Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Predictors of Low-Level Disease-Specific Knowledge in Patients with Chronic Obstructive Pulmonary Disease
Authors Lee SH , Lee H, Kim YS , Park HK , Lee MK, Kim KU
Received 6 January 2020
Accepted for publication 3 May 2020
Published 19 May 2020 Volume 2020:15 Pages 1103—1110
DOI https://doi.org/10.2147/COPD.S244925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Sang Hee Lee,1,2 Haejung Lee,3 Yun Seong Kim,4 Hye-Kyung Park,5,6 Min Ki Lee,5,6 Ki Uk Kim5,6
1Department of Internal Medicine, Wonkwang University Sanbon Hospital, Gunpo-si, Republic of Korea; 2Department of Internal Medicine, Wonkwang University College of Medicine, Iksan, Republic of Korea; 3Department of Nursing, Pusan National University College of Nursing, Yangsan-si, Republic of Korea; 4Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan-si, Republic of Korea; 5Department of Internal Medicine, Pusan National University Hospital, Busan, Republic of Korea; 6Medical Research Institute, Pusan National University Hospital, Busan, Republic of Korea
Correspondence: Ki Uk Kim
Department of Internal Medicine, Pusan National University School of Medicine, 179 Gudeok-ro, Seo-gu, Busan 49241, Republic of Korea
Tel +82-51-240-7804
Fax +82-51-254-3127
Email [email protected]
Background: Disease-specific knowledge is associated with outcomes of patients, but the knowledge level of chronic obstructive pulmonary disease (COPD) patients is known to be low.
Objective: We measured the level of disease-specific knowledge and defined factors associated with poor disease knowledge in COPD patients.
Materials and Methods: A cross-sectional survey was performed in five hospitals in South Korea. At enrolment, all patients completed the Bristol COPD Knowledge Questionnaire (BCKQ), Satisfaction with Life Scale (SWLS), Personal Resource Questionnaire (PRQ), St. George’s Respiratory Questionnaire (SGRQ), 36-item Short-Form Health Survey (SF-36), and the Hospital Anxiety and Depression Scale (HADS). The data were analyzed via linear regression to identify factors associated with low-level knowledge of COPD.
Results: A total of 245 COPD patients were enrolled in this study. The mean total BCKQ score was 28.1 (SD, 7.4). The lowest scores were seen for items exploring knowledge of “Oral steroids” and “Inhaled steroids”. In univariate analysis, higher level of education (r = 0.17), low income (r = 0.13), the post-bronchodilator FEV1, % predicted (r = − 0.24), the post-bronchodilator FEV1/FVC ratio (r = − 0.13), SWLS (r = 0.15), PRQ (r = 0.16), SF-36 MCS (r = 0.13), HADS-A (r = − 0.17), and HADS-D (r = − 0.28) scores correlated with the BCKQ score (all p < 0.05). FEV1 (r = − 0.25, p < 0.001) and HADS-D score (r = − 0.29, p < 0.001) were significantly associated with the total BCKQ score in multivariate analysis.
Conclusion: Our Korean patients with COPD lacked knowledge on oral and inhaled steroid treatments. In particular, patients with higher-level lung function and/or depressive symptoms exhibited poorer disease-specific knowledge; such patients may require additional education.
Keywords: chronic obstructive pulmonary disease, disease knowledge, lung function, depression
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable disease characterized by persistent respiratory symptoms and airflow limitations.1 COPD may be diagnosed in patients with symptoms such as dyspnea, a chronic cough or sputum production, and/or a history of exposure to risk factors for the disease; a pulmonary function test can reveal the airway obstruction. Many treatment strategies are available to COPD patients and have proven effective in the management of symptoms and can also improve a patient’s quality of life. Drugs such as long-acting bronchodilators and/or inhaled corticosteroids are the mainstay of current pharmacotherapy.2,3 Non-pharmacologic treatment modalities such as smoking cessation strategies, pulmonary rehabilitation, and physical activity are all vital to patient care in COPD.1 One of the greatest challenges in health care is educating and enabling patients to understand and implement these various interventions.4 This has been driven in part by patients wishing to be better informed about their condition and in part by the recognition by health professionals that self-management is important to patients.5 It is crucial for patients with COPD to understand the nature of the disease, risk factors for its progression, and the role that they and their health-care workers must play in order to achieve optimal management and health outcomes.
