Back to Journals » Clinical Interventions in Aging » Volume 15
Predicting Adverse Outcomes in Healthy Aging Community-Dwelling Early-Old Adults with the Timed Up and Go Test
Authors Batko-Szwaczka A , Wilczyński K , Hornik B , Janusz-Jenczeń M , Włodarczyk I, Wnuk B , Szołtysek J , Durmała J , Szuster-Kowolik K , Antoniak-Sobczak K , Dulawa J , Szewieczek J
Received 31 March 2020
Accepted for publication 26 June 2020
Published 31 July 2020 Volume 2020:15 Pages 1263—1270
DOI https://doi.org/10.2147/CIA.S256312
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Agnieszka Batko-Szwaczka,1 Krzysztof Wilczyński,1 Beata Hornik,2 Magdalena Janusz-Jenczeń,2 Iwona Włodarczyk,2 Bartosz Wnuk,3 Joanna Szołtysek,3 Jacek Durmała,3 Karolina Szuster-Kowolik,1 Katarzyna Antoniak-Sobczak,1 Jan Dulawa,4 Jan Szewieczek1
1Department of Geriatrics, Faculty of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland; 2Department of Internal Nursing, Faculty of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland; 3Department of Rehabilitation, Faculty of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland; 4Department of Internal Medicine and Metabolic Diseases, Faculty of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland
Correspondence: Agnieszka Batko-Szwaczka
Department of Geriatrics, Faculty of Health Sciences in Katowice, Medical University of Silesia, GCM, Ul. Ziolowa 45/47, Katowice 40-635, Poland
Tel +48323598239
Fax +48322059483
Email [email protected]
Background: Simple, easy-to-perform, safe and cost-effective methods for the prediction of adverse outcomes in older adults are essential for the identification of patients who are most likely to benefit from early preventive interventions.
Methods: The study included 160 community-dwelling individuals aged 60– 74 years, with 44.4% women. A comprehensive geriatric assessment was performed in all participants. Bioimpedance body composition analysis included 149 subjects. Among other tests, functional assessment included the Barthel Index of Activities of Daily Living (Barthel Index), Mini-Mental State Examination (MMSE), Timed Up and Go (TUG) and Fried frailty phenotype. Follow-up by telephone was made after at least 365 days. The composite endpoint (CE) included fall, hospitalization, institutionalization and death.
Results: Cohort characteristics: age 66.8± 4.2 years (mean±SD), 3.81± 2.23 diseases, 4.29± 3.60 medications or supplements, and good functional status (MMSE 29.0± 1.5, Barthel Index 98.1± 8.2, prevalence of Fried frailty phenotype 2.5%). During one-year follow-up, 34 subjects (21.3%; 95% confidence interval [CI] =14.9− 27.6%) experienced CE: hospitalizations (13.8%; 95% CI=8.41− 19.1), falls (9.38%; 95% CI=4.86− 13.9), death (0.63%; 95% CI=0− 1.85) and no institutionalization. A higher probability of CE was associated with age ≥ 70 years (P=0.018), taking any medication or supplements (P=0.007), usual pace gait speed ≤ 0.8 m/s (P=0.028) and TUG > 9 s (P< 0.002). TUG was the only independent measure predicting one-year CE occurrence (OR=1.22, 95% CI=1.07− 1.40, P=0.003) in multivariate logistic regression. However, its predictive power was poor; the area under the receiver operating characteristic curve was 0.659 (95% CI 0.551− 0.766, P=0.004) and Youden’s J statistic for a TUG cut-off of 9.0 s was 0.261 (sensitivity 0.618 and specificity 0.643).
Conclusion: The TUG test was superior to frailty phenotype measures in predicting one-year incidence of a CE consisting of fall, hospitalization, institutionalization and death in a cohort of healthy-aging community-dwelling early-old adults, although its value as a stand-alone test was limited.
