Back to Journals » Risk Management and Healthcare Policy » Volume 16
Post-ASPECTS and Post-PC-ASPECTS Predict the Outcome of Anterior and Posterior Ischemic Stroke Following Thrombectomy
Authors Liang W, Kwan ATH , Ye H, Mofatteh M , Feng M, Wellington J, Fu P, Wei W, Sun Y, Huang J, Luo J, Chen Y , Yang S, Zhou S
Received 23 August 2023
Accepted for publication 5 December 2023
Published 16 December 2023 Volume 2023:16 Pages 2757—2769
DOI https://doi.org/10.2147/RMHP.S436661
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Wenjun Liang,1 Angela TH Kwan,2 Huifang Ye,3 Mohammad Mofatteh,4 Mingzhu Feng,1 Jack Wellington,5 Pingzhong Fu,6 Wenlong Wei,1 Yu Sun,1 Jianhui Huang,7 Jie Luo,7 Yimin Chen,1 Shuiquan Yang,1 Sijie Zhou7
1Department of Neurology and Advanced National Stroke Center, Foshan Sanshui District People’s Hospital, Foshan, People’s Republic of China; 2Faculty of Medicine, University of Ottawa, Ottawa, Ontario, Canada; 3Department of Pharmacy, Foshan Sanshui District People’s Hospital, Foshan, People’s Republic of China; 4School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, Belfast, United Kingdom; 5School of Medicine, Cardiff University, Cardiff, United Kingdom; 6Department of Radiology, Foshan Sanshui District People’s Hospital, Foshan, Guangdong Province, People’s Republic of China; 7Department of Surgery of Cerebrovascular Diseases, First People’s Hospital of Foshan, Foshan, Guangdong Province, People’s Republic of China
Correspondence: Shuiquan Yang, Department of Neurology and Advanced National Stroke Center, Foshan Sanshui District People’s Hospital, Foshan, Guangdong Province, 528100, People’s Republic of China, Email [email protected] Sijie Zhou, Department of Neurosurgery, First People’s Hospital of Foshan, Foshan, Guangdong Province, 528000, People’s Republic of China, Email [email protected]
Purpose: In this study, we aimed to determine whether post-Alberta Stroke Project Early CT Changes Score (post-ASPECTS) in anterior stroke and post-(posterior circulation) PC-ASPECTS in posterior stroke on CT can predict post-endovascular thrombectomy (EVT) functional outcomes among patients with acute ischemic stroke (AIS) after EVT.
Patients and Methods: A total of 247 consecutive patients aged 18 and over receiving EVT for LVO-related AIS were recruited into a prospective database. The data was retrospectively analyzed between March 2019 and February 2022 from two comprehensive tertiary care stroke centers: Foshan Sanshui District People’s Hospital and First People’s Hospital of Foshan in China. Patient parameters included EVT within 24 hr of symptom onset, premorbid modified Rankin scale (mRS) ≤ 2, presence of distal and terminal cerebral blood vessel occlusion, and subsequent 24– 72-hr post-stroke onset CT scan. Univariate comparisons were performed using the Fisher’s exact test or χ2 test for categorical variables and the Mann–Whitney U-test for continuous variables. Logistic regression analysis was performed to further analyze for adjusting for confounding factors. A p-value of ≤ 0.05 was statistically significant.
Results: Overall, 236 individuals with 196 anterior circulation ischemic strokes and 40 posterior strokes of basilar artery occlusion were examined. Post-ASPECTS in anterior stroke and post-pc-ASPECTS as strong positive markers of favorable outcome at 90 days post-EVT; and lower rates of inpatient mortality/hospice discharge, 90-day mortality, and 90-day poor outcome were observed. Moreover, patients in the post-ASPECTS ≥ 7 cohort experienced shorter door-to-recanalization time (DRT), puncture-to-recanalization time (PRT), and last known normal-to-puncture time (LKNPT).
Conclusion: Post-ASPECTS ≥ 7 in anterior circulation AIS and post-pc-ASPECTS ≥ 7 in posterior circulation can serve as strong prognostic markers of functional outcome after EVT.
