Back to Journals » Cancer Management and Research » Volume 14
Predictive Factors Correlated with the Development of Immune-Related Adverse Events in Patients with Non-Small Cell Lung Cancer Treated with Immune Checkpoint Inhibitors
Authors Sonehara K , Tateishi K , Araki T, Komatsu M , Akahane J, Yamamoto H , Hanaoka M
Received 4 November 2021
Accepted for publication 31 December 2021
Published 2 February 2022 Volume 2022:14 Pages 427—435
DOI https://doi.org/10.2147/CMAR.S347852
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Kei Sonehara, Kazunari Tateishi, Taisuke Araki, Masamichi Komatsu, Jumpei Akahane, Hiroshi Yamamoto, Masayuki Hanaoka
First Department of Internal Medicine, Shinshu University School of Medicine, Matsumoto City, Nagano, Japan
Correspondence: Kazunari Tateishi
First Department of Internal Medicine, Shinshu University School of Medicine, 3-1-1 Asahi, Matsumoto City, Nagano, 390-8621, Japan
, Tel +81-263-37-2631
, Fax +81-263-36-3722
, Email [email protected]
Purpose: Similar to the neutrophil-to-lymphocyte ratio and lung immune prognostic index (LIPI), immune-related adverse events (irAEs) were favorable prognostic factors in several studies, for patients with non-small cell lung cancer who received immune checkpoint inhibitors (ICIs). However, few studies have investigated patient characteristics and markers that predict the development of irAEs, and factors predicting the development of irAEs have not been clarified. Thus, the present study aimed to examine the predictive factors correlated with the development of irAEs in non-small cell lung cancer (NSCLC) patients who received anti-programmed cell death protein 1/programmed cell death ligand 1 inhibitor monotherapy.
Patients and Methods: The present study was retrospectively enrolled 113 advanced NSCLC patients who received ICIs between February 2016 and May 2021 and was conducted at Shinshu University Hospital. All patients were divided into two groups according to with or without of irAEs. We compared the clinical findings and laboratory data between the two groups and considered predictive factors correlated with the development of irAEs.
Results: Forty-four (38.9%) patients developed irAEs of any grade. The most common irAEs were hypothyroidism (12.4%), followed by skin rash (7.1%) and interstitial lung disease (7.1%). The survival time in patients with irAEs was significantly more prolonged compared to those without irAEs (median progression-free survival: 6.8 vs 2.1 months, p < 0.001; median overall survival: 25.3 vs 9.6 months, p = 0.001). Multivariate analyses based on logistic regression revealed independent predictive factors that correlated with the development of irAEs to be first-line ICI treatment and a score of 0 or 1 on LIPI.
Conclusion: The present study revealed that lines of immunotherapy and LIPI were correlated with the development of irAEs in NSCLC patients who received ICIs and can help clinicians who manage patients experiencing irAEs receiving ICIs.
Keywords: non-small cell lung cancer, programmed cell death ligand 1 inhibitor monotherapy, immune-related adverse events, lung immune prognostic index, predictive factor
Introduction
The standard treatment for advanced non-small cell lung cancer (NSCLC) has dramatically evolved with the introduction of immune checkpoint inhibitors (ICIs). Anti-programmed cell death protein 1 (PD-1) inhibitors such as nivolumab and pembrolizumab, anti-programmed cell death ligand 1 (PD-L1) inhibitors such as atezolizumab have been currently used in first- or subsequent-line treatment for NSCLC.1–5 As the use of ICIs increases, toxicity associated with ICIs is an important issue. Toxicities due to ICIs are recognized as immune-related adverse events (irAEs). IrAEs develop in various organ of the body by promoting the activation and expansion of T cells. Skin rash, thyroid dysfunction, hepatitis, colitis, and interstitial lung disease are frequent irAEs, and a meta-analysis of irAEs for NSCLC patients who received anti-PD-1/PD-L1 inhibitors reported an incidence rate of irAEs of up to 22%. Appropriate treatment for irAEs is important because 4% of patients had severe irAEs and 0.34% had ICI-related deaths.6 Recently, several studies have reported that ICI treatment was more effective in patients with NSCLC who developed irAEs than in those who did not develop irAEs.7,8 Many previous studies have revealed the prognostic factors correlated with the efficacy of immunotherapy, including the development of irAEs and the utility of markers reflected on systemic nutritional and inflammatory statuses, such as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lung immune prognostic index (LIPI).9,10 As described above, various simple markers related to prognostic factors have been examined. IrAEs as a prognostic factor have been fully investigated, but few studies have investigated the predictive factors correlated with the development of irAEs. Early detection of irAEs not only prevents the decrease in patients’ quality of life, resulting in a more severe condition, but also affects patients’ prognosis. Egami et al reported that pretreatment NLR > 2.3 and PLR > 165 were significantly correlated with an increasing incidence of irAEs in NSCLC patients who received pembrolizumab monotherapy.11 Another retrospective study reported that elevated body mass index, higher number of pembrolizumab cycles, and derived NLR < 3 were correlated with an increased incidence of irAEs in patients receiving pembrolizumab for various cancers, such as lung cancer, melanoma, lymphoma, gastric cancer, and urothelial cancer.12 Although these studies have reported on predictive factors correlated with the development of irAEs in clinical practice, patients in these studies only received pembrolizumab; other ICIs have not been investigated. Therefore, the present study aimed to examine the factors predicting the development of irAEs in NSCLC patients who received anti-PD-1/PD-L1 inhibitor monotherapy.