However, disease-specific knowledge is inadequate in about half of all COPD patients.6 One study found that both COPD patients and their family members lacked comprehensive knowledge of COPD.7 In particular, there has not been much research on which patients have low levels of disease-specific knowledge and need for education. Here, we measured the level of disease-specific knowledge using the Bristol COPD Knowledge Questionnaire (BCKQ) and defined factors associated with poor disease knowledge in COPD patients.
Materials and Methods
Subjects and Study Design
A cross-sectional study was conducted between March 2010 and November 2010. Data analyzed in this study were derived from a baseline survey of symptom management intervention study of COPD patients. A total of 245 COPD patients were enrolled from five respiratory outpatient clinics, which were three university affiliated hospitals and two general hospitals in South Korea. Trained research assistants collected the data. COPD was diagnosed based on medical history, current symptoms, and pulmonary function tests (PFTs) that revealed a post-bronchodilator forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC) ratio (FEV1/FVC) <0.7 in all patients.1 Patients with any illness other than COPD likely to cause death within 6 months, or who were unable to undergo the PFT and 6-minute walk test (6MWT), were excluded; such patients had experienced myocardial infarction within the preceding 4 months, or showed unstable angina or congestive heart failure (New York Heart Association class III or IV). Patients considered clinically unstable were also excluded; these patients were characterized by significant changes in medications (including systemic corticosteroids and antibiotics), disease exacerbation, or hospital admission within the last 6 weeks. Approval of Institutional Review Boards (IRB) was obtained from Pusan National University Hospital (IRB No. 0740–326), Pusan National University Yangsan Hospital (IRB No. 2010019), and Ulsan University Hospital (IRB No. 10–66) before data collection. Two hospitals did not have official internal ethics committees and managerial committees in the hospitals reviewed the ethical aspects of the study and approved. Since the same study procedures were applied, those two hospitals accepted the IRB approval from other university hospitals. This study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients.
Clinical and Physiological Measurements
Baseline characteristics including age, smoking status (nonsmoker, ex-smoker, or current smoker), cumulative smoking history (pack-years), alcohol consumption status, educational level, total family income, marital, and employment status, and comorbidities were investigated using self-report questionnaires. Patient weight and height were measured prior to the PFT; the body mass index (BMI) was calculated as the weight in kilograms divided by the height squared (m2). The BCKQ, Satisfaction with Life Scale (SWLS), Personal Resource Questionnaire (PRQ), St. George’s Respiratory Questionnaire (SGRQ), 36-item Short-Form Health Survey (SF-36), and the Hospital Anxiety and Depression Scale (HADS) were utilized to assess disease-specific knowledge, life satisfaction, social support, HRQL, anxiety, and depression, respectively. Dyspnea severity was assessed using the modified Medical Research Council (mMRC) scale, and the 6MWT (total distance walked during 6 min) was performed. Furthermore, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) spirometric assessment for classification of disease severity was applied (Stage I [mild], FEV1 ≥ 80% predicted; Stage II [moderate], 50 ≤ FEV1 < 80% predicted; Stage III [severe], 30 ≤ FEV1 < 50% predicted; Stage IV [very severe], FEV1 < 30% predicted).1
Disease-Specific Knowledge
Disease-specific knowledge was measured using the BCKQ, which is a self-administered instrument, composed of 13 domains; each domain includes five statements with response options of “true”, “false” and “don’t know”.5 The domains are as follows: 1) epidemiology, 2) etiology, 3) symptoms, 4) breathlessness, 5) phlegm production, 6) infection, 7) exercise, 8) smoking, 9) vaccination, 10) inhaled bronchodilators, 11) antibiotics, 12) oral steroids, and 13) inhaled steroids. Correct responses are scored “1”; all other answers are scored zero. The total score ranges from 0 to 65; higher scores indicate greater knowledge of COPD.