Keywords: endovascular therapy, thrombectomy, large vessel occlusion, cerebral ischemic stroke, ASPECTS
Introduction
Stroke is the second-leading cause of death and the third-leading cause of disability globally, despite decreases in age-standardized stroke incidence and mortality in high- versus low- and middle-income countries.1 Ischemic strokes occurring in the anterior circulation are the most common of all acute ischemic strokes (AIS) and have epidemiological and clinical features distinct from posterior circulation infarctions, which account for 20–30% of all cases.2,3 Endovascular Therapy (EVT)—in the form of mechanical thrombectomy—following intravenous thrombolysis, which remains the standard of care for patients with AIS due to large vessel occlusion (LVO) of the anterior circulation.1,4–6 For posterior circulation LVO, successful reperfusion post-EVT has been shown to be associated with favorable outcomes in many previous studies.7–12 However, its efficacy has not yet been established, as results from two recent randomized clinical trials failed to show improvement in functional outcomes following EVT for posterior circulation stroke (PCS).13,14 This suggests a need to identify prognostic factors beyond recanalization that impact EVT outcomes, as poor outcomes are observed despite successful recanalization.6 Appropriate patient selection may be the solution to the success of posterior circulation-EVT.6
Early ischemic changes in the middle cerebral artery (MCA) territory on pre-treatment non-contrast CT scans (NCCT) can be quantified using the Alberta Stroke Project Early CT Changes Score (ASPECTS) for hyperacute anterior circulation ischemic stroke, which divides the MCA area into 10 regions of interest.15–17 Based on this 10-point scoring system, 10 indicates normal, and 1 point is removed for each abnormal region.1 As such, this tool can be used to select appropriate patients for EVT based on the estimation of infarct size, as it serves as a potent predictor of post-EVT functional outcomes.1,18,19 Specifically, patients with smaller baseline infarcts experience better long-term functional dependence, decreased reperfusion hemorrhage, and lower rates of mortality as compared to those with larger infarcts.19 Results from a post-hoc analysis of the PROACT II trial suggested an association between baseline APSECTS (>7 vs ≤7) and intra-arterial treatment effect.20
Previous studies have shown that patients with an ASPECTS ≥ 7 were more likely than those with ASPECTS < 7 to receive favorable post-EVT outcomes, suggesting the benefit of fast recanalization for cases with evident damage on CT scan.21 Patients with lower e-ASPECTS—a tool for automated use of ASPECTS—were found to be associated with a higher modified Rankin scale (mRS) after 3 months and an increased risk for symptomatic intracerebral hemorrhage.18,22 For posterior circulation LVO, prognostic utility has been shown in combining posterior circulation ASPECTS (PC-ASPECTS) with magnetic resonance imaging (MRI) for evaluating post-EVT functional outcomes.23 However, due to the low accessibility of MRIs, previous studies have applied PC-ASPECTS to computed tomography angiography source images (CTA-SI) for patients with suspected acute basilar artery occlusion (BAO).24 Future studies should focus on comparing the efficacy of multimodal MRI, CTA, and CT perfusion (CTP) in predicting clinical outcomes in patients with BAO and determining the most reliable scoring system.24 To our knowledge, there is only one study that applied PC-ASPECTS to pre-intervention non-contrast CT, a widely used and accessible tool to assess patients before EVT.25 Thus, in this study, we aim to determine whether post-ASPECTS in anterior circulation AIS and post-PC-ASPECTS in posterior circulation can serve as prognostic markers of functional outcome after EVT.
Materials and Methods
Study Design
This study included the retrospective analysis of prospectively collected data from 247 consecutive patients who underwent EVT for LVO-related AIS from March 2019 to February 2022 at two comprehensive tertiary care stroke centers: Foshan Sanshui District People’s Hospital and First People’s Hospital of Foshan, China. The data were derived from the Big Data Observatory Platform for Stroke in China (https://ss.chinasdc.cn) and individual hospital data platforms. Inclusion criteria were as follows: 1) patients aged 18 years or older; 2) underwent EVT within 24 hr of symptom onset; 3) with a premorbid Modified Rankin Score (mRS) ≤ 2; 4) have vessel occlusion including distal/terminal ICA, MCA-M1, MCA-M2, tandem (ICA+M1) and basilar artery; and 5) received a head CT scan after 24 to 72 hr post-onset, if the patients deteriorated, the CT was scanned earlier or followed up head image as medical necessity. Exclusion criteria included 1) a pre-EVT ASPECTS < 7 and 2) unavailable images to assess ASPECTS.
Data Collection
The following demographics and clinical data were collected for all patients: age, sex, vascular risk factors (including hypertension, diabetes, coronary artery disease, chronic kidney disease, frequency of prior stroke, smoking status, and dyslipidemia), lung infection, urinary tract infection, and serum laboratory examination. Time metrics of EVT consisted of the door-to-puncture time (DPT), door-to-recanalization time (DRT), puncture-to-recanalization time (PRT), and last known normal-to-puncture time (LKNPT). Measurements of the National Institute of Health Stroke Scale (NIHSS), pre-EVT ASPECTS, and post ASPECTS on CT scans to assess the infarct core volume, initial premorbid modified Rankin Scale (mRS), modified thrombolysis in cerebral infarction (mTICI) score, and treatment with intravenous (IV) thrombolysis were also recorded.
