Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Predictors of Adherence to Self-Care Behavior Among Patients with Diabetes at Public Hospitals in West Ethiopia
Authors Oluma A , Mosisa G , Abadiga M , Tsegaye R , Habte A , Abdissa E
Received 12 June 2020
Accepted for publication 20 August 2020
Published 18 September 2020 Volume 2020:13 Pages 3277—3288
DOI https://doi.org/10.2147/DMSO.S266589
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Adugna Oluma, Getu Mosisa, Muktar Abadiga, Reta Tsegaye, Ashenafi Habte, Eba Abdissa
School of Nursing and Midwifery, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Correspondence: Adugna Oluma Tel +251917814582
Email [email protected]
Background: Diabetes is a typical chronic disease that needs integrated and multifaceted approaches. Self-care practices are fundamental to achieve good blood glucose control and prevent long-term complications. Therefore, the aim of the study was to determine the level and predictors of adherence to self-care behavior among patients with diabetes on follow-up at public hospitals of western Ethiopia.
Patients and Methods: The cross-sectional study design was employed on a sample of 423 diabetic patients on follow-up at public hospitals of western Ethiopia. A systematic random sampling method was employed. The data were entered into Epi data version 3.1 and exported into Statistical Package for the Social Sciences window version 24 for analysis. All variables significant at p-value < 0.05 in the bivariable were entered in multivariate regression analysis. Backward stepwise goodness of fit was used to ascertain the suitable variables in multiple linear regression analysis. Finally, multivariate linear regression analysis with adjusted B, CI at 95%, and the significance level was set at p < 0.05. All predictive variables were reported in terms of adjusted R2.
Results: The overall mean and standard deviation of adherence to self-care behavior was 23.09 ± 6.55. Among the study participants, 42.70% had good self-care behavior. Self-efficacy (B=0.106, p< 0.001), home blood glucose test (B=0.075, p< 0.001), exercise per week (0.035, P< 0.002), meal planning (B=0.039, P< 0.001), dietary restriction (B=0.077, P< 0.001), duration of diabetes< 4 years (B=0.030, P< 0.013), non-pharmacological intervention (B=0.055, P< 0.011), and good appetite (B=0.039, P< 0.045) were significant variables associated with adherence to self-care behaviors.
Conclusion: The overall level of adherence to self-care behavior was low. Therefore, we recommended that it is better if the national health policymaker focused on dietary management modality that engages patients’ behavior change to develop self-care practices and closely monitoring of glucose level. Also, we recommended an additional longitudinal study incorporating a qualitative study that focused on behavioral changes.
Keywords: diabetes mellitus, adherence, self-care behavior, Ethiopia
Plain Language Summary
Globally, an estimated prevalence of diabetes was around 463 million adults (20–79 years) with projection rising to 700 million by 2045 years. In the context of Ethiopia, its prevalence is rapidly increasing from 3.80–5.20%. An increment in the prevalence of diabetes is related to an increase in modifiable risk factors such as unhealthy dietary patterns, lack of physical exercise, excess body weight, and sedentary lifestyle. About 95.00% of diabetes treatment relies on self-care behaviors. The magnitude of adherence to physical activity was 74.00%, adherence to self-monitoring blood glucose was 16.50% and adherence to diet management was 37.00%. Adherence is a primary determinant for the effectiveness of treatment and poor adherence attenuates optimum clinical benefit. In the current study, 42.70% of the participants had good adherence to self-care behavior and the remaining 57.30% had poor adherence to self-care behavior. In particular, 52.50% were adherent to dietary, 66.80% adherent to glucose control, and about 63.10% were adherent to exercise. High self-efficacy, home blood glucose test, exercise per week, having meal planning, having dietary restriction, duration of diabetes < years, non-pharmacological treatment, and good appetite were significant variables associated with adherence to self-care behaviors. Among associated factors, high self-efficacy was the strongest variable related to adherence to self-care behaviors among diabetes patients. The national health policymaker should focus on management modality that engages patients’ behavioral change to develop self-care practices and closely monitoring of glucose level.