Life Satisfaction
The Satisfaction With Life Scale (SWLS) is an internationally recognized self-report questionnaire that yields an overall measure of satisfaction.8 The SWLS includes the following five questions on life satisfaction (including non-affective subjective well-being) measured using seven-point Likert scales: 1) In most ways my life is close to my ideal; 2) The conditions of my life are excellent; 3) I am satisfied with my life; 4) So far I have gotten the important things I want in life; and, 5) If I could live my life over, I would change almost nothing. High SWLS scores represent high life satisfaction. Scores range from 5 to 35. A score of 20 represents the midpoint between dissatisfaction and satisfaction.
Social Support
Social support was measured using the Personal Resource Questionnaire (PRQ), which is a self-administered instrument composed of 15 items. The PRQ measures perceived social support.9 The PRQ-2000 is the latest version of the instrument and was used herein. Each item has seven possible responses ranging from 1 (“strongly disagree”) to 7 (“strongly agree”). Higher scores indicate higher levels of perceived situational social support.
Health-Related Quality of Life
Disease-specific HRQL was assessed using the St. George’s Respiratory Questionnaire (SGRQ), which is a standard instrument for measuring health impairment in patients with airway diseases.10 The SGRQ contains 50 items divided into three domains: Symptoms, Activity, and Impact. A score is calculated for each domain and a total score is also calculated. Lower scores indicate higher HRQL.
For a generic HRQL score, the 36-item Short-Form health survey (SF-36) was used.11 The SF-36 comprises 36 items divided into eight domains: Physical Functioning (PF), Role-Physical (RP), Bodily Pain (BP), General Health (GH), Vitality (VT), Social Functioning (SF), Role-Emotional (RE), and Mental Health (MH). These domains create a profile of the subject. Two summary scores can also be aggregated, the Physical Component Summary (PCS) and the Mental Component Summary (MCS). Scores range from 0 to 100, with higher scores representing higher HRQL.
Anxiety and Depression
Anxiety and depression symptoms were evaluated using the Hospital Anxiety and Depression Scale (HADS).12 This instrument includes an anxiety subscale (HADS-A) and a depression subscale (HADS-D), both of which include seven items. Total scores range from 0 to 21. A score of 0 to 7 on either subscale is considered within the normal range, while scores ≥8 indicate the presence of an anxiety or depressive disorder.13
Statistical Analysis
Continuous data are expressed as means ± standard deviation (SD) and categorical data as numbers with percentages. Univariate linear regression was used to analyze the relationships between level of COPD knowledge and other variables. Multivariate linear regression was performed to identify factors independently associated with COPD knowledge. Statistical analysis was performed using MedCalc Statistical Software version 19.1.3 (MedCalc Software bv, Ostend, Belgium; https://www.medcalc.org; 2019). The level of significance was set at P < 0.05.
Results
A total of 245 patients were included in this study, of whom 226 (92.2%) were male; the mean age was 66.9 years and the mean BMI was 22.3 kg/m2 (Table 1). The mean cumulative smoking history was 38.2 pack-years and 31.4% of the participants drank alcohol. Twenty-six patients had received extensive education (≥13 years) (10.6%) and 39 (15.9%) had high monthly incomes (> 3000 US$). A total of 127 patients had dyspnea of mMRC grade ≥ 2 (51.8%). The mean FEV1% predicted was 60.6%. The most common comorbidities were hypertension (22.0%) and diabetes (8.2%).
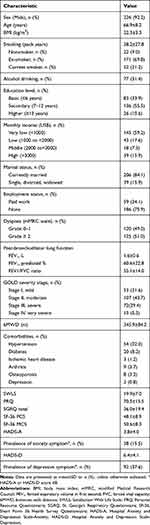 |
Table 1 Baseline Characteristics of the Patients with COPD (n = 245) |
Table 2 shows the overall BCKQ score and the individual scores for all 13 topics. The mean total BCKQ score was 28.1 (SD, 7.4; range: 5–46). The highest scores were seen for “Symptoms” (3.1, SD 1.1) and “Exercise” (3.1, SD 1.1), and the lowest for “Oral steroids” (0.7, SD 1.0) and “Inhaled steroids” (0.6, SD 0.9). Table 3 shows the percentage of patients who answered each item correctly, which was lowest for “Oral steroids” (14.0%) and “Inhaled steroids” (11.9%), and highest for “Exercise” (61.5%).
