Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
Post-Traumatic Stress Disorder and Coping Strategies Among People with HIV in Lira District, Uganda: A Cross-Sectional Study
Authors Arebo B, Ewach GF, Omara J, Oyella P, Aciro Lucky R, Kabunga A
Received 15 March 2022
Accepted for publication 26 May 2022
Published 30 May 2022 Volume 2022:14 Pages 255—264
DOI https://doi.org/10.2147/HIV.S358575
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Benedict Arebo,1 Gracious Faith Ewach,2 Jacob Omara,3 Pamella Oyella,1 Ruth Aciro Lucky,4 Amir Kabunga4
1Department of Nursing and Midwifery, Lira University, Lira City, Uganda; 2Department of Public Health, Lira University, Lira City, Uganda; 3Faculty of Medicine, Gulu University, Gulu city, Uganda; 4Department of Psychiatry, Faculty of medicine, Lira University, Lira City, Uganda
Correspondence: Amir Kabunga, Department of Psychiatry, Faculty of medicine, Lira University, Lira City, Uganda, Email [email protected]
Background: Post-traumatic stress disorder (PTSD) is the most commonly reported mental health consequence following traumatic events. However, little is known about how people with HIV cope with the PTSD burden in Lira city, northern Uganda.
Materials and Methods: This study was carried out in Lira District Health Centre IVs from February 10, 2022, to March 10, 2022. A facility-based cross-sectional study was employed among 390 people with HIV attending Lira Health Centre IVs. A consecutive sampling technique was used to select the sample size. Questionnaires were used to collect data. A binary logistic regression model was fitted to identify factors associated with independent variables, and AOR was employed to estimate the strength of association between independent and dependent variables.
Results: Results show that the estimated prevalence of PTSD was 254 (65.1%) and was higher among the females 191 (75.2%), those with no formal education 143 (56.3%), aged 40 years and above 121 (47.6%), and married 127 (50.0%). Results indicate that male respondents had a 51% reduced odds of developing PTSD burden compared to female respondents (AOR: 0.49; 95% CI: 0.30– 0.81; P = 0.005). Individuals who did not use planning activities as a coping strategy had more than 2-fold increased odds of experiencing PTSD compared to those who planned activities (AOR: 2.43; 1.26– 4.70; P = 0.008). Participants who did not have emotional support had close to 3-fold increased chances of developing PTSD compared to those who had emotional support (AOR: 2.94; 1.74– 4.98; P ≤ 0.001). Participants who indicated they were not taking recourse to spirituality had more than 4-fold increased odds of experiencing PTSD compared to those who had spirituality (AOR: 4.40; 1.83– 10.46; P = 0.001).
Conclusion: A considerable burden of PTSD among HIV clients attending health centre IVs in Lira District was notably higher and was associated with gender, planning activities, emotional support and spirituality. Early screening of PTSD among HIV clients is needed to alleviate the burden. There is also a need to include PTSD treatment services in the treatment programme of HIV care services in health centre IVs in Lira District.
Keywords: coping strategies, HIV, mental health, post-traumatic stress disorder
Background
The burden of the HIV pandemic remains a complex reality.1 First, there is not yet a tangible breakthrough in the world of medical research culminating in the successful discovery of HIV cure.1 Second, HIV infection is known for its tendency to present with neuropsychiatric disorders including Post-Traumatic Stress Disorder (PTSD).2 PTSD is a health concern and sub-Saharan Africa, which is home to more than one-third of all people living with HIV, is disproportionately affected.3 The prevalence of PTSD among people with HIV (PWH) varies across studies, ranging from 10% to 74%,2 which is higher than those recorded among the general population.4 While the levels of PTSD in sub-Saharan Africa are significantly higher, few studies have examined PSTD5 and have indicated a degree of heterogeneity in the results.3 Additionally, few studies have focused on coping strategies among PWH.
