Back to Journals » Clinical Ophthalmology » Volume 17
Posterior Segment Ocular Findings in HLA-B27 Positive Patients with Uveitis: A Retrospective Analysis
Authors Or C, Lajevardi S, Ghoraba H, Park JH, Onghanseng N, Halim MS , Hasanreisoglu M, Hassan M, Uludag G, Akhavanrezayat A , Nguyen QD
Received 15 February 2023
Accepted for publication 17 April 2023
Published 1 May 2023 Volume 2023:17 Pages 1271—1276
DOI https://doi.org/10.2147/OPTH.S408728
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Chris Or,1 Sherin Lajevardi,1 Hashem Ghoraba,1 Jung Hyun Park,1 Neil Onghanseng,1,2 Muhammad Sohail Halim,1 Murat Hasanreisoglu,3 Muhammad Hassan,1 Gunay Uludag,1 Amir Akhavanrezayat,1 Quan Dong Nguyen1
1Department of Ophthalmology, Stanford University, Palo Alto, CA, USA; 2Department of Ophthalmology, Makati Medical Center, Manila, Philippines; 3Department of Ophthalmology, Koç University, School of Medicine, Istanbul, Turkey
Correspondence: Quan Dong Nguyen, Spencer Center for Vision Research, Byers Eye Institute at Stanford University, 2370 Watson Court, Suite 200, Palo Alto, CA, 94303, USA, Tel +1 650 725 7245, Email [email protected]
Purpose: To describe the prevalence and characteristics of posterior segment manifestations in patients with HLA-B27-associated uveitis using wide field imaging.
Methods: Medical records of patients diagnosed with HLA-B27-associated uveitis from a tertiary uveitis clinic were reviewed. Posterior segment involvements including but not limited to peripheral vasculitis, optic disc inflammation, and macula edema documented based on medical records and various imaging modalities including wide field fluorescein angiography and optical coherence tomography, were noted. Demographic characteristics, accompanied with systemic diseases as well as duration and chronicity of uveitis, were also evaluated. Patients with significant systemic and ocular comorbidities were excluded. Statistical analyses including chi-squared tests and paired t-tests were employed.
Results: Of the 44 patients with HLA-B27 associated uveitis, 22 patients (50%) were noted to demonstrate posterior segment involvement. Disc leakage and peripheral vasculitis were the most common findings of posterior involvement. Those with anterior chamber inflammation were found to have a significantly increased risk of posterior involvement. Those with posterior involvement were also noted to have a statistically significant decreased visual acuity. No significant association was found between documented duration of disease and posterior segment involvement.
Conclusion: The prevalence of posterior segment involvement in HLA-B27 associated uveitis is higher compared to previous reports when evaluated with wide angle imaging modalities. Careful examination of the posterior segment is required in patients with HLA-B27 associated uveitis.
Keywords: HLA-B27, uveitis, retinal vasculitis, vitreous haze, vitreous cells, macular edema, anterior chamber cells, anterior chamber flare
Introduction
Human leukocyte antigen B27 (HLA-B27) associated uveitis is the most common cause of noninfectious uveitis worldwide.1,2 It typically presents as unilateral acute anterior uveitis (AU) and rarely, may be bilateral at onset. Recurrences usually involve the same eye with approximately a third of patients experiencing alternating AU.3 Long-term visual outcomes are generally favorable.4 Though it usually follows a benign course, about 20% of cases may progress to develop into chronic uveitis, which increases the risks of ocular complications such as cataracts and glaucoma up to sevenfold compared to patients with other causes of acute AU.5,6 HLA-B27 positivity has also been linked to increased risks for systemic diseases such as spondyloarthropathy, ankylosing spondylitis, psoriatic arthritis, and inflammatory bowel diseases often necessitating the need for collaboration with other specialties in the patient’s management.1,7,8 Furthermore, the presence of concurrent systemic disease may also increase risks of complications.1,2,6
Posterior segment disease, aside from cystoid macular edema (CME), has been reported to be associated with HLA-B27 positivity and includes vitritis, optic disc edema, and vasculitis, both diffuse and peripheral.1,4 Gastrointestinal involvement has been shown to have a greater predilection to develop posterior segment disease with reports demonstrating a spectrum from peripheral vasculitis to frosted branch angiitis.8,9 A recent review demonstrated that 23.1% of HLA-B27 patients included in the study had some forms of posterior segment involvement, using routine posterior segment imaging techniques, with vitritis, CME and retinal vasculitis being the most reported.10 Such finding was of particular importance as patients with posterior segment involvement were both less responsive to conventional therapy and more likely to progress to recurrent or chronic disease.10 A review by Rodriguez and Foster likewise showed a high proportion (17.4%) of HLA-B27-associated uveitis patients having posterior segment disease demonstrated by routine imaging with vitritis, papillitis, and retinal vasculitis being the most encountered. The authors suggested that the presence of posterior segment disease in HLA-B27 patients may necessitate a more aggressive course of therapy.2 Overall, there is a paucity of studies investigating the prevalence of posterior segment involvement in HLA-B27-associated uveitis and studies that have been done did not utilize wide field imaging. Therefore, we aim to perform a retrospective analysis to determine the prevalence and various clinical characteristics of posterior segment involvement in HLA-B27-associated uveitis using wide field imaging techniques.