Patients and Methods
Study Design
We retrospectively enrolled and identified 113 patients with advanced or recurrent NSCLC who received ICIs as the first- or subsequent-line treatment between February 2016 and May 2021 at the Shinshu University Hospital. The study protocol was approved by the Institutional Ethics Review Board of the Shinshu University School of Medicine. All the clinical findings and laboratory data were obtained from electronic medical records. The study was performed in accordance with the principles of the Declaration of Helsinki of 1964. We used a form on our website to allow patients to opt out of the research, use of the data but did not obtain informed consent. All the patient’s data in the present study have been anonymized.
Collection of Data
Clinical findings and laboratory data were evaluated at the beginning of the treatment with ICIs. PD-L1 expression was evaluated using Daco 22C3 antibody. The best objective response to ICI treatment was evaluated using the Response Evaluation Criteria in Solid Tumors (version 1.1).13 IrAEs were graded according to the Common Terminology Criteria for Adverse Events version 5.0. Systemic immune-inflammation index (SII) was defined as follows: platelet count × neutrophil count/lymphocyte count.14 The LIPI categorizes patients into three groups. Briefly, patients with derived NLR (dNLR) greater than 3 and lactate dehydrogenase (LDH) greater than the upper limit of normal (ULN) were categorized as LIPI 2, patients with dNLR lower than 3 and LDH greater than the ULN or dNLR greater than 3 and LDH lower than the ULN were categorized as LIPI 1, and patients with dNLR lesser than 3 and LDH lesser than the ULN were categorized as LIPI 0.7
Data Analysis
The objective response rate (ORR) and the disease control rate (DCR) were defined as follows: ORR, complete response rate plus the partial response rate; and DCR, ORR plus stable disease rate. The progression-free survival (PFS) and overall survival (OS) were calculated from the beginning of the ICI treatment to the period of disease progression and the period of death or last date of follow-up, respectively. Clinical findings, laboratory data, and efficacy of ICIs were compared between the patients with and without irAEs.
Statistical Analyses
Date of the data cutoff was August 31, 2021. PFS and OS were evaluated and compared using the Kaplan–Meier method and Log rank test. Categorical variables and continuous variables were analyzed using the Fisher’s exact test and Mann-Whitney U-test, respectively. Multivariate Logistic regression analysis was used for investigating the predictive factors correlated with the development of irAEs. The univariate analysis included age, sex, performance status (PS), body mass index, body surface area, histologic subtype, staging, lines of immunotherapy, albumin, NLR, PLR, SII, and LIPI; significant variables (p < 0.05) in the univariate analysis were included in the multivariate analysis. All the statistical analyses were conducted using SPSS version 26.
Results
Patient Characteristics
Characteristics of 113 patients are summarized in Table 1. Ninety-one (80.5%) and 22 (19.5%) were men and women, respectively. A median age of enrolled patients was 70 (range: 29–87) years. Patients with negative driver mutations were negative for epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) genes. The numbers of patients receiving first- and subsequent-line ICI treatments were 23 (20.4%) and 90 (79.6%) patients, respectively. Regarding ICI treatments, 63 (55.8%), 40 (35.4%), and 10 (8.8%) patients received nivolumab, pembrolizumab, and atezolizumab, respectively. Moreover, 44 (38.9%) and 69 (61.1%) patients were categorized as with irAEs and without irAEs, respectively. Patient characteristics and efficacy of ICIs among patients with and without irAEs are shown in Table 2.