PTSD is a trauma-related disorder that is characterized by re-experiencing, avoidance, negative cognition and mood and arousal for at least one month.6 PTSD is particularly relevant to HIV because being diagnosed with HIV, a life-threatening illness is a potentially traumatic event and PTSD may emerge as a result of the diagnosis.7 On receiving the diagnosis of HIV, infected people may experience intrusive thoughts of illness or death and may try to avoid people, activities, and places that remind them of the illness.8 PTSD is more common among PWH compared with the general population.9 The pooled prevalence of PTSD across 10 countries in low-income countries was 22%3 which was significantly higher than 4% of lifetime PTSD recorded in 25 countries in high-income countries.10 Studies indicate that the risk factors for PTSD symptomatology include HIV-related physical symptoms, history of pre-HIV trauma, less perceived support and, a greater degree of stigma.11
Considerable evidence has shown that PTSD covaries with poor HIV clinical outcome, nonadherence to medical interventions, substance use disorder, depression, physical dysfunction, and risky sexual behaviours.12 Additionally, there is evidence indicating that PTSD may lead to HIV disease progression characterized by significant CD4 decline.13 Given that PTSD is associated with disease progression, its identification and treatment among PWH have vast potential clinical and public health benefits.12 Studies show that PWH who receive mental health services have higher rates of ARV utilization, better viral control, and a lower risk of early mortality.14 Despite the high prevalence of HIV-related PTSD and the World Health Organization (WHO) recommendations to integrate mental health needs in HIV care, little is known about coping strategies among PWH in low-income countries.9
Coping is an active effort to reduce, master or tolerate the demands of stress,15 involving several behavioural and cognitive strategies. Although researchers are yet to reach an agreement on the categories of coping styles,16 some suggest classifying coping based on the purpose and intentions of different coping behaviours.17 In light of the purpose of different behaviours, PWH’s coping can be divided into two types: approach coping and avoidant coping.17 Approach coping that aims to directly address the stressors includes behaviours such as emotional support, problem-solving and cognitive restructuring. On the other hand, avoidant coping means behaviours that aim to avoid stressful situations including blaming, social withdrawal, denial, and disengagement. There is evidence to show that coping strategies are related to the quality of life18 and improved mental health.19 Consistent with this, one study demonstrated that relying on emotional support reduced the impact of PTSD.20 However, studies targeting PTSD in PWH indicate that coping styles vary from culture to culture.21 Additionally, these studies have produced inconsistent findings due to the complex nature of the relationship between stressors, coping strategies, and mental health.22
PTSD is prevalent among PWH in Uganda. A recent study in southwestern Uganda among PWH indicated that 28.3% and 27.3% had symptoms of PTSD of avoidance and nightmare, respectively.5 Notably, this study focused on the prevalence of PTSD and not coping strategies. The incidence of PTSD is likely to be higher in northern Uganda. The region has experienced political upheavals for more than two decades and it is still experiencing the aftermath of this traumatic exposure.23 This may be a double tragedy among PWH living in northern Uganda. There is, however, little evidence of the prevalence and how PWH cope with PTSD in the region. In addition, interventions promoting coping should align with cultural context to provide PWH with the appropriate skills in response to their social environment.24 Thus, this study assessed PTSD and coping strategies among PWH in rural northern Uganda.
Materials and Methods
Study Setting
This study was conducted at ART clinics in health centre IVs in the Lira District. Lira District is located in the Lango sub-region. The district is bordered by Pader District to the north, Otuke District to the northeast, Alebtong District to the east, Dokolo District to the southeast, Apach District to the southwest, and Kole District to the west. It is located approximately 337 Kilometers by road, north of Kampala, Uganda’s capital city. Lira District was chosen because of the high patient load.25
Research Design
A facility-based cross-sectional research design using a quantitative approach was used for this study. Data was collected from three health centre IVs between February 10, 2022, to March 10, 2022.
Study Participants and Sample Size Estimation
The study population included PWH seeking care in Lira district health centre IVs. The accessible population was 3002 HIV-positive clients attending three ART clinics in Lira health centre IVs. These included 1300 PWH attending Ogur Health Centre IV, 997 attending Amach Health Centre IV and 705 attending Ober Health Centre IV. The sample size was calculated using Yamane’s table for sample size determination.26 The calculated sample is 388 plus a 10% allowance for nonresponse.
Sampling Criteria
To ensure representativeness, a proportionate sampling technique was used to obtain the sample from each health centre. Thus, 168 participants were selected from Ogur Health Centre IV, 129 were selected from Amach Health Centre IV and 91 were selected from Ober Health Centre IV. We used the consecutive random sampling techniques to select the representative samples. All participants meeting the inclusion criteria and available during the clinic days were recruited. Adults aged 18 years and above were eligible for recruitment. Pregnant women in their last trimester and women within the 3-month postnatal period were excluded.
