Back to Journals » International Journal of Women's Health » Volume 14
Predictors of Hepatitis B Virus Infection Vaccine Hesitancy Among Pregnant Women Attending Antenatal Care at Lubaga Hospital, Kampala, Uganda
Authors Afolabi IB , Aremu AB , Maidoki LA, Atulomah NO
Received 10 June 2022
Accepted for publication 8 August 2022
Published 17 August 2022 Volume 2022:14 Pages 1093—1104
DOI https://doi.org/10.2147/IJWH.S378000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Marleen van Gelder
Ismail Bamidele Afolabi,1 Abdulmujeeb Babatunde Aremu,2 Lawal Abdurraheem Maidoki,1 Nnodimele Onuigbo Atulomah1
1Faculty of Science and Technology, Department of Public Health, Cavendish University, Kampala, Uganda; 2Faculty of Health Sciences, Department of Human Anatomy, Islamic University in Uganda, Kampala Campus, Kampala, Uganda
Correspondence: Ismail Bamidele Afolabi, Email [email protected]
Background: While hepatitis B virus infection may be seen as a global threat within the medical and scientific community, primary prevention via vaccination remains the most effective approach towards breaking the chain of transmission of HBV infection. However, vaccination uptake in Uganda has been modest despite a very endemic national figure resulting from the vertical transmission of this infection. This study assessed the predictors of HBV vaccine hesitancy among pregnant women attending Antenatal clinic in Central Uganda.
Methodology: A hospital-based cross-sectional study employing a five-sectioned pretested interviewer-administered questionnaire was conducted to obtain data from 385 consenting pregnant women. Responses for the antecedent variables were transformed into weighted aggregate scores using SPSS version 26. Multivariable logistic regression analysis was employed to ascertain the predictors of HBV vaccine hesitancy with the cut-off for hypotheses set at 5% level of significance.
Results: The majority of the respondents (59%) were between the ages of 18 and 28 years. Women with secondary educational attainment were predominant (42.3%). The respondents had mean scores of 5.97± 6.61, 17.10± 18.31, and 12.39± 13.37, respectively, computed for knowledge of HBV infection, perception, and behavioral skills towards HBV prevention. Regarding vaccine hesitancy, three-quarters of the women (74%) hesitated to uptake HBV vaccine. While negative significant associations exist between marital status (AOR = 0.47, 95% CI = 0.22– 1.01), knowledge (AOR = 0.79, 95% CI = 0.70– 0.89), behavioral skills (AOR = 0.88, 95% CI = 0.81– 0.95) and vaccine hesitancy, level of education (AOR = 1.88, 95% CI = 1.08– 3.27) and perception (AOR = 1.11, 95% CI = 1.05– 1.18) on the other hand, positively predicted vaccine hesitancy.
Conclusion: The findings reported an extremely high degree of HBV vaccine hesitancy among the expectant mothers discovered to be linked with marital status, educational attainment, HBV-specific knowledge, perception and behavioral skills. This necessitates targeted health education for married women with lower educational attainment to improve their knowledge which will in turn shape their perception and behavioral skills towards satisfactory uptake of HBV vaccine.
Keywords: knowledge, perception, behavioral skills, vaccine uptake, hesitancy
Background
Globally, Hepatitis B virus (HBV) infection continues to be linked with mortality from deteriorating cirrhosis and carcinoma of the liver.1 The magnitude of hepatitis B virus infection varies geographically. WHO Western Pacific Region boasts the highest HBV epidemiological burden. This is followed by the African Region, where the infected adult population is, respectively, 6.2% and 6.1%. In the WHO Region of Europe, Asia South-East Region as well as the Region of Eastern Mediterranean, the population generally, is proportionately infected with estimates of 1.6%, 2.0%, and 3.3%, respectively. More so, in the WHO American Regions, 0.7% of the population is reported to have been infected.2
Hepatitis B virus is known to be the cause of hepatitis B virus infection. It is a virus with bounded DNA that targets the liver for infection.3 The majority of its carriers do not become aware that they have the viral infection because of its asymptomatic nature at the onset and its slow development, which makes the virus kill silently.4
During the last decade, the magnitude of HBV infection, whether acute or chronic, among adults in Tanzania based on the prevalence, was reported to be 8.8% and 6%,5,6 respectively, where 74% of north-eastern Tanzanian women prior to the study above have been documented to be HBV-positive.7 Furthermore, a report from the study conducted in a tertiary-owned health facility on the workers determined the prevalence of chronic HBV to be 7.0%,8 with the current report for children under-five years of age estimated to be at a prevalence rate of 1.69%.9
Similarly, in Ethiopia, a study on pregnant women’s hepatitis B virus infection burden documented the prevalence to be 6.9%, denoting a high-intermediate endemicity of the infection in the area.10 Concerning vertical transmission, the epidemiological burden among children aged under 5 was recently reported to be 2.61% in the country.9 This implies that HBV infection remains a significant issue that needs to be resolved by public health. Additionally, a prevalence of 11% among pregnant women was reported in Nigeria, where 33% HBeAg positivity was also demonstrated, indicating an active viral replication and risk of infectivity.11 Over time, as a result of vertical transmission, the prevalence among under-five children was reported to be 2.61%.9 The trend in the burden of the infection has overwhelmingly increased to 10.5% as documented in the study conducted on pregnant women in South-West Nigeria.12 The 2016 survey by Uganda Population-based HIV Impact Assessment (UPHIA) affirmed that adults’ infection of hepatitis B virus prevalence stands at 4.3%, accounting for 5.6% and 