The frequency of symptomatic intracranial hemorrhage (sICH) was assessed for individual patient cases, which is defined as any hemorrhage related to transient neurological worsening, manifested by an increase in the NIHSS score ≥ 4. Three-month mRS scores post-EVT were evaluated by routine follow-up and used to assess patient outcomes. Favorable outcome was defined as a 90-day mRS score of 0–2, as compared to a 90-day mRS score of 3–6 for poor outcome, as shown previously.26,27 Mortality was defined as a 90-day mRS score of 6.
Ethics Approval
The study was approved by the medical ethical committee at the Foshan Sanshui District People’s Hospital. All participants’ legal guardians and/or next of kin consented to perform EVT. Written informed consent from the participants’ legal guardians and/or next of kin was not required to participate in this study due to the nature of the retrospective study with no harm. All patient data were confidential, and all procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Statistical Analysis
Statistical analysis was performed using the SPSS Statistics Package (Version 26.0; IBM Corporation, Armonk, NY, USA). Continuous variables are summarized as the mean ± standard deviation for normally distributed variables or as the median with interquartile range for non-normally distributed variables as requirements. Proportions were expressed in percentages. The independent t-test was used to compare means between groups, the non-parametric Mann–Whitney U-test for medians, and the chi-square (χ2) test and Fisher's exact test for proportions. Results were considered statistically significant for a p value < 0.05. We also calculated the area under the curve (AUC) of the receiver operating characteristic (ROC). Univariate logistic regression analyses were performed as they are shown in the Supplementary Tables 1–6. Multivariate binary logistic regression was performed to further analyze for adjusting for confounding factors. Results were considered statistically significant for a p value < 0.05.
Results
Study Population
A total of 247 patients met the inclusion criteria, with 3 excluded due to the absence of post-CT and 8 excluded for pre-EVT ASPECTS < 7. Overall, 236 patients were analyzed during the study period and incorporated into the final analysis, where 196 had anterior circulation occlusion stroke and 40 had posterior stroke of basilar occlusion. Table 1 shows the comparison of baseline demographic and clinical characteristics between individuals with post-thrombectomy ASPECTS (post-ASPECTS) ≥ 7 versus post-ASPECTS < 7. There were 110 patients with post-ASPECTS ≥ 7 (56.1%) and 86 patients with post-ASPECTS < 7 (43.9%). There were no statistically significant differences regarding age, sex, triglyceride, cholesterol, high-density lipoprotein, low-density lipoprotein, uric acid, cerebrovascular risk factors except coronary artery disease (CAD), pre-EVT ASPECTS, mRS pre-morbidity, IV thrombolysis, DPT, and length of stay of study participants (Table 1). Admission NIHSS pre-EVT (interquartile range (IQR)) of study participants between post-ASPECTS ≥ 7 and post-ASPECTS < 7 were 14.00 (10.00, 17.00) and 15.00 (12.75, 19.00), respectively (p = 0.004). Time metrics of EVT included 226.50 (166.75, 264.25) vs 248.50 (194.50, 308.25) for DRT (IQR) (p = 0.042), 54.00 (35.00, 76.00) vs 86.00 (50.75, 125.25) for PRT (IQR) (p < 0.001), and 319.50 (240.00, 495.25) vs 285.50 (195.00, 399.25) for LKNPT (IQR) (p = 0.029), respectively. The mTICI post ≥ 2b were 93.64% (n = 103) versus 73.26% (n = 3) (p < 0.001). There were significant differences in sICH at 0.91% (n = 1) vs 25.58% (n = 22) (p =< 0.001), hospitalization costs at 101,957.34 (83,996.59, 128,430.92) vs 130,348.80 (88,059.48, 164,432.45) (p = 0.002), mRS discharge (IQR) at 2.00 (1.00, 4.00) vs 5.00 (4.00, 5.00) (p < 0.001), inpatient mortality/hospice discharge at 3.64% (n = 4) vs 41.86% (n = 36) (p < 0.001), 90-day favorable outcome at 70.00% (n = 77) vs 12.79% (n = 11) (p < 0.001), 90-day mortality at 7.27% (n = 8) vs 48.84% (n = 42), and 90-day poor outcome at 30.00% (n = 33) vs 87.21% (n = 75) between post-ASPECTS ≥ 7 and post-ASPECTS < 7 (Table 1).