Background
Diabetes mellitus is a group of metabolic disorders characterized by the presence of hyperglycemia.1 The global diabetes prevalence in 2019 is estimated at 463 million (20–79 years) adults, with this projection probably rising to 700 million by 2045years. Approximately about 79.00% of adults with diabetes were living in low and middle-income countries. In context of Ethiopia, its prevalence is rapidly increasing from 3.80–5.20%.2
Uncontrolled diabetes mellitus considerably affects the individuals’ quality of life, social interaction, and economic product, costing millions of health care budgets and as a whole that can lead to poor health outcomes.3
Worldwide a radical increment in prevalence of diabetes was related to an increased prevalence of modifiable risk factors such as unhealthy dietary patterns, lack of physical exercise, excess body weight, and sedentary lifestyle. These factors are highly responsible for the current increasing incidence of diabetes.4
A study conducted by Zhou et al revealed about (95.00%) of diabetes treatment relies on self-care behaviors which were usually provided by their families. This finding indicated diabetic patients must adjust their behavior particularly dietary and physical activity concurrently with prescribed treatments.5
The study showed that self-care is an important part of treating diabetes. Diabetes’s self-care behaviors are a dynamic and cognitive practice that includes healthy eating, physical activity, monitoring blood glucose, compliance with medication, and healthy coping skills. A sentimental intervention seeks to enhance adherence self-care by providing emotional support and encouragement for recent diet and exercise intervention through lifestyle “tutor” to help people adhere to the behavioral changes.6
Adherence to self-care behaviour is a primary determinant for effectiveness of treatment as good adherence improves healthy lifestyles, through diet modification, increased physical activity, non-smoking and safe sexual behaviour. However, poor adherence to self-care behaviour attenuates optimum clinical benefit and also affects secondary prevention and disease treatment interventions.7
Researchers have conducted a variety of studies to investigate the magnitude of adherence to self-care behavior in different settings. The majorities of these findings were explored through dimensions of self-care components including adherence to physical activity (74.00%), adherence to self-monitoring blood glucose 16.5%, adherence to diet management practice (37.00%).6,8
A study conducted in India indicated that only (23.00%) of study participants were performing glucose monitoring 115 at home as frequently as recommended.9 Study conducted by Nyunt et al showed that around (62.00%) patients had self-efficacy and (30.80%) of them practiced good self-care behavior of diabetes self-management.10 Another study conducted in northern California, the United States showed that about (67.00%) of patients with type 2 diabetes did not perform self-monitoring of blood glucose.11
Another study conducted in northern California, United States showed that about (67.00%) of patients with type 2 diabetes did not perform self-monitoring of blood glucose. Similar findings were reported in India that only (23.00%) of study participants were performing glucose monitoring at home as frequently as recommended.
Effective diabetes care requires a comprehensive approach for patients’ behavioral changes in terms of healthy lifestyle such as physical activity, healthy eating, tobacco cessation, weight management, taking medication, self-monitoring of glucose, as well as prevention of acute and chronic diabetes complications.12,13
A previous study indicated patients’ age, gender, education, doctor–patient relationships, psychological stress, social support, overweight, and obesity were factors associated with adherence to self-care behaviors.14
A study conducted in Debre Tabor general hospital showed that dietary modification was the underpinning management of T2DM. However, this finding revealed common barriers to dietary adherence including socioeconomic status, duration of disease, lack of diabetes knowledge, cost of a healthy diet, and poor communication with healthcare providers.15
Several studies showed that training on self-care behaviors, drug use, self-monitoring of blood sugar, diet, exercise, and foot care, sufficient knowledge about self-care in diabetes was associated with lower HbA1c level.16–19
The requirement of adherence to diabetes self-care behavior such as adherence to medication, exercise, diet, and self-monitoring of blood glucose familiarize diabetes patients to avoid, and free from fears that they have diabetes. This robust routine diabetes self-management leads to good glycaemic control and subsequently reduces the risk of diabetic complications.20
Furthermore, studies conducted in varieties of areas showed adherence rates for medication for diabetes vary between 36–93%, adherence with oral glucose lowering drugs 61–85%, and the adherence to anti diabetic drug therapy and self-management practice showed that about two third of patients are not adherent. Adherence to prescribed medication is crucial to reach metabolic control whereas non-adherence is associated with higher HbAIc and cholesterol, levels.21–24
Therefore, adherences to self-care through behavior changes are the cornerstone particularly for the management of type II diabetes. In the context of the western part of Ethiopia, there was limited study conducted regarding adherence to self-care behaviors among patients with chronic diseases specifically diabetes. Thus, this study will fill this existing gap and contribute to minimizing the adverse effect of prolonged uses of medications through customizing self-arranged routine diabetes management.
Patients and Methods
Study Design
The institutional-based cross-sectional study design was employed.
Study Setting
The study was conducted in multi-facility-based public hospitals found in western Ethiopia from January 20-March 20, 2020. The public hospitals were selected randomly by lottery method from all public hospitals found in western Ethiopia. The four selected hospitals were Wollega university referral hospital and Nekemte specialized hospitals which are found in Nekemte town at a distance of 331km from Addis Ababa. Nekemte town has a latitude and longitude of 9º5ʹN36º33ʹE and an elevation of 2088 meters. Ghimbi general hospital is found in Gimbi town West Wollega Zone. It has a latitude and longitude of 9º10ʹN35º50ʹE with an elevation between 1845 and 1930 meters above sea level. Shambu hospital is found in Shambu town Horo Guduru Wollega Zone. It has an elevation of 2503 meters above sea level. The selected public hospitals were serving as primary service, general services, and specialized level of services for more than a total population of 11 million for the western part of Ethiopia.