 |
Table 1 Patient Characteristics |
 |
Table 2 Characteristics and Efficacy of Immunotherapy in Patients with and without Immune-Related Adverse Events |
Efficacy of Immune Checkpoint Inhibitors
The ORR and DCR for patients who were developed irAEs were significantly higher than those who were not developed irAEs (ORR: 54.5% [95% confidence interval {CI}: 39.7–69.4] vs 7.7% [95% CI: 1.2–14.2], respectively, p < 0.001; DCR: 84.1% [95% CI: 73.2–95.0] vs 38.5% [95% CI: 26.5–50.3], respectively, p < 0.001). Kaplan–Meier curves for survival time are shown in Figure 1. The PFS and OS in patients with irAEs were significantly longer than in those without irAEs (PFS: 6.8 months [95% CI: 1.2–12.4] vs 2.1 months [95% CI: 1.7–2.5], respectively, p < 0.001; OS: 25.3 months [95% CI: 12.1–38.5] vs 9.6 months [95% CI: 7.0–12.1], respectively, p < 0.001).
The Kaplan–Meier curves for patients with LIPI 0 or 1 and LIPI 2 are shown in Figure 2. The PFS and OS in patients with LIPI 0 or 1 were 4.3 months [95% CI: 3.0–5.6] and 15.8 months [95% CI: 10.8–20.7], respectively. The PFS and OS of patients with LIPI 2 were 2.1 months [95% CI: 1.0–3.2] and 8.2 months [95% CI: 4.1–12.3], respectively. There was no statistically significant difference in PFS (p = 0.299) and OS (p = 0.079) between patients with LIPI 0 or 1 and those with LIPI 2.
 |
Figure 2 Evaluation of survival for patients with LIPI 0 or 1 and LIPI 2. Kaplan–Meier curves for (A) progression-free survival (B) and overall survival in patients with LIPI 0 or 1 and LIPI 2. |
Predictive Factors Associated with the Development of Immune-Related Adverse Events (irAEs)
The univariate analyses are shown in Table 2 and revealed that the development of irAEs was independently predicted by older age (p = 0.047), first-line immunotherapy (p = 0.016), and LIPI 0 or 1 (p = 0.040). The multivariate logistic regression analyses are shown in Table 3 and revealed that the development of irAEs was independently predicted by first-line ICI treatment (ORR: 0.209, 95% CI: 0.066–0.656, p = 0.007) and LIPI 0 or 1 (ORR: 0.200, 95% CI: 0.088–0.693, p = 0.011).
 |
Table 3 Analyses Based on Multivariate Logistic Regression of Predictive Factors Correlated with the Development of Immune-Related Adverse Events |
Categorization of irAEs
The categorization of irAEs in all patients is shown in Table 4. The most common irAEs was hypothyroidism (12.4%), followed by interstitial lung disease (7.1%), skin rash (7.1%), and increased aminotransferase level (4.4%). Moreover, irAEs of grade ≥ 3 were interstitial lung disease (5.3%), followed by increased aminotransferase level (1.8%), and skin rash (1.8%). ICI treatment-related deaths were not observed.
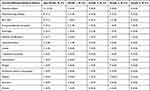 |
Table 4 Categorization of Immune-Related Adverse Events |
Discussion
We demonstrated that the lines of immunotherapy and LIPI were correlated with the development of irAEs in NSCLC patients who received ICIs. The survival time in NSCLC patients with irAEs were significantly longer than in those without irAEs, as in previous studies.
