Back to Journals » International Journal of Women's Health » Volume 15
Prediction of Emergency Cesarean Section Using Detectable Maternal and Fetal Characteristics Among Saudi Women
Authors Wahabi H , Fayed A, Elmorshedy H, Esmaeil SA, Amer YS, Saeed E, Jamal A, Aleban SA, Aldawish RA, Alyahiwi LS , Abdullah Alnafisah H , AlSubki RE, Albahli NK, Almutairi AA
Received 27 March 2023
Accepted for publication 20 July 2023
Published 8 August 2023 Volume 2023:15 Pages 1283—1293
DOI https://doi.org/10.2147/IJWH.S414380
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Hayfaa Wahabi,1,2 Amel Fayed,3 Hala Elmorshedy,3 Samia Ahmad Esmaeil,1,2 Yasser S Amer,1,4 Elshazaly Saeed,5 Amr Jamal,1,2 Sarah A Aleban,3 Reema Abdullah Aldawish,3 Lara Sabri Alyahiwi,3 Haya Abdullah Alnafisah,3 Raghad E AlSubki,3 Norah khalid Albahli,3 Aljohara Ayed Almutairi3
1Research Chair for Evidence-Based Health Care and Knowledge Translation, King Saud University, Riyadh, Saudi Arabia; 2Department of Family and Community Medicine, King Saud University Medical City and College of Medicine, Riyadh, Saudi Arabia; 3Clinical Sciences Department, College of Medicine, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia; 4Clinical Practice Guidelines Unit, Quality Management Department, King Khalid University Hospital, King Saud University, Riyadh, Saudi Arabia; 5Prince Abdulla bin Khaled Coeliac Disease Research Chair, King Saud University, Riyadh, Saudi Arabia
Correspondence: Amel Fayed, Clinical Sciences Department, College of Medicine, Princess Nourah bint Abdulrahman University, P.O. Box: 84428, Riyadh, 11671, Saudi Arabia, Tel + (966) 5943 95059, Email [email protected]
Background: The worldwide rate of cesarean section (CS) is increasing. Development of prediction models for a specific population may improve the unmet need for CS as well as reduce the overuse of CS.
Objective: To explore risk factors associated with emergency CS, and to determine the accuracy of predicting it.
Methods: A retrospective analysis of the medical records of women who delivered between January 1, 2021-December 2022 was conducted, relevant maternal and neonatal data were retrieved.
Results: Out of 1793 deliveries, 447 (25.0%) had emergency CS. Compared to control, the risk of emergency CS was higher in primiparous women (OR 2.13, 95% CI 1.48 to 3.06), in women with higher Body mass index (BMI) (OR 1.77, 95% CI 1.27 to 2.47), in association with history of previous CS (OR 4.81, 95% CI 3.24 to 7.15) and in women with abnormal amniotic fluid (OR 2.30, 95% CI 1.55 to 3.41). Additionally, women with hypertensive disorders had a 176% increased risk of emergency CS (OR 2.76, 95% CI 1.35– 5.63). Of note, the risk of emergency CS was more than three times higher in women who delivered a small for gestational age infant (OR 3.29, 95% CI 1.93– 5.59). Based on the number of risk factors, a prediction model was developed, about 80% of pregnant women in the emergency CS group scored higher grades compared to control group. The area under the curve was 0.72, indicating a good discriminant ability of the model.
Conclusion: This study identified several risk factors associated with emergency CS in pregnant Saudi women. A prediction model showed 72% accuracy in predicting the likelihood of emergency CS. This information can be useful to individualize the risk of emergency CS, and to implement appropriate measures to prevent unnecessary CS.