3.1% prevalence among men and women, respectively.13 This assessment is an indication that hepatitis B virus infection lingers endemically in Uganda despite the most efficacious intervention put in place through vaccination by the Ministry of Health across high prevalence areas within the country.14 Pregnant women who tested positive are vulnerable to passing this infection to their babies because vertical transmission constitutes the main route of HBV infection perpetuation.15 Therefore, they are to be treated as a population sub-group of focus for any likely micro-elimination of hepatitis B of viral origin.16 The prevalence of HBV infection among reproductive-aged women in Uganda was lately reported to be approximately 12%.17 More recently, due to vertical transmission, the magnitude proportion for hepatitis B virus infection among children under-five years of age was found to be 3.16%.9 In this kind of setting where the magnitude among women of reproductive age is high, vaccination is always recommended as an effective tool in national policies directed toward the prevention and control.18 Therefore, it is necessary that: for the surface antigen of hepatitis B to be detected, likewise, for birth administration of HBV vaccine to the neonates of positive mothers tested during pregnancy to break the cycle of materno-foetal transmission, pregnant women need to be routinely screened to know their states of vaccination requirement.19 This is because 84% of world HBV infection-related mortality could be prevented by dispensing vaccines to 90% of neonates not later than a day after birth.2,20
Numerous studies conducted on HBV vaccine uptake have been limited mostly to different sub-population groups like health-care workers and pregnant women among others. These studies have indeed demonstrated unsatisfactory low uptake of hepatitis B virus infection vaccination across different endemic regions of the world such as Sub-Saharan Africa and Asia, with factors like knowledge of HBV infection and vaccine, perception of risk, personal factors, accessibility to vaccine and costs of vaccination believed to contribute to the non-uptake of the vaccine.21–24 These findings corroborate the reasons why there remains lingering chronicity of HBV infection in most of these settings. Pregnant women need to protect themselves and their unborn babies from the infection by vaccine uptake as a means of halting early transmission of the prevailing HBV infection.25 However, evidence on the factors associated with the reluctance to up-taking HBV vaccine among this vulnerable group in Central Uganda is limited. It is in this view that this study aimed at exploring the predictors of the hesitancy in up-taking hepatitis B virus infection vaccine among expectant mothers, by focusing on the knowledge of hepatitis B virus infection, the perception of risk associated with HBV infection and vaccination and the behavioral skills towards HBV prevention behaviors such as vaccination, in order to guide HBV vaccination policy directed towards breaking the chain of vertical transmission of the infection.
Methods
Study Site
This study was conducted at Lubaga Hospital which is otherwise known as Uganda Martyrs Hospital. It is located in the west of Kampala within Lubaga Division situated on Lubaga Hill. The private not-for-profit health facility is owned by Kampala Roman Catholic Archdiocese. Over the years, the hospital, which is relatively a high-volume 237-bed-capacity facility, has gained a reputation as a highly affordable health-care provider. Subsequently, it has persistency allured and managed the treatment of individuals of low and middle socio-economic status. Millions of people have been reported to have benefited from its health-care services during its long history of existence. Hitherto, this hospital is known to have built a very strong anecdotal reputation for treatment/management of liver diseases and often enjoyed the referral of anybody with liver problems in Uganda. The hospital is one of the few authorized hospitals in Kampala that is given the liberty by the Ministry of Health to administer HBV vaccine in an attempt to stop the fake supply of vaccines within the country.13 The vaccination clinic operates from Mondays through Saturdays at the Public Health Department of the Health Facility and the Facility boasts approximately 400 antenatal attendees per week.
Study Design
The study was a health facility-based cross-sectional study that employed a pretested interviewer-administered questionnaire to capture quantitative data on the predictors of HBV infection vaccine hesitancy among 385 randomly selected expectant mothers using Lubaga health facility for antenatal care between September and October 2020.
Sample Size Estimation and Sampling Procedure
The sample size was estimated using Kish Leslie formula for cross-sectional study26 on the account of 47% prevalence of HBV infection awareness reported by a previous study,27 level of precision of 0.05 and Alpha (α) error of 5% as shown below:
P = reported true proportion of HBV infection awareness (47%).
Zα = Confidence interval at 95% corresponding to 1.96.
d = 5% error of maximum acceptability.
The study employed a systematic random sampling technique. Upon the arrival of the expectant mothers to the ANC, they were registered, and following a random start, every second pregnant woman on the register waiting to be attended to was recruited. The periodic interval was continuously employed until the required sample size was attained. On average, depending on the number of antenatal visitations per day, 30 expectant mothers were recruited per day from Mondays through Fridays every week for the complete study duration.
Inclusion and Exclusion Criteria
The study included consenting pregnant women using the health facility for ANC and who aged not less than 18 years. Those who were severely indisposed were excluded from participation in the study procedures.