Study Population and Samples
First, we selected randomly four hospitals by lottery method from all public hospitals found in western Ethiopia. After the selection of hospitals, we took the sampling frame from a medical record of the diabetic patients on follow-up receiving ant diabetic medication from the chronic outpatient department of respective hospitals. Then we calculated a constant k value and included all our potential participants from all selected hospitals. Finally, oral informed consent was provided for all selected participants. The study was conducted on a total of 1280 patients with diabetes on follow-up and receiving diabetic medications. All diabetic patients including type I and II attending selected hospitals were the source population and all the sampled patients with diabetic on follow-up receiving diabetic medication for at least six months and present during data collection period were the study population. All diabetic patients on follow-up with measured A1C ≥7.0% (53mmol/mol) were included and those taking anti-diabetic medication for less than six months were excluded from the study.
Sample Size Determination and Sampling Techniques
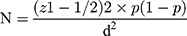
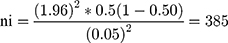
The sample size of the study was calculated using the formula for estimation of a single population proportion with the assumptions of 95% confidence level (CL), marginal error (d) of 0.05. Since the previous study conducted in Ethiopia was emphasized on type II diabetes for the considering variation when both types were conducted, we considered a population proportion of 0.50 (50%).
Thus, by adding a non-response rate of 10% and using the correction formula; the final sample size was 423 of people living with diabetes mellitus and treated with anti-hyperglycemic medication were enrolled in the study. Study participants were selected by using systematic random sampling techniques from each hospital.
Data Collection Tool and Procedures
Data collection tools consist of three-part questionnaires: The first part consists of demographic questions developed by investigators. Participants’ height and weight were measured as part of the physical examination. Body mass index (BMI) was classified as <18.50kg/m2 (underweight), 18.50–24.90kg/m2 (normal weight), 25–29.90 kg/m2 (overweight) and that of ≥30kg/m2 defined as obesity based on the World Health Organization criteria.
The second part measures self-care behaviors: The revised version of the Summary of Diabetes Self-Care Activities (SDSCA) questionnaire taken from the previous study originally developed by Schmitt et al25 was used to measure participants’ self-reported frequency of adhering to self-care behaviors. The SDSCA assesses participants’ frequency of engaging in diabetes self-care behaviors in terms of thirteen items with three dimensions including glucose management (4 items), physical activity (4 items), and dietary control (5 items). Six items are formulated positively and the remaining seven negatively stated were reversed. Participants were asked to indicate the number of days they engaged in each of the self-care behaviors for the past 7 days. The greater the number of days reported for behavior the better the self-care. The scale was measured on a 4-point Likert scale that starts from 0= does not apply to me, 1= applies to me to some degree, 2= applies to me to a considerable degree, and 3=applies to me very much and the higher score indicated more effective self-care. The reliability of the SDSCA was reported with Cronbach's alpha =0.856 which was acceptable.
The third part questionnaire was self-efficacy-related questions collected via 8 modified questions from the diabetes mellitus self-efficacy scale (DMSES) adapted from the previous study originally developed by Wellston et al.26 The responses were rated on a 5-point Likert scale: “1=not confident, 2=not very confident, 3=confident half the time, 4=usually confident, 5=always confident". The lower score indicated poor/fair self-efficacy and higher score high self-efficacy. The reliability of the diabetes mellitus self-efficacy scale (DMSES) was reported with Cronbach's alpha =0.880hwhich was acceptable. A close-ended interviewer-administered structured questionnaire was distributed to participants by trained data collectors. Four trained Bsc nurses collectors and two supervisors were employed for consecutive two months.
Operational Definition
Adherence: Defined as the degree to which a patient follows a predetermined set of behaviors or actions including taking medication, following a diet, executing lifestyle changes to care for diabetes on a daily basis.27
Self-care behaviors: Refers to self-care activities such as following a diet plan, avoiding high-fat foods, regular physical activity, self-glucose monitoring, administration of medication engaged for the past 7 days which measured by Summary of Diabetes Self-Care Activities.28
Poor self-care behaviors: Those patients’ adherence to self-care behaviors scored below the mean of self-care behavior items
Good Self-care behaviors: Those patients’ adherence to self-care behaviors scored above the mean of self-care behavior items
Self-efficacy: “The diabetes patients’ belief and judgment of their capability of carrying out diabetes self-management activities” (Bandura, 1994)
Poor self –efficacy: Those patients’ self-efficacy scored below the mean of self-efficacy scores.
High self –efficacy: Those patients' self-efficacy scored above mean of self-efficacy scores.
Reliability of the Instruments
The sampling adequacy was checked by the Kaiser Meyer Olkin test. For all scales, confirmatory factor analysis was performed to know the adequacy of all instruments (accepted standard >0.5). The intraclass correlation coefficient was used for testing the reliability of scales. Some items were reduced based on the value of the intraclass correlation coefficient using the principal component method, Varimax rotation with Kaiser Normalization at Eigenvalue >1.