Keywords: emergency cesarean section, indications, prediction, Saudi Arabia
Introduction
Cesarean section (CS) is the most performed major operation in obstetric practice around the globe. Worldwide rate of CS, according to the latest estimate, is 21%, with the lowest rate of 5% in Sub-Saharan Africa and the highest rate of 42.8% in Latin America and the Caribbean.1 It has been estimated that by the year 2030 more than 38 million births will be by CS and the rate of cesarean birth will increase to 28%.1 In Saudi Arabia, the CS rate is estimated at 25–27%.2,3 The World Health Organization (WHO) recommendation on the rate of CS in a population of 10–15%, has been challenged repeatedly.4,5 In 2015 the WHO released a statement recommending the use of Robson classification by all obstetrics units worldwide to provide data and evidence on a realistic recommended rate for CS. Such evidence may help in reducing the burden of unmet need of CS in many low- and middle-income countries (LMIC), as well as reduce the burden of overuse of CS.
Vaginal delivery (VD) is the natural history of normal pregnancy and normal labor. However, in certain circumstances, CS is performed as a lifesaving intervention to avoid undue complications to the mother or the baby. Common indications for CS include previous CS, fetopelvic disproportion, fetal malpresentation, fetal distress and failure of labor progress.6,7 Nevertheless, overuse of CS without medical indication will result in unnecessary waste of resources especially because CS birth is not without potential complications to the mother and the infant including postpartum hemorrhage, postpartum infection and childhood asthma and obesity.8–10 Additional complications such as intraoperative massive blood loss and unintended surgical trauma are recognized more frequently in emergency compared to elective CS.11 Hence, the decision to perform emergency CS entails rapid assessment of the risks associated with continuing attempt of natural birth versus CS delivery.12 Based on the results of many studies which showed the higher rate of morbidity and mortality associated with emergency CS compared to scheduled procedures,13 many models for prediction of possibility of delivery by CS have been suggested. Some models used both antenatal and intrapartum factors,14 other models were developed for certain groups such as nulliparous women15 or those with previous CS.16 Moreover, CS prediction models differ in terms of ethnicity, demographic characteristics of different communities and the common medical problems in the community such as obesity or diabetes which can influence the course of labor and normal birth.17,18
In Saudi Arabia, few studies reported on the rate of CS. Recently published studies reported an overall rate of 13.6% (range; 7.1–16.3%) for emergency CS and 7.8% (range; 4.5–12.5%) for elective CS.2,19 However, the rate of CS in Saudi Arabia has increased more than twofold (25–27%) compared to the 9–10% rate reported in 1994–1997.20,21 The exponential change in the rate of CS observed in Saudi Arabia over time may be due to factors such as the wide spread use of electronic fetal monitoring,22 change in the prevalence of maternal obesity and diabetes,19,23 increased fear of litigation24 or maternal request for CS delivery.
Emergency cesarean section predictive regression models are valuable tools in obstetrics to assess the risk of emergency CS before the onset of labor. These models utilize various antenatal obstetric and non-obstetric factors to predict the likelihood of an emergency CS. The model’s performance accuracy is assessed using the area under the receiver operating characteristic curve (AUC).18,25 These predictive models have identified various factors associated with an increased risk of emergency cesarean section. Factors such as maternal age, BMI, previous CS, abnormality in amniotic fluid, induction of labor, and fetal physical measurements have been found to be significant predictors.18,26 Overall, there are few published studies evaluating predictive performance of emergency CS models, and to the best of our knowledge, no studies were conducted in Saudi Arabia.
The objectives of this study were to investigate the main obstetric and non-obstetric risk factors for emergency CS then to develop an emergency CS prediction tool, which will help clinicians to counsel women on the risk of delivering by CS.
Materials and Methods
This study was performed in accordance with the principles stated in the Declaration of Helsinki.27 We conducted a retrospective analysis of medical records of deliveries that occurred from January 1, 2021, to December 31, 2022. We included all pregnancies who delivered during the study period irrespective of maternal age, parity, type of onset of labor, obstetrics, or medical complications, and excluded those with gestational ages less than 25 weeks and multiple pregnancies. A total of 1793 cases met the eligibility criteria for the study. We classified all cases according to the mode of delivery, and women were assigned to one of three groups: vaginal delivery (VD), elective (CS), or emergency CS. We defined elective CS as a planned surgical delivery that was scheduled prior to the onset of labor or any other obstetric complication. Emergency CS, on the other hand, was defined as a cesarean delivery performed urgently due to unforeseen maternal or fetal complications during labor or delivery. We excluded those who delivered by elective CS from further analysis.
