Back to Journals » Risk Management and Healthcare Policy » Volume 16
Prediction of Late Hospital Arrival in Patients with Mild and Rapidly Improving Acute Ischemic Stroke in a Rural Area of China
Authors Song Y, Shen F, Dong Q, Wang L , Mi J
Received 28 March 2023
Accepted for publication 3 June 2023
Published 20 June 2023 Volume 2023:16 Pages 1119—1129
DOI https://doi.org/10.2147/RMHP.S414700
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Yeping Song,1 Fei Shen,1 Qing Dong,1 Liling Wang,1,* Jianhua Mi2,*
1Cerebrovascular Disease Center, Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, 200127, People’s Republic of China; 2Health Management Center, Renji Hospital, School of Medical School, Shanghai Jiaotong University, Shanghai, 200127, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Liling Wang; Jianhua Mi, Email [email protected]; [email protected]
Purpose: Among all ischemic stroke patients, more than half are mild and rapidly improving acute ischemic stroke (MaRAIS) patients. However, many MaRAIS patients do not recognize the disease early on, and thus they delay access to the treatment that would be most effective if provided earlier. This is especially true in rural areas. The aim of this study was to develop and validate a late hospital arrival risk nomogram in a rural Chinese population of patients with MaRAIS.
Methods: We developed a prediction model based on a training dataset of 173 MaRAIS patients collected from September 9, 2019 to May 13, 2020. Data analyzed included demographics and disease characteristics. A least absolute shrinkage and selection operator (LASSO) regression model was used to optimize feature selection for the late hospital arrival risk model. Multivariable logistic regression analysis was applied to build a prediction model incorporating the features selected in the LASSO regression models. The discrimination, calibration, and clinical usefulness of the prediction model were assessed using the C-index, calibration plot, and decision curve analysis, respectively. Internal validation was then assessed using bootstrapping validation.
Results: Variables contained in the prediction nomogram included transportation mode, history of diabetes, knowledge of stroke symptoms, and thrombolytic therapy. The model had moderate predictive power with a C-index of 0.709 (95% confidence interval: 0.636– 0.783) and good calibration. In the internal validation, the C-index reached 0.692. The risk threshold was 30– 97% according to the analysis of the decision curve, and the nomogram could be applied in clinical practice.
Conclusion: This novel nomogram, which incorporates transportation mode, history of diabetes, knowledge of stroke symptoms, and thrombolytic therapy, was conveniently applied to facilitate individual late hospital arrival risk prediction among MaRAIS patients in a rural area of Shanghai, China.
Keywords: mild and rapidly improving acute ischemic stroke, mild stroke, prehospital delay, late hospital arrival
Introduction
The prevalence and incidence of ischemic stroke in China have increased over the past 20 years,1,2 which has substantially increased the economic burden on families and society.3 Among all ischemic stroke patients, more than half are mild and rapidly improving acute ischemic stroke (MaRAIS) patients.4–6 Although there is no specific criteria defining MaRAIS (patients with 18 years or older with mild stroke symptoms or rapidly improving acute ischemic stroke defined clinically), most of these patients present with a National Institutes of Health Stroke Scale (NIHSS) score ≤ 5.7,8 Most MaRAIS patients are considered to have a benign prognosis, even if untreated. Nevertheless, research has shown that 23–38% of patients who initially present with MaRAIS subsequently develop functional disability and poor clinical outcomes compared with other types of stroke.9,10
Previous studies indicate that thrombolytic therapy with recombinant tissue plasminogen activator can significantly improve outcomes for MaRAIS patients.7 Additionally, various studies have shown that early treatment, including the combination of clopidogrel and aspirin, could improve prognosis in mild stroke patients who are treated within 24 hours of symptom onset.11,12 Consequently, early intervention is vital for MaRAIS patients. We defined late hospital arrival in patients with MaRAIS as more than 24 hours from onset to emergency visit. Indeed, many MaRAIS patients do not recognize the disease early, and thus they delay access to the treatment that would be most effective if provided earlier. This is especially true in rural areas.13 In China, over half of the population lives in rural areas. The prevalence of stroke in rural areas of China has increased substantially.1 However, the early emergency treatment rate of stroke remains low.2
Late hospital arrival is affected by multiple determinants.14,15 Although there are many risk factors, developing tools for the accurate prediction of late hospital arrival and early intervention may be the most effective actions to improve the unsatisfactory onset-to-door time. The purpose of our study is to develop a valid and easy-to-use prediction model to determine factors associated with late hospital arrival in MaRAIS patients in our rural area and provide evidence for efficient stroke interventions in the future.