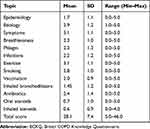 |
Table 2 Disease Knowledge Scores According to the BCKQ |
 |
Table 3 Percentage of Patients Giving a Correct Response for All 65 Items Indexed by 13 Topics and Their Five Stems (a, b, c, d, e) |
Table 4 shows the results of univariate analysis of variables associated with the total BCKQ score. Higher level of education (≥13 years) was associated with the total BCKQ score (r = 0.17, p = 0.01), while basic or secondary education was not. Low income (r = 0.13, p = 0.037), the post-bronchodilator FEV1, % predicted (r = −0.24, p < 0.001), post-bronchodilator FEV1/FVC ratio (r = −0.13, p = 0.044), and SWLS (r = 0.15, p = 0.02), PRQ (r = 0.16, p = 0.012), SF-36 MCS (r = 0.13, p = 0.045), HADS-A (r = −0.17, p = 0.006), and HADS-D (r = −0.28, p < 0.001) scores were also correlated with the total BCKQ score. The total BCKQ score increased progressively as the GOLD stage was increased (as the post-bronchodilator FEV1, % predicted decreased) (Figure 1).
 |
Table 4 Correlation Between the Total BCKQ Score and Variables |
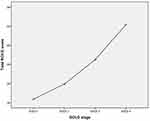 |
Figure 1 The total BCKQ score according to the disease severity (GOLD stage). |
Table 5 shows the results of multivariate analysis of factors associated with the total BCKQ score. Higher level of education, low income, the post-bronchodilator FEV1, % predicted, the post-bronchodilator FEV1/FVC ratio, and the SWLS, PRQ, SF-36 MCS, HADS-A, and HADS-D scores, all of which were statistically significant in univariate analysis, were entered into the multivariate regression model. Both the post-bronchodilator FEV1, % predicted (r = −0.25, p < 0.001) and the HADS-D score (r = −0.29, p < 0.001) were significantly associated with the total BCKQ score.
 |
Table 5 Multivariate Analysis of the Factors Associated with the Total BCKQ Score |
Discussion
We found that the total BCKQ score, which indicates the level of disease-specific knowledge, was about 28.0 points in our cohort South Korean COPD patients. This result is higher than that of a previous study reported in South Korea.14 Compared to the patients in both studies, the average age, gender ratio, and the percentage of college education were similar. However, there were some differences in pulmonary function test; the average FEV1 value was higher in our study (60.6 vs 52.2).
In our study, the lowest scores were seen for “Oral steroids” and “Inhaled steroids”. In particular, only 4–6% of patients were aware that “Steroid inhalers can be used for rapid relief of breathlessness” and “Inhaled steroids improve lung function in COPD patients”. Familiarity with inhaled bronchodilator was also low among our participants. Inappropriate knowledge of medications can have a negative effect on drug adherence and efficacy. Previous study reported that poor adherence of COPD patients to inhaled steroids and inhaled bronchodilator (tiotropium) was associated with an increased risk of mortality.15 Another study also reported that adherence with the inhaled medication increases symptoms, acute exacerbations, and hospitalizations.16 No studies have yet shown that low level of disease-specific knowledge affect directly poor outcomes such as acute exacerbations or mortality in patients with COPD. However, it is believed that the appropriate knowledge of the medications can affect drug adherence and efficacy, as a result, have a good effect on patients’ outcomes. Therefore, it is necessary to identify what areas of knowledge are low and to intensively improve those areas when developing patient education programs.