Data extraction was done using a standardized data collection sheet that included the following sections; demographic data such as maternal age, weight, height, obstetric history including parity and previous CS, perinatal complications such as diabetes, hypertensive events, amniotic fluid abnormalities, umbilical cord status along with pre-labor events such as induction of labor. Neonatal characteristics were also retrieved including birth weight and gender.
Definitions
- Emergency CS: was defined as a case in which the procedure of VD was terminated due to the occurrence of emergency events which put the life of the mother or the baby at risk.
- Pregestational diabetes: is a condition in which the mother has diabetes (most commonly type 1 or type 2 diabetes) before the onset of pregnancy.28
- Gestational diabetes (GDM): is defined as any degree of glucose intolerance with onset or first recognition during pregnancy.29
- Hypertensive events of pregnancy: all cases who developed gestational hypertension, pre-eclampsia or eclampsia were aggregated in this category.
- Amniotic fluid abnormality: the patients were classified according to the amniotic fluid index into polyhydramnios group if the amniotic fluid index ≥ 24 cm or oligohydramnios if amniotic fluid index ≤ 5 cm, provided that the assessment was done within seven days of the delivery.
- Amniotic fluid quality: according to the clarity of the amniotic fluid, it was categorized as clear (clear thin yellowish color), stage I (fresh meconium stain), stage II (old meconium stain) and stage III is blood-stained fluid. When developing the regression model, the three stages were aggregated in one group of abnormal quality of the amniotic fluid and compared to the clear group that was considered as the reference group.
- Macrosomia: birth weight ≥ 4 Kg.
- Small for gestational age (SGA): birth weight less than the tenth percentile.
Statistical Analyses
Analyses were performed using SPSS version 22.0 (SPSS Inc, Chicago, Illinois, USA) and Stata version 16. Quantitative variables were displayed as mean± Standard Deviation while qualitative variables were expressed as frequencies and percentages. Association between mode of delivery and all perinatal characteristics was tested using Chi-square test or t-test as indicated. Logistic regression was applied to define the independent effect of each perinatal variable on the mode of delivery and both the crude and adjusted Odds Ratios (OR) were reported with its 95% Confidence interval (CI).
A scoring system was developed to identify pregnant women at high risk for emergency CS based on the adjusted OR values. Women who had a risk factor with OR value between 1 and 2 were scored as 1 point, women with a risk factor with OR value between 2 and 3 were scored as 2 points, and so on.
The score was 0 if there was no risk factor. Subsequently, according to the number of risk factors, the emergency CS risk scoring system was further established: scores of 1–2 were classified as grade 1, scores of 3–5 were grade 2, scores 6–8 were grade 3, and scores of 9–15 were grade 4.
To confirm the predictability of the selected model, we used Receiver Operating Curve (ROC) to depict the area under the curve for the model and for individual factors.30
Ethical Consideration
This study was approved by the Institutional Review Board of Princess Nourah bint Abdulrahman [IRB number 22–0009], and all data were anonymized and kept confidential. No identifiable information was included in the final manuscript. Written informed consent was not needed for this study since we used retrospectively retrieved clinically relevant data and did not alter the treatment or medical plans.
Results
Out of the 1793 women of the studied sample, 1436 (75.0%) had VD and 447 (25.0%) had emergency CS. Women in the Emergency CS group were of comparable age to women in the VD group, while they had significantly higher BMI (31.52±5.47 kg/m2 versus 30.17±5.45 kg/m2) and shorter gestational age (38.24±2.96 weeks versus 38.85±1.88 weeks) as compared to the VD group (Table 1). Most women who had emergency CS were primiparous (69.2%) while 18.8% of the group had history of previous CS. Nearly all perinatal complications were reported significantly more often among the emergency CS group, such as hypertensive disorders of pregnancy, diabetes (pregestational and gestational), abnormal amniotic fluid, entanglement or knot of umbilical cord, placenta abruptio and low laying placenta. Induction of labor and use of epidural anesthesia were higher in the emergency CS group (Table 1). Additionally, both macrosomia and SGA were more frequent in the emergency CS as compared to VD group. Indications for emergency CS in this study were fetal distress in 48.6% of the participants, failure to progress in 28.6%, and maternal request in 2.7% (Table 2).