Methodology
All patients diagnosed with HLA-B27 associated uveitis from 2018 to 2022 at a single tertiary referral uveitis clinic with at least one follow up visit in 1 year were retrospectively reviewed and included in this cross-sectional study. Patients found to have existing comorbidities that may present with posterior segment manifestations such as age-related macular degeneration, retinopathy secondary to diabetes or hypertension, tuberculosis, sarcoidosis, cytomegalovirus, herpes simplex or juvenile rheumatoid arthritis were excluded. Patients who have a history of intraocular procedures, retinal laser procedures or significant ocular trauma were also excluded. Patients with other known infectious and non-infectious causes of uveitis were excluded.
All patients underwent a complete ophthalmologic evaluation including best-corrected visual acuity (BCVA), slit-lamp examination, fundus examination, color fundus photography (Carl Zeiss Meditec Inc., Jena, Germany), ultrawide field fundus photography (WAFP) and fluorescein angiography (WAFA) (OPTOS Plc, Dunfermline, UK), Heidelberg Spectralis spectral domain optical coherence tomography (OCT) (Heidelberg Engineering, Heidelberg, Germany) at the initial visit to be included to our study. Demographic data including age, sex, race were collected, as well as clinical information such as the visual acuity (converted to logMAR), laterality of disease, and history of systemic illness correlated to HLA-B27 positivity, if any, were collected. Information regarding their uveitis, including its location, time course and severity, was also collected. Posterior segment involvements including but not limited to peripheral retinal vasculitis, optic disc inflammation seen as staining and/or leakage and macula edema were documented based on medical records and various imaging modalities including WAFA and OCT.
The study was conducted in compliance with the Declaration of Helsinki, the United States Code of Federal Regulations Title 21, and the Harmonized Tripartite Guidelines for Good Clinical Practice (1996). Stanford University institutional review board approved the study, and an informed consent waiver was obtained as the charts of enrolled patients were retrospectively reviewed. Confidentiality of patient data was maintained.
Statistical analyses were performed including chi-squared tests and paired t-tests, comparing the various metrics collected between the group that had posterior involvement against the group that did not.
Results
Forty-four HLA-B27 patients (80 eyes) were included in the study. Of the 44 patients, 12 patients (28%) were female. Caucasian (34%) and Asian (30%) were the most common races. Demographical and clinical information are summarized in Table 1. Mean age of all patients is 39.2 with a standard deviation of 14.
 |
Table 1 Demographical and Clinical Information Among the Study Population |
Of these 44 patients, 22 patients (50%) were noted with posterior manifestations of uveitis. Seven of the 22 patients (32%) were female. Anterior chamber cell was present in 18 out of 44 patients (41%) and anterior chamber flare was present in 28 out of 44 patients (64%). Of the ones with anterior chamber cell, 13 out of 22 eyes had posterior involvement, whilst in those without anterior chamber cell, 16 out of 58 eyes had posterior involvement. The most common presenting signs were disc leakage (41%) and peripheral vasculitis (32%) followed by vitreous cells (7%), vitreous haze (5%), and macular edema (5%) (Table 2). A representative case is demonstrated in Figure 1. Six patients (27%) demonstrated bilateral involvements. Mean age of those with posterior segment inflammation was 37 and those without was 41.9. No significant relationship was found between age and presence of posterior segment inflammation (p = 0.26).
