Back to Journals » Cancer Management and Research » Volume 14
Prediction of Early Recurrence After R0 Resection for Gallbladder Carcinoma of Stage T1b–T3
Authors Peng DZ , Nie GL, Li B, Cai YL, Lu J, Xiong XZ, Cheng NS
Received 6 October 2021
Accepted for publication 7 December 2021
Published 3 January 2022 Volume 2022:14 Pages 37—47
DOI https://doi.org/10.2147/CMAR.S342674
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Ding-Zhong Peng,* Gui-Lin Nie,* Bei Li, Yu-Long Cai, Jiong Lu, Xian-Ze Xiong, Nan-Sheng Cheng
Department of Biliary Surgery, West China Hospital of Sichuan University, Chengdu, Sichuan Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Nan-Sheng Cheng
Department of Biliary Surgery, West China Hospital of Sichuan University, Chengdu, 610041, Sichuan Province, People’s Republic of China
Tel/Fax +86-28-85422465
Email [email protected]
Purpose: The time-to-tumor recurrence can predict the prognosis of hepatobiliary cancers following curative-intent resection. Therefore, for patients with gallbladder carcinoma (GBC) of stage T1b–T3 who had undergone R0 resection, we investigated the risk factors for early recurrence of GBC and their prognosis.
Patients and Methods: A total of 260 patients with GBC with T1b–T3 disease and an R0 margin were identified. Their clinicopathologic characteristics, perioperative details and prognostic data were reviewed. Survival analyses were carried out using the Kaplan–Meier method. Logistic regression models were used to identify the risk factors for early recurrence.
Results: The optimal cutoff for early recurrence was 29 months. Early recurrence tended to result in relapse far from the primary tumor, and such patients tended to have significantly worse overall survival. Multivariate analysis revealed that T3 disease, N1/N2 stage, poor differentiation of tumor, and lymphovascular invasion (LI) were associated with a greater risk of early recurrence. Patients diagnosed as having GBC incidentally and who had the risk factors of early recurrence were more likely to benefit from re-resection 2– 4 weeks after a cholecystectomy.
Conclusion: T3 stage, N1–N2 stage, poor differentiation, and LI were independent risk factors associated with early recurrence for patients with GBC with stage T1b–T3 disease after R0 resection.
Keywords: gallbladder carcinoma, early recurrence, prognosis, re-resection
Introduction
Gallbladder carcinoma (GBC) constitutes 80–95% of all biliary-tract tumors worldwide and is the most prevalent malignancy of the biliary tract.1 A lack of effective screening and early symptoms have resulted in GBC being discovered incidentally in many patients during or after cholecystectomy for a presumed benign disease [ie, incidental gallbladder carcinoma (IGBC)].2–4 The mainstay of curative-intent therapy for GBC is radical resection aimed at achieving an R0 margin. This strategy might involve an extended hepatectomy combined with an adequate lymphadenectomy.5,6 However, GBC is a highly malignant tumor characterized by early involvement of lymph nodes and distant metastases. Such aggressiveness results in high prevalence of postoperative recurrence and a dismal prognosis, even after R0 resection.7,8
The timing of recurrence tends to be associated with the long-term survival of GBC cases. Several studies have revealed the impact of early recurrence on the prognosis of numerous hepatobiliary cancers, such as hepatocellular carcinoma, cholangiocarcinoma, and pancreatic carcinoma.9–11 Sahara et al12 reported that early recurrence impaired the prognosis of patients with GBC with stage T1–T4 after R0/R1 resection. Kota et al proposed a scoring system incorporating the T stage, margin status, differentiation, and type of liver resection for recurrence prediction. In comparison, only GBCs at stage T1b–T3 necessitating hepatectomy were included in this research, whereas T1a tumors are adequately treated with cholecystectomy alone, and the extent of primary resection is controversial for T4 lesions.13,14 Moreover, patients with GBC who had undergone R1 resection were excluded in the current cohort because the R0 margin is of the utmost priority in curative-intent surgery.15
We aimed to identify the best cutoff period to define early recurrence for patients with GBC with T1b–T3 disease who have undergone R0 resection. In addition, the clinicopathological variables associated with early recurrence were studied. We also investigated if the time interval of re-resection for IGBC affected the prognosis of patients with the risk factors for early recurrence.