 |
Table 1 Comparison Between Participating Women According to the Mode of Delivery |
 |
Table 2 Indication of Cesarean Section |
In the univariate analysis, variables with differences between the emergency CS and the VD groups were included. The results showed that the risk of emergency CS increased if the pregnant woman had one of the following conditions: BMI ≥28 at delivery, nulliparity, history of previous CS, abnormal characteristics of amniotic fluid, hypertensive disorders, diabetes, SGA and macrosomia (p<0.05 for all) (Table 3). However, by incorporating these risk factors into multivariate analysis with adjustment of gestational age, diabetes, macrosomia, and induction of labor were no longer independent risk factors for emergency CS (Table 3). The risk of emergency CS in primiparous women was about two times higher than in multiparous women (OR 2.13, 95% CI 1.48 to 3.06, p<0.001), and the risk was almost doubled among women with higher BMI (OR 1.77, 95% CI 1.27 to 2.47) as compared to those with normal BMI (Table 3). The risk of emergency CS in pregnant women with history of previous CS was nearly five times higher than that in women without such history (OR 4.81, 95% CI 3.24 to 7.15, p<0.01), and the risk among those with abnormal amniotic fluid was two times higher than that in those with normal amniotic fluid (OR 2.30, 95% CI 1.55 to 3.41, p<0.01). In addition, women with hypertensive disorders were nearly three times as likely to deliver by emergency CS compared to those without the condition (OR 2.76, 95% CI 1.35–5.63, p<0.01) (Table 3). Furthermore, the risk of emergency CS was more than three times higher in women with SGA infants than in those with average birth weight infants (OR 3.29, 95% CI 1.93 to 5.59) (Table 3).
 |
Table 3 Univariate and Multivariate Analysis of Factors Associated with Emergency Cesarean Section |
Based on the adjusted OR values, a scoring system was developed to identify pregnant women at high risk for emergency CS (Table 4). We included six factors which were scored as follows: BMI ≥28 before delivery (1 point), primiparous (2 points), previous history of CS (4 points), abnormal characteristics of amniotic fluid (2 points), hypertensive disorder of pregnancy (3 points), and neonatal weight <2500 (3 points) (Table 4). For each woman, the sum of the six factors was scored (0–15 points). Based on the grading system (Table 5), 92.6% of CS were clustered in grades 1–3, with 73.8% clustered in grades 2–3. In comparison, 93% of the group with vaginal delivery were clustered in grades 0–2, with 50.2% clustered in grades 0–1 and 42.8% clustered in grade 2. The proportion of grade three was about three times higher in the emergency CS group compared to the group with vaginal delivery, while the proportion of grade four was more than six times higher in the emergency CS group than in the group with vaginal delivery (Table 5). The area under the curve of the risk scoring system was 0.72 (95% CI 0.69 to 0.75), the difference was statistically significant p<0.001, which was more valuable than any other single risk factor, indicating that the regression model of the risk factors had a good predictive ability (Figure 1).
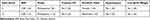 |
Table 4 Scoring of Individual Factors |
 |
Table 5 Development of Emergency CS Risk Scoring System |
Discussion
The results of this study showed that nulliparity, high BMI, SGA, hypertensive disorders during pregnancy in addition to previous CS, and the quality of amniotic fluid are predictors of emergency CS in Saudi women. Our model, which included all of these factors, showed an area under the curve of 0.72 with an acceptable power to predict women at high risk for emergency CS.31 The AUC value of 0.72 agrees with the few studies reporting performance of emergency CS prediction models, in which the AUC ranged from 0.70–0.81.14,15,25,32 The main indications for emergency CS in this cohort were fetal distress and failure to progress in labor.