Variables and Tests of Significance
Measures
Independent Variables
The predictors measured in this study include the demographic attributes eliciting information on the respondents’ age, region of birth, educational attainment, marital status, the religion of the respondents, and employment status. We also measured the levels of knowledge regarding HBV infection and vaccination, perception of risk associated with HBV infection and vaccination as well as behavioral skills towards HBV prevention. The knowledge was operationalized as the comprehension of the participants about the characteristic features of HBV infection ranging from the cause, transmission, risk factors, prevention and vaccination. It was measured by 13 questions and all given answers to questions on the disease-specific knowledge was transformed by computation to generate the overall score and the summaries of descriptive statistics. The level of knowledge displayed by the participants was described using the following statistics: the obtained mean score on the rating scale, standard deviation, 95% confidence interval and the percentage mean score.
The perception measured in this study denotes motivation as it measures how risky the respondents perceive the infection to be, and their possibility of acting because of it. It was assessed by 12 questions on a 4-point Likert’s scale. All responses to the constructs of motivational perception were transformed by computation to generate the weighted aggregate score. The obtained mean score on the rating scale or the percentage mean score was used to describe the level of perception. Hence, perception was measured on a rating scale of 33-points. The behavioral skills were operationalized as the certainty and the confidence that the respondents will engage in prevention behaviors defined by their self-efficacy, outcome expectancy, perceived severity, and perceived barriers. It was explored using the generated mean score from the computed responses of 7-items measured on a 4-point Likert’s scale. Therefore, the behavioral skills were measured on an aggregate weighted 21-point rating scale.
Dependent Variable
The main outcome of the study is the self-reported hepatitis B virus infection vaccine hesitancy measured categorically as thus: “hesitate to take vaccine (Yes)” (if respondents had not taken any of the recommended 3 doses of vaccines) and “do not hesitate to take vaccine (No)” (if respondents had previously taken vaccine once, twice or completely). The response “Yes is coded” “0” while the response “No” is coded “1”.
Data Collection Procedure
The study employed a pretested interviewer-administered questionnaire designed in the English language to capture data from the expectant mothers. Two trained nurses on ethics in human subject research from the antenatal unit of the public health department of the hospital were recruited to aid the data collection. The aim of the study was explained to the respondents by the research assistants and written consents were obtained from the eligible expectant mothers before administering the data collection tool to them. The informed consent form and questionnaire are available as Appendices.
Data Analysis
The collected data were entered into SPSS version 26 where the predictor variables were transformed into a rating scale. The responses from the predictor variables were computed to obtain descriptive statistics like mean and standard deviations. Frequency and percentages were generated for the categorical study variables. Analysis of variance was done to test variability in levels of knowledge, perception, and behavioral skills across the demographic characteristics and how vaccine hesitancy could be better explained by these variables. Pearson correlation was evaluated to test the linear relationship between the predictor variables in accordance with the employed theoretical framework (Information-motivation-behavioral skills model).
Bivariate logistic regression was employed to test each predictor variable against the outcome variable and generate crude associations. Based on the employed theoretical framework and previous empirical studies, variables were selected for the multivariable logistic model, and the multivariable logistic regression analysis was used to ascertain the independent predictors of vaccine hesitancy with the level of significance set at a cut-off of (p ≤ 0.05).
Ethical Issues
Lubaga Hospital Ethical Review Committee (LHREC) granted an approval letter with a referenced protocol number LHREC/2020/07 to conduct the study following a thorough review of the study proposal to ensure adherence to the safety and protection of the rights of human subjects. The study procedures were conducted in accordance with the Declaration of Helsinki. All the selected pregnant women gave their written informed consent before their participation, and confidentiality was attached to data disclosure.
Results
Demographic Characteristics
The findings from the study on the frequency across the demographic information of the respondents showed that, out of the total 385 pregnant women, more than half of them (59%) were between the ages of 18 and 28. Relatively three-quarters of the respondents (70.6%) reported to be from the central region while less than half of the respondents 201 (42.3%) had secondary educational attainment. Further, 8 out of every 10 pregnant women were married (85.5%). Religious-wise, Catholics (36.4%) were predominant and the overwhelming majority (81.3%) reported to be employed. Upon assessing the mean scores for HBV infection specific-knowledge, perception of risk towards HBV infection/vaccination as well as behavioral skills towards HBV prevention, better HBV infection knowledge was observed among the following: older respondents (6.9), respondents from the Central region (6.5), respondents with above secondary education (7.4), Protestants (6.6) and the mothers who are employed (6.6). Regarding perception, the following demonstrated better mean scores: older respondents between the ages of 29 and 39 (18.4), respondents from the Central region (17.9), respondents with post-secondary education (18.7), married women (17.9), Muslims (18.5) and the respondents who reported to be employed (18.1). Furthermore, on the reference scale, the oldest group of respondents (12.9), respondents from the Central region (12.9), mothers with University education (14.0), married respondents (13.1), Protestants (13.2), and those employed (13.3) demonstrated the better scores for behavioral skills (see Table 1).