Methods
Patient Selection
Data for 260 patients who underwent R0 resection for GBC of stage T1b–T3 between 2004 and 2018 at the West China Hospital of Sichuan University were analyzed. The exclusion criteria comprised patients: (i) with macroscopically/microscopically positive margins; (ii) with T1a disease or metastatic disease; or (iii) who died <30 days after surgery (Figure 1). Ethical approval for this retrospective research was obtained from the institutional review board of West China Hospital of Sichuan University. Written informed consent was waived because of the retrospective design of the study. This study was conducted in accordance with the Declaration of Helsinki, and all patient data were kept confidential.
 |
Figure 1 Derivation of the final study cohort. |
Preoperative Workup and Treatments
Systematic assessment and in-depth imaging were conducted in patients suspected of having GBC preoperatively. Surgical management was determined considering the preoperative and intraoperative findings. According to established consensus guidelines, the standard surgical procedure for GBC of stage T1b-T3 in our institute is cholecystectomy and wedge resection of the gallbladder bed or hepatectomy of segments IVb/V.16–18 Additional procedures, such as major hepatectomy or pancreatoduodenectomy, were undertaken in cases of tumor invasion of neighboring organs (liver parenchyma, pancreas, and duodenum). Dissection of lymph nodes near the cystic duct, portal vein in the hepatoduodenal ligament, and the hilum of the liver has been part of the standard approach for patients with GBC in our hospital for some time. Postoperative complications within 90 days after radical surgery were graded using the Clavien–Dindo classification system.19 Patients with more than one postoperative complication were determined to have the highest grade of severity.19
Follow-Up Protocol
Patients were followed up routinely every 3 months for the first 12 months after hospital discharge, and every 6 months beyond the first year.20 Surveillance (liver function, tumor markers, and hepatic ultrasonography) was conducted regularly for all patients in the outpatient department. Imaging (computed tomography, magnetic resonance imaging, and positron emission tomography) and pathology (histology) were undertaken for a definitive diagnosis in patients with suspected tumor recurrence. Recurrence in the surgical bed, porta hepatis, and regional lymph nodes was defined as regional recurrence. Distant recurrence was defined as the discovery of metastasis in the discontiguous liver parenchyma, peritoneum, and other organs.
Data Collection
Details of the demographic features, imaging findings, surgical records, pathology data, and survival outcome of patients after radical surgery were collected and reviewed retrospectively. GBC in resected tumor samples was determined using histopathology reports. Tumor stage was classified according to the eighth edition of the American Joint Committee on Cancer (AJCC) tumor-node-metastasis (TNM) staging system. Upon pathology, complete removal of any tumor lesions with microscopically negative margins was defined as a curative resection (R0). Overall survival (OS) was defined as the time from the date of radical surgery to the date of death from any cause or the date of the last follow-up. Disease-free survival (DFS) was measured from the date of curative resection to the date of recurrence or last follow-up.
Statistical Analyses
Continuous variables are described by the median [interquartile range (IQR)] and categorical variables by the frequency (%). Comparisons of continuous variables between two groups were undertaken using Student’s t-test or Wilcoxon test. Comparisons of categorical factors were carried out using the chi-squared test or Fisher’s exact test. Survival was estimated using the Kaplan–Meier method. Differences were compared between groups using the log‐rank test. Univariate and multivariate logistic regression models were used to identify independent factors that were associated with early recurrence. P < 0.05 (two-tailed) was considered significant. Data analyses were carried out using SPSS 19.0 (IBM, Armonk, NY, USA).