Keywords: frailty phenotype, community-dwelling older adults, healthy aging, comprehensive geriatric assessment, Timed Up and Go test
Introduction
Population aging has profound implications for the planning and delivery of health and social care. Falls, hospitalization, institutionalization and death are among the most serious adverse health outcomes of age-associated multimorbidity and frailty.1,2 Simple, easy-to-perform, safe and cost-effective methods of predicting increased risk of adverse outcomes in older adults are essential for the early identification of patients who may benefit from preventive interventions.1,3 Owing to the diverse rate of biological aging and age-associated multimorbidity, the prediction of negative outcomes is difficult or impossible based on the diagnosis of medical conditions alone.4,5 The concept of frailty, a geriatric syndrome that reflects the complex nature of age-associated multidimensional functional decline, is regarded as the most promising method of identifying geriatric patients who would benefit from preventive interventions.2,6 Epidemiological investigations show associations between different frailty models and adverse health outcomes in community-dwelling, institutionalized and hospitalized older adults. However, standardization of concepts and measures of frailty models are still lacking, and models used for epidemiological studies are not necessarily useful for routine clinical practice in primary care.2,3,6 Furthermore, the same frailty model may not be applicable to patients with different health status.7 Comprehensive geriatric assessment (CGA), a standard assessment of patients in geriatric medicine units, takes into account the multidimensional nature of health determinants of older people.2–4,6 CGA is a multidisciplinary, coordinated method that addresses the physical, mental, medical and social needs of an older person with frailty.2 The frailty index is predictive of adverse outcomes in older people and may be derived from CGA.3 However, the practical limitations of CGA are time and an interdisciplinary team being required for completion of the process.2 In our previous study, we explored the prevalence of prefrailty and frailty phenotype in early-old community-dwelling inhabitants of southern Poland, and examined conditions associated with frailty assessment components.8 In this paper, we analyze the usefulness of frailty phenotype components and other functional measures for one-year adverse outcome prediction.
Participants and Methods
A detailed description of patient enrolment and the study methodology was included in our previous paper.8 Therefore, we present here an abridged description of the study group and measurements.
Participants
The study group consisted of 160 subjects, 71 (44.4%) women, randomized from community-dwelling 60–74-year-old inhabitants of southern Poland. To achieve this number of participants, invitation letters were sent to 4963 people randomized out of 843,278 relevant candidates for the study. A response was received from 163 invitees, of whom 160 gave written consent for participation in the project. The only exclusion criterion was lack of informed consent for participation in this study.
Measurements
A CGA was complemented with frailty phenotype and body mass assessment, as described in our previous paper.8 A structured patient history included indicators of morbidity, specific signs of geriatric conditions, chronic disease, pharmacological treatment, alcohol consumption, smoking, living conditions, and family or social service support. Physical examination included general status, body build, mental status, speech, vision, hearing, gait, resting blood pressure of both arms, pulse, body mass, height, and waist and hip circumference.
The Charlson Comorbidity Index9 was used to assess multimorbidity. The Berlin Initiative Study (BIS) creatinine equation10 was used to estimate glomerular filtration rate (eGFR). The Barthel Index of Activities of Daily Living (Barthel Index)11 and Instrumental Activities of Daily Living Scale (IADL)12 were used to determine functional independence. The Mini-Mental State Examination (MMSE)13 was used to assess global cognitive performance. The Geriatric Depression Scale – Short Form (GDS-SF) was used to screen for depression.14