 |
Table 1 Demographic Characteristics of the Study Participants |
Knowledge, Perception and Behavioral Skills
Findings on the predictor variables among the study respondents showed that regarding hepatitis B virus infection knowledge measured on an aggregate weighted 12-points rating scale, the respondents scored a mean of 6.29 (5.97±6.61) which denotes a prevalence of 52.4%. On a rating scale of 33-points, the respondents scored an overall mean of 17.71 (17.10± 18.31) for perception, depicting 53.6% of the total perception anticipated from the respondents. Furthermore, the observed aggregate weighted score for behavioral skills of the respondents as measured on a 21-points reference scale was 12.88 (12.39±13.37) contributing to a percentage mean score of 61.3%. Upon the analysis of the relationship between knowledge, perception and behavioral skills using Pearson correlation, a positive significant linear relationship was observed between knowledge and behavioral skills (r = 0.699, p < 0.001) as well as perception and behavioral skills (r = 0.630, p < 0.001). The general mean scores computed for the predictor variables and their linear relationships are presented in Table 2 and also displayed in the conceptual framework that guided the study (see Figure 1).
 |
Table 2 Findings on the Predictor Variables Among the Study Respondents (N = 385) |
 |
Figure 1 Conceptual Framework derived from IMB model for the diagnosis of health outcomes related to HBV infection via vaccine uptake. |
HBV Infection Vaccine Hesitancy Among the Study Participants
Findings from this study regarding hesitation to uptake vaccine revealed that relatively 3 out of every 4 respondents (74%) hesitate to take HBV vaccine (see Figure 2). Additionally, upon assessing the mean scores for HBV infection knowledge, perception and behavioral skills, respondents who demonstrated vaccine hesitancy consistently displayed the poorest scores for HBV infection knowledge ( =5.65, SD = 3.25), perception of risk towards HBV infection and vaccination (
=5.65, SD = 3.25), perception of risk towards HBV infection and vaccination ( =17.44, SD = 6.23) and behavioral skills towards preventing HBV infection (
=17.44, SD = 6.23) and behavioral skills towards preventing HBV infection ( =12.02, SD = 4.97). Table 3 describes in detail, the mean scores reported for the variables across the status of HBV infection vaccine hesitancy among the respondents.
=12.02, SD = 4.97). Table 3 describes in detail, the mean scores reported for the variables across the status of HBV infection vaccine hesitancy among the respondents.
 |
Table 3 Findings on HBV Infection Vaccine Hesitancy Among the Study Respondents |
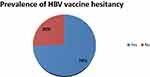 |
Figure 2 Showing the prevalence of vaccine hesitancy among the study respondents. |
Predictors of HBV Infection Vaccine Hesitancy Among the Pregnant Women
Regarding the factors associated with HBV vaccine hesitancy, findings from this study showed that at bivariate level, age and educational attainment were significantly associated with vaccine hesitancy. It was observed that younger respondents (between 18 and 28 years) were 3.8 times more likely to hesitate vaccine uptake compared to others (COR = 3.83, 95% CI = 0.92–15.89). Similarly, expectant mothers with secondary education and below were 2.7 times more likely not to vaccinate compared to those with above secondary educational attainment (COR = 2.74, 95% CI = 1.69–4.46). However, at the multivariable model, vaccine hesitancy is independently predicted by the educational attainment and marital status of the respondents when tested across the demographic attributes. The results further showed that pregnant women who had secondary education and below were 1.9 times more likely not to uptake vaccine compared to women who had above secondary educational attainment (AOR = 1.88, 95% CI = 1.08±3.27) and single respondents were 53% less likely to hesitate vaccine compared to the married respondents (AOR = 0.47, 95% CI = 0.22–1.01). This implies that single respondents were 2.1 times more likely not to hesitate vaccine uptake compared to married respondents. Furthermore, knowledge of HBV infection and behavioural skills were observed to be negatively associated with vaccine hesitancy. At bivariate level, the odds of vaccine hesitancy decrease as the levels of knowledge (COR = 0.76, 95% CI = 0.69–0.83) and behavioural skills (COR = 0.97, 95% CI = 0.69–0.83) increase. At the multivariable logistic model, while perception (AOR = 1.11, 95% CI = 1.05–1.18) was observed to be positively associated with vaccine hesitancy after no significant negative association at bivariate analysis, knowledge (AOR = 0.79, 95% CI = 0.70–0.89) and behavioural skills (AOR = 0.88, 95% CI = 0.81–0.95) remain negatively associated with vaccine hesitancy. This denotes that for every increase in the levels of knowledge and behavioural skills, the odds of hesitating vaccine decrease by 21% and 12%, respectively, among the expectant mothers. Therefore, as the knowledge of HBV infection increases by a unit among the respondents, the odds of vaccinating are 1.27 times higher. Also, as the level of behavioural skills increases, the odds of not hesitating vaccine (ie, up-taking vaccine) are 1.1 times higher (see Table 4).