Results
Characteristics of the Study Population
The characteristics of the entire cohort are provided in Table 1. A total of 260 patients (79 males and 181 females) with a median age of 64 (IQR, 53–70) years underwent R0 resection for GBC of grade T1b–T3. The median body mass index was 23.5 (IQR, 20.2–25.3) kg/m2. The preoperative albumin level was 40.4 (IQR, 36.8–43.1) g/L. A subset of cases underwent re-resection (n = 65, 25.0%). At the time of radical surgery, the type of resection consisted primarily of cholecystectomy with partial hepatic resection (n = 245, 94.2%). Resection of regional lymph nodes was performed routinely in all patients. The median number of harvested lymph nodes and positive lymph nodes was 5 (range, 1–19) and 0 (range, 0–9), respectively. Pathologically, most patients had tumors at stage I/II according to the AJCC classification (n = 172, 66.2%), with a median tumor diameter of 3.2 (IQR, 1.2–4.3) cm. Postoperatively, 54 patients had at least one complication, and the overall morbidity was 20.8%; 30 individuals (11.5%) developed major complications (Clavien–Dindo class > II).
 |
Table 1 Characteristics of the Entire Cohort (n = 260) |
Survival Outcomes and Definition of Early Recurrence
Median OS for the entire cohort was 45.5 months. OS at 1, 3, and 5 years was 91.9%, 63.5%, and 33.8%, respectively. At a median follow-up of 50.5 months, 84 (32.3%) patients experienced tumor recurrence after treatment; among them, 35.7% (n = 30) developed a local recurrence alone, while 40.5% (n = 34) and 23.8% (n = 20) experienced either a distant recurrence alone or both local and distant recurrence, respectively. The liver parenchyma (n = 22, 26.2%) was the most prevalent site of relapse. To determine the optimal cutoff point for early recurrence and late recurrence, recurrence prevalence was calculated at 6-month intervals. According to the intercept value of the two curves identified by linear regression, 29 months was defined as the cutoff to distinguish early recurrence from late recurrence for GBC (Figure 2A). The majority (n = 69, 82.1%) of recurrence occurred within 29 months after surgery (early recurrence), with the remaining (n = 15, 17.9%) cases were discovered beyond 29 months (late recurrence). OS of patients with GBC who experienced early recurrence was markedly lower than that of patients who experienced late recurrence (P < 0.001) (Figure 2B). Moreover, patients who experienced early recurrence were more likely to have distant metastasis than those who had late recurrence (P = 0.022) (Figure 2C).
Risk Factors Associated with Early Recurrence of GBC
The results of univariate and multivariate analysis for early recurrence are summarized in Table 2. Univariate analysis revealed the positive predictors of early recurrence to be cancer antigen 19–9 > 40 U/mL, high T category, high N category, poor differentiation, lymphovascular invasion (LI) and perineural invasion. Multivariate analyses of the logistic regression model revealed T3 stage, N1–N2 stage, poor differentiation, and LI as independent risk factors associated with early recurrence following R0 resection of GBC of stage T1b–T3.
 |
Table 2 Analysis of the Factors Associated with Early Recurrence Among Patients Undergoing R0 Resection for Gallbladder Carcinoma of Stage T1b–T3 |
Subgrouping of Patients with IGBC
Patients with IGBC who underwent re-resection were separated into three subgroups according to the time interval from the date of initial cholecystectomy to the date of radical resection: A (<2 weeks), B (2–4 weeks), and C (>4 weeks). Table 3 shows the comparative analyses of clinicopathological factors across these three subgroups. There was no difference in baseline demographics or tumor-related factors between the three subgroups (P > 0.05 for all). The 5-year OS was comparable among groups A, B, and C (P > 0.05 for all) (Figure 3A), as was DFS (P > 0.05 for all) (Figure 3B).