 |
Table 1 Characteristic and Clinical Data of Patients with Post-ASPECTS ≥ 7 versus Post-ASPECTS < 7 in Anterior Circulation Large Vessel Occlusion Following EVT |
The results of the comparison of baseline demographic and clinical characteristics between individuals with post-PC-ASPECTS ≥ 7 and post-PC-ASPECTS < 7 in posterior circulation stroke post-EVT are presented in Table 2. There were 16 patients with pc-ASPECTS ≥ 7 (40.0%) and 24 patients with pc-ASPECTS < 7 (60.0%). There were no statistically significant differences regarding age, sex, triglyceride, cholesterol, high-density lipoprotein, low-density lipoprotein, uric acid, cerebrovascular risk factors, mRS pre-morbidity, IV thrombolysis, time metrics of EVT, mTICI post ≥ 2b, sICH, length of stay, and hospitalization costs of study participants (Table 2). Admission NIHSS pre-EVT of study participants for the post-PC-ASPECTS ≥ 7 cohort [IQR: 22.50 (15.25, 26.75)] and pc-ASPECTS < 7 cohort [IQR: 25.50 (23.25, 33.50)] was statistically significant (X2 = 2.469; p = 0.013). The pc-ASPECTS ≥ 7 pre-EVT cohort [IQR: 9.00 (8.25, 9.00)] compared to the pc-ASPECTS < 7 pre-EVT cohort [IQR: 8.00 (8.00, 9.00)] was also statistically significant (X2: 2.908; p = 0.007). Additionally, there were significant differences in mRS discharge at [IQR: 2.00 (1.00, 3.00)] vs [IQR: 5.00 (5.00, 5.00)] (X2: 5.129; p < 0.001), inpatient mortality/hospice discharge at 0.00% (n = 0) vs 45.83% (n = 11) (X2: 7.947, p = 0.005), 90-day favorable outcome at 68.75% (n = 11) vs 4.17% (n = 1) (X2: 16.116, p < 0.001), 90-day mortality at 0.00% (n = 0) vs 58.33% (n = 14) (X2: 14.359, p < 0.001), and 90-day poor outcome at 31.25% (n = 5) vs 95.83% (n = 23) (X2: 16.116, p < 0.001) between PC-ASPECTS ≥ 7 and pc-ASPECTS < 7, respectively (Table 2). The mRS of post-ASPECTS in anterior and posterior circulation ischemic stroke following EVT is shown in Supplementary Tables 7 and 8, respectively.
 |
Table 2 Characteristic and Clinical Data of Patients with pc-ASPECTS ≥ 7 versus pc-ASPECTS < 7 in Posterior Circulation Stroke Following EVT |
Clinical Outcomes
For anterior circulation ischemic stroke post-EVT, the distribution of mRS from 0 to 6 at baseline for patients with post-ASPECTS ≥ 7 were 26.36%, 27.27%, 16.36%, 3.64%, 17.27%, 1.82%, and 7.27%, and for patients with post-ASPECTS < 7 were 1.16%, 4.65%, 6.98%, 18.60%, 12.79%, and 48.84%, respectively (Figure 1). We found that patients with lower post-ASPECTS (<7) accounted for a greater proportion of poor outcomes (mRS of 5: 12.79%, mRS of 6: 48.84%) as compared to patients with higher post-ASPECTS (≥7) (mRS of 5: 1.82%, mRS of 6: 7.27%).
 |
Figure 1 Distribution of mRS by baseline comparison of post-ASPECTS ≥ 7 and post-ASPECTS < 7 in anterior circulation ischemic stroke following EVT. |
For posterior circulation ischemic stroke post-EVT, the distribution of mRS from 0 to 6 at baseline for patients with post-PC-ASPECTS ≥ 7 were 18.75%, 31.25%, 18.75%, 12.50%, 12.50%, and 6.25%, and for patients with post-pc-ASPECTS < 7 were 4.17%, 25.00%, 12.50%, and 58.33%, respectively (Figure 2). Similarly, we found that patients with lower post-pc-ASPECTS (<7) accounted for a greater proportion of poor outcomes (mRS of 5: 12.50%, mRS of 6: 58.33%) as compared to patients with higher pc-ASPECTS (≥7) (mRS of 5: 6.25%, mRS of 6: 0%).
 |
Figure 2 Distribution of mRS by baseline comparison of post-PC-ASPECTS ≥ 7 and post-PC-ASPECTS < 7 in posterior circulation ischemic stroke following EVT. |
Results on the univariate analysis of the clinical outcomes between post-ASPECTS ≥ 7 and post-ASPECTS < 7 in anterior circulation ischemic stroke, after adjusting for CAD, NIHSS, and pre-EVT ASPECTS, are presented in Table 3. Significant differences were observed for inpatient mortality/hospice discharge (OR: 0.051, 95% CI: 0.016–0.164, p < 0.001), 90-day favorable outcome (OR: 15.132, 95% CI: 6.889–33.237, p < 0.001), 90-day mortality (OR: 0.089, 95% CI: 0.037–0.216, p < 0.001), and 90-day poor outcome (OR: 0.066, 95% CI: 0.030–0.145, p < 0.001).