Materials and Methods
Patients
A total of 173 patients were enrolled from the South Campus of Renji Hospital affiliated with the Shanghai Jiao Tong University School of Medicine between September 9, 2019 and May 13, 2020. The inclusion criteria was that patients presented with stroke symptoms within 14 days from symptom onset and had a brain computed tomography scan. All patients were diagnosed as having MaRAIS, defined by an NIHSS score of 0–5. The exclusion criteria was that patients with non-ischemic strokes, or NIHSS score>6 ischemic strokes. All participants signed the informed consent and completed a brief survey questionnaire. Information collected included demographics (ie, age, sex, education level, weight and height, medical insurance, and occupation), clinical characteristics, lifestyle factors (eg, smoking and alcohol use), vascular risk factors (eg, hypertension, diabetes, hyperlipemia, coronary disease, and atrial fibrillation), family history of stroke, medication history (eg, aspirin, clopidogrel, statins, or warfarin or other anticoagulants), personal disease history (eg, ischemic stroke, hemorrhage stroke), arrival characteristics (eg, transportation mode [ambulance or other]), knowledge of stroke symptoms and thrombolytic therapy, onset-to-door time (time from stroke symptom onset to the time of arrival at the hospital), and NIHSS score (Supplementary Table 1). Body mass index (BMI) was calculated using weight (kg) and height (m) based on BMI (kg/m2) = weight/height2. Research approval was obtained from the Ethics Committee at Renji Hospital, Shanghai Jiao Tong University School of Medicine (2018–182-SR-01) and this study complies with the Declaration of Helsinki.
Statistical Analysis
Using onset-to-door time, the 173 patients in our study were divided into early (<24 hours) and late (≥24 hours) arrival groups. All data in this study were analyzed with R software (version 3.6.3; https://www.r-project.org).
First, we screened the risk factors for the two groups with the least absolute contraction selection operator (LASSO). This method is suitable for high dimensional data compression and can be used to analyze the optimal predicted risk factors of the disease.16 Features with nonzero coefficients in the LASSO regression model were selected.17 Then, multivariable logistic regression analysis was used to build a prediction model by incorporating the features selected in the LASSO regression model. The features were assessed with odds ratios (ORs) and 95% confidence intervals (CIs), and the corresponding p-values were then obtained. The statistical significance levels were all two-sided. All potential predictors were applied to develop a prediction model for the risk of late hospital arrival by using the cohort.18,19
Calibration curves were plotted to assess the calibration of the late hospital arrival nomogram. To quantify the discrimination performance of the late hospital arrival nomogram, Harrell’s C-index was measured. To further verify the stability of this prediction model, the entire dataset was used for internal verification and the late hospital arrival nomogram was subjected to bootstrapping validation (1000 bootstrap resamples) to calculate a relatively corrected C-index.20 Decision curve analysis was conducted to determine the clinical usefulness of the late hospital arrival nomogram by quantifying the net benefits at different threshold probabilities in the MaRAIS cohort.21 The net benefit was calculated by subtracting the proportion of all patients who were false positive from the proportion of the patients who were true positive, and then by weighing the relative harm of forgoing interventions compared with the negative consequences of an unnecessary intervention.22
Results
Demographic Characteristics of the Patients
In the present study, 173 patients were included in our final analysis. All patients were divided into early (n = 97) and late (n = 76) arrival groups (128 men and 45 women; median age 66 years [range 33–91 years]). The specific demographic indicators and clinical characteristics of the two groups are shown in Table 1.
