz CN, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118(8):1273–1293.
70. Vaccarino V, Bremner JD. Behavioral, emotional and neurobiological determinants of coronary heart disease risk in women. Neurosci Biobehav Rev. 2017;74:297–309.
71. Roy A, Rawal I, Jabbour S, Prabhakaran D. Tobacco and Cardiovascular Disease: A Summary of Evidence. Cardiovascular, Respiratory, and Related Disorders.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.