 |
Table 4 Bivariate and Multivariable Relationships Between Predictor Variables and Vaccine Hesitancy |
Discussion
This present study captured pertinent hepatitis B virus infection and vaccination-related data from 385 eligible pregnant women in a private-not-profit health facility in central Uganda, where it was found that demographically, the majority of the expectant mothers were between the ages of 18 and 28 years and had secondary educational attainment. It was further observed that 3 out of every 4 expectant mothers (74%) that participated in this study displayed hesitation to uptake hepatitis B virus infection vaccine. The predictors of this extremely high and unsatisfactory vaccine hesitancy reported in our study were having secondary education attainment or below, being inadequately informed about hepatitis B virus infection and vaccination, having a correct perception of risk towards HBV infection, and displaying bad behavioral skills towards HBV prevention. This extremely high degree of HBV infection vaccine hesitancy among our study respondents invariably denotes a very low uptake of hepatitis B vaccination and this is found to be in concord to what numerous studies have reported like the ones previously conducted towards screening and vaccination in a highly endemic region in Northern Uganda,21 in Nigeria22 and Pakistan.23 Contrary to this report of low vaccine uptake or hesitation to vaccinate for HBV infection, is the report from a study conducted in Uganda among health-care givers28 and in Ethiopia,29 although our present facility-based study focuses on expectant mothers and not health-care workers as the cited studies explored. The perpetuation of this poor reluctancy in vaccination for HBV infection could be linked to inadequate HBV infection-related awareness and education generally in Uganda whereas other diseases of infectious origin like HIV/AIDS have captured the attention of the government sufficiently21 to the extent that during Antenatal visitations, testing for HIV for all expectant mothers is a mandatory service among the services offered at the ANC clinics.14 However, testing for HBV infection that could have warranted for vaccine for negative mothers or for the neonates of positive mothers has not been taken with a similar approach. Should this hesitancy to uptake vaccine persists, the initial global health sector strategy by the World Health Organization to get rid of hepatitis B virus infection on or before 2030 as a major global health threat16 will be hampered and fail to reach its goal.
Again, this present study revealed the age of the expectant mothers to be a predictor of hepatitis B virus infection vaccine hesitancy at bivariate level, where younger aged pregnant women or women between the ages of 18 and 28 were more likely to hesitate getting vaccinated compared to older expectant mothers who aged 29 and above (COR = 3.83, 95% CI = 0.92–15.89). However, at the multivariable logistic model, age ceased to be a significant predictor of vaccine hesitancy. Similar studies like that of21,22,30,31 in contrast with our study reported an independent association between age and uptake of maternal health services including HBV vaccine uptake. This could be best explained by saying that perhaps older women are adequately informed about HBV infection and vaccination compared to their counterparts and to better explain this, evidently from this study regarding the information adequacy about the infection, older women displayed higher levels of knowledge and behavioral skills compared to the younger aged women. The reports from similar studies within sub-Saharan Africa that employed a relatively larger sample size than ours tend to be in contrast to the report from our findings, where a negative association is demonstrated between being older and up-taking health-care services like vaccination.32,33
Furthermore, another demographic variable found to be predicting hesitancy of vaccine among the pregnant women in our study is educational attainment. It was demonstrated that respondents with above secondary education are likely to uptake HBV vaccine compared to the pregnant women who had secondary educational attainment and below. This could imply that having above secondary education predisposes the women to get themselves more informed about HBV infection and vaccination, it may also have shaped their perception of the risk of HBV infection to be positive and also provide them with the necessary behavioral skills needed to engage in uptaking the required doses of vaccination as it was also obviously observed from this study that respondents with above secondary education consistently displayed better score for knowledge of HBV infection and vaccination, perception or risk and vaccination uptake as well as the behavioral skills towards the prevention behaviors which include vaccination. A similar cross-sectional but pilot study conducted among pregnant women in Nigeria reported a contrasting finding regarding educational attainment and vaccination uptake,24 where having higher educational attainment was observed to be associated significantly with vaccine hesitancy among the pregnant women. Another study with such a report not in line with our study is that of Katamba et al,21 where women’s education is not a predictor of vaccine uptake or hesitancy. In line with our present findings, studies conducted in West Africa34,35 showed a significant association between women’s educational attainment and vaccination uptake, although, their target population specifically was not expectant mothers that were employed in our study. However, this finding implies that interventions directed towards improving the uptake of HBV vaccine should focus more on women of lower educational attainment. Additionally, a negative significant association was observed between the marital status of the respondents and vaccine hesitancy where there is a 53% reduction in the odds of vaccine hesitancy among unmarried respondents compared to the married respondents. This implies that unmarried pregnant women were 2.1 times more likely to get vaccinated compared to the married expectant mothers. The finding from this study opposes the reports of no significant association observed between marital status and vaccine uptake in the study conducted by.24,28 Hence, intervention to promote vaccine uptake should pay more attention to married women in this endemic setting.