 |
Table 1 Demographic and Clinical Characteristics of Patients in the Early and Late Groups |
Factor Selection
Of all demographic and clinical characteristics, 31 factors were reduced to four potential predictors on the basis of the data from the 173 patients in the cohort (~8:1 ratio; Figure 1A and B), and those with nonzero coefficients were incorporated into the LASSO regression model. Those factors included transportation mode, history of diabetes, knowledge of stroke symptoms, and knowledge of thrombolytic therapy (Table 2).
 |
Table 2 Screening Out Risk Factors for Late Hospital Arrival with LASSO Regression |
Development of an Individualized Prediction Model
The results of the logistic regression analysis for transportation mode, history of diabetes, knowledge of stroke performance, and knowledge of thrombolytic therapy are shown in Table 3. The model that incorporated the above independent variables was developed and presented as the nomogram (Figure 2).
 |
Table 3 Screening Out Risk Factors for Late Hospital Arrival with Logistic Regression |
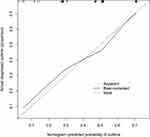
Apparent Performance of the Late Hospital Arrival Nomogram in the Cohort
The calibration curve of the late hospital arrival nomogram for the prediction of late hospital arrival risk in MaRAIS patients demonstrated moderate agreement in this cohort (Figure 3). The C-index for the prediction nomogram was 0.709 (95% CI: 0.636–0.783) for the cohort. This was confirmed to be 0.692 through bootstrapping validation, which suggested that the model had satisfactory prediction accuracy. To summarize the results from the above verification, the nomogram of the model had moderate predictive ability.
Clinical Use
The decision curve analysis for the late hospital arrival nomogram is presented in Figure 4. The decision curve showed that if the threshold probabilities of a patient and doctor were 3% and 71%, respectively, using this nomogram to predict the late hospital arrival risk adds more benefit than the intervention-all-patients scheme or the intervention-none scheme. Within this range, the net benefit was comparable, with several overlaps, on the basis of the late hospital arrival risk nomogram.
Discussion
In this study, the nomogram, which included transportation mode, history of diabetes, KOSP, and KOTT, had a moderate ability with a C-index of 0.709 to predict the individual late hospital arrival risk prediction among MaRAIS patients in a rural area of Shanghai, China. And this nomogram could be applied in clinical practice. Nomograms are currently widely used as a novel predictive tool. A nomogram is considered to be a user-friendly digital interface with high accuracy and an easily understood prognosis, which facilitates better clinical decision-making.23 However, nomograms are rarely applied to cerebral ischemic diseases.
Regarding MaRAIS patients, earlier hospital arrival after symptom onset was associated with better outcomes than late arrival.4,9 Accurate risk assessment would assist physicians in distinguishing those at a high risk of seeking later treatment and provide timely interventions to increase the probability of a favorable net benefit. Indeed, predicting late-seeking treatment of individual patients was previously quite difficult. Here, we developed and validated a novel prediction tool for the risk of late hospital arrival among MaRAIS patients using four easily assessed variables. Incorporating demographic and clinical characteristic factors into an easy-to-use nomogram facilitates the MaRAIS individualized prediction of late hospital arrival. For example, a MaRAIS patient with diabetes who does not take an ambulance to the hospital and lacks knowledge about stroke symptoms and thrombolytic therapy has an estimated 90% probability of arriving late to the hospital.
Prior studies have shown that 29% of patients with mild or rapidly improving symptoms not receiving thrombolysis had a poor outcome.24 Thus, recurrence and progression of stroke events in patients with an initial mild stroke or transient ischemic attack (TIA) are frustrating.25 Previous nomogram studies focused more on prognostic factors for acute stroke.26 Our study is the first to establish a nomogram model for predicting late hospital arrival in MaRAIS patients in rural China, which could assist clinicians with identification of patients at high risk of late hospital arrival.