Obesity and overweight are recognized risk for adverse pregnancy outcome among Saudi women including delivery by CS.19,33 In this study, high BMI increased the risk of emergency CS delivery by almost twofold, which agrees with previous studies for prediction of risk of emergency CS.32,34 Obesity in pregnancy is associated with, fetal macrosomia, GDM and hypertensive disorders,19,33 all of which can increase the risk of emergency CS in otherwise low risk women.
Similar to our findings in this study, nulliparity has been recognized in more than one model as a predictor for CS delivery,26,30,35 especially if it is associated with certain intrapartum findings such as, mild to moderate contractions, slow cervical dilatation and high fetal station, in addition to advanced maternal age, high pre-pregnancy BMI and shorter maternal height.15
Previous delivery by CS imposed the highest risk of delivering by emergency CS in this study. These results were different to those found by Guan et al,30 which confirm that each community of pregnant women have different predictors for emergency CS delivery influenced by many factors including maternal characteristics.
Our analysis showed that the odds of emergency CS increase by threefold in women with small for gestational age pregnancies, which is in agreement with previous reports.36,37 Small for gestational age SGA fetuses are at greater risk of perinatal mortality38 and intrapartum hypoxia due to compromised uteroplacental reserve which increases the possibility of CS delivery due to fetal distress,37 which was an indication for nearly half of the CS in this cohort (Table 2). Nwabuobi et al developed a model for risk factors for CS for SGA which included additional factors such as abnormal umbilical Doppler and gestational age at delivery.39
Similar to the findings of previous reports, this study showed that the presence of echogenic particles in the amniotic fluid was associated with increased risk of delivery by CS.30,40 High density amniotic fluid particles are, in most cases, related to the presence of vernix, however they may be due to the presence of meconium or blood and may indicate fetal compromise in a small proportion of cases, nevertheless, the presence of echogenic amniotic fluid is associated with low APGAR scores and increase in the rate of primary CS irrespective of their nature.40,41
Hypertensive disorders during pregnancy were found in this study to increase the odds for CS by almost threefold. The prevalence of hypertensive disorders in pregnancy in Saudi women is 4.0%,2 which is comparable to that reported globally of 5–8%.42 Previous studies reported the association of hypertension in pregnancy with adverse pregnancy outcomes including delivery by emergency CS.43
In this study, the women who delivered normally were of similar age to the women who delivered by CS, as shown in Table 1. This explains the finding that maternal age was not an independent risk factor for emergency CS in this group of participants. Nevertheless, other studies showed that; each year increase of maternal age was associated with additional 6% increase in the risk of CS.18
Previous studies from Saudi Arabia showed that GDM and pre-gestational diabetes significantly increase the rate of CS delivery,23,44 however, contrary to our expectations we did not find macrosomia or maternal diabetes independent risk factors for emergency CS in this study. This finding may be explained by the fact that pregnancies complicated with GDM or pre-gestational diabetes are monitored closely and those complicated with fetal macrosomia will be scheduled for elective CS rather than going into trial of VD. In addition, many of the mothers with pre-GDM would have had previous CS delivery, hence, they will be electively scheduled for CS.
We did not find umbilical cord knot and entanglement as independent risk factors for emergency CS; however, these abnormalities of the cord were proven to be associated with risk of emergency CS and fetal compromise45 which is manifested by abnormalities in fetal heart rate.
Contrary to the findings of previous investigators, induction of labor was not a risk factor for emergency CS in this study. This may be explained by the small number of women who had induction of labor in this study.32,46
The results showed that our model can effectively identify 70% of the women at high risk of emergency CS, and was superior to any single factor on its own, as shown in Figure 1. The scoring system we developed from the model can easily be used. The antenatal information is readily available for all women who are admitted for delivery and the assessment of the amniotic fluid, and fetal weight can be estimated by ultrasound examination at the time of admission to the delivery room. Hence, we suggest close monitoring of women with high scores using this system of evaluation as they are at high risk of having emergency CS delivery.