In addition to the demographic predictors of vaccine hesitancy, knowledge and behavioral skills were also significantly associated with vaccine hesitancy among the respondents. This study, having been premised on the information motivation and behavioral skills model (IMB) that proposes that, to the extent where individuals are informed adequately about a disease condition or health problem and they display a positive perception towards preventing themselves because of the risk, in other words, they are motivated to act positively towards prevention as well as possessing the relevant or good behavioral skills to embark on prevention behaviors, they are likely going to adopt prevention practices such as uptake of vaccine compared to when it is otherwise.36 We found an average but inadequate knowledge about the nature of hepatitis B virus infection, cause, transmission, risk factors and the prevention via vaccination among our respondents with a percentage mean score of 52.4%. Further, an increase in knowledge score is associated with a decrease in the odds of vaccine hesitancy among the expectant mothers and as their level of knowledge about HBV infection increases, the odds of vaccinating against HBV infection is 1.27 times higher. This is an implication that when knowledge decreases, the odds of hesitating vaccine uptake will increase. This finding is similar to the report from a study conducted in South Sudan,37 although it was conducted among health-care workers, another study that linked being adequately informed about hepatitis B virus infection to the uptake of vaccination is that of Eleje et al24 conducted in Nigeria. This link is proof that not being knowledgeable about HBV infection will predispose the pregnant women to the risk of HBV infection and the prevention scale-up through vaccination will be affected if targeted health education is not initiated. Findings from this study would guide the educational intervention for this vulnerable group since it can be observed that the target should be women of younger age group, who possess secondary educational attainment or below and who are unemployed due to the fact that they consistently displayed the lowest score for knowledge about hepatitis B virus infection and vaccination.
Amazingly, where a general average level of perception (53.6%) was displayed by the respondents and no significant difference exists in the score on perception among the pregnant women who displayed hesitancy towards vaccine uptake (17.4) and those who get vaccinated (18.5), it was realized that there is a significant independent positive association between perception and vaccine hesitancy at the multivariable model. Evidently, the odds of vaccine hesitancy are 1.1 times higher as the perception of risk towards HBV infection increases. This could denote that as they perceived HBV infection to be risky with increasing knowledge and behavioral skills, they do not trust the effectiveness of the vaccine or they perceived their likelihood of being infected to be low and vaccine uptake might be deemed unnecessary. Hence, efforts should be directed towards educating the expectant mothers on the effectiveness and the outcome expectancy of HBV infection vaccine. Contrary to this finding, studies like those conducted in Uganda among pregnant women21,28 reported a positive association between perception of hepatitis B virus infection risk and vaccine uptake. However, in agreement with this study that reported a positive association with reluctance to uptake vaccine, a study conducted in Asia by38 reported a negative association between perception of risk and engagement in prevention practice. Despite this positive predicting relationship between perception and vaccine hesitancy reported in our study, targeted health education remains very important considering the fact that the scores on perception across the level of education and the employment status of the women significantly varied and could put them at the risk of HBV infection if actions are not directed towards clearing the misperception among the younger aged women and unemployed women. Furthermore, our study also reported behavioral skills as a predictor of vaccine hesitancy and the odds of hesitating vaccine uptake among the respondents decrease by 12% as the level of behavioral skills increases. Generally, the expectant mothers displayed good behavioral skills ( =12.88, SD = 4.91) for initiating prevention behavior ranging from their self-efficacy, outcome expectancy, perceived severity, and perceived barriers when measured on a rating scale of 33-points. The negative association reported between behavioral skills and reluctance to uptake vaccine denotes that when women possess low confidence in themselves towards embarking on the prevention of HBV infection, their likelihood of hesitating vaccine will increase. Contrarily, when they demonstrate good behavioral skills towards adopting HBV prevention, the odds of vaccination will be 1.1 times higher. This is an indication that behavioral skills interact with intermediate variables like knowledge and perception among others to translate to better prevention behavior as explained by the information-motivation-behavioral skills model and supported by the correlation analysis employed in this study to test the linear relationship between the constructs of the model. Therefore, efforts should lay emphasis on improving the knowledge and perception of the married women and women with lower educational attainment to better shape their behavioral skills towards embarking on preventive behaviors such as vaccination that will translate to positive health outcomes for them and their unborn babies. To the best of our knowledge, this is the first study conducted among expectant mothers in Kampala to assess the predictors of vaccine hesitancy and evidence from this study has been able to justify the probable dynamics of the infection progress in obstetric population on the account of their demographic information and the disease-specific information. Hence, it will be useful in informing hepatitis B prevention policy among pregnant women in this highly endemic setting.
=12.88, SD = 4.91) for initiating prevention behavior ranging from their self-efficacy, outcome expectancy, perceived severity, and perceived barriers when measured on a rating scale of 33-points. The negative association reported between behavioral skills and reluctance to uptake vaccine denotes that when women possess low confidence in themselves towards embarking on the prevention of HBV infection, their likelihood of hesitating vaccine will increase. Contrarily, when they demonstrate good behavioral skills towards adopting HBV prevention, the odds of vaccination will be 1.1 times higher. This is an indication that behavioral skills interact with intermediate variables like knowledge and perception among others to translate to better prevention behavior as explained by the information-motivation-behavioral skills model and supported by the correlation analysis employed in this study to test the linear relationship between the constructs of the model. Therefore, efforts should lay emphasis on improving the knowledge and perception of the married women and women with lower educational attainment to better shape their behavioral skills towards embarking on preventive behaviors such as vaccination that will translate to positive health outcomes for them and their unborn babies. To the best of our knowledge, this is the first study conducted among expectant mothers in Kampala to assess the predictors of vaccine hesitancy and evidence from this study has been able to justify the probable dynamics of the infection progress in obstetric population on the account of their demographic information and the disease-specific information. Hence, it will be useful in informing hepatitis B prevention policy among pregnant women in this highly endemic setting.