Data Collection Instruments
Interviewer-administered questionnaires were used to collect data. An English version of PTSD Checklist Civilian Version (PCL-C-5) was used to measure PTSD symptoms among PWH. PCL-C-5 consists of 17 items, which comprise three domains: reexperiencing, avoidance, and hyperarousal.27 The three domains correspond to the DSM-IV symptoms for PTSD27 on a 5 Likert scale based on the extent to which the respondent has been troubled by specific symptoms in the past month. The total possible score is calculated by summing up the scores for all the items, and it ranges from 17 to 85 points. A total score of ≥50 indicates a full diagnosis.28 However, a cut-off of 44 points was associated with increased specificity and sensitivity, which improved diagnostic efficacy.28 In this study, the traumatic event in the original PCL-C-5 is replaced by HIV/AIDS. Nineteen studies assessed total score internal consistency and returned values above 0.75.29 In this study, the Cronbach's alpha for PCL-C was 0.84. The first section of the questionnaire is researcher-made and seeks to capture demographic data including gender, age, educational background, and marital status.
Coping responses to PTSD were assessed using researcher-developed items. These items were chosen from a review of the literature. Based on the previous studies on coping with PTSD, items used to collect data were adapted. The items were reviewed and adjusted accordingly before data collection. Eight questions on information support, active coping, planning activities, emotional support, spirituality, acceptance, denial and substance abuse were used to evaluate the respondents’ coping styles. The questions were: 1) Have you done something about the situation you are in and taken action to try to make the situation better? 2) Have you got help and advice from other people about what to do regarding your problem? 3) Have you come up with a strategy about what to do and what steps to take regarding your problem? 4) Have you got emotional support and comfort from other people? 5) Have you accepted the reality of the fact that it has happened and thought hard about what steps to take? 6) Have you been praying or meditating to find comfort in your spiritual beliefs? 7) Have you said to yourself “this is not real and refused to believe that it has happened? 8) Have you been using alcohol or other drugs to make yourself feel better? The items were pretested on a sample of 38 respondents attending HIV clinic at Aboke Health Centre IV. After pre-testing, ambiguous items or questions were omitted. The items were measured independently with yes or no responses.
Procedures
Four research assistants were trained in preparation for data collection. We visited the health centres on HIV/AIDs clinic days; waiting for the prospective participants who were asked to be part of the study. Participants were enrolled after receiving their medical services without inconveniencing the daily routine. Those who consented were recruited into the study. The purpose of the study, the methods of data collection, and the time frame for the study were explained to the participants before data collection. Informed consent forms were hand-delivered by the researchers to the prospective respondents. The researcher-administered tools were then distributed to the respondents who agreed to be part of the study.
Statistical Analysis
At the end of data collection, the field tools were reviewed for completeness. Data were entered in duplicate into Excel. We cleaned the data, coded it, and then exported it into the SPSS V-23. After entering the data, the statistical command (list) under the analyzed data by the SPSS software was used to identify the missing data at entry. Mistakes in the entry were identified through validation and corrected by recalling the questionnaire using its unique identifier.
Descriptive statistics, including frequencies, percentages, and measures of central tendency and dispersion, were used to analyze and summarize data. Chi-Square test was used to test for association. Binary logistic and multiple regression analyses were used to predict the independent variable of PTSD. Crude odds ratios (COR) and adjusted odds ratios (AOR) and their 95% CI were calculated. P-value ≤0.05 was considered to be statistically significant.
Ethical Approval and Consent to Participation
This study was conducted per the declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board (IRB) of Gulu University (GUREC-2021-164). All participants provided written informed consent. Participation was voluntary, and no form of coercion was used. The data collected were confidential and anonymous with no information like names linking the study participants to the data. The COVID-19 protocols were strictly maintained throughout data collection. The respondents without masks were provided with masks. Sanitisers were available and social distancing was maintained.