Tinetti Performance-Oriented Mobility Assessment (Performance-Oriented Mobility Assessment, POMA)15 and Timed Up and Go (TUG) test were used to evaluate fall risk.16 Equipment for the TUG includes a standard armchair (approximate seat height 45 cm), a stopwatch and a 3-m-long walking path, extended by another ≥1 m in length (0.5 m for the chair and 0.5 m to enable an easy 180-degree-turn at the 3 m mark), making a minimum of 4 m combined. The test subject, wearing regular footwear, was instructed to get up from the chair upon a verbal command, walk at a comfortable and safe pace to a line on the floor 3 m away, then turn, return to the chair and sit down again. Walking aids were permitted if previously utilized by the patient, but no caregiver assistance was allowed. A practice trial preceded the timed test. The average time to provide TUG patient instruction, a test run and a timed run was 2 min 30 s. The 6-Minute Walk Test (6MWT) was used as an integrated measure of aerobic capacity, endurance and functional exercise performance, and consisted of measuring the total distance the subject walked in 6 min.17,18
Frailty was diagnosed using three different phenotype approaches: (1) Fried et al criteria;19 (2) Saum et al criteria based on predefined cut-off values;20 and (3) modified Saum et al criteria,20 with cut-off values based on the lowest-quintile approach of our cohort for weakness, slowness, physical activity and ≥5% one-year unintentional weight loss in the cohort (mean and median values of grip strength, usual pace walking speed and physical activity were presented in our previous paper8). For assessment of physical activity, Saum et al20 used a modified version of the Physical Activity Questionnaire for the Elderly (PAQE)21 instead of the Minnesota Leisure Time Activity Questionnaire22,23 used by Fried et al.19 Equipment required to complete the Fried frailty phenotype (FFP) assessment includes a grip strength dynamometer, a stopwatch, a 4.57-m-long walking path prolonged by another ≥2 m, making a minimum of 7.0 m, medical weight and a standard chair with arms. The average time to complete FFP assessment in fit subjects (including instructions for the patient, measurement of handgrip strength [three repetitions], usual pace walking speed [two repetitions], measurement of body weight and calculating 12-month body weight change, completion of the exhaustion self-report questionnaire and data collection for the Modified Minnesota Leisure Time Activity Questionnaire with weekly kilocalorie expenditure calculation) was 20 min.
Body mass index (BMI) and waist to hip ratio (WHR) were calculated for all subjects. Body composition analysis was performed in 149 subjects with the use of Tanita BC-418MA Body Composition Analyzer and Tanita Viscan Analyzer AB140, as described in our previous paper.8 The examination was not performed in 11 subjects: eight subjects had contraindications to the measurement of bioelectrical impedance (any metal implants in the body), two subjects were not tested owing to equipment failure, and one subject had difficulty maintaining an upright position. Subjects were examined at the Department of Geriatrics of the Leszek Giec Upper-Silesian Medical Centre of the Silesian Medical University in Katowice on an outpatient basis or at the patient’s home if they were unable to ambulate to our medical facilities. Follow-up by telephone call was made at least 365 days after the initial examination. The composite endpoint (CE) included fall, hospitalization, institutionalization and death.
Statistical Analysis
Data were analyzed using Statistica version 13 (StatSoft Polska). The non-parametric Mann–Whitney U-test for quantitative variables, and chi-squared test, V-squared test and Fisher’s exact test for categorical variables, were used. The Kaplan–Meier method was used to estimate one-year CE-free probability for subjects classified according to age, total number of medications and supplements, usual pace gait speed and TUG, while differences between these subgroups were assessed with the Wilcoxon–Gehan statistic. Different cut-off values were tested to define the value corresponding to the lowest P-level. Multivariate logistic regression was used to assess measures associated with CE incidence. Analysis with backward elimination included variables with P-values of 0.1 or lower in the initial univariate analysis. Collinearity of independent variables was eliminated before odds ratio (OR) calculation. The receiver operating characteristics (ROC) curve was used to evaluate the predictive value of the TUG for one-year CE occurrence and to determine an optimal TUG threshold for predicting CE incidence. P values <0.05 were considered statistically significant.
Ethics
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Bioethical Committee of the Medical University of Silesia in Katowice, Poland (Letter KNW/0022/KB1/1/14).