Conclusion
The findings reported a drastically high degree of HBV infection vaccine hesitancy among the expectant mothers which is found to be predicted positively on the one hand, by the respondents’ educational attainment and perception while on the other hand associated negatively with HBV-specific knowledge and behavioral skills. This necessitates targeted health education during health campaigns and antenatal visitations with much attention on married women with lower educational attainment in order to improve their knowledge of HBV infection and vaccination that will in turn positively shape their perception and behavioral skills towards satisfactory uptake of HBV preventive services like screening and vaccination.
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; ANOVA, analysis of variance; DNA, deoxy-ribonucleic-acid; HBV, hepatitis B virus; LHREC, Lubaga Hospital Research Ethical Committee; SPSS, Statistical Package for Social Sciences, UPHIA, Population-based HIV Impact Assessment; WHO, World Health Organization.
Data Sharing Statement
The data spreadsheet used for the manuscript is available upon request on reasonable grounds from the corresponding author.
Acknowledgment
We express our profound gratitude to the public health department of Lubaga hospital for their support throughout the period of the study at the Antenatal clinic.
Funding
The authors received no external funding for this study.
Disclosure
The authors declared no conflicts of interest in relation to this work.
References
1. World Health Organization, 2017. WHO Guidelines on Hepatitis B and C Testing. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO; 2017.
2. World Health Organization. Hepatitis B; 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b.
3. World Health Organization. Hepatitis B Factsheet no 204. Geneva; 2015. Available from: http://www.who.int/mediacentre/factsheets/fs204/en/.
4. Pungpapong S, Kim WR, Poterucha JJ. Natural history of HBV infection: an update for clinicians. Mayo Clin Proced. 2007;82:967–975. doi:10.4065/82.8.967
5. Miller WC, Shao JF, Weaver DJ, Shimokura GH, Paul DA, Lallinger GJ. Seroprevalence of viral hepatitis in Tanzanian adults. Trop Med Int Health TM IH. 1998;3:757–763. doi:10.1046/j.1365-3156.1998.00289.x
6. Matee MIN, Magesa PM, Lyamuya EF. Seroprevalence of human immunodeficiency virus, hepatitis B and C viruses and syphilis infections among blood donors at the muhimbili national hospital in dar es salaam, Tanzania. BMC Public Health. 2006;6:21. doi:10.1186/1471-2458-6-21
7. Stark K, Poggensee G, Höhne M, Bienzle U, Kiwelu I, Schreier E. Seroepidemiology of TT virus, GBC-C/HGV, and hepatitis viruses B, C, and E among women in a rural area of Tanzania. Journal of Medical Virology. 2000;62:524–530. PMID: 11074483. doi:10.1002/1096-9071(200012)62:4<524::AID-JMV19>3.0.CO;2-N
8. Mueller A, Stoetter L, Kalluvya S, et al. Prevalence of hepatitis B virus infection among health care workers in a tertiary hospital in Tanzania. BMC Infect Dis. 2015;15. doi:10.1186/s12879-015-1129-z
9. World Health Organization. Global and Country Estimates of immunization coverage and chronic HBV infection. Geneva; 2017. Available from: http://whohbsagdashboard.com/#global-strategies.
10. Umare A, Seyoum B, Gobena T, Haile Mariyam T. Hepatitis B virus infections and associated factors among pregnant women attending antenatal care clinic at deder hospital, Eastern Ethiopia. PLoS One. 2014;11:e0166936.
11. Mbaawuaga EM, Enenebeaku MNO, Okopi JA, et al. Hepatitis B virus (HBV) infection among pregnant women in Makurdi, Nigeria. Afr J Biomed Res. 2008;11:155–159.
12. Atilola G, Tomisin O, Randle M, et al. Epidemiology of HBV in pregnant women, South West Nigeria. J Epidemiol Glob Health. 2018;8(3–4):115–123. doi:10.1016/j.jegh.2018.09.002
13. Ministry of health Uganda. World hepatitis day 2018: report 2016 Uganda population-based HIV impact assessment (UPHIA) Survey: press statement on the progress of implementation of hepatitis b vaccination program in Uganda. Hon. Sarah Opendi, Minister of state for health (general duties); 2018.
14. Health MO. Ministerial Statement by the Hon. Minister of Health to parliament on the progress of the control of the Hepatitis B virus in Uganda; 2015.
15. Dionne-Odom J, Tita AT, Silverman NS. Medicine SfM-F. #38: hepatitis B in pregnancy screening, treatment, and prevention of vertical transmission. Am J Obstet Gynecol. 2016;24(1):6–14. doi:10.1016/j.ajog.2015.09.100
16. World Health Organization. Global health sector strategy on viral hepatitis: towards ending viral hepatitis, 2016–2021; 2016. Available from: http://apps.who.int/iris/bitstream/10665/246177/1/WHO-HIV2016.06-eng.pdf?ua=1.