We found that neither educational nor income levels were independently associated with disease-specific patient knowledge. On the other hand, it was found that lung function and depressive symptoms are independent factors in this study. Patients with better lung function (ie, higher FEV1 levels) showed inadequate knowledge of COPD. The FEV1 is used to clarify the severity of the airflow limitation. It is an important parameter in the prediction of clinical outcomes such as mortality and hospitalization.1 However, the correlation between FEV1, symptoms, and impairment of a patient’s health status is known to be weak.17 For this reason, patient symptoms and health status are commonly used for clinical assessment of COPD.18 However, a previous study reported that patients with COPD who have low FEV1 use more COPD medications and incur higher COPD-related health-care costs than those with high FEV1. This study results confirm that lung function (FEV1) may be a useful way for providers to identify and monitor respiratory impairment in COPD patients.19 The results of our study show that patients at mild disease tend to have a low disease-knowledge. This is probably because these patients do not often use the health-care resources due to the low level of symptoms and impairment on daily activities. However, even mild COPD patients reported significant deterioration of HRQL and experienced exacerbations.20 Education at this stage of the disease may have a great impact on prevention of disease progression and exacerbations.
Depression was associated with knowledge of COPD among our patients. The risk of depression is higher in COPD patients than the general population, even after adjusting for disease severity.21,22 However, only 30–50% of COPD patients with depressive symptoms were adequately treated according to previous studies.23 We found that 37.6% of patients had depressive symptoms; however, only 0.8% had been diagnosed with depression. Patients who are depressed may be more likely to feel unsupported by clinic staff and be poorly adherent to treatment.24 These may affect their health-care utilization and the low level of disease knowledge. Although the direction of causality cannot be inferred from the results of this study, it is reasonable to suggest that COPD patients must be screened for depression, and patients who are depressed must be educated regarding the issues associated with the disease. Additionally, it is necessary to increase levels of clinic support, including efforts to adhere to pharmacotherapy.
The strength of this study lays in its analysis of disease-specific knowledge using a validated instrument in relatively large number of Asian patients with COPD. In addition, this study suggests a solution to improve the disease-specific knowledge through analysis of factors that may affect low level of knowledge. However, this study had several limitations. First, the COPD patients were recruited from a small geographical area and were mostly male. Although this may result from the gender ratio characteristic of COPD in South Korea,25 our findings should be generalized with caution. Second, the study used a cross-sectional design, such that we could not address causality. Third, the overall explanatory value of multivariable regression model was weak. Therefore, the results may not strongly explain the disease knowledge in patients with COPD. However, since no studies have been conducted to analyze factors associated with low level of disease-specific knowledge through multivariate analysis in patients with COPD, the results are considered meaningful and suggest that further research will be needed to increase knowledge in this area.
Conclusion
Our Korean patients with COPD lacked disease-specific knowledge on oral and inhaled steroid treatments. In particular, patients with higher-level lung function and/or depressive symptoms exhibited poorer disease-specific knowledge; such patients may require targeted educational programs.
Acknowledgments
This research was supported by the Wonkwang University in 2020.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the prevention, diagnosis and management of COPD; 2019. Available from: http://goldcopd.org.