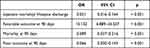 |
Table 3 Comparison of Outcome of Post-ASPECTS ≥ 7 versus Post-ASPECTS < 7 in Anterior Circulation Ischemic Stroke After Adjusting for CAD, NIHSS Pre-EVT, and ASPECTS Pre-EVT |
According to the dataset, when comparing post-PC-ASPECTS ≥ 7 and post-PC-ASPECTS < 7 in anterior circulation ischemic stroke post-adjustment of NIHSS and pre-EVT ASPECTS, patient parameters comprising 90-day favorable outcome (OR: 70.799, 95% CI: 4.550–1101.583, p = 0.002) and 90-day poor outcome (OR: 0.014, 95% CI: 0.001–0.220, p = 0.002) were both statistically significant (Table 4).
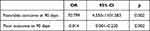 |
Table 4 Comparison of Outcome of Post-PC-ASPECTS ≥ 7 versus Post-PC-ASPECTS < 7 in Posterior Circulation Ischemic Stroke After Adjusting for, NIHSS Pre-EVT, and ASPECTS Pre-EVT |
Based on the receiving operating characteristic (ROC) curve analysis, the area under curve (AUC) for post-ASPECTS was 0.860 (95% CI, 0.809–0.911, p < 0.001) (Figure 3 and Table 5).
 |
Table 5 Area Under the Curve for Test Result Variable(s): Post-ASPECTS |
 |
Figure 3 ROC curve of post-ASPECTS predicts 90-day favorable outcome of anterior circulation ischemic stroke following EVT. The blue line represents the boundary of the post-ASPECTS AUC. |
As a result of ROC curve analysis, the AUC for PC-ASPECTS was 0.860 (95% CI, 0.809–0.911, p < 0.001) (Figure 4 and Table 6).
 |
Table 6 Area Under the Curve Test Result Variable(S): Pc-ASPECTS |
 |
Figure 4 ROC curve of post-PC-ASPECTS predicts 90-day favorable outcome of posterior circulation stroke following EVT. The blue line represents the boundary of the post-PC-ASPECTS AUC. |
Discussion
Reliable early predictions of poor outcomes after successful treatment are essential for the selection of appropriate patients for EVT upon imaging criteria to help make better decisions, improve prognosis, and reduce unnecessary cost.17,28 In this multi-center study of 247 patients, we showed that post-ASPECTS and post-PC-ASPECTS on CT can accurately predict post-EVT survival and functional outcomes of anterior and posterior AIS due to LVO, respectively. Post-ASPECTS and post-PC-ASPECTS can be dichotomized at <7 vs ≥7 to prognosticate inpatient mortality/hospice discharge, 90-day favorable outcome, 90-day poor outcome, and 90-day mortality. Consistent with previous studies, we found that both post-ASPECTS and post-PC-ASPECTS ≥ 7 serve as strong positive markers of favorable outcome at 90 days post-EVT; as well, lower rates of inpatient mortality/hospice discharge, 90-day mortality, and 90-day poor outcome were observed.17,27–29 Differences between post-ASPECTS ≥ 7 versus post-ASPECTS < 7 were statistically significant for inpatient mortality/hospice discharge, 90-day favorable outcome, 90-day poor outcome, and 90-day mortality after adjusting for CAD, NIHSS pre-EVT, and ASPECTS pre-EVT. For pc-ASPECTS ≥ 7 versus pc-ASPECTS < 7, only 90-day favorable outcome and 90-day poor outcome were statistically significant after adjusting for CAD, NIHSS pre-EVT, and ASPECTS pre-EVT.
For acute BAO—the most devastating form of posterior circulation infarction—the following factors have been identified as independent variables impacting functional outcomes: basilar artery recanalization, location of thrombus, length of obstruction, and state of collaterals.24 However, there are still presently no criteria developed for the appropriate identification of patients who would benefit from EVT.24 Our current standard of care for the diagnosis of PCS is MRI using diffusion (DWI)- or perfusion-weighted (PWI) imaging sequences, but there are drawbacks such as general inaccessibility in local hospitals, limited practicability for unstable patients, comparatively higher costs, and slow scanning speed.24,30
CT remains the imaging modality of first choice for AIS patients due to its widespread availability.31,32 Non-contrast CT (NCCT) is used to exclude intracranial hemorrhage and non-stroke pathologies, followed by CTA-SI, an advanced CT technique, to further characterize early signs of an infarct such as tissue status.17,33 CTA also provides value in the detection of vessel occlusion. Thus, at community hospitals without readily available MRIs, an alternative diagnostic tool that can accurately and rapidly detect intracranial hemorrhage, assess vessel status and extent of ischemia, identify occlusion of major arteries at the base of the brain if present, and estimate at-risk tissue is needed. A previous study found that the quality of diagnostic assessment by combining non–contrast-enhanced CT (to exclude intracranial hemorrhage), CTA (to assess vessel status), and early contrast-enhanced CTA-SI (to predict final infarct volume) together is comparable to that of multiparametric stroke MRI, including DWI, in patients with AIS within 6 hr of onset.33 This diagnostic protocol—similar to the stroke MRI mismatch concept—can identify patients who are more likely to be at risk of infarct growth based on the assessment of their collateral status, which is strongly tied to significantly poorer clinical outcomes.34 Consequently, combined CT/CTA/CTA-SI may be used not only to understand stroke pathology but also to predict clinical outcomes.