17. Bayo P, Ochola E, Oleo C, et al. High prevalence of hepatitis B virus infection among pregnant women attending antenatal care: a cross-sectional study in two hospitals in northern Uganda. BMJ Open. 2014;4:e005889. doi:10.1136/bmjopen-2014-005889
18. Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection. A systematic review of data published between 1965 and 2013. Lancet. 2015;386:1546–1555. doi:10.1016/S0140-6736(15)61412-X
19. World Health Organization. Introduction of hepatitis B vaccine into childhood immunization services: management guidelines, including information for health workers and parents. In: Department of Vaccines and Biologicals. Geneva: World Health Organisation; 2001.
20. Goldstein ST, Zhou F, Hadler SC, et al. A mathematical model to estimate global hepatitis B disease burden and vaccination impact. Int J Epidemiol. 2005;34(6):1329–1339. doi:10.1093/ije/dyi206
21. Katamba PS, Mukunya D, Kwesiga D, et al. Prenatal hepatitis B screening and associated factors in a high prevalence district of Lira, Northern Uganda: a community based cross sectional study. BMC Public Health. 2019;19:1004. doi:10.1186/s12889-019-7344-6
22. Omotowo I, Meka I, Ijomu U, et al. Uptake of hepatitis B vaccination and its determinants among health care workers in a tertiary health facility in Enugu, south-east, Nigeria. BMC Infect Dis. 2018;18(1):288. doi:10.1186/s12879-018-3191-9
23. Kumar A, Khuwaja AK, Khuwaja AM. Knowledge practice gaps about needle stick injuries among healthcare workers at tertiary care hospitals of Pakistan. J Ayub Med Coll Abbottabad. 2012;24(3–4):50–52.
24. Eleje GU, Akaba GO, Mbachu II, et al. Pregnant women’s hepatitis B coverage in Nigeria: a national pilot cross-sectional study. Ther Adv Vaccines Immunother. 2021;9:25151355211032595. doi:10.1177/25151355211032595
25. Andersson MI, Rajbhandari R, Kew MC, et al. Mother-to-child transmission of hepatitis B virus in sub-Saharan Africa: time to act. Lancet Glob Health. 2015;3(7):e358–e9. doi:10.1016/S2214-109X(15)00056-X
26. Kish L. Sampling organizations and groups of unequal sizes. Am Sociol Rev. 1965;30(4):564–572. doi:10.2307/2091346
27. Nankya-Mutyoba J, Aizire J, Makumbi F, Atuyambe L, Ocama P, Kirk G. Correlates of hepatitis B awareness and disease-specific knowledge among pregnant women in northern and central Uganda. Hepatol Med Policy. 2018;3:14. doi:10.1186/s41124-018-0043-6
28. Ssekamatte T, Mukama T, Kibira SPS, et al. Hepatitis B screening and vaccination status of healthcare providers in Wakiso district, Uganda. PLoS One. 2020;15(7):e0235470. doi:10.1371/journal.pone.0235470
29. Gedefaw A, Muluken A. Hepatitis B vaccine Knowledge and vaccination status among health care workers of Bahir Dar City Administration, Northwest Ethiopia: a cross sectional study. BMC Infect Dis. 2015;15:30–35. doi:10.1186/s12879-015-0756-8
30. Akowuah JA, Agyei-Baffour P, Awunyo-Vitor D. Determinants of antenatal healthcare utilization by pregnant women in third trimester in Peri-urban Ghana. J Trop Med. 2018;12(1):52.
31. Godha D, Gage AJ, Hotchkiss DR, Cappa C. Predicting maternal health care use by age at marriage in multiple countries. J Adolesc Health. 2016;58(5):504–511. doi:10.1016/j.jadohealth.2016.01.001
32. Owili PO, Muga MA, Chou Y-J, Hsu Y-HE, Huang N, Chien L-Y. Family structure types and adequate utilization of antenatal care in Kenya. Fam Community Health. 2016;39(3):188–198. doi:10.1097/FCH.0000000000000109
33. Arthur E. Wealth and antenatal care use: implications for maternal health care utilisation in Ghana. Heal Econ Rev. 2102;2(1):14. doi:10.1186/2191-1991-2-14
34. Greenaway ES, Leon J, Baker DP. Understanding the association between maternal education and use of health services in Ghana: exploring the role of health knowledge. J Biosoc Sci. 2012;44(6):733–747. doi:10.1017/S0021932012000041
35. Yar’Zever I, Said I. Knowledge and barriers in utilization of maternal health care services in Kano state, northern Nigeria. Eur J Biol Med Sci Res. 2013;1(1):1–14.
36. Fisher JD, Fisher WA. Theoretical approaches to individual level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV Prevention. New York: Kluwer Academic/Plenum; 2000.
37. Alege JB, Gulom G, Ochom A, Kaku VE. Assessing level of knowledge and uptake of hepatitis b vaccination among health care workers at Juba teaching hospital, Juba City, South Sudan. Adv Prev Med. 2020;2020:11. doi:10.1155/2020/8888409
38. Lee SH, Ham EM. The relationship between the optimistic bias about cancer and cancer preventive behavior of the Korean, Chinese, American, and Japanese adult residing in Korea. J Korean Acad Nurs. 2010;40(1):52–59. doi:10.4040/jkan.2010.40.1.52
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