 |
Table 3 Clinicopathologic Features of Patients with Incidental Gallbladder Carcinoma Stratified by Time Interval of Treatment After Initial Resection |
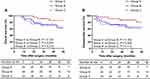 |
Figure 3 (A) Overall survival of IGBC patients stratified by the time interval of repeat resection; (B) disease-free survival of IGBC patients stratified by the time interval of repeat resection. |
Patients with IGBC were further divided into two groups based on the presence or absence of the risk factors associated with early recurrence. For patients with IGBC with risk factors, the 5-year OS of group B was significantly higher than that of the groups A and C (P < 0.05) (Figure 4A), and the 5-year DFS in group B was significantly higher than that in groups A and C (P < 0.05 for both) (Figure 4B). For patients with IGBC without the risk factors associated with early recurrence, OS and DFS were not significantly different among the groups (P > 0.05 for all) (Figure 4C and D).
Discussion
Radical surgery aiming to achieve R0 resection is the only curative treatment for GBC. However, because of its aggressive local infiltration and early metastasis, the prevalence of postoperative recurrence of GBC has been reported to be 25–65%.7,21 Several studies have demonstrated the association between early recurrence and poor prognosis for patients with hepatobiliary carcinoma.9–11 Although the recurrence patterns of patients with GBCs after R0 resection have been revealed in some studies, little is known about the predictive factors of early recurrence.
Our cohort comprised patients with GBC with T1b–T3 disease who had undergone R0 resection. We calculated 29 months as being the optimal cutoff to distinguish early recurrence from late recurrence. Perhaps unsurprisingly, the 5-year OS of patients in the early recurrence group was significantly shorter than that of patients in the late recurrence group. In addition, early recurrence tended to occur in a location distal to the primary tumor, whereas regional recurrence was more prevalent in the late recurrence group. This phenomenon has been demonstrated in other cancer types, but until now, it has not been reported for GBC.10,22
Sahara et al evaluated patients with GBC with T1–T4 disease and found that major hepatectomy was a prognostic factor for early recurrence when compared with minor hepatectomy involving segments IVB/V.12 In our cohort, however, major hepatectomy failed to remain a risk factor of early recurrence for patients with GBC with T1b–T3 disease. This inconsistency could reflect the variation in patient selection. As mentioned above, cholecystectomy alone is sufficient for GBC of stage T1a, whereas radical resection for a T4 lesion is controversial,23 thus neither of these two stages were included in our cohort. Besides, a subset of patients with stage T1b–T2 disease underwent hepatic wedge resection in our institute, whereas in the study by Sahara et al, minor hepatectomy referred solely to resection of IVB/V segments.12 Kwon et al24 demonstrated that patients with T2 lesions who had wedge resection of liver tissue around the gallbladder bed had comparable long-term survival to those who underwent resection of hepatic IVB/V segments. Therefore, wedge resection and resection of IVB/V segments were classified as “partial hepatectomy” in our study, and patients who underwent partial hepatectomy had a similar prevalence of early recurrence as those who had major hepatectomy. The scope of liver resection for GBC should be performed according to the T stage. We hypothesized that it is the T stage, rather than the scope of liver resection, that affects the risk of early recurrence in patients with GBC. We also discovered that the tumors in the early-recurrence group had more advanced T categories than those in the non-early-recurrence group. This result emphasized the importance of an adequate scope of resection to achieve long-term survival of patients with GBC.
To date, most guidelines for GBC have recommended routine follow-up with a 3-month interval during the first 2 years after curative-intent therapy, and a 6-month interval thereafter, up to 5 years.25,26 However, there is no research supporting a specific surveillance schedule for patients with GBC nor has there been any study focusing on the impact of regular follow-up on prognosis. The present study demonstrated that more than 80% of recurrence occurred within 29 months after resection (early recurrence), typically in a location distant from the primary tumor site. Therefore, a more intense follow-up schedule in the first 2.5 years after surgery might be required for patients with T1–T3 stage GBC with early-recurrence-related risk factors, namely T3 stage, N1/N2 stage, positive LI, and poor differentiation.