In the present study, first-line ICI treatment was a predictive factor correlated with the development of irAEs. In KEYNOTE024 and KEYNOTE010 trials, previously untreated or previously treated NSCLC patients with high PD-L1 expression who received pembrolizumab had longer PFS and OS than those who received cytotoxic anticancer agents.1,2 In the KEYNOTE024, KEYNOTE042, and IMpower110 trials, the incidence rates of irAEs were 29.2%, 28%, and 40.2%, respectively.15,16
Although these studies have already revealed that PD-L1 status ≥ 50% is a favorable prognostic factor associated with immunotherapy, an association between high PD-L1 expression and the development of irAEs has not been examined in these large prospective clinical trials. However, in a retrospective study, Sugisaka et al reported that PD-L1 status ≥ 50% was a predictive factor correlated with the development of irAEs in NSCLC patients who were treated with pembrolizumab.17 In the present study, of the 23 patients who received first-line ICI treatment, 22 had high PD-L1 expression (≥ 50%). Regarding efficacy, the PFS in patients with first-line ICI treatment was significantly longer than that in patients with subsequent-line ICI treatment (12.7 months vs 2.7 months, p = 0.001); the median number of ICI cycles in patients receiving first- and subsequent-line ICIs was 6 and 4 cycles, respectively. Thus, the number of ICI cycles was higher in patients receiving first-line ICI treatment. A retrospective study by Eun et al reported an association between the cycles of pembrolizumab and the development of irAEs, which is same as the results of the present study.12 Currently, it remains unclear why first-line ICI treatment increased the development of irAEs, but the present study considered two hypotheses. First, irAEs develop due to the reactivation of exhausted T cells and some influence on homeostasis by using ICIs. In patients with high PD-L1 status in tumor cells, inhibition of PD-L1 and PD-1 binding with an antibody can strongly inhibit T cell activity suppression, leading to T cell activation. Thus, high PD-L1 expression is correlated with reactivation of exhausted T cells, which may lead to an increasing development of irAEs. Second, patients treated with ICIs in the first-line treatment had better clinical outcomes than those treated with the subsequent-line treatment, and ICIs were used for a long period of time. In other words, there is a possibility that the development of irAEs has increased because there were not only early-onset irAEs but also late-onset irAEs. In general, irAEs are most likely to develop within 12 weeks of commencing ICIs; however, there are cases of late onset and onset after completing ICIs.18 The difference in patient characteristics between the early-onset group and the late-onset group is unclear; hence, it is necessary to collect and examine more cases.
LIPI can be easily measured at all institutions in clinical practice and has been a useful prognostic factor correlated with therapeutic response of ICIs in advanced lung cancer patients in several previous studies.19,20 LIPI is a useful marker because it has a clear cutoff value, different from NLR, PLR, and SII. Kazandjian et al reported an exploratory pooled analysis of NSCLC patients who were treated with ICIs and showed that the OSs of LIPI 0, LIPI 1, and LIPI 2 were 15.6, 8.9, and 4.5 months, respectively (p < 0.001).21 Thus, the correlation between LIPI and therapeutic response of ICIs has been demonstrated in NSCLC patients. No previous studies have reported the correlation between LIPI and the development of irAEs. The present study firstly report that LIPI 0 or 1 is a predictive factor correlated with the development of irAEs; it demonstrated no statistically significant difference in PFS (p = 0.299) and OS (p = 0.079) between patients with LIPI 0 or 1 and those with LIPI 2. However, the survival time tended to be prolonged in the LIPI 0 or 1 group, suggesting that LIPI reflects the efficacy of ICIs. Considering the positive association between the development of irAEs and efficacy of ICIs, the result of the low incidence rate of irAEs in patients with LIPI 2 is valuable. In the present study, NLR, PLR, and SII values were not significant difference between patients with and without irAEs, and the correlation between the development of irAEs and these markers was not shown. Egami et al reported that markers, such as NLR, PLR, absolute lymphocyte count, and lymphocyte-to-monocyte ratio, were useful predictors associated with the development of irAEs by setting an optimal cutoff value using the receiver operating characteristic curve.11 Optimal cutoff values for these markers vary depending on the target patient population and should be interpreted with caution.
The present study has some limitations. First, there may have been a selection bias of using ICI alone instead of combination ICI with cytotoxic anticancer agents as first-line treatment. Second, treatment for irAEs, such as administration of corticosteroids, has not been investigated, and the effect on survival outcomes of patients with irAEs is unknown. Third, the present study was a retrospective and had a small sample size in a single institution. Fourth, since 30.1% of the patients had not been measured for PD-L1 expression, the correlation between PD-L1 expression and irAE development was not investigated. Fifth, LIPI analysis could not be performed in three groups of 0, 1, and 2 due to the small sample size.
Conclusion
The present study indicated that first-line ICI treatment and LIPI 0 or 1 were correlated with the development of irAEs in NSCLC patients who received ICIs. These results are useful for leading to early detection of irAEs and early response to irAEs in clinical practice. Further studies relating to the correlation between various blood markers and the development of irAEs should be conducted using multicenter large-scale cohorts.
Abbreviations
CI, confidence interval; DCR, disease control rate; dNLR, derived NLR; ICIs, immune checkpoint inhibitors; irAEs, Immune-related adverse events; LDH, lactate dehydrogenase; LIPI, lung immune prognostic index; NLR, neutrophil-to-lymphocyte ratio; NSCLC, non-small cell lung cancer; ORR, objective response rate; OS, overall survival; PFS, progression-free survival; PLR, platelet-to-lymphocyte ratio; PS, Performance Status; SII, Systemic immune-inflammation index; ULN, upper limit of normal.