Although there are advanced imaging modalities, quantification of hypoattenuation on NCCT is widely used to assess patients pre-EVT based on baseline infarct size, which, as shown by the PROACT II trial, is associated with intra-arterial treatment effect.19 Patients with smaller infarcts (APSECTS > 7) were five times more likely to have better functional outcomes with intra-arterial treatment compared to the control group, whereas patients with larger infarcts (APSECTS ≤ 7) did not benefit from treatment.19 Our findings show post-ASPECTS and post-PC-ASPECTS ≥ 7 groups had higher rates of favorable outcome at 90 days, and lower rates of inpatient mortality/hospice discharge, 90-day mortality, and 90-day poor outcome were observed following EVT treatment. Thus, post-ASPECTS and post-pc-ASPECTS applied to NCCT have strong prognostic utility in determining clinical outcomes of anterior and posterior circulation AIS, respectively.17,24,25,35 Moreover, we found that patients in the post-ASPECTS ≥ 7 anterior circulation group also had shorter DRT, PRT, and LKNPT. To our knowledge, there is only one other study that applied pc-ASPECTS to pre-intervention NCCT; they found that patients of BAO with a pc-ASPECTS ≥ 5 could benefit from EVT.25 Results from the current study can be used in combination with other variables to build prognostic models to predict the outcome of EVT in stroke patients.36–38
Time is brain; we should spare no effort to help reduce procedural times and LKNPT through workflow optimization with multidisciplinary collaboration, reduce infarct volume and early prediction to improve endovascular time metrics and patient outcomes.39–43 DRT and PRT can be further shortened through the standardization of acute stroke workflows to improve patient outcomes.40
The main limitations of this study include its retrospective study design and small sample size. Future large-scale cohort studies with larger sample sizes are required to validate and expand these findings. In addition, the current study lacks information on follow-up therapeutic drugs, such as antiplatelets and anticoagulants, due to the unavailability of patients, which may affect patient outcomes. Despite these limitations, our findings add to the overall body of knowledge on its prognostic utility in evaluating post-EVT functional outcomes among patients with anterior and posterior circulation AIS-LVO.
Conclusion
In conclusion, post-ASPECTS ≥ 7 in anterior circulation AIS and post-PC-ASPECTS ≥ 7 in posterior circulation can serve as strong prognostic markers of functional outcome after EVT.
Data Sharing Statement
Data and materials will be made available by contacting the corresponding authors, either Shuiquan Yang or Sijie Zhou.
Acknowledgments
We would like to thank all colleagues for the data collection and all patients for their contribution.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accounFigure for all aspects of the work.
Funding
The study was supported by the Foshan Science and Technology Bureau (Grant No. 2220001005022) (Grant No.2220001005354), the Medical Science and Technology Research Foundation of Guangdong Province (Grant No. 20221027164016611), the Foshan 14th Five-Year Plan Key Discipline Foundation, China, the Guangdong provincial TCM Bureau Key Discipline Foundation, China.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ansari J, Triay R, Kandregula S, Adeeb N, Cuellar H, Sharma P. Endovascular intervention in acute ischemic stroke: history and evolution. Biomedicines. 2022;10(2):418. doi:10.3390/biomedicines10020418
2. von Sarnowski B, Schminke U, Grittner U, et al. Posterior versus anterior circulation stroke in young adults: a comparative study of stroke aetiologies and risk factors in stroke among young Fabry patients (sifap1). Cerebrovasc Dis. 2017;43(3–4):152–160. doi:10.1159/000454840
3. Cai Y, Liu X, Zhang L, Guo H, Gong Q, Lv F. Prevalence and characteristics of atherosclerotic plaque: left compared with right arteries and anterior compared with posterior circulation stroke. Eur J Radiol. 2021;142:109862. doi:10.1016/j.ejrad.2021.109862
4. Saver JL, Goyal M, van der Lugt A, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316(12):1279–1288. doi:10.1001/jama.2016.13647