This study is not without limitation, including the retrospective nature of the investigation and the relatively small number of participants. However, the findings of the study should be validated in a multicenter study to complete this important step in developing a model for the prediction of the risk of emergency CS in Saudi women.
Conclusion
This study identified several important risk factors associated with emergency CS in a population of pregnant Saudi women. A prediction tool was developed based on these risk factors and showed 70% accuracy in predicting the likelihood of emergency CS among this population. This information can be useful for clinicians to counsel pregnant women on their individualized risk of delivering by emergency CS, and to implement appropriate measures to prevent unnecessary CS while ensuring the safety of the mother and the infant.
Acknowledgment
We extend our gratitude to all the women who participated in this study and to Princess Nourah bint Abdulrahman university researchers supporting project for funding this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This project was funded by Princess Nourah bint Abdulrahman university researchers supporting project (number PNURSP2022R21) Princess Nourah bint Abdulrahman university, Riyadh, Saudi Arabia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Betran AP, Ye J, Moller A-B, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Global Health. 2021;6(6):e005671. doi:10.1136/bmjgh-2021-005671
2. Wahabi H, Fayed A, Esmaeil S, et al. Riyadh mother and baby multicenter cohort study: the cohort profile. PLoS One. 2016;11(3):e0150297. doi:10.1371/journal.pone.0150297
3. Alsulami SM, Ashmawi MT, Jarwan RO, Malli IA, Albar SK, Al-Jifree HM. The rates of cesarean section deliveries according to Robson Classification System during the year of 2018 among patients in King Abdul-Aziz Medical City, Jeddah, Saudi Arabia. Cureus. 2020;12(11):56.
4. Molina G, Weiser TG, Lipsitz SR, et al. Relationship Between Cesarean Delivery Rate and Maternal and Neonatal Mortality. JAMA. 2015;314(21):2263–2270. doi:10.1001/jama.2015.15553
5. Betrán AP, Zhang J, Torloni MR, Gülmezoglu AM. Determination of a single, universal threshold for caesarean section rate is not the way forward. BMJ Evid Based Med. 2016;21(6):237. doi:10.1136/ebmed-2016-110393
6. Begum T, Rahman A, Nababan H, et al. Indications and determinants of caesarean section delivery: evidence from a population-based study in Matlab, Bangladesh. PLoS One. 2017;12(11):e0188074. doi:10.1371/journal.pone.0188074
7. Penn Z, Ghaem-Maghami S. Indications for caesarean section. Best Pract Res Clin Obstet Gynaecol. 2001;15(1):1–15. doi:10.1053/beog.2000.0146
8. Harrison MS, Pasha O, Saleem S, et al. A prospective study of maternal, fetal and neonatal outcomes in the setting of cesarean section in low‐and middle‐income countries. Acta Obstet Gynecol Scand. 2017;96(4):410–420. doi:10.1111/aogs.13098
9. Black M, Bhattacharya S, Philip S, Norman JE, McLernon DJ. Planned cesarean delivery at term and adverse outcomes in childhood health. JAMA. 2015;314(21):2271–2279. doi:10.1001/jama.2015.16176
10. Yuan C, Gaskins AJ, Blaine AI, et al. Association between cesarean birth and risk of obesity in offspring in childhood, adolescence, and early adulthood. JAMA Pediatr. 2016;170(11):e162385–e162385. doi:10.1001/jamapediatrics.2016.2385
11. Bergholt T, Stenderup JK, Vedsted-Jakobsen A, Helm P, Lenstrup C. Intraoperative surgical complication during cesarean section: an observational study of the incidence and risk factors. Acta Obstet Gynecol Scand. 2003;82(3):251–256. doi:10.1034/j.1600-0412.2003.00095.x