Ethics Approval and Informed Consent
All data collection and analyses were performed in accordance with the principles of the Declaration of Helsinki. The study protocol was reviewed and approved by the research ethics board of the Shinshu University School of Medicine (4772). Our institution uses a form on its website to allow patients to opt out of the research use of their data, although written informed consent was not obtained.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375:1823–1833. doi:10.1056/NEJMoa1606774
2. Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–1545. doi:10.1016/S0140-6736(15)01281-7
3. Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced non-squamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–1639. doi:10.1056/NEJMoa1507643
4. Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–135. doi:10.1056/NEJMoa1504627
5. Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a Phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–265. doi:10.1016/S0140-6736(16)32517-X
6. Sun X, Roudi R, Dai T, et al. Immune-related adverse events associated with programmed cell death protein-1 and programmed cell death ligand 1 inhibitors for non-small cell lung cancer: a PRISMA systematic review and meta-analysis. BMC Cancer. 2019;19:558. doi:10.1186/s12885-019-5701-6
7. Haratani K, Hayashi H, Chiba Y, et al. Association of immune-related adverse events with nivolumab efficacy in non-small-cell lung cancer. JAMA Oncol. 2018;4:374–378. doi:10.1001/jamaoncol.2017.2925
8. Sonehara K, Tateishi K, Araki T, et al. The role of immune-related adverse events in prognosis and efficacy prediction for patients with non-small cell lung cancer treated with immunotherapy: a retrospective clinical analysis. Oncology. 2021;99:271–279. doi:10.1159/000511999
9. Diem S, Schmid S, Krapf M, et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017;111:176–178. doi:10.1016/j.lungcan.2017.07.024
10. Mezquita L, Auclin E, Ferrara R, et al. Association of the lung immune prognostic index with immune checkpoint inhibitor outcomes in patients with advanced non-small cell lung cancer. JAMA Oncol. 2018;4:351–357. doi:10.1001/jamaoncol.2017.4771
11. Egami S, Kawazoe H, Hashimoto H, et al. Peripheral blood biomarkers predict immune-related adverse events in non-small cell lung cancer patients treated with pembrolizumab: a multicenter retrospective study. J Cancer. 2021;12:2105–2112. doi:10.7150/jca.53242
12. Eun Y, Kim IY, Sun JM, et al. Risk factors for immune-related adverse events associated with anti-PD-1 pembrolizumab. Sci Rep. 2019;9:14039. doi:10.1038/s41598-019-50574-6
13. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–247. doi:10.1016/j.ejca.2008.10.026
14. Liu J, Li S, Zhang S, et al. Systemic immune-inflammation index, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio can predict clinical outcomes in patients with metastatic non-small-cell lung cancer treated with nivolumab. J Clin Lab Anal. 2019;33:e22964. doi:10.1002/jcla.22964
15. Mok TSK, Wu YL, Kudaba I, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393:1819–1830. doi:10.1016/S0140-6736(18)32409-7
16. Geater S, Özgüroğlu M, Zou W, et al. Atezolizumab for first-line treatment of PD-L1-selected patients with NSCLC. N Engl J Med. 2020;383:1328–1339. doi:10.1056/NEJMoa1917346
17. Sugisaka J, Toi Y, Taguri M, et al. Relationship between programmed cell death protein ligand 1 expression and immune-related adverse events in non-small-cell lung cancer patients treated with pembrolizumab. JMA J. 2020;3:58–66. doi:10.31662/jmaj.2019-0005
18. Haanen JBAG, Carbonnel F, Robert C, et al. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv119–iv142. doi:10.1093/annonc/mdx225
19. Minami S, Ihara S, Komuta K, et al. Pretreatment lung immune prognostic index is a prognostic marker of chemotherapy and epidermal growth factor receptor tyrosine kinase inhibitor. World J Oncol. 2019;10:35–45. doi:10.14740/wjon1179
20. Sonehara K, Tateishi K, Komatsu M, et al. Lung immune prognostic index as a prognostic factor in patients with small cell lung cancer. Thorac Cancer. 2020;11:1578–1586. doi:10.1111/1759-7714.13432
21. Kazandjian D, Gong Y, Keegan P, et al. Prognostic value of the lung immune prognostic index for patients treated for metastatic non-small cell lung cancer. JAMA Oncol. 2019;5:1481–1485. doi:10.1001/jamaoncol.2019.1747
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