5. Campbell BCV, Nguyen TN. Advances in Stroke: treatments-Interventional. Stroke Jan. 2022;53(1):264–267. doi:10.1161/strokeaha.121.037039
6. Lee SJ, Hong JM, Kim JS, Lee JS. Endovascular treatment for posterior circulation stroke: ways to maximize therapeutic efficacy. J Stroke. 2022;24(2):207–223. doi:10.5853/jos.2022.00941
7. Zi W, Qiu Z, Wu D, et al. Assessment of endovascular treatment for acute basilar artery occlusion via a nationwide prospective registry. JAMA Neurol. 2020;77(5):561–573. doi:10.1001/jamaneurol.2020.0156
8. Mokin M, Sonig A, Sivakanthan S, et al. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke Mar. 2016;47(3):782–788. doi:10.1161/strokeaha.115.011598
9. Bouslama M, Haussen DC, Aghaebrahim A, et al. Predictors of good outcome after endovascular therapy for vertebrobasilar occlusion stroke. Stroke. 2017;48(12):3252–3257. doi:10.1161/strokeaha.117.018270
10. Gory B, Mazighi M, Blanc R, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg. 2018;129(6):1482–1491. doi:10.3171/2017.7.Jns171043
11. Gory B, Mazighi M, Labreuche J, et al. Predictors for mortality after mechanical thrombectomy of acute basilar artery occlusion. Cerebrovasc Dis. 2018;45(1–2):61–67. doi:10.1159/000486690
12. Novakovic-White R, Corona JM, White JA. Posterior circulation ischemia in the endovascular era. Neurology. 2021;97(20 Suppl 2):S158–s169. doi:10.1212/wnl.0000000000012808
13. Liu X, Dai Q, Ye R, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. 2020;19(2):115–122. doi:10.1016/s1474-4422(19)30395-3
14. Langezaal LCM, van der Hoeven E, Mont’Alverne FJA, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. 2021;384(20):1910–1920. doi:10.1056/NEJMoa2030297
15. Leker RR, Honig A, Filioglo A, Simaan N, Gomori JM, Cohen JE. Post-stroke ASPECTS predicts outcome after thrombectomy. Neuroradiology. 2021;63(5):769–775. doi:10.1007/s00234-020-02576-9
16. Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355(9216):1670–1674. doi:10.1016/s0140-6736(00)02237-6
17. Coutts SB, Lev MH, Eliasziw M, et al. ASPECTS on CTA source images versus unenhanced CT: added value in predicting final infarct extent and clinical outcome. Stroke. 2004;35(11):2472–2476. doi:10.1161/01.STR.0000145330.14928.2a
18. Pfaff J, Herweh C, Schieber S, et al. e-ASPECTS correlates with and is predictive of outcome after mechanical thrombectomy. AJNR Am J Neuroradiol. 2017;38(8):1594–1599. doi:10.3174/ajnr.A5236
19. Yoo AJ, Berkhemer OA, Fransen PSS, et al. Effect of baseline Alberta stroke program early CT Score on safety and efficacy of intra-arterial treatment: a subgroup analysis of a randomised Phase 3 trial (MR CLEAN). Lancet Neurol. 2016;15(7):685–694. doi:10.1016/s1474-4422(16)00124-1
20. Hill MD, Rowley HA, Adler F, et al. Selection of acute ischemic stroke patients for intra-arterial thrombolysis with pro-urokinase by using ASPECTS. Stroke. 2003;34(8):1925–1931. doi:10.1161/01.Str.0000082483.37127.D0
21. Goyal M, Menon BK, Coutts SB, Hill MD, Demchuk AM. Effect of baseline CT scan appearance and time to recanalization on clinical outcomes in endovascular thrombectomy of acute ischemic strokes. Stroke. 2011;42(1):93–97. doi:10.1161/strokeaha.110.594481
22. Catanese L, Tarsia J, Fisher M. Acute ischemic stroke therapy overview. Circ Res. 2017;120(3):541–558. doi:10.1161/circresaha.116.309278
23. Khatibi K, Nour M, Tateshima S, et al. Posterior circulation thrombectomy-pc-ASPECT score applied to preintervention magnetic resonance imaging can accurately predict functional outcome. World Neurosurg. 2019;129:e566–e571. doi:10.1016/j.wneu.2019.05.217
24. Ouyang K, Kang Z, Liu Z, et al. Posterior circulation ASPECTS on CT angiography predicts futile recanalization of endovascular thrombectomy for acute basilar artery occlusion. Front Neurol. 2022;13:831386. doi:10.3389/fneur.2022.831386
25. Sang H, Li F, Yuan J, et al. Values of baseline posterior circulation acute stroke prognosis early computed tomography score for treatment decision of acute basilar artery occlusion. Stroke Mar. 2021;52(3):811–820. doi:10.1161/strokeaha.120.031371
26. Chen Y, Diana F, Mofatteh M, et al. Functional and technical outcomes in acute ischemic stroke patients with hyperdense middle cerebral artery sign treated with endovascular thrombectomy. Front Neurol. 2023;14:1150058. doi:10.3389/fneur.2023.1150058