In the present study, approximately 44% of patients arrived late at hospital. Consistent with previous studies,14,15 MaRAIS patients with diabetes were more likely to delay their hospital arrival when they had a stroke compared with people without diabetes. It has been speculated that patients with diabetes may mistake the symptoms of stroke as hypoglycemia and that self-management may delay stroke treatment.27 Therefore, it is necessary to improve the knowledge of strokes in the community, endocrine ward, and outpatient diabetes clinics.
Additionally, we found that the rate of ambulance use was only 16.8%. For patients with ischemic stroke, early transportation to the hospital is associated with effective stroke treatment.28 Despite this, many patients in China with MaRAIS failed to immediately call ambulances.28,29 Because the rural emergency medical service (EMS) system is inefficient and because rural residents have less knowledge about stroke and lower incomes, this phenomenon is rather common in rural areas.30,31 It is necessary to improve the ambulance service system and community education in rural areas, so that residents will call an ambulance immediately when a stroke occurs.
The incidence of stroke in rural areas of China has dramatically increased; however, little is known about stroke symptoms in patients in rural areas compared with urban areas.32 According to our research, the rate of stroke symptom awareness was 39.3%. Knowledge of stroke symptoms alone may not lead to patients going to the hospital sooner,30,33 but patients may act quicker when they know the time window for stroke treatments, such as intravenous thrombolysis. However, only 8.7% of the MaRAIS patients in the present study had knowledge of recombinant tissue plasminogen activator treatment. Thus, future public education campaigns should emphasize that accessing treatment sooner maximizes treatment effects. This education may reduce the treatment seeking time.
No significant differences in arrival time were noted for various other factors, including sex, medical insurance, and neurological deficits. Different from other studies,15,34 a history of chronic diseases, like hypertension, atrial fibrillation, coronary disease, or hyperlipidemia, did not increase the risk of late hospital arrival. Surprisingly, educational level was not associated with late treatment-seeking behavior. This suggests that stroke education should focus on stroke information, including early symptoms and treatment, regardless of educational level.33
In conclusion, our prediction nomogram could be used for a wide range of individuals. Our prediction tool may serve as a guide for further rural community intervention. It also indicates that the government should improve public stroke education and increase awareness of stroke and the importance of timely treatment, including using ambulances for transportation, particularly among people with diabetes. Targeted education may be more efficient.
Our study has some limitations. First, this observational study was based on hospitals’ voluntary enrollment and did not have a well-designed sampling frame. Our sample size was relatively small. Additionally, we did not analyze the distance between the patient’s residence and the hospital because our hospital was the only tertiary hospital in our rural town and almost all patients lived in the vicinity of this hospital. In subsequent studies, it will be crucial to consider additional factors such as distance to hospital, patient marital status, whether patients live alone, and whether they have communication difficulties at stroke symptoms onset. Finally, we should verify the applicability and validity of this model in a larger sample and in multiple centers.
Conclusions
This study establishes a simple nomogram that can guide clinicians in developing a medical education program to target MaRAIS patients who may arrive late to the hospital. This is especially true for diabetic patients. The government should implement related stroke education for MaRAIS patients according to the risk factors identified here. This is urgent and salient in rural areas. This nomogram needs more extensive clinical external verification and further research is needed to determine whether interventions in MaRAIS patients on the basis of this nomogram would encourage them to go to hospital as early as possible.
Abbreviations
MaRAIS, mild and rapidly improving acute ischemic stroke; LASSO, least absolute shrinkage and selection operator; NIHSS, National Institutes of Health Stroke Scale; BMI, Body mass index; ORs, odds ratios; Cis, confidence intervals; TIA, transient ischemic attack; EMS, emergency medical service.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Ethics Approval and Informed Consent
Research approval was obtained from the Ethics Committee at Renji Hospital, Shanghai Jiao Tong University School of Medicine (2018-182-SR-01). All participants signed the informed consent.