As shown below factor analysis for Diabetes self-management tools with Kaiser-Meyer-Olkin Measure of Sampling Adequacy was 0.83 (DF=105, p=00). The rotated component matrix of loading factors showed three dimensions (1, 2 and 3). The total variance explained for the first dimension was 23.44%, the 2nd dimension 39.28% and the third dimension was 57.69%. The overall Cronbach's alpha of the tool was =0.86.
Below was illustrated the factor analysis of the self-efficacy scale with Kaiser-Meyer-Olkin Measure of Sampling Adequacy was 0.86 (DF=28, p=00). The rotated component matrix of loading factors resulted in two dimensions (1 and 2) with total variance explained for the 1st and 2nd dimensions (35.76% 68.76%) respectively. The overall Cronbach’s alpha =0.88 (Table 1).
 |
Table 1 Loading Factor of Diabetes Mellitus Self-Efficacy Scale |
Data Quality Control
All questionnaires adopted in the English language translated into the local language Afan Oromo and then re-translated back into English by experts. A pretest was conducted on 5% of the questionnaire on diabetic patients at Ghimbi Adventist hospital that was outside the actual study setting before data collection. The training was given one day for both data collectors and supervisors. Data were cleaned, coded, and checked for consistency and completeness. A consistency was checked by a double-entry method to improve the quality of the data, and inconsistent entries and responses were crosschecked.
Data Processing and Analysis
Data were cleaned, edited, coded, and entered into Epi data version 3.1 and was exported to SPSS windows version 24 for analysis. Descriptive statistics including, percentage, ratios, frequency distribution, mean and standard deviation, and pie chart was used to describe the data. Normalization of the data was checked using histograms, normal Q-Q, Scatter plot, Shapiro–Wilk’s test, and Durbin-Watson was used to know the homogeneity of variables. Multicollinearity was checked using tolerance and the Variance Inflation Factor (VIF). All variables significant at p-value <0.05 in the bivariable were entered in multivariate regression analysis. Backward stepwise goodness of fit was used to ascertain the suitable variables in multiple linear regression analysis. Finally, multivariate linear regression analysis with adjusted B, CI at 95%, and the significance level was set at p <0.05. All predictive variables were reported in terms of adjusted R2.
Results
Socio-Demographic Characteristics of Participants
A total of four hundred twenty-three participants participated giving a response rate of 94.10%. More than half 210 (52.80%) of the participants were male with a median age of 45 (±15.88SD). The majority of the participants 168 (42.20%) were aged above 50 years followed by 40–49 (24.10%) years. Concerning their ethnicity, the majority of the participants 355 (89.20%) were Oromo with 327 (82.20%) language speakers of Afan Oromo. Nearly half 189 (47.50%) of the respondents were protestant followers followed by 134 (33.70%) were an orthodox believer. Concerning marital status, about 308 (77.40%) were married. Moreover, concerning the educational status majority of the respondents were 109 (27.40%) college/university and about 97 (24.40%) had no formal education. With regard to their occupation, most of them 169 (42.50%) were employees, and about 246 (61.80%) urban indwellers (Table 2).
 |
Table 2 Distribution of Socio-Demographic Characteristics of Diabetes Patients Attending Public Hospitals of Western Ethiopia (N=398) |
Clinical Characteristics of Participants
The study results showed most of the participants (88.20%) were non-smokers. The majority (76.10%) of the respondents had no family history of diabetes. More than half (53.80%) of patients have suffered from diabetes mellitus for less than five years. Of the total of respondents, 68.10% of them had no diabetes-related complications (hypertension, neuropathy, diabetic coma, foot gangrene) and the remaining 31.90% had diabetes-related complications. Approximately three-fourth (74.10%) of the respondents did physical activity per week and nearly half (53.30%) of them test their blood glucose by glucometer at home. The majority (39.40%) of the respondents were overweight (BMI=25-29.90) and they reported that they experienced increased body weight (51.80%). The participants reported that about seventy percent (70.10%) of them had no special diet and 29.90% of them had a self-arranged special diet. The majority of the patients 285 (71.60%) had been taking a combination of oral hypoglycemic agents and insulin and the remaining had been taking insulin injection and non-pharmacological treatment (23.40% and 5.00%, respectively) (Table 3).