27. Lai Y, Diana F, Mofatteh M, et al. Predictors of failure of early neurological improvement in early time window following endovascular thrombectomy: a multi-center study. Front Neurol. 2023;14:1227825. doi:10.3389/fneur.2023.1227825
28. Lu WZ, Lin HA, Bai CH, Lin SF. Posterior circulation acute stroke prognosis early CT scores in predicting functional outcomes: a meta-analysis. PLoS One. 2021;16(2):e0246906. doi:10.1371/journal.pone.0246906
29. Guillaume M, Lapergue B, Gory B, et al. Rapid successful reperfusion of basilar artery occlusion strokes with pretreatment diffusion-weighted imaging posterior-circulation ASPECTS <8 is associated with good outcome. J Am Heart Assoc. 2019;8(10):e010962. doi:10.1161/jaha.118.010962
30. Schramm P, Schellinger PD, Fiebach JB, et al. Comparison of CT and CT angiography source images with diffusion-weighted imaging in patients with acute stroke within 6 hours after onset. Stroke. 2002;33(10):2426–2432. doi:10.1161/01.str.0000032244.03134.37
31. Song Y, Shen F, Dong Q, Wang L, Mi J. Prediction of late hospital arrival in patients with mild and rapidly improving acute ischemic stroke in a rural area of China. Risk Manag Healthc Policy. 2023;16:1119–1129. doi:10.2147/rmhp.S414700
32. Wu K, Xiong Z, Ding Y. Management of elevated blood pressure after stroke thrombectomy for anterior circulation. Risk Manag Healthc Policy. 2021;14:405–413. doi:10.2147/rmhp.S285316
33. Douglas V, Shamy M, Bhattacharya P. Should CT angiography be a routine component of acute stroke imaging? Neurohospitalist. 2015;5(3):97–98. doi:10.1177/1941874415588393
34. Schramm P, Schellinger PD, Klotz E, et al. Comparison of perfusion computed tomography and computed tomography angiography source images with perfusion-weighted imaging and diffusion-weighted imaging in patients with acute stroke of less than 6 hours’ duration. Stroke. 2004;35(7):1652–1658. doi:10.1161/01.Str.0000131271.54098.22
35. Caruso P, Ridolfi M, Lugnan C, et al. Multimodal CT pc-ASPECTS in infratentorial stroke: diagnostic and prognostic value. Neurol Sci. 2021;42(10):4231–4240. doi:10.1007/s10072-021-05072-x
36. Chen Y, Zhou S, Yang S, et al. Developing and predicting of early mortality after endovascular thrombectomy in patients with acute ischemic stroke. Front Neurosci. 2022;16:1034472. doi:10.3389/fnins.2022.1034472
37. Chen Y, Nguyen TN, Mofatteh M, et al. Association of early increase in body temperature with symptomatic intracranial hemorrhage and unfavorable outcome following endovascular therapy in patients with large vessel occlusion stroke. J Integr Neurosci. 2022;21(6):156. doi:10.31083/j.jin2106156
38. Wu W, Pitton Rissardo J, Nguyen TN, et al. Effect of atrial fibrillation on outcomes in patients with anterior circulation occlusion stroke receiving endovascular therapy. Front Aging Neurosci. 2023;15:1160265. doi:10.3389/fnagi.2023.1160265
39. Chen Y, Nguyen TN, Wellington J, et al. Shortening door-to-needle time by multidisciplinary collaboration and workflow optimization during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2022;31(1):106179. doi:10.1016/j.jstrokecerebrovasdis.2021.106179
40. Yang S, Yao W, Siegler JE, et al. Shortening door-to-puncture time and improving patient outcome with workflow optimization in patients with acute ischemic stroke associated with large vessel occlusion. BMC Emerg Med. 2022;22(1):136. doi:10.1186/s12873-022-00692-8
41. Wang D, Shu H, Meng Y, Zhang H, Wang H, He S. Factors promoting futile recanalization after stent retriever thrombectomy for stroke affecting the anterior circulation: a retrospective analysis. World Neurosurg. 2020;133:e576–e582. doi:10.1016/j.wneu.2019.09.098
42. Raoult H, Eugène F, Ferré JC, et al. Prognostic factors for outcomes after mechanical thrombectomy with solitaire stent. J Neuroradiol. 2013;40(4):252–259. doi:10.1016/j.neurad.2013.04.001
43. Hou J, Guo Z-L, Huang Z-C, Wang H-S, You S-J, Xiao G-D. Influences of different referral modes on clinical outcomes after endovascular therapy for acute ischemic stroke. BMC Neurology. 2022;22(1):228. doi:10.1186/s12883-022-02751-w
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