Acknowledgments
The authors thank Dr. Gang Wang at Shanghai Institute of Neurology, Shanghai Jiao Tong University School of Medicine for critical reading of the manuscript, and Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac) for editing a draft of this manuscript.
Author Contributions
Liling Wang and Jianhua Mi contributed equally to this work as co-corresponding authors. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Renji Hospital National Natural Breeding Fund (No. 2017PYQA01).
Disclosure
The authors declare that they have no competing interests.
References
1. Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405. doi:10.1016/S1474-4422(18)30500-3
2. Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 Adults. Circulation. 2017;135(8):759–771. doi:10.1161/CIRCULATIONAHA.116.025250
3. Gao Y, Jiang B, Sun H, et al. The burden of stroke in China: results from a nationwide population-based epidemiological survey. PLoS One. 2018;13(12):e0208398. doi:10.1371/journal.pone.0208398
4. Reeves M, Khoury J, Alwell K, et al. Distribution of national institutes of health stroke scale in the Cincinnati/Northern Kentucky stroke study. Stroke. 2013;44(11):3211–3213. doi:10.1161/STROKEAHA.113.002881
5. Khatri P, Kleindorfer DO, Devlin T, et al. Effect of alteplase vs aspirin on functional outcome for patients with acute ischemic stroke and minor nondisabling neurologic deficits: the PRISMS randomized clinical trial. JAMA. 2018;320(2):156–166. doi:10.1001/jama.2018.8496
6. Wang Y, Li Z, Wang Y, et al. Chinese stroke center alliance: a national effort to improve healthcare quality for acute stroke and transient ischaemic attack: rationale, design and preliminary findings. Stroke Vasc Neurol. 2018;3(4):256–262. doi:10.1136/svn-2018-000154
7. Laurencin C, Philippeau F, Blanc-Lasserre K, et al. Thrombolysis for acute minor stroke: outcome and barriers to management. Results from the RESUVAL stroke network. Cerebrovasc Dis. 2015;40(1–2):3–9. doi:10.1159/000381866
8. Romano JG, Smith EE, Liang L, et al. Outcomes in mild acute ischemic stroke treated with intravenous thrombolysis: a retrospective analysis of the get with the guidelines-stroke registry. JAMA Neurol. 2015;72(4):423–431. doi:10.1001/jamaneurol.2014.4354
9. Smith EE, Fonarow GC, Reeves MJ, et al. Outcomes in mild or rapidly improving stroke not treated with intravenous recombinant tissue-type plasminogen activator: findings from get with the guidelines-stroke. Stroke. 2011;42(11):3110–3115. doi:10.1161/STROKEAHA.111.613208
10. Romano JG, Smith EE, Liang L, et al. Distinct short-term outcomes in patients with mild versus rapidly improving stroke not treated with thrombolytics. Stroke. 2016;47(5):1278–1285. doi:10.1161/STROKEAHA.115.011528
11. Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369(1):11–19. doi:10.1056/NEJMoa1215340
12. Hao Q, Tampi M, O’Donnell M, et al. Clopidogrel plus aspirin versus aspirin alone for acute minor ischaemic stroke or high risk transient ischaemic attack: systematic review and meta-analysis. BMJ. 2018;363:5108. doi:10.1136/bmj.k5108
13. Sobral S, Taveira I, Seixas R, et al. Late hospital arrival for thrombolysis after stroke in Southern Portugal: who Is at Risk? J Stroke Cerebrovasc Dis. 2019;28(4):900–905. doi:10.1016/j.jstrokecerebrovasdis.2018.12.009
14. Hong ES, Kim SH, Kim WY, Ahn R, Hong JS. Factors associated with prehospital delay in acute stroke. Emerg Med J. 2011;28(9):790–793. doi:10.1136/emj.2010.094425
15. Jin H, Zhu S, Wei JW, et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. 2012;43(2):362–370. doi:10.1161/STROKEAHA.111.623512