2. Decramer M, Celli B, Kesten S, Lystig T, Mehra S, Tashkin DP. Effect of tiotropium on outcomes in patients with moderate chronic obstructive pulmonary disease (UPLIFT): a prespecified subgroup analysis of a randomised controlled trial. Lancet. 2009;374(9696):1171–1178. doi:10.1016/s0140-6736(09)61298-8
3. O’Donnell DE, Sciurba F, Celli B, et al. Effect of fluticasone propionate/salmeterol on lung hyperinflation and exercise endurance in COPD. Chest. 2006;130(3):647–656. doi:10.1378/chest.130.3.647
4. Scott AS, Baltzan MA, Dajczman E, Wolkove N. Patient knowledge in chronic obstructive pulmonary disease: back to basics. COPD. 2011;8(5):375–379. doi:10.3109/15412555.2011.605402
5. White R, Walker P, Roberts S, Kalisky S, White P. Bristol COPD knowledge questionnaire (BCKQ): testing what we teach patients about COPD. Chron Respir Dis. 2006;3(3):123–131. doi:10.1191/1479972306cd117oa
6. Boot CR, van der Gulden JW, Vercoulen JH, et al. Knowledge about asthma and COPD: associations with sick leave, health complaints, functional limitations, adaptation, and perceived control. Patient Educ Couns. 2005;59(1):103–109. doi:10.1016/j.pec.2004.10.007
7. Nakken N, Janssen DJA, van den Bogaart EHA, et al. Knowledge gaps in patients with COPD and their proxies. BMC Pulm Med. 2017;17(1):136. doi:10.1186/s12890-017-0481-8
8. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1):71–75. doi:10.1207/s15327752jpa4901_13
9. Weinert C, Brandt PA. Measuring social support with the personal resource questionnaire. West J Nurs Res. 1987;9(4):589–602. doi:10.1177/019394598700900411
10. Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327. doi:10.1164/ajrccm/145.6.1321
11. Kil SY, Oh WO, Koo BJ, Suk MH. Relationship between depression and health-related quality of life in older Korean patients with chronic obstructive pulmonary disease. J Clin Nurs. 2010;19(9–10):1307–1314. doi:10.1111/j.1365-2702.2009.03053.x
12. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
13. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi:10.1016/s0022-3999(01)00296-3
14. Choi JY, Chung HI, Han G. Patient outcomes according to COPD action plan adherence. J Clin Nurs. 2014;23(5–6):883–891. doi:10.1111/jocn.12293
15. Koehorst-Ter Huurne K, Groothuis-Oudshoorn CG, vanderValk PD, Movig KL, van der Palen J, Brusse-Keizer M. Association between poor therapy adherence to inhaled corticosteroids and tiotropium and morbidity and mortality in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1683–1690. doi:10.2147/copd.s161374
16. Ngo CQ, Phan DM, Vu GV, et al. Inhaler technique and adherence to inhaled medications among patients with acute exacerbation of chronic obstructive pulmonary disease in vietnam. Int J Environ Res Public Health. 2019;16(2). doi:10.3390/ijerph16020185
17. Han MK, Muellerova H, Curran-Everett D, et al. GOLD 2011 disease severity classification in COPDGene: a prospective cohort study. Lancet Respir Med. 2013;1(1):43–50. doi:10.1016/s2213-2600(12)70044-9
18. Westwood M, Bourbeau J, Jones PW, Cerulli A, Capkun-Niggli G, Worthy G. Relationship between FEV1 change and patient-reported outcomes in randomised trials of inhaled bronchodilators for stable COPD: a systematic review. Respir Res. 2011;12:40. doi:10.1186/1465-9921-12-40
19. Ke X, Marvel J, Yu TC, et al. Impact of lung function on exacerbations, health care utilization, and costs among patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:1689–1703. doi:10.2147/copd.s108967
20. Rennard SI, Vestbo J. Natural histories of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(9):878–883. doi:10.1513/pats.200804-035QC
21. Di Marco F, Verga M, Reggente M, et al. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006;100(10):1767–1774. doi:10.1016/j.rmed.2006.01.026
22. Omachi TA, Katz PP, Yelin EH, et al. Depression and health-related quality of life in chronic obstructive pulmonary disease. Am J Med. 2009;122(8):778 e779–715. doi:10.1016/j.amjmed.2009.01.036
23. Jordan N, Lee TA, Valenstein M, Weiss KB. Effect of care setting on evidence-based depression treatment for veterans with COPD and comorbid depression. J Gen Intern Med. 2007;22(10):1447–1452. doi:10.1007/s11606-007-0328-8
24. Bosley CM, Corden ZM, Rees PJ, Cochrane GM. Psychological factors associated with use of home nebulized therapy for COPD. Eur Respir J. 1996;9(11):2346–2350. doi:10.1183/09031936.96.09112346
25. Kim DS, Kim YS, Jung KS, et al. Prevalence of chronic obstructive pulmonary disease in Korea: a population-based spirometry survey. Am J Respir Crit Care Med. 2005;172(7):842–847. doi:10.1164/rccm.200502-259OC
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