GBC that is diagnosed by pathology during or after resection for a presumed benign disease is defined as IGBC and accounts for about 50–70% of all cases of GBC.27,28 Avoidance of a secondary surgical procedure requires frozen-section histopathology during cholecystectomy; however, this is not feasible for all hospitals in view of the increased medical expenditure and operative time.29 For IGBC diagnosed postoperatively, few studies have focused on the timing of repeat resection. For example, the timing of radical resection after initial treatment has been studied in cancers of the esophagus and rectum, yet the primary focus has been on the timing between resection and neoadjuvant therapy.30,31 A multicenter study suggested that the optimal time interval for IGBC diagnosed postoperatively is 4–8 weeks.32 He et al33 showed that patients with IGBC diagnosed postoperatively at an interval of 2–4 weeks had a longer OS than those with an interval of <2 weeks or >4 weeks. However, in our study, there was no significant difference between groups A, B, and C. Notably, important risk factors, such as T stage, N stage, differentiation, and LI, were also similar among the subgroups. When excluding patients without the risk factors of early recurrence, patients with IGBC in group B had longer survival than those in group A and group C. We assumed that for IGBC with the risk factors of early recurrence, a time interval <2 weeks might not be sufficient to evaluate and stage the tumors due to misinterpretation of frozen section analysis and imaging analysis in the setting of acute inflammation, whereas IGBC with time interval >4 weeks might carry a higher risk of tumor dissemination. The two aspects mentioned above might have contributed to early recurrence and resulted in a worse prognosis. For patients with IGBC without any of the risk factors of early recurrence, the prognoses of patients in groups A, B, and C were comparable. Hence, these patients did not benefit from preoperative imaging or a timely secondary surgical procedure to the same extent as those with risk factors. In brief, this finding emphasizes the gravity of complete preoperative tumor evaluation and timely performance of radical resection, especially for those with potential risk factors. However, a significant bias might have been present in the survival analyses of the time interval because the number of patients in the three subgroups was small. A better definition of the correct timing of a secondary surgical procedure following cholecystectomy requires additional research.
Our study had three main limitations. First, it had a retrospective design, comprising data from a single tertiary center, whereas data from a multi-institution analysis would be less biased and more reliable. Second, some vital clinicopathological information was not recorded and analyzed in our study. The location of a T2 tumor, for instance, has been shown to be an important prognostic factor;34 however, this was absent from our histology reports. Third, only 39 patients with IGBC had the risk factors for early recurrence; therefore, a larger scale study is needed to identify the variables that determine the optimal timing of a secondary surgical procedure.
Conclusions
T3 stage, N1–N2 stage, poor differentiation, and LI were identified as independent risk factors associated with early recurrence in patients with GBC with stage T1b–T3 disease after R0 resection. IGBC patients with risk factors undergoing re-resection between 2 and 4 weeks after the initial cholecystectomy had superior survival compared with those within 2 weeks or beyond 4 weeks. Moreover, intense follow-up schedule might be recommended for those with early-recurrence-related risk factors in the first 2.5 years after surgery.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval Statement
Ethical approval for this retrospective research was obtained from the institutional review board of West China Hospital of Sichuan University. Written informed consent was waived because of the retrospective design of the study. This study was conducted in accordance with the Declaration of Helsinki, and all patient data were kept confidential.
Consent for Publication
The authors confirm that the details of any images, videos, recordings, etc. can be published, and that the person(s) providing consent have been shown the article contents to be published.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare no competing interests.