Results
The cohort was characterized by a mean±SD age of 66.8±4.2 years, mean number of 3.81±2.23 diseases or comorbidities (with predominant osteoarthritis and hypertension), and mean number of 4.29±3.60 medicine or supplements used by the participants (Table 1). Nevertheless, functional status was good, as indicated by the high MMSE score of 29.0±1.5 and Barthel Index of 98.1±8.2, low (2.5%) prevalence of frailty phenotype according to the Fried at al criteria, and other functional measures (Table 2).
 |
Table 1 Cohort Clinical Characteristics Organized by Incidence of Composite Endpoint (Fall, Hospitalization Institutionalization or Death) Within One Year |
 |
Table 2 Cohort Functional Characteristics Organized by Incidence of the Composite Endpoint (Fall, Hospitalization, Institutionalization or Death) Within One Year |
During the one-year follow-up, 34 subjects (21.3%; 95% confidence interval [CI] =14.9−27.6%) experienced CE: 15 subjects (9.38%; 95% CI=4.86−13.9) experienced falls, 22 subjects (13.8%; 95% CI=8.41−19.1) were hospitalized and one subject (0.63%; 95% CI=0−1.85) died. No institutionalization was reported during this time. Study participants who experienced CE were characterized by advanced age, increased number of medications and supplements, lower diastolic blood pressure (Table 1), higher incidence of Saum et al frailty criterion for slowness and worse TUG and 6MWT results (Table 2).
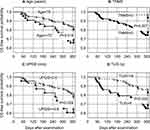
According to the Wilcoxon–Gehan test, a higher probability of one-year CE occurrence was associated with age ≥70 years (P=0.018), taking any medication or supplement (P=0.007), usual pace gait speed ≤0.8 m/s (P=0.028) and TUG >9 s (P<0.002) (Figure 1).
TUG was the only independent measure predicting one-year CE occurrence (OR=1.22, 95% CI=1.07−1.40, P=0.003) in multivariate logistic regression analysis adjusted for age, sex, disease prevalence, number of medications, functional tests (Barthel Index, IADL, MMSE, GDS-SF, frailty phenotype components, prefrailty and frailty phenotype), BMI, bioimpedance body composition scores and blood tests. However, evaluated with the ROC curve, the predictive value of TUG for CE incidence was poor: the area under the curve was 0.659 (95% CI=0.551−0.766, P=0.004) and Youden’s J statistic for a TUG cut-off of 9.0 s was 0.261 (sensitivity 0.618 and specificity 0.643).
Discussion
We assessed the predictive value of different clinical and functional measures over a one-year period for adverse events in community-dwelling early-old adults. As we discussed in our previous paper, the functional status of study participants was better than would be expected from other studies. Despite randomization, owing to sampling bias, our sample was most likely not representative of the general population of early-old adults of our region.8 Maintaining functional ability that enables well-being in older age is defined by the World Health Organization as healthy aging.4 In the context of this definition, our cohort may be considered as representative of healthy-aging older adults.
Increased occurrence of CE over a one-year period was associated with age of 70 or more years, taking any medicine or supplement, usual pace gait speed of 0.8 m/s or lower and TUG over 9 s.
An association between age and risk for adverse outcomes has been shown in multiple studies.1–4
The relationship between pharmacological treatment and risk of CE is complex. Adverse drug reactions (ADRs) account for significant morbidity in elderly patients.24,25 One in ten hospital admissions of older patients is due to ADRs.26 Psychotropic medications and polypharmacy increase the risk of falling.27 However, disease, rather than the medication prescribed for a particular disease, should be considered the primary risk factor for adverse outcomes. Our sample power is not sufficient to allow for analysis of associations between pharmacological treatment and adverse outcomes. However, along with other studies,24,25 our clinical observations support the general principle of avoiding polypharmacy.