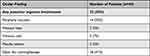 |
Table 2 Posterior Segment Findings in Patients with HLA-B27 Associated Uveitis |
 |
Figure 1 Fundus photo (A) and late phase fluorescein angiography (B) of a representative case of HLA-B27 uveitis with peripheral vasculitis and optic nerve inflammation, as depicted by the arrows. |
Analysis regarding the presence of HLA-B27 associated systemic diseases and its relationship with posterior involvements was also performed (Table 3). Most of the patients in our group had a diagnosis of ankylosing spondylitis (n = 17). No patients in our cohort had Reiter syndrome (Reactive Arthritis) or inflammatory bowel diseases. No relationship was found between the presence of any seronegative spondyloarthropathies and the presence of posterior segment inflammation (Table 3).
 |
Table 3 Sub-Analysis of Patients with Known HLA-B27 Associated Systemic Diseases and Its Relationship with Posterior Segment Involvement on Ocular Imaging and Examination |
There is no significant relationship between posterior segment involvement and duration of ocular disease (p = 0.13). However, those with posterior segment inflammation presented with a shorter duration of disease in our cohort with a mean duration of 6.4 years, whereas those without posterior segment inflammation had a mean duration of 11.59 years. There is also no relationship between the presence of retinal vasculitis or optic disc inflammation and duration of ocular disease (p = 0.44 and 0.25, respectively).
Patients with posterior segment inflammation had a statistically significant decrease in visual acuity compared to those without posterior segment inflammation (p = 0.03). Patients with the presence of anterior chamber (AC) cell or flare are also significantly associated with the presence of posterior segment inflammation (p = 0.02 for AC cell and p = 0.01 for AC flare).
Discussion
Posterior segment involvement in patients with HLA-B27 associated uveitis is reported to be a relatively uncommon condition, with previous studies reporting a prevalence of 17.4 to 23.1%.2,10 The use of wide-field imaging has gained popularity since its induction and has allowed for the proper assessment of the extent of posterior segment disease in patients with uveitis. In our current study, 50% of HLA-B27 positive patients presented with posterior segment involvement, with the most common presenting signs of posterior involvement being optic disc inflammation and peripheral vasculitis followed by vitreous haze, vitreous cells, and macular edema. Previous studies noted that the most common form of posterior segment involvement is vitritis, followed by papillitis and cystoid macular edema.2 The frequency of retinal vasculitis varied depending on study but ranged from 21.7 to 24% of cases, which is lower compared to our results.2,10,11 The use of wide-field imaging likely allowed for the detection of more peripheral findings, namely peripheral retinal vasculitis as demonstrated in Figure 1, which increased the incidence of posterior segment involvement seen in our cohort compared to previously reported studies. Our finding reinforces the necessity of wide-field imaging in patients with HLA-B27 associated uveitis. It should be noted that previous reports of optic nerve inflammation was only noted as papillitis, reported to be present in approximately 14% of cases in a case series by Rodriguez et al2 The proportion of patients in our cohort with optic nerve inflammation was significant higher at 41%, as we included cases with both optic nerve staining and leakage, which may also have contributed to our noted increase in individuals with posterior segment findings.
In keeping with previous reports,2 our results suggest that HLA-B27 positive patients with posterior segment involvement have a lower visual acuity than those without posterior segment involvement, further underscoring the importance of its detection and subsequent proper management. Our study also noted that investigation into posterior segment involvement should especially be considered in patients with active AC inflammation, in whom rates of posterior segment involvement was significantly increased over those without AC inflammation.
In our study, there is no relationship between presence of systemic disease including ankylosing spondylitis and posterior segment involvement. This result is in contrast to a previous report citing that the presence of associated systemic diseases was significantly associated with posterior segment involvement.11 However, Yang et al noted retrospectively that HLA-B27 positive patients with or without ankylosing spondylitis had similar rates of peripheral vasculitis on FA imaging, which is in keeping with our current study.12 Further investigations are required to clearly elucidate this finding.
There are several limitations in our study. As all subjects included were seen in our tertiary referral center, our results may not fully represent the general population with HLA-B27 associated uveitis. The retrospective nature of our study has its associated limitations. Another limitation is that follow-up data were not collected as part of this cross-sectional study. Another limitation is our small number of patients included, which may not have been fully representative of the entire population of patients with HLA-B27 associated uveitis. Another limitation would be our expanded definition of optic nerve inflammation, which may limit the ability to compare our results to those reported previously. Further studies will be conducted to assess the response to therapy in our cohort and its effects on the posterior segment involvement observed.