12. Thomas J, Paranjothy S, James D. National cross sectional survey to determine whether the decision to delivery interval is critical in emergency caesarean section. BMJ. 2004;328(7441):665. doi:10.1136/bmj.38031.775845.7C
13. Yang X-J, Sun -S-S. Comparison of maternal and fetal complications in elective and emergency cesarean section: a systematic review and meta-analysis. Arch Gynecol Obstet. 2017;296(3):503–512. doi:10.1007/s00404-017-4445-2
14. de Souza HC, Perdoná GSC, Marcolin AC, et al. Development of caesarean section prediction models: secondary analysis of a prospective cohort study in two sub-Saharan African countries. Reprod Health. 2019;16(1):1–11. doi:10.1186/s12978-019-0832-4
15. Janssen PA, Stienen JJ, Brant R, Hanley GE. A predictive model for cesarean among low‐risk nulliparous women in spontaneous labor at hospital admission. Birth. 2017;44(1):21–28. doi:10.1111/birt.12257
16. Grobman WA, Lai Y, Landon MB, et al. Can a prediction model for vaginal birth after cesarean also predict the probability of morbidity related to a trial of labor? Am J Obstet Gynecol. 2009;200(1):56. e1–56. e6. doi:10.1016/j.ajog.2008.06.039
17. Apanga PA, Awoonor-Williams JK. Predictors of caesarean section in northern Ghana: a case-control study. Pan Af Med J. 2018;29(1):1–11. doi:10.11604/pamj.2018.29.20.13917
18. Tun MH, Chari R, Kaul P, et al. Prediction of odds for emergency cesarean section: a secondary analysis of the CHILD term birth cohort study. PLoS One. 2022;17(10):e0268229. doi:10.1371/journal.pone.0268229
19. Wahabi H, Esmaeil S, Fayed A. maternal prepregnancy weight and pregnancy outcomes in Saudi women: subgroup analysis from Riyadh Mother and Baby Cohort Study (RAHMA). Biomed Res Int. 2021;2021:1–10. doi:10.1155/2021/6655942
20. Elhag BI, Milaat WA, Taylouni ER. An audit of caesarean section among Saudi females in Jeddah, Saudi Arabia. J Egypt Public Health Assoc. 1994;69(1–2):1–17.
21. Ba’aqeel HS. Cesarean delivery rates in Saudi Arabia: a ten-year review. Ann Saudi Med. 2009;29(3):179–183. doi:10.5144/0256-4947.51773
22. Alfirevic Z, Devane D, Gyte GM, Cuthbert A. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labor. Cochrane Database Syst Rev. 2017;2(2):Cd006066. doi:10.1002/14651858.CD006066.pub3
23. Wahabi H, Fayed A, Esmaeil S, Mamdouh H, Kotb R. Prevalence and complications of pregestational and gestational diabetes in Saudi women: analysis from Riyadh Mother and Baby cohort study (RAHMA). Biomed Res Int. 2017;2017:1–9. doi:10.1155/2017/6878263
24. Fineschi V, Arcangeli M, Di Fazio N, et al. Defensive medicine in the management of cesarean delivery: a survey among Italian Physicians. Healthcare. 2021;9(9):1097. doi:10.3390/healthcare9091097
25. Campillo-Artero C, Serra-Burriel M, Calvo-Pérez A. Predictive modeling of emergency cesarean delivery. PLoS One. 2018;13(1):e0191248. doi:10.1371/journal.pone.0191248
26. Quach D, Eikelder M, Jozwiak M, et al. Maternal and fetal characteristics for predicting risk of Cesarean section following induction of labor: pooled analysis of PROBAAT trials. Ultrasound Obstetrics Gynecol. 2022;59(1):83–92. doi:10.1002/uog.24764
27. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
28. Mellitus PD. Acog Practice Bulletin Summary. Obstet Gynecol. 2018;132:e228–e248.
29. American Diabetes Association. Gestational Diabetes Mellitus. Diabetes Care. 2003;26(suppl_1):s103–s105. doi:10.2337/diacare.26.2007.S103
30. Guan P, Tang F, Sun G, Ren W. Prediction of emergency cesarean section by measurable maternal and fetal characteristics. J Invest Med. 2020;68(3):799–806. doi:10.1136/jim-2019-001175