In line with other studies,4,5 our results also support the thesis that functional tests, rather than the diagnosis of any single disease, may be predictive of adverse outcomes in the elderly. In this study, TUG was the only independent measure predictive of one-year incidence of CE, albeit with poor ROC performance. The power of TUG in predicting CE was nonetheless superior to frailty phenotype measures in this cohort. Previous studies have evaluated the usefulness of the TUG to assess risk for adverse outcomes in elderly adults, and especially the risk for falls. A systematic review and meta-analysis demonstrated that TUG (at a cut-off value of 13.5 s) has limited value for fall prediction in community-dwelling elderly people.28 A more recent systematic review and meta-analysis concluded that no single test or measure demonstrated significant value for the post-test fall probability of community-dwelling older adults. However, the Berg Balance Scale (≤50 points), TUG (≥12 s) and Five Times Sit to Stand scores (≥12 s) were the best evidence-based functional measures for determining individual fall risk.29 A prospective study of community-dwelling elderly in China showed that TUG (using a cut-off point of 15.96 s) can predict recurrent falls in community-dwelling elderly individuals aged 67.4±5.6 years.30 The TUG did not predict falls in another group of 192 community-dwelling older adults aged 73.0±6.2 years.31 Discrepancies in the results obtained from different studies may be explained by the fact that TUG performance may be influenced by multiple factors, among them age, sex and cognitive impairment.32 Since the TUG inherently incorporates gait at usual speed, we can also consider an umbrella review that demonstrated good predictive ability of gait speed assessment and development of disability in activities of daily living.33 Compared to gait assessment alone, TUG incorporates more complex functions: rising from a sitting position, changes in gait direction and re-sitting.16 Compared with frailty phenotype assessment, TUG requires less equipment and less time. By some accounts, assessment of the FFP takes approximately 15–20 min (a single patient encounter for testing all Fried frailty components), although less than 10 min for assessment was also reported.3 In our experience, frailty phenotype assessment in a fit older adult requires approximately 20 min, while TUG requires about 2 min. Functional assessment for preventive purposes in elderly patients in routine outpatient counseling is strongly indicated.1 However, the increased time burden may discourage both patient and clinician participation in rigorous frailty assessment.34 Implementation of complex and time-consuming geriatric assessments is not feasible owing to the ever increasing pressures for short patient encounters. Simple and short functional tests seem more likely to be incorporated into health service provider routines. Unfortunately, no single such test is available with strong predictive properties for adverse outcomes in elderly community-dwelling adults. The ROC performance of the TUG for predicting CE in this cohort was also poor. While the TUG may not represent the highest predictive ability, its simplicity suggests that further studies may be warranted. Despite the limitations of our study, namely a small number of subjects and limited follow-up time, we achieved statistically significant results that may suggest future research directions.
Conclusion
The TUG test was superior to frailty phenotype measures in predicting one-year incidence of a CE consisting of fall, hospitalization, institutionalization and death in a cohort of healthy-aging community-dwelling early-old adults, although its value as a stand-alone test was limited.
Disclosure
The authors report no conflicts of interest in this work.
References
1. O’Caoimh R, Cornally N, Weathers E, et al. Risk prediction in the community: a systematic review of case-finding instruments that predict adverse healthcare outcomes in community-dwelling older adults. Maturitas. 2015;82:3–21. doi:10.1016/j.maturitas.2015.03.009
2. Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394:1376–1386. doi:10.1016/S0140-6736(19)31785-4
3. Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med. 2016;31:3–10. doi:10.1016/j.ejim.2016.03.007
4. World Health Organization. Healthy ageing. World Report on Ageing and Health. 2015:25–39 Available from: https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=2805CBB1B9DFF3E1461AD185273315A6?sequence=1.
5. Lordos EF, Herrmann FR, Robine JM, et al. Comparative value of medical diagnosis versus physical functioning in predicting the 6-year survival of 1951 hospitalized old patients. Rejuvenation Res. 2008;11:829–836. doi:10.1089/rej.2008.0721
6. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375. doi:10.1016/S0140-6736(19)31786-6
7. Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–397. doi:10.1016/j.jamda.2013.03.022
8. Batko-Szwaczka A, Dudzińska-Griszek J, Hornik B, et al. Frailty phenotype: evidence of both physical and mental health components in community-dwelling early-old adults. Clin Interv Aging. 2020;15:141–150. doi:10.2147/CIA.S238521
9. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi:10.1016/0021-9681(87)90171-8
10. Schaeffner ES, Ebert N, Delanaye P, et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Ann Intern Med. 2012;157:471–481. doi:10.7326/0003-4819-157-7-201210020-00003
11. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:56–61.
12. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3 Part 1):179–186. doi:10.1093/geront/9.3_Part_1.179
13. Folstein MF, Folstein SE, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi:10.1016/0022-3956(75)90026-6
14. Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–173. doi:10.1300/J018v05n01_09
15. Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126. doi:10.1111/jgs.1986.34.issue-2
16. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi:10.1111/j.1532-5415.1991.tb01616.x
17. Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80:837–841. doi:10.1016/s0003-9993(99)90236-8
18. Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128–137. doi:10.1093/ptj/82.2.128
19. Fried LP, Tangen CM, Walston J, et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol Med Sci. 2001;56A:M146–M156. doi:10.1093/gerona/56.3.M146
20. Saum KU, Müller H, Stegmaier C, Hauer K, Raum E, Brenner H. Development and evaluation of a modification of the Fried frailty criteria using population-independent cutpoints. J Am Geriatr Soc. 2012;60:2110–2115. doi:10.1111/j.1532-5415.2012.04192.x
21. Voorrips LE, Ravelli AC, Dongelmans PC, Deurenberg P, Van Staveren WA. A physical activity questionnaire for the elderly. Med Sci Sports Exerc. 1991;23:974–979. doi:10.1249/00005768-199108000-00015
22. Taylor HL, Jacobs DR
23. Siscovick DS, Fried L, Mittelmark M, Rutan G, Bild D, O’Leary DH. Exercise intensity and subclinical cardiovascular disease in the elderly. The Cardiovascular Health Study. Am J Epidemiol. 1997;145:977–986. doi:10.1093/oxfordjournals.aje.a009066
24. By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel; Fick DM, Semla TP, Steinman M, et al. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67:674–694. doi:10.1111/jgs.15767
25. O’Mahony D. STOPP/START criteria for potentially inappropriate medications/potential prescribing omissions in older people: origin and progress. Expert Rev Clin Pharmacol. 2020;13:15–22. doi:10.1080/17512433.2020.1697676
26. Oscanoa TJ, Lizaraso F, Carvajal A. Hospital admissions due to adverse drug reactions in the elderly. A meta-analysis. Eur J Clin Pharmacol. 2017;73:759–770. doi:10.1007/s00228-017-2225-3
27. Park H, Satoh H, Miki A, Urushihara H, Sawada Y. Medications associated with falls in older people: systematic review of publications from a recent 5-year period. Eur J Clin Pharmacol. 2015;71(12):1429–1440. doi:10.1007/s00228-015-1955-3
28. Barry E, Galvin R, Keogh C, et al. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr. 2014;14(1):14. doi:10.1186/1471-2318-14-14
29. Lusardi MM, Fritz S, Middleton A, et al. Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. J Geriatr Phys Ther. 2017;40:1–36. doi:10.1519/JPT.0000000000000099
30. Kang L, Han P, Wang J, et al. Timed Up and Go Test can predict recurrent falls: a longitudinal study of the community-dwelling elderly in China. Clin Interv Aging. 2017;12:2009–2016. doi:10.2147/CIA.S138287
31. Mulasso A, Roppolo M, Gobbens RJ, Rabaglietti E. Mobility, balance and frailty in community-dwelling older adults: what is the best 1-year predictor of falls? Geriatr Gerontol Int. 2017;17:1463–1469. doi:10.1111/ggi.12893
32. Ibrahim A, Singh DKA, Shahar S. ‘Timed Up and Go’ test: age, gender and cognitive impairment stratified normative values of older adults. PLoS One. 2017;12:e0185641. doi:10.1371/journal.pone.0185641
33. Apóstolo J, Cooke R, Bobrowicz-Campos E, et al. Predicting risk and outcomes for frail older adults: an umbrella review of frailty screening tools. JBI Database System Rev Implement Rep. 2017;15:1154–1208. doi:10.11124/JBISRIR-2016-003018
34. Pritchard JM, Kennedy CC, Karampatos S, et al. Measuring frailty in clinical practice: a comparison of physical frailty assessment methods in a geriatric out-patient clinic. BMC Geriatr. 2017;17:264. doi:10.1186/s12877-017-0623-0
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.