References
1. Ertel AE, Bentrem D, Abbott DE. Gall bladder cancer. Cancer Treat Res. 2016;168:101–120.
2. Choi KS, Choi SB, Park P, Kim WB, Choi SY. Clinical characteristics of incidental or unsuspected gallbladder cancers diagnosed during or after cholecystectomy: a systematic review and meta-analysis. World J Gastroenterol. 2015;21(4):1315–1323. doi:10.3748/wjg.v21.i4.1315
3. Fuks D, Regimbeau JM, Le Treut YP, et al. Incidental gallbladder cancer by the AFC-GBC-2009 study group. World J Surg. 2011;35(8):1887–1897. doi:10.1007/s00268-011-1134-3
4. Pawlik TM, Gleisner AL, Vigano L, et al. Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. J Gastrointest Surg. 2007;11(11):
5. Sahara K, Tsilimigras DI, Maithel SK, et al. Survival benefit of lymphadenectomy for gallbladder cancer based on the therapeutic index: an analysis of the US extrahepatic biliary malignancy consortium. J Surg Oncol. 2020;121(3):503–510. doi:10.1002/jso.25825
6. Engineer R, Goel M, Chopra S, et al. Neoadjuvant chemoradiation followed by surgery for locally advanced gallbladder cancers: a new paradigm. Ann Surg Oncol. 2016;23(9):3009–3015. doi:10.1245/s10434-016-5197-0
7. Jarnagin WR, Ruo L, Little SA, et al. Patterns of initial disease recurrence after resection of gallbladder carcinoma and hilar cholangiocarcinoma: implications for adjuvant therapeutic strategies. Cancer. 2003;98(8):1689–1700. doi:10.1002/cncr.11699
8. Wang X, Yu GY, Chen M, Wei R, Chen J, Wang Z. Pattern of distant metastases in primary extrahepatic bile-duct cancer: a SEER-based study. Cancer Med. 2018;7(10):5006–5014. doi:10.1002/cam4.1772
9. Imamura H, Matsuyama Y, Tanaka E, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38(2):200–207. doi:10.1016/S0168-8278(02)00360-4
10. Zhang XF, Beal EW, Bagante F, et al. Early versus late recurrence of intrahepatic cholangiocarcinoma after resection with curative intent. Br J Surg. 2018;105(7):848–856. doi:10.1002/bjs.10676
11. Groot VP, Gemenetzis G, Blair AB, et al. Defining and predicting early recurrence in 957 patients with resected pancreatic ductal adenocarcinoma. Ann Surg. 2019;269(6):1154–1162. doi:10.1097/SLA.0000000000002734
12. Sahara K, Tsilimigras DI, Kikuchi Y, et al. Defining and predicting early recurrence after resection for gallbladder cancer. Ann Surg Oncol. 2021;28(1):417–425. doi:10.1245/s10434-020-09108-y
13. Mizuno T, Ebata T, Yokoyama Y, et al. Major hepatectomy with or without pancreatoduodenectomy for advanced gallbladder cancer. Br J Surg. 2019;106(5):626–635. doi:10.1002/bjs.11088
14. Kohn N, Maubach J, Warschkow R, et al. High rate of positive lymph nodes in T1a gallbladder cancer does not translate to decreased survival: a population-based, propensity score adjusted analysis. HPB. 2018;20(11):1073–1081. doi:10.1016/j.hpb.2018.05.007
15. Aloia TA, Jarufe N, Javle M, et al. Gallbladder cancer: expert consensus statement. HPB. 2015;17(8):681–690. doi:10.1111/hpb.12444
16. Lee SE, Kim KS, Kim WB, et al. Practical guidelines for the surgical treatment of gallbladder cancer. J Korean Med Sci. 2014;29(10):1333–1340. doi:10.3346/jkms.2014.29.10.1333
17. Han HS, Yoon YS, Agarwal AK, et al. Laparoscopic surgery for gallbladder cancer: an expert consensus statement. Dig Surg. 2019;36(1):1–6. doi:10.1159/000486207
18. Yoon YS, Han HS, Agarwal A, et al. Survey results of the expert meeting on laparoscopic surgery for gallbladder cancer and a review of relevant literature. Dig Surg. 2019;36(1):7–12. doi:10.1159/000486208
19. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi:10.1097/01.sla.0000133083.54934.ae
20. Im JH, Lee WJ, Kang CM, Hwang HK, Seong J. Prognostic factors and patterns of loco-regional failure in patients with R0 resected gallbladder cancer. HPB. 2020;22(8):1168–1173. doi:10.1016/j.hpb.2019.10.2447
21. Kim WS, Choi DW, You DD, Ho CY, Heo JS, Choi SH. Risk factors influencing recurrence, patterns of recurrence, and the efficacy of adjuvant therapy after radical resection for gallbladder carcinoma. J Gastrointest Surg. 2010;14(4):679–687. doi:10.1007/s11605-009-1140-z
22. Zhang XF, Beal EW, Chakedis J, et al. Defining early recurrence of hilar cholangiocarcinoma after curative-intent surgery: a multi-institutional study from the US extrahepatic biliary malignancy consortium. World J Surg. 2018;42(9):2919–2929. doi:10.1007/s00268-018-4530-0
23. Hari DM, Howard JH, Leung AM, Chui CG, Sim MS, Bilchik AJ. A 21-year analysis of stage I gallbladder carcinoma: is cholecystectomy alone adequate? HPB. 2013;15(1):40–48. doi:10.1111/j.1477-2574.2012.00559.x
24. Kwon W, Kim H, Han Y, et al. Role of tumour location and surgical extent on prognosis in T2 gallbladder cancer: an international multicentre study. Br J Surg. 2020;107(10):1334–1343.
25. Valle JW, Borbath I, Khan SA, et al. Biliary cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v28–v37. doi:10.1093/annonc/mdw324
26. Gomez-Espana MA, Montes AF, Garcia-Carbonero R, et al. SEOM clinical guidelines for pancreatic and biliary tract cancer (2020). Clin Transl Oncol. 2021;23(5):988–1000. doi:10.1007/s12094-021-02573-1
27. Ethun CG, Postlewait LM, Le N, et al. A novel pathology-based preoperative risk score to predict locoregional residual and distant disease and survival for incidental gallbladder cancer: a 10-institution study from the U.S. extrahepatic biliary malignancy consortium. Ann Surg Oncol. 2017;24(5):1343–1350. doi:10.1245/s10434-016-5637-x
28. Kim JH, Kim WH, Kim JH, Yoo BM, Kim MW. Unsuspected gallbladder cancer diagnosed after laparoscopic cholecystectomy: focus on acute cholecystitis. World J Surg. 2010;34(1):114–120. doi:10.1007/s00268-009-0279-9
29. Jayasundara JA, de Silva WM. Histological assessment of cholecystectomy specimens performed for symptomatic cholelithiasis: routine or selective? Ann R Coll Surg Engl. 2013;95(5):317–322. doi:10.1308/003588413X13629960046471
30. Franko J, Voynov G, Goldman CD. Esophagectomy timing after neoadjuvant therapy for distal esophageal adenocarcinoma. Ann Thorac Surg. 2016;101(3):1123–1130. doi:10.1016/j.athoracsur.2015.09.044
31. Huntington CR, Boselli D, Symanowski J, Hill JS, Crimaldi A, Salo JC. Optimal timing of surgical resection after radiation in locally advanced rectal adenocarcinoma: an analysis of the national cancer database. Ann Surg Oncol. 2016;23(3):877–887.
32. Ethun CG, Postlewait LM, Le N, et al. Association of optimal time interval to re-resection for incidental gallbladder cancer with overall survival: a multi-institution analysis from the US extrahepatic biliary malignancy consortium. JAMA Surg. 2017;152(2):143–149. doi:10.1001/jamasurg.2016.3642
33. He S, Yu T, Khadaroo PA, et al. A comparison between the prognosis of simultaneous and salvage radical resection in incidental gallbladder cancer. Cancer Manag Res. 2020;12:13469–13478. doi:10.2147/CMAR.S286292
34. Shindoh J, de Aretxabala X, Aloia TA, et al. Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Ann Surg. 2015;261(4):733–739. doi:10.1097/SLA.0000000000000728
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