Results
Results in Table 1 show that of the total 390 respondents, 178 (45.6%) were aged between 40 years and above, 268 (68.7%) were females, 215 (55.1%) were married and, 207 (53.1%) had no formal education. In this study (Table 2) the estimated prevalence of PTSD was 254 (65.1%) and was higher among the females 191 (75.2%), those with no formal education 143 (56.3%), aged 40 years and above 121 (47.6%) and, married 127 (50.0%). Also, results in Table 1 indicate that gender (p=<0.001), education levels (p = 0.018) and marital status (p = 0.013) were associated with PTSD.
 |
Table 1 Socio-Demographic Characteristics of 390 HIV Positive Clients |
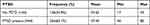 |
Table 2 Prevalence of PTSD |
Coping Strategies and Post-Traumatic Stress
Binary logistic regression analysis (Table 3) was conducted to identify potential factors. The elevated levels of PTSD symptoms were more likely to be associated with planning activities (p=<0.001), emotional support (p=<0.001, active coping (p = 0.037), information support (p=<0.001) and spirituality (p=<0.001).
 |
Table 3 Coping Strategies and Post-Traumatic Stress |
Multivariable Analysis
The multivariate logistic regression analysis (Table 4) was conducted on the potential variables significantly and independently associated with PTSD at a p-value of <0.05. Results indicate that male respondents had a 51% reduced odds of developing PTSD burden compared to female respondents (AOR: 0.49; 95% CI: 0.30–0.81; P = 0.005). Individuals who did not use planning activities as a coping strategy had more than 2-fold increased odds of experiencing PTSD compared to those who planned activities (AOR: 2.43; 1.26–4.70; P = 0.008). Participants who received no emotional support had close to 3-fold increased chances of developing PTSD compared to those who had emotional support (AOR: 2.94; 1.74–4.98; P ≤ 0.001). Participants who indicated they were not taking recourse to spirituality had more than 4-fold increased odds of experiencing PTSD compared to those who had spirituality (AOR: 4.40; 1.83–10.46; P = 0.001).
 |
Table 4 Multivariable Logistic Regression Analysis |
Discussion
We evaluated coping strategies and PTSD among HIV-positive clients in Lira District. Our findings demonstrated that 65.1% of the respondents reported PTSD. This result may not be surprising because some of the respondents are trauma survivors facing unique challenges related to two decades of conflicts in northern Uganda.23 This may be a double tragedy among HIV-positive clients living in the region. In addition, being diagnosed with HIV, a life-threatening illness is potentially traumatic and is likely to increase the risk of developing PTSD.7 In line with our results, the prevalence of PTSD in HIV-infected patients is higher than that in the general population,30 varying between 10% and 74%31 compared to 3.9% in the general population.10 Comparable rates of PTSD have been reported in other studies indicating the rates of HIV-related PTSD ranging from 15% to 64%.32 The PTSD prevalence reported in our study is higher than 55.3% in Zimbabwe33 and 22% reported from a meta-analysis of data from 10 counties in sub-Saharan Africa.3 This difference may be attributed to regional differences in experiences of PTSD, social support, historical context and self-evaluation.34 The present results underscore the importance of early assessment and trauma-directed mental health interventions for HIV clients.
Our results indicated male respondents had a 51% reduced odds of developing PTSD burden compared to female respondents (AOR: 0.49; 95% CI: 0.30–0.81; P = 0.005). We can infer that females are more vulnerable to PTSD than males. This may be attributed to the fact that HIV-positive females have significant trauma exposure history before, during and following diagnosis.14 It may also be attributed to women being more likely to experience gender-based violence and stigma.11 Our findings are consistent with earlier studies, which found that HIV-positive women were twice as likely as HIV-positive men to develop PTSD.30 Similarly, in a study in Rwanda, three of five HIV-positive women met the criteria for PTSD.35 Also consistent with our findings, HIV-positive women in Canada, British Columbia and Ontario experienced high levels of PTSD.36
The current study investigated the relationship between planning activities as a coping strategy and PTSD in HIV positive clients. The results showed that individuals who did not use planning activities as a coping strategy had more than 2-fold increased odds of experiencing PTSD compared to those who planned activities (AOR: 2.43; 1.26–4.70; P = 0.008). Planning activities as a coping style involve focusing on a certain behaviour to alleviate the mental health burden.37 Studies have shown that individuals using planning activities report lower levels of mental health issues.37 Scott and colleagues added that generally planning activities coping strategy is associated with reduced mental health distress.38 Our results corroborate the findings of Simon and Ng, who established that HIV-positive clients in New York used planning activities more frequently than avoidant strategies.39