 |
Table 3 Proportion of Clinical Characteristics of Diabetes Patients Attending Public Hospitals of Western Ethiopia (N=398) |
Level of Adherence to Self-Care Behavior
Descriptive statistics were conducted to find out the mean and standard deviation of the adherence to self-care behaviors. The summary of the diabetes self-care scale was measured by thirteen questionnaires with minimum zero (0) and a maximum score of sixty-three (63) for the previous seven days. After construct validity of factor analysis performed three items were removed due to low coefficient. Therefore, three dimensions extracted to determine the magnitude of adherence to self-care with the mean, and standard deviation of dietary adherence 7.32±3.39SD (52.50%), adherence to glucose control 9.30±2.29SD (66.80%), and adherence to exercise 6.46±2.75SD (63.10%). The overall mean and standard deviation of adherence to self-care behavior was 23.09 ±6.55. The overall level of adherence to self-care behavior was classified as good and poor adherence to self-care behaviors using average mean. The average score above the mean indicates good adherence to self-care behavior (42.70%) and below the mean were poor adherence self-care behavior 57.30% (Figure 1).
 |
Figure 1 Level of adherence to self-care behavior among patient with diabetes on follow-up at public hospitals of West Ethiopia, 2020. |
Assumption of Normality Analysis Result of Study Variables
A Shapiro–Wilk’s test (P>0.05) and visual inspection of their histograms, normal Q-Q plots and scatter plot showed that adherence to self-care behavior was approximately normally distributed for the following variables at 95% CI: blood glucose testing at home with skewness of 0.311 (SE=0.201) and kurtosis of 0.140 (SE=0.399), taking a special diet at with skewness of −0.215 (SE=0.512) and kurtosis of −0.805 (SE=0.992), exercising physical activity per week with skewness of 0.483 (SE=−0.580) and kurtosis of −0.316 (SE=1.121), good appetite with skewness of −0.153 (SE=0.217) and kurtosis of −0.197 (SE=0.450), self-efficacy with skewness of 0.162 (SE=−0.166) and kurtosis of 0.029 (SE=0.330), dietary restriction with skewness of −0.067 (SE=0.564) and kurtosis of −0.632 (SE=1.091), presence of meal planning with skewness of −0.109 (SE=0.414) and kurtosis of −0.078 (SE=0.809), nonsmoker with skewness of −0.396 (SE=0.414) and kurtosis of −0.624 (SE=0.809), and non-pharmacological management with skewness of −0.482 (0.550) and kurtosis of −0.670 (1.063).
Bivariable Linear Regression Analysis
Simple linear regression analysis was done in order to determine how much each independent variable was associated with adherence to self-care behaviour. In simple linear regression analysis, occupational status and residences were significant variables to adherence to self-care behaviour. Clinical variables such as self efficacy, treatment types, special diet, exercise per week, blood glucose test at home, description of appetite, types of meal planning, dietary restriction, smoking status were significant variables associated with adherence to self-care behaviour (Table 4).
 |
Table 4 Bivariable Linear Regression Analyses of Factors Associated with Adherence to Self-Care Behaviour Among Diabetic Patient on Follow-Up at Public Hospitals of West Ethiopia, 2020 (N=398) |
Multivariable Linear Regression Analysis
Multivariate linear regression analysis was conducted to determine the best combination of factors for predicting adherence to self-care behaviour. So Multivariable linear regression model with stepwise elimination was used to extract predictors that best predict adherence to self-care behaviour. In the final model of multivariable regression self efficacy, home blood glucose test, exercise per week, meal planning, dietary restriction, duration of diabetes, types of treatment and description of appetite were significant variables associated with adherence to self-care behaviors. Therefore, a unit increases in high self efficacy increases adherence to self-care behaviour by 10.60% (B=0.106, p<0.00) when compared to poor self efficacy, a unit increases in home blood glucose test increases adherence to self-care behaviour by 7.50% (B=0.075, p<0.00) compared to did not test blood glucose at home, a unit increases in exercise per week increases adherence to self-care behaviour by3.50% (0.035, P<0.002), a unit increases in food planning increases adherence to self-care behaviour by 3.9% (B=039, P<0.001), a unit increases in dietary restriction increases adherence to self-care behaviour by 7.7% (B=0.077, P<0.001), a unit increases in duration of diabetes <4 years compared to >8 years increases adherence to self-care behaviour by 3% (B=030, P<0.013), a unit increases in usage of non pharmacological intervention compared with insulin and oral hypoglycemic agent increases adherence to self-care behaviour by 5.5% (B=0.055, P<0.011), and a unit increases in good appetite increases adherence to self-care behaviour by 3.9% compared to poor appetite. In the multivariable regression analysis the final model is significant (F=53.597, P<0.000) and the adjusted R2 =0.524 with Durbin-Watson=1.676. Therefore, overall variance by 52.4% of adherence to self-care behaviour is due to the effect of all predictors as summarized below (Table 5). This indicates that variance by average 47.6% of adherence to self-care behaviour was due to other factors.
 |
Table 5 Multivariable Linear Regression Analyses of Predictors of Adherence to Self-Care Behaviour Among Diabetic Patient on Follow-Up at Public Hospitals of West Ethiopia, 2020 (N=398) |
The final model described as:
Adherence to self-care behaviour= 1.095 + 0.106 (high self efficacy) + 0.075 (home blood glucose test) +0.036 (exercise per week) + 0.039 (meal planning) + 0.077 (dietary restriction) + 0.030 (≤4 years duration of diabetes) + 0.055 (non-pharmacological treatment) + 0.039 (good appetite)
Discussion
The aim of the study was to determine level and predictors of adherence to self-care behaviour among patients with diabetes on follow-up at public hospitals of west Ethiopia.