In conclusion, posterior segment involvement may be present in up to 50% of patients with HLA-B27 associated uveitis. Advancements in wide-field imaging have allowed for a more complete assessment into the extent of posterior segment involvements, likely resulting in the increased proportion of patients with posterior segment involvement in our current study when compared to previous studies. Patients with HLA-B27 associated uveitis with posterior segment involvement are known to have worse visual prognosis, which was also supported by our current study. Careful assessment into the presence of posterior segment involvements should be considered in all patients with HLA-B27 uveitis, particularly in those with active AC inflammation.
PPI Statement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Ethics Approval
The study was conducted in accordance with the Declaration of Helsinki. Approval for retrospective studies was obtained from the IRB committee of the Stanford University (IRB-68008). All data was anonymized and maintained with confidentiality.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
Dr Muhammad Hassan reports Consultant for Alumis, outside the submitted work. All involved authors do not report a competing interest with the contents of this article.
References
1. Pathanapitoon K, Dodds EM, Cunningham ET, Rothova A. Clinical spectrum of HLA-B27-associated ocular inflammation. Ocul Immunol Inflamm. 2017;25(4):569–576. doi:10.1080/09273948.2016.1185527
2. Rodriguez A, Akova YA, Pedroza-Seres M, Foster CS. Posterior segment ocular manifestations in patients with HLA-B27-associated uveitis. Ophthalmology. 1994;101(7):1267–1274. doi:10.1016/S0161-6420(94)31179-1
3. Agnani S, Choi D, Martin TM, et al. Gender and laterality affect recurrences of acute anterior uveitis. Br J Ophthalmol. 2010;94(12):1643–1647. doi:10.1136/bjo.2009.172312
4. Rothova A, van Veenedaal WG, Linssen A, Glasius E, Kijlstra A, de Jong PT. Clinical features of acute anterior uveitis. Am J Ophthalmol. 1987;103(2):137–145. doi:10.1016/S0002-9394(14)74218-7
5. Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS. Outcomes in anterior uveitis associated with the HLA-B27 haplotype. Ophthalmology. 1998;105(9):1646–1651. doi:10.1016/S0161-6420(98)99033-9
6. Loh AR, Acharya NR. Incidence rates and risk factors for ocular complications and vision loss in HLA-B27-associated uveitis. Am J Ophthalmol. 2010;150(4):534–42 e2. doi:10.1016/j.ajo.2010.04.031
7. Juanola X, Loza Santamaria E, Cordero-Coma M, Group SW. Description and prevalence of spondyloarthritis in patients with anterior uveitis: the SENTINEL interdisciplinary collaborative project. Ophthalmology. 2016;123(8):1632–1636. doi:10.1016/j.ophtha.2016.03.010
8. Calvo P, Pablo L. Managing IBD outside the gut: ocular manifestations. Dig Dis. 2013;31(2):229–232. doi:10.1159/000353375
9. Sykes SO, Horton JC. Steroid-responsive retinal vasculitis with a frosted branch appearance in Crohn's disease. Retina. 1997;17(5):451–454. doi:10.1097/00006982-199717050-00017
10. Kim SJ, Chung H, Yu HG. Posterior segment involvement in Korean patients with HLA-B27-associated uveitis. Ocul Immunol Inflamm. 2009;17(1):26–32. doi:10.1080/09273940802553261
11. Dodds EM, Lowder CY, Meisler DM. Posterior segment inflammation in HLA-B27+ acute anterior uveitis: clinical characteristics. Ocul Immunol Inflamm. 1999;7(2):85–92. doi:10.1076/ocii.7.2.85.4015
12. Yang P, Wan W, Du L, et al. Clinical features of HLA-B27-positive acute anterior uveitis with or without ankylosing spondylitis in a Chinese cohort. Br J Ophthalmol. 2018;102(2):215–219. doi:10.1136/bjophthalmol-2016-309499
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Reactive Arthritis Triggered by Adalimumab and Leflunomide in a Patient with Ankylosing Spondylitis
Liu Y, He J, Jiang J, Wang Y, Liu T
Clinical, Cosmetic and Investigational Dermatology 2022, 15:2601-2605
Published Date: 2 December 2022