Our results revealed that participants who did not have emotional support had close to 3-fold increased odds of developing PTSD compared to those who had emotional support (AOR: 2.94; 1.74–4.98; P ≤ 0.001). Emotional support involves genuine encouragement, reassurance and compassion from family members, friends, healthcare providers or spiritual leaders. Emotional support received from close family and friends helps individuals after traumatic events to express negative emotions, which is crucial in reducing mental health issues like PTSD.40 The present findings suggest that emotional support is more important for HIV-positive clients experiencing PTSD symptoms. The amount of perceived emotional support displayed may facilitate the use of more adaptive traumatic coping strategies.40 The results of the current study are consistent with other studies demonstrating that relying on emotional support is an important coping strategy for people suffering from PTSD.20 Our findings highlight the importance of setting in place a therapeutic action based on emotional support to address risk-associated responses. Further, the help of an empathetic counsellor may be of great importance.41
Our findings showed that participants who indicated they were not taking recourse to spirituality as a coping strategy had more than 4-fold increased odds of developing PTSD compared to those who had spirituality (AOR: 4.40; 1.83–10.46; P = 0.001). Literature on HIV-positive clients emphasises the role of spirituality as an essential coping strategy in overcoming trauma and hardship.42 People tend to use spirituality to gain comfort and protection.43 Thus, PTSD may motivate HIV-positive clients to seek support in spirituality.44 Spirituality promotes hope and acceptance for the greater well-being of HIV-positive clients.45 The positive association between spirituality and well-being in HIV-positive clients is based on the assumption that spirituality is the source of recovery of meaning in life, social support and coping strategy.45 Studies show that spirituality determines well-being and allows individuals to better process traumatic experiences to better cope with PTSD symptoms.42 In line with our results, studies suggest that spiritual factors contribute to high levels of satisfaction with life in HIV-positive clients.45 Spiritual coping was also significantly associated with life satisfaction and reduced PTSD in HIV-positive clients.46 Contrary to our results, other studies have proved that HIV-positive clients rarely return to spirituality as a form of coping with HIV-related trauma.47
Strength and Limitations of the Study
The findings of this study provide evidence about the relationship between coping strategies and PTSD among HIV-positive adults in the rural Ugandan context. This is a cross-sectional study and may not establish a causal correlation. The results may not be generalizable due to geographical limitations. Items measuring coping strategies were researcher-generated and future research may be needed to validate measures of coping strategies. Lastly, PTSD was determined using a self-report rating scale and diagnosis was not confirmed using a clinician administered instrument.
Conclusion
A considerable burden of PTSD among HIV clients attending health centre IVs in Lira District was notably higher and was associated with gender, planning activities, emotional support and spirituality. Early screening of PTSD among HIV clients is needed to alleviate the burden. There is also a need to include PTSD treatment services in the treatment programme of HIV care services in health centre IVs in Lira District. Further studies on similar population are needed to replicate their findings.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors wish to acknowledge the participants included in this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit it to the current journal; gave final approval for the version to be published; and agreed to be accountable for all aspects of the work.
Funding
Research reported in this publication was supported by the Fogarty International Center (US Department of State’s Office of the US Global AIDS Coordinator and Health Diplomacy [S/GAC] and the President’s Emergency Plan for AIDS Relief [PEPFAR]) of the National Institutes of Health under Award Number R25TW011210. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure
The authors declared no conflicts of interest in relation to this work and no potential conflict of interest concerning the research and/or publication of the article.
References
1. Adina JO, Maritim EK, Sindabi AM, Disiye MA. Effect of cognitive behaviour therapy on depressive symptoms among HIV-infected outpatients in Kenya. Int J Psychol Psychological Therapy. 2017;17(2):161–173.
2. Applebaum AJ, Bedoya CA, Hendriksen ES, Wilkinson JL, Safren SA, O’Cleirigh C. Future directions for interventions targeting PTSD in HIV-infected adults. J Assoc Nurses AIDS Care. 2015;26(2):127–138.
3. Ng LC, Stevenson A, Kalapurakkel SS, et al. National and regional prevalence of posttraumatic stress disorder in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med. 2020;17(5):e1003090.
4. Neigh GN, Rhodes ST, Valdez A, Jovanovic T. PTSD co-morbid with HIV: separate but equal, or two parts of a whole? Neurobiol Dis. 2016;92:116–123.