This finding of the study showed that around 52.5% of diabetic patients were adhered to dietary management. This finding was higher than the result of the study conducted in Debre Tabor hospital which revealed 25.7% of the participants had good adherence towards dietary recommendations. However, this finding was lower than the result of a study conducted in Nigeria in which about67.4% of participants were strictly adhering to dietary treatment. This difference might be related to variation in nutritional habits and improved usage of non-pharmacological intervention among diabetic patients.13,29
In line with a study carried out by Voon Goeler et al found that 60% of the participants performed SMBG once or twice daily which was lower than the result of the current study showed about 66.8% participants adherence to blood glucose monitoring. However, this finding was almost similar with a report in Alexandria which 64.7% had good compliance of blood glucose control. The higher adherence to SMBG practices could probably be attributed to relevant economic improvement to purchase glucometer.30,31
The current study revealed that about 63.1% respondents were adherent to self-care behaviour for exercise. This finding was similar to the result of the study conducted by Park et al which indicated about 63.0% subjects were exercising regularly. This finding was higher than the results of the study conducted by Bonger et al which showed about 46.3% and also systematic review conducted by Mogre et al which indicated about 26.7–69.0% participants adherent to self care practice for exercise. This variation probably related to improved public awareness toward the benefit of physical activity to control chronic diseases including diabetes through weight reduction.6,32,33
The overall prevalence of good adherence to self-care behaviors in this study was 42.7%. This finding was higher than the finding of a study conducted by Ayele; et al found 39.0% of diabetes patients adhered to recommended self‐care practices. However, the current finding was lower than the result of a systematic review and meta-analysis conducted by Ketema et al (49%) and Kassahun et al (50.9%) which revealed the overall prevalence of good diabetes self-care behavior among diabetic patients. This difference might be related to improved awareness regarding self controlling of diabetes.34–36
The study also showed independent predictors of adherence to self-care behaviour such as a unit increase in home blood glucose test increase adherence to self-care behaviour by 7.5% and also a unit increase in exercising per week increases adherence to self-care behaviour by 3.5%. Additionally, a unit increase in food planning increases adherence to self-care behaviour by 3.9%. These findings were similar with study conducted in Ben-Gurion University of the Negev, Israel found that a unit increase in healthful eating plan increased adherence to self-care behaviour by 4.8% and a unit decrease in consumption of fat increase adherence to self-care behaviour by 4.7% and also a unit increase in exercise increased adherence to self-care behaviour by 7.3% as well a unit increase in blood glucose monitoring increases adherence to self-care behaviour by 6.9%. These similarities might reveal that there was public awareness regarding implementation of non-pharmacological management across the globe as patient practices of non-pharmacological intervention were pivotal to control blood glucose level.37
The unit increase in self efficacy increases adherence to self-care behaviour by 10.6% which was similar with study conducted by Karimy et al explained a unit increase in self efficacy increased adherence to self-care behaviour by 3.9%. This similar finding proved that individuals' levels of their confidence toward diabetes management basic to reduce blood glucose.38
Conclusion
The overall prevalence of adherence to self-care behaviour was low. Self efficacy, home blood glucose test, exercise per week, meal planning, dietary restriction, duration of diabetes, types of treatment and description of appetite were significant variables associated with adherence to self-care behaviors. Therefore, based on the findings of the study we recommended that it is better, if the national health policy maker focused on dietary management modality that engages patients’ behavior change to develop self-care practices and closely monitoring of glucose level. Also, we recommended additional longitudinal study incorporating qualitative study that focused on behavioral changes.
Limitations and Strengths of the Study
The Strength of the Study
- Appropriate sampling technique was employed and a high response rate was achieved.
- The data collection tools were anonymously structured.
Limitations of the Study
- The research design is cross-sectional in nature and cannot confirm causality.
- Since this study was the behavioral outcomes recall biases cannot be ruled out.
Study Implications
The findings of the study found important parameters related to adherence to self-care behaviors including self-efficacy, testing blood glucose at home, doing regular physical activities per week, and adherence to dietary restriction. These parameters were important implications of this study for integrating with national health policy making and practicing confidently self-monitoring blood glucose in order to reduce potential complication.
Abbreviations
ADA, American Diabetes Association; BMI, Body Mass Index; DMSES, Diabetes Mellitus Self-efficacy Scale; SDSCA, Summary of diabetes self-Care Activities; HIV, Human Immunodeficiency Virus; SE, Standard Error; SD, Standard Deviation; SMBG, self-monitoring of blood glucose; T2DM, Type Two Diabetes Mellitus; VIF, Variance Inflation Factor.