31. Hosmer D, Lemeshow S. Applied logistic regression. New York: John Wiley & Sons; 2000.
32. Levine LD, Downes KL, Parry S, Elovitz MA, Sammel MD, Srinivas SK. A validated calculator to estimate risk of cesarean after an induction of labor with an unfavorable cervix. Am J Obstet Gynecol. 2018;218(2):254. e1–254. e7. doi:10.1016/j.ajog.2017.11.603
33. Fayed A, Wahabi HA, Esmaeil S, Elkouny R, Elmorshedy H, Bakhsh H. Independent effect of gestational weight gain and prepregnancy obesity on pregnancy outcomes among Saudi women: a sub-cohort analysis from Riyadh mother and baby cohort study (RAHMA). PLoS One. 2022;17(1):e0262437. doi:10.1371/journal.pone.0262437
34. Branger B, Dochez V, Gervier S, Winer N. Cesarean after labor induction: risk factors and prediction score. Gynecol Obstetrique Fertilite Senologie. 2018;46(5):458–465. doi:10.1016/j.gofs.2018.03.008
35. Dorwal M, Yadav G, Singh P, et al. Deriving a prediction model for emergency cesarean delivery following induction of labor in singleton term pregnancies. Int J Gynaecol Obstet. 2023;160(2):698–706. doi:10.1002/ijgo.14403
36. Maslovitz S, Shenhav M, Levin I, et al. Outcome of induced deliveries in growth-restricted fetuses: second thoughts about the vaginal option. Arch Gynecol Obstet. 2009;279(2):139–143. doi:10.1007/s00404-008-0685-5
37. Prior T, Paramasivam G, Bennett P, Kumar S. Are fetuses that fail to achieve their growth potential at increased risk of intrapartum compromise? Ultrasound Obstetrics Gynecol. 2015;46(4):460–464. doi:10.1002/uog.14758
38. Gardosi J, Francis A. Adverse pregnancy outcome and association with small for gestational age birthweight by customized and population-based percentiles. Am J Obstet Gynecol. 2009;201(1):28. e1–28. e8. doi:10.1016/j.ajog.2009.04.034
39. Nwabuobi C, Gowda N, Schmitz J, et al. Risk factors for Cesarean delivery in pregnancy with small‐for‐gestational‐age fetus undergoing induction of labor. Ultrasound Obstetrics Gynecol. 2020;55(6):799–805. doi:10.1002/uog.20850
40. Buyuk GN, Oskovi-Kaplan ZA, Kahyaoglu S, Engin-Ustun Y. Echogenic particles in the amniotic fluid of term low-risk pregnant women: does it have a clinical significance? J Obstet Gynaecol. 2021;41(7):1048–1052. doi:10.1080/01443615.2020.1834520
41. Karamustafaoglu Balci B, Goynumer G. Incidence of echogenic amniotic fluid at term pregnancy and its association with meconium. Arch Gynecol Obstet. 2018;297:915–918. doi:10.1007/s00404-018-4679-7
42. Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertension Res. 2017;40(3):213–220. doi:10.1038/hr.2016.126
43. Agrawal A, Wenger NK. Hypertension during pregnancy. Curr Hypertens Rep. 2020;22:1–9. doi:10.1007/s11906-020-01070-0
44. Wahabi HA, Esmaeil SA, Fayed A, Alzeidan RA. Gestational diabetes mellitus: maternal and perinatal outcomes in King Khalid University Hospital, Saudi Arabia. J Egypt Public Health Assoc. 2013;88(2):104–108. doi:10.1097/01.EPX.0000430392.57811.20
45. Weiner E, Fainstein N, Schreiber L, Sagiv R, Bar J, Kovo M. The association between umbilical cord abnormalities and the development of non-reassuring fetal heart rate leading to emergent cesarean deliveries. J Perinatol. 2015;35(11):919–923. doi:10.1038/jp.2015.102
46. Tolcher MC, Holbert MR, Weaver AL, et al. Predicting cesarean delivery after induction of labor among nulliparous women at term. Obstet Gynecol. 2015;126(5):1059. doi:10.1097/AOG.0000000000001083
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