5. Kekibiina A, Adong J, Fatch R, et al. Post-traumatic stress disorder among persons with HIV who engage in heavy alcohol consumption in southwestern Uganda. BMC Psychiatry. 2021;21(1):1–9.
6. Compean E, Hamner M. Posttraumatic stress disorder with secondary psychotic features (PTSD-SP): diagnostic and treatment challenges. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:265–275.
7. Tang C, Goldsamt L, Meng J, et al. Global estimate of the prevalence of post-traumatic stress disorder among adults living with HIV: a systematic review and meta-analysis. BMJ open. 2020;10(4):e032435.
8. Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: risk factors for chronicity. Am J Psychiatry. 1992;1:874.
9. Verhey R, Chibanda D, Brakarsh J, Seedat S. Psychological interventions for post‐traumatic stress disorder in people living with HIV in Resource poor settings: a systematic review. Tropical Med Int Health. 2016;21(10):1198–1208.
10. Koenen K, Ratanatharathorn A, Ng L, et al. Posttraumatic stress disorder in the world mental health surveys. Psychol Med. 2017;47(13):2260–2274.
11. Katz S, Nevid JS. Risk factors associated with posttraumatic stress disorder symptomatology in HIV-infected women. AIDS Patient Care STDS. 2005;19(2):110–120.
12. McLean CP, Fitzgerald H. Treating posttraumatic stress symptoms among people living with HIV: a critical review of intervention trials. Curr Psychiatry Rep. 2016;18(9):1–9.
13. Ebrahimzadeh Z, Goodarzi MA, Joulaei H. Predicting the antiretroviral medication adherence and CD4 measure in patients with HIV/AIDS based on the post traumatic stress disorder and depression. Iran J Public Health. 2019;48(1):139.
14. Machtinger EL, Wilson T, Haberer JE, Weiss DS. Psychological trauma and PTSD in HIV-positive women: a meta-analysis. AIDS Behav. 2012;16(8):2091–2100.
15. Wang J-L, Jackson LA, Zhang D-J, Su Z-Q. The relationships among the Big Five Personality factors, self-esteem, narcissism, and sensation-seeking to Chinese University students’ uses of social networking sites (SNSs). Comput Human Behav. 2012;28(6):2313–2319.
16. Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull. 2001;127(1):87.
17. Connor-Smith JK, Compas BE. Vulnerability to social stress: coping as a mediator or moderator of sociotropy and symptoms of anxiety and depression. Cognit Ther Res. 2002;26(1):39–55.
18. Côté J, Delmas P, Delpierre C, Sylvain H, Delon S, Rouleau G. Factors related to quality of life in treatment-adherent, successfully treated HIV Patients in France. Open Nurs J. 2009;3:10.
19. Armon C, Lichtenstein K. The associations among coping, nadir CD4+ T-cell count, and non-HIV-related variables with health-related quality of life among an ambulatory HIV-positive patient population. Quality Life Rese. 2012;21(6):993–1003.
20. Ogińska-Bulik N, Kraska K. Posttraumatic stress disorder and posttraumatic growth in HIV-infected patients–the role of coping strategies. Health Psychol Rep. 2017;5(4):323–332.
21. Ye Z, Chen L, Lin D. The relationship between posttraumatic stress disorder symptoms and posttraumatic growth among HIV-Infected men who have sex with men in Beijing, China: the mediating roles of coping strategies. Front Psychol. 2018;9:1787.
22. García FE, Barraza-Peña CG, Wlodarczyk A, Alvear-Carrasco M, Reyes-Reyes A. Psychometric properties of the Brief-COPE for the evaluation of coping strategies in the Chilean population. Psicologia. 2018;1:31.
23. Kabunga A, Anyolitho MK, Betty A. Emotional intelligence and compassion fatigue among psychotherapists in selected districts of Northern Uganda. South African J Psychol. 2020;50(3):359–370.
24. Kuo BC. Collectivism and coping: current theories, evidence, and measurements of collective coping. Int J Psychol. 2013;48(3):374–388.
25. Benyumiza D, Amongin JF, Ochaba I, et al. Factors Associated with Utilization of HIV Testing Services among Adolescents Aged 10-19 Years in Lira District, Northern Uganda: a Cross-Sectional Study. Biomed Res Int. 2021;2021:485.