Data Sharing Statement
The data used during this study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
The study was reviewed and approved by the Institutional Review Boards of Wollega University Ethical review board. The purpose of the study was explained to the medical director and staff of the hospital and permission was obtained. All participants of the study were provided written consent, clearly stating the objectives of the study and their right to refuse. No minors were involved in the study and the consent was obtained from the participants themselves. Moreover, the confidentiality of the information was assured.
Acknowledgment
We would like to acknowledge Wollega University for financial support. We also would like to acknowledge Wollega public hospitals. We are also grateful to the study participants who voluntarily agreed to be interviewed and participated in the study.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
We declare that we have no competing interests.
References
1. World Health Organization. Classification of Diabetes Mellitus. Geneva: Department for Management of Noncommunicable Diseases, Disability, Violence, and Injury Prevention; 2019. License: CC BY-NC-SA 3.0 IGO.
2. International Diabetes Federation. IDF Diabetes Atlas – 9th Edition; 2019. Available from:: www.idf.org/diabetesatlas.
3. Katz ML, Laffel LM, Perrin JM, Kuhlthau K. Impact of type 1 diabetes mellitus on the family is reduced with the medical home, care coordination, and family-centered care. J Pediatr. 2012;160(5):861–867. doi:10.1016/j.jpeds.2011.10.010
4. Cramer JA. A systematic review of adherence with medications for diabetes. J Diabetes Care. 2004;27:1218–1224. doi:10.2337/diacare.27.5.1218
5. Zhou Y, Liao L, Sun M. Self care behaviors of Chinese individuals with diabetes. Exp.The.Med. 2013;5(1):1137–1142. doi:10.3892/etm.2013.945
6. Bonger Z, Shiferraw S, Tariku ZE. Adherence to diabetic self-care practices and its associated factors among patients with type 2 diabetes in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2018;12(1):963–970. doi:10.2147/PPA.S156043
7. World Health Organization. The worlds health report 2002 - Reducing Risks, Promoting Healthy Life. Available from: https://www.who.int/whr/2002/en/.
8. Ali ZH. Health and knowledge progress among diabetic patients after implementation of a Nursing Care Program based on their profile. J Diabetes Metab. 2010;2:121.
9. Rajasekharan D, Kulkarni V, Unnikrishnan B, Kumar N, Holla R, Thapar R. Self-care activities among patients with diabetes attending a tertiary care hospital in Mangalore Karnataka, India. Ann Med HealthSci Res. 2015;5(1):59–64. doi:10.4103/2141-9248.149791
10. Nyunt SW, How Teerakol N, Suwannapong N, Rajatanun T. Self-efficacy, self-care behaviors and glycaemic control among type 2 diabetes patients attending two private clinics in Yangon, Myanmar. Southeast Asian J Trop Med Public Health. 2010;41(4):943–951.
11. Cameron C, Coyle D, Ur E, Klarenbach S.Cost-effectiveness of self-monitoring of blood glucose in patients with type 2 diabetes mellitus managed without insulin. CMAJ. 2010;182(1):28–33. doi:10.1503/cmaj.090765
12. Lustman PJ, Griffith LS, Clouse RE, et al. Effects of alprazolam on glucose regulation in diabetes. Results of double-blind, placebo-controlled trial. Diabetes Care. 1995;18:1133–1139. doi:10.2337/diacare.18.8.1133
13. Karimy M, Araban M, Zareban I, Taher M, Abedi A. Determinants of adherence to self-care behavior among women with type 2 diabetes: an explanation based on health belief model. Med J Islam Repub Iran. 2016;30(1):368.