16. Wang H, Zhang L, Liu Z, et al. Predicting medication nonadherence risk in a Chinese inflammatory rheumatic disease population: development and assessment of a new predictive nomogram. Patient Prefer Adherence. 2018;12:1757–1765. doi:10.2147/PPA.S159293
17. Kidd AC, McGettrick M, Tsim S, et al. Survival prediction in mesothelioma using a scalable Lasso regression model: instructions for use and initial performance using clinical predictors. BMJ Open Respir Res. 2018;5(1):e000240. doi:10.1136/bmjresp-2017-000240
18. Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–180. doi:10.1016/S1470-2045(14)71116-7
19. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–1370. doi:10.1200/JCO.2007.12.9791
20. Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med. 2004;23(13):2109–2123. doi:10.1002/sim.1802
21. Vickers AJ, Cronin AM, Elkin EB, Gonen M. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inform Decis Mak. 2008;8(53). doi:10.1186/1472-6947-8-53
22. Huang YQ, Liang CH, He L, et al. Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol. 2016;34(18):2157–2164. doi:10.1200/JCO.2015.65.9128
23. Yuan K, Chen J, Xu P, et al. A nomogram for predicting stroke recurrence among young adults. Stroke. 2020:120029740. doi:10.1161/STROKEAHA.120.029740
24. Khatri P, Conaway MR, Johnston KC. Acute Stroke Accurate Prediction Study I. Ninety-day outcome rates of a prospective cohort of consecutive patients with mild ischemic stroke. Stroke. 2012;43(2):560–562. doi:10.1161/STROKEAHA.110.593897
25. Chen W, Pan Y, Zhao X, et al. Intravenous thrombolysis in Chinese patients with different subtype of mild stroke: thrombolysis in patients with mild stroke. Sci Rep. 2017;7(1):2299. doi:10.1038/s41598-017-02579-2
26. Bautista AF, Lenhardt R, Yang D, et al. Early prediction of prognosis in elderly acute stroke patients. Crit Care Explor. 2019;1(4):e0007. doi:10.1097/CCE.0000000000000007
27. Angerud KH, Brulin C, Naslund U, Eliasson M. Longer pre-hospital delay in first myocardial infarction among patients with diabetes: an analysis of 4266 patients in the northern Sweden MONICA Study. BMC Cardiovasc Disord. 2013;13(6). doi:10.1186/1471-2261-13-6
28. Li S, Cui LY, Anderson C, et al. Barriers from calling ambulance after recognizing stroke differed in adults younger or older than 75 years old in China. BMC Neurol. 2019;19(1):283. doi:10.1186/s12883-019-1480-6
29. Wang L, Chao Y, Zhao X, et al. Factors associated with delayed presentation in patients with TIA and minor stroke in China: analysis of data from the China National Stroke Registry (CNSR). Neurol Res. 2013;35(5):517–521. doi:10.1179/1743132813Y.0000000204
30. Li S, Cui LY, Anderson C, et al. Public awareness of stroke and the appropriate responses in china: a cross-sectional community-based study (FAST-RIGHT). Stroke. 2019;50(2):455–462. doi:10.1161/STROKEAHA.118.023317
31. Thomas TL, Clem KJ. Emergency medical services in China. Acad Emerg Med. 1999;6(2):150–155. doi:10.1111/j.1553-2712.1999.tb01054.x
32. Yang J, Zheng M, Chen S, et al. Knowledge of thrombolytic therapy for acute ischemic stroke among community residents in western urban China. PLoS One. 2014;9(9):e107892. doi:10.1371/journal.pone.0107892
33. Faiz KW, Sundseth A, Thommessen B, Ronning OM. Patient knowledge on stroke risk factors, symptoms and treatment options. Vasc Health Risk Manag. 2018;14:37–40. doi:10.2147/VHRM.S152173
34. Fladt J, Meier N, Thilemann S, et al. Reasons for prehospital delay in acute ischemic stroke. J Am Heart Assoc. 2019;8(20):e013101. doi:10.1161/JAHA.119.013101
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.