26. Israel GD. Determining Sample Size. Israel GD; 1992.
27. LeardMann CA, McMaster HS, Warner S, et al. Comparison of posttraumatic stress disorder checklist instruments from Diagnostic and Statistical Manual of Mental Disorders, vs Fifth Edition in a large cohort of US Military service members and veterans. JAMA network open. 2021;4(4):e218072–e218072.
28. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34(8):669–673.
29. Maselesele VM, Idemudia ES. The role of social support in the relationship between mental health and posttraumatic stress disorder amongst orthopaedic patients. Curationis. 2013;36(1):1–7.
30. Sherr L, Nagra N, Kulubya G, Catalan J, Clucas C, Harding R. HIV infection associated post-traumatic stress disorder and post-traumatic growth–a systematic review. Psychol Health Med. 2011;16(5):612–629.
31. Beckerman NL, Auerbach C. Post-traumatic stress disorder and HIV: a snapshot of co-occurrence. Soc Work Health Care. 2010;49(8):687–702.
32. Olley B, Zeier M, Seedat S, Stein D. Post-traumatic stress disorder among recently diagnosed patients with HIV/AIDS in South Africa. AIDS Care. 2005;17(5):550–557.
33. Verhey R, Gibson L, Brakarsh J, Chibanda D, Seedat S. Prevalence and correlates of probable post-traumatic stress disorder and common mental disorders in a population with a high prevalence of HIV in Zimbabwe. Eur J Psychotraumatol. 2018;9(1):1536286.
34. Weems CF, Watts SE, Marsee MA, et al. The psychosocial impact of Hurricane Katrina: contextual differences in psychological symptoms, social support, and discrimination. Behav Res Ther. 2007;45(10):2295–2306.
35. Cohen MH, Fabri M, Cai X, et al. Prevalence and predictors of posttraumatic stress disorder and depression in HIV-infected and at-risk Rwandan women. J Women’s Health. 2009;18(11):1783–1791.
36. Wagner AC, Jaworsky D, Logie CH, et al. High rates of posttraumatic stress symptoms in women living with HIV in Canada. PLoS One. 2018;13(7):e0200526.
37. Schneider BP, Palmer GA, Romero R, O’Regan J. Post-traumatic stress disorder and quality-of-life outcomes of veterans seeking treatment in a residential rehabilitation treatment program. Military Behavioral Health. 2015;3(2):157–166.
38. Scott‐Tilley D, Tilton A, Sandel M. Biologic correlates to the development of post‐traumatic stress disorder in female victims of intimate partner violence: implications for practice. Perspect Psychiatr Care. 2010;46(1):26–36.
39. Simoni JM, Ng M. Trauma, coping, and depression among women with HIV/AIDS in New York City. AIDS Care. 2000;12(5):567–580.
40. Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence”. Psychol Inq. 2004;15(1):1–18.
41. Paivio SC, Laurent C. Empathy and emotion regulation: reprocessing memories of childhood abuse. J Clin Psychol. 2001;57(2):213–226.
42. Hamader G, Noehammer E. Prevention of Anxiety, Depression and Burnout During Medical Studies and Residency Training (Experts’ Opinion, Medical Students’ and Young Doctors’ Point of view). In: Psychology of Well-Being: Theory, Perspectives and Practice. Hauppauge, NY: Nova Science Publishers; 2013; 33–42.
43. Carlucci L, Tommasi M, Balsamo M, Furnham A, Saggino A. Religious fundamentalism and psychological well-being: an Italian study. J Psychol Theol. 2015;43(1):23–33.
44. Cotton S, Puchalski CM, Sherman SN, et al. Spirituality and religion in patients with HIV/AIDS. J Gen Intern Med. 2006;21(S5):S5–S13.
45. Liboro RM, Walsh RT. Understanding the irony: Canadian gay men living with HIV/AIDS, their Catholic devotion, and greater well-being. J Relig Health. 2016;55(2):650–670.
46. Brownley JR, Fallot RD, Wolfson Berley R, Himelhoch SS. Trauma history in African-American women living with HIV: effects on psychiatric symptom severity and religious coping. AIDS Care. 2015;27(8):964–971.
47. Wanyama J, Castelnuovo B, Wandera B, et al. Belief in divine healing can be a barrier to antiretroviral therapy adherence in Uganda. Aids. 2007;21(11):1486–1487.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