14. Sorato MM, Tesfahun C, Lamessa D. Levels and predictors of adherence to self-care behaviour among adult type 2 diabetics at Arba Minch General Hospital, Southern Ethiopia. J Diabetes Metab. 2016;7:684. doi:10.4172/2155-6156.1000684
15. Victor Mogre V, Abanga OZ, Tzelepis F, Natalie A, Paul C. Adherence to and factors associated with self-care behaviors in type 2 diabetes patients in Ghana. BMC Endocr Disord. 2017;17(20):2–8. doi:10.1186/s12902-016-0152-4
16. Ayele AA, Emiru KY, Tiruneh AS, Ayele BA, Gebremariam DA, Tegegn GH. Level of adherence to dietary recommendations and barriers among type 2 diabetic patient. Clin Diabetes Endocrinol. 2018;4(21):2–7. doi:10.1186/s40842-018-0070-7
17. Heisler M, Spencer M, Forman J, Robinson C, Shultz C, Palmisano G. Participants assessments of the effects of a community health worker intervention on their diabetes self management and interactions with healthcare providers. Am J Prev Med. 2009;37(6):270–279. doi:10.1016/j.amepre.2009.08.016
18. Hernandez R, Ruggiero L, Riley B, Wang Y, Chavez N, Quinn LT. Correlates of self-care in low-income African American and Latino patients with diabetes. Health Psychol. 2014;33(7):597. doi:10.1037/hea0000043
19. Ortiz LGC, Pérez BDÁ, González ER, Martínez SP, Quirarte NHG, Berry DC. Self-care behaviors and glycemic control in low-income adults in México with type 2 diabetes mellitus. Clin Nurs Res. 2016;25(2):120–138. doi:10.1177/1054773815586542
20. Apini R, Annan R, Apprey C, Boakye AO. Predictors of glycaemic control among Ghanaian type 2 diabetic patients using diabetes self-management approach. Int J Biochem Res Rev. 2018;23(2):1–18. doi:10.9734/IJBCRR/2018/42976
21. Wabe NT, Angamo MT, Hussein S. Medication adherence in diabetes mellitus and self-management practices among type-2 diabetics in Ethiopia. North Am J Med Sci. 2011;3:418–423. doi:10.4297/najms.2011.3418
22. Yusuff KB, Obe O, Joseph BY. Adherence to anti diabetic drug therapy and self-management practices among type-2 diabetics in Nigeria. Pharm World Sci. 2008;30(1):876–883. doi:10.1007/s11096-008-9243-2
23. Demoz GT, Wahdey S, Bahrey D, et al. Predictors of poor adherence to ant diabetic therapy in patients with type 2 diabetes: a cross-sectional study insight from Ethiopia. Diabetol Metab Syndr. 2020;12(1):62. doi:10.1186/s13098-020-00567-7
24. Divya S, Nadig P. Factors contributing to non-adherence to medication among type 2 diabetes mellitus in patients attending tertiary care hospital in south India. Asian J Pharm Clin Res. 2015;8(2):274–276.
25. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. Diabetes self management questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycemic control. Health Qual Life Outcomes. 2013;11(2):138–143. doi:10.1186/1477-7525-11-138
26. Wallston K, Rothman R, Cherrington A. Psychometric properties of the perceived diabetes self-management scale (PDSMS). J Behav Med. 2007;30(1):395–401. doi:10.1007/s10865-007-9110-y
27. Burkhart PV, Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. Available from:. Geneva, Switzerland: World Health Organization; 2003. http://www.who.int/chronic_conditions/adherencereport/en/.
28. Glasgow RE, Strycker LA. Preventive care practices for diabetes management in two primary care samples. Am J Prev Med. 2000;19(1):9–14. doi:10.1016/S0749-3797(00)00157-4
29. Emmanuel OO, Otovwe A. Patterns of adherence to management among patients with type 2 diabetes mellitus in South Region of Nigeria. J Soc Health Diabetes. 2015;3:115–119. doi:10.4103/2321-0656.152808
30. Von Goeler DS, Rosal MC, Ockene JK, Scavron J, De Torrijos F. Selfmanagement of type 2 diabetes: a survey of low-lncome urban Puerto Ricans. Diabetes Educ. 2003;29:663–672. doi:10.1177/014572170302900412
31. Stephani V, Opoku D, Beran D. Self-management of diabetes in sub-Saharan Africa: a systematic review. BMC Public Health. 2018;18(1):1148. doi:10.1186/s12889-018-6050-0
32. Mogre V, Johnson NA, Tzelepis F, Shaw JE, Paul C. A systematic review of adherence to diabetes self‐care behaviors: evidence from low‐ and middle‐income countries. J Adv Nurs. 2019;1–16. doi:10.1111/jan.14190
33. Park SH, Hong SY, Lee JH, Sung AY. Individuals with type 2 diabetes and depressive symptoms exhibited lower adherence with self-care. J Clin Epidemiol. 2004;57(1):978–984. doi:10.1016/j.jclinepi.2004.01.015
34. Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E. Self care behavior among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. PLoS One. 2012;7(4):e35515. doi:10.1371/journal.pone.0035515
35. Ketema BD, Leshargie TC, Kibret DG, et al. Level of self-care practice among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20(309):2–7. doi:10.1186/s12889-020-8425-2
36. Kassahun T, Eshetie T, Gesesew H. Factors associated with glycemic control among adult patients with type 2 diabetes mellitus: a cross-sectional survey in Ethiopia. BMC Endocr Disord. 2016;16(28):2–11. doi:10.1186/s12902-016-0114
37. Tuval ST, Shmueli A, Boehm HI. Adherence to self-care behaviors among patients with type 2 diabetes. ISPOR. 2016;9(1):844–851.
38. Karimy M, Koohestani RH, Araban M. The association between attitude, self-efficacy, and social support and adherence to diabetes self-care behavior. Diabetol Metab Syndr. 2018;10(86):2–7. doi:10.1186/s13098-018-0386-